The main objective in the imaging differential diagnosis of an ovarian mass is to establish whether it is cystic or solid; solid lesions are less common. Ovarian fibromatosis is a benign disease of the ovary that is rarely included in the differential diagnosis of solid ovarian lesions. Characteristic features of masses that have a fibrous component are low signal in T1-weighted MRI sequences and especially in T2-weighted MRI sequences. The presence of peripheral fibrotic tissue around the residual ovarian tissue is specific to ovarian fibromatosis; on MRI, this results in marked hypointensity on T2-weighted images that has been dubbed the “black garland sign”. This sign, together with slight peripheral enhancement after the administration of contrast material and the preservation of the ovarian architecture, facilitates the diagnosis, making it possible to avoid unnecessary surgical interventions.
El primer objetivo del diagnóstico diferencial por imagen ante una masa ovárica es establecer su naturaleza quística o, menos frecuente, sólida. La fibromatosis ovárica es una patología benigna del ovario rara, incluida en el diagnóstico diferencial ante el hallazgo de lesiones ováricas sólidas. Características propias de las masas que presentan componente fibrótico son su baja señal en secuencias de resonancia magnética potenciadas en T1 y especialmente en T2. La presencia de tejido fibrótico periférico alrededor del tejido ovárico residual es una característica específica en la fibromatosis ovárica y que tiene como traducción en la RM una marcada hipointensidad en T2 conocida como “signo de la guirnalda negra”. Este signo, junto con una débil captación poscontraste periférica, así como la preservación de la arquitectura ovárica, nos facilita el diagnóstico y puede evitar cirugías innecesarias.
The differential diagnosis of ovarian masses is very broad; neoplastic lesions represent the primary entity to be considered. For this reason, on many occasions it is decided to opt for aggressive surgical treatment when diagnostic imaging is inconclusive. However, benign ovarian masses are very common, and a correct preoperative diagnosis can allow for more conservative treatment, especially in women of childbearing age.1
Case descriptionA 41-year-old nulligravida woman with a history of irregular menstrual cycles and amenorrhoea for the past two years visited the gynaecological emergency unit due to hypogastric discomfort that had started two months earlier. The only laboratory finding of note was slight elevation of the CA-125 marker (46U/mL; normal <35U/mL).
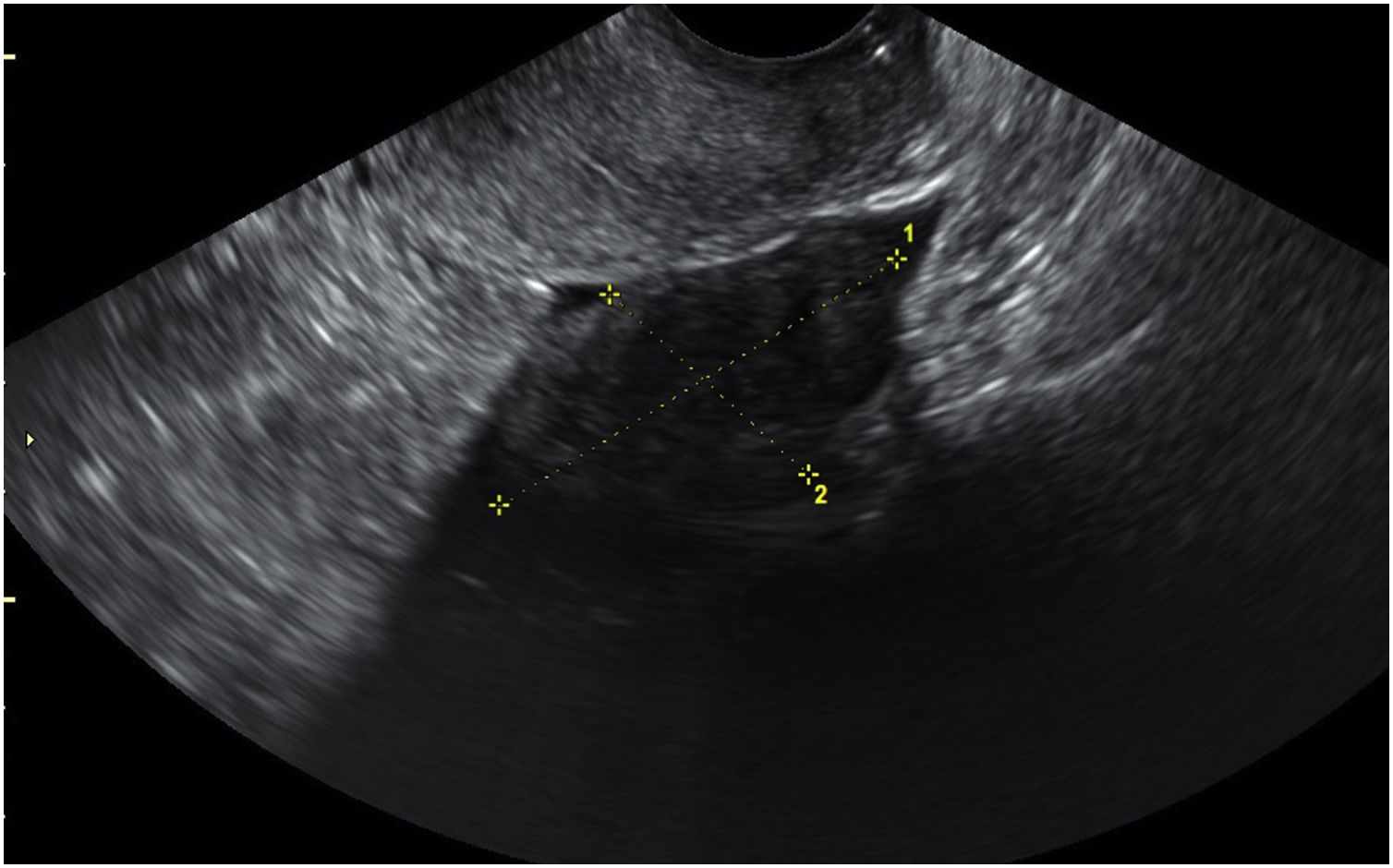
The patient’s physical examination included a pelvic examination in which a firm, immobile mass at the base of the Pouch of Douglas was palpated. An emergency transvaginal ultrasound detected two heterogeneous solid lesions at the base of the Pouch of Douglas (Fig. 1). With this discovery, a decision was made to contact the diagnostic imaging department to complete the study.
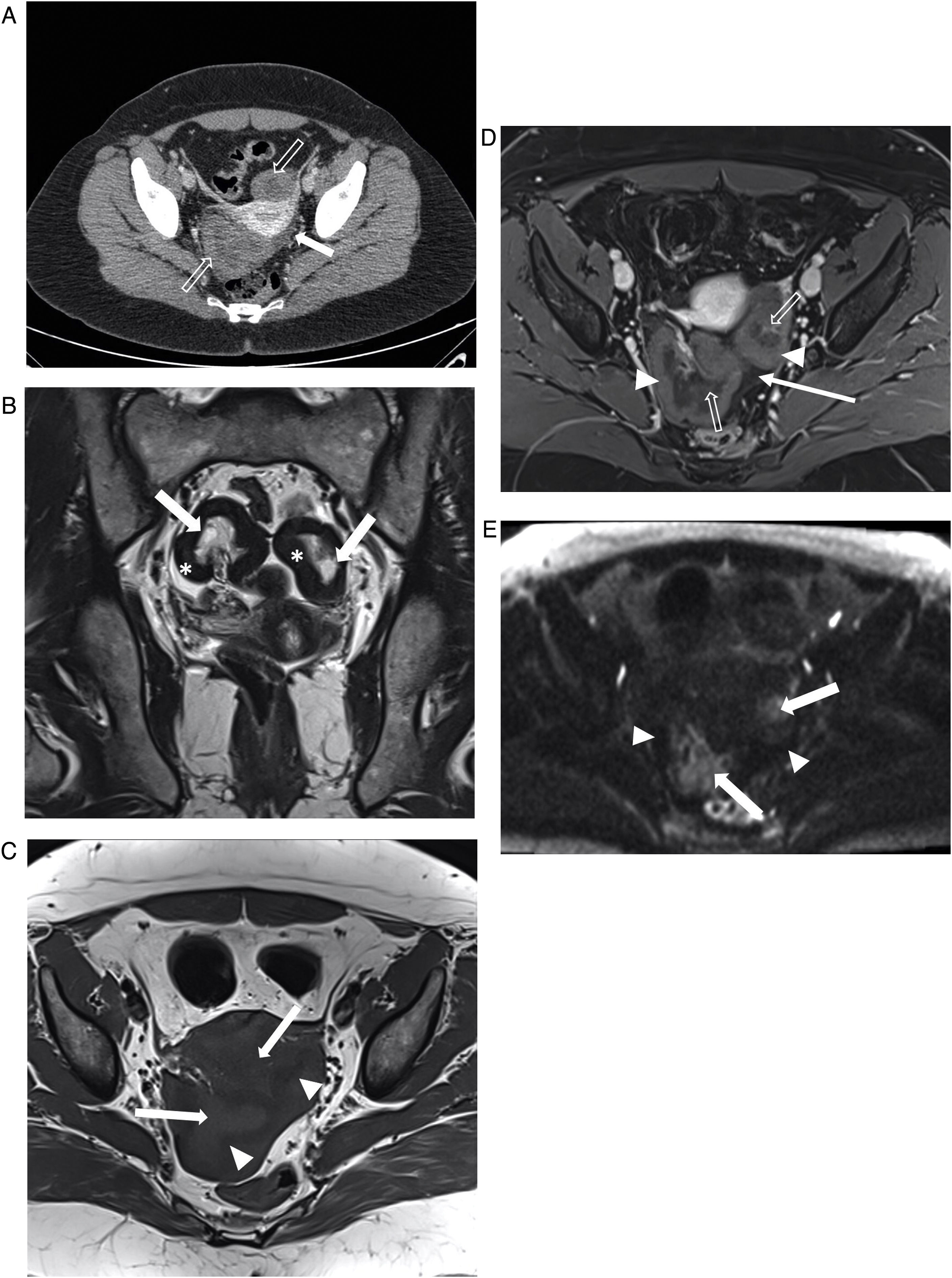
An abdominal and pelvic computed tomography (CT) scan with intravenous contrast (Fig. 2A) confirmed the presence of two well-delimited parauterine lesions, with slight thick peripheral enhancement and central hypouptake. The study was completed with pelvic magnetic resonance imaging (MRI) (Fig. 2B–E), which identified two polylobulated lesions measuring approximately 6cm on the left side and 5cm on the right side. Both images corresponded to enlarged ovaries with a thickened, markedly hypointense cortex on T2-weighted sequences in relation to the presence of peripheral fibrous tissue, known as the “black garland sign”.1 The central ovarian stroma was intact, with at least one identifiable follicle. Following intravenous contrast administration, slight enhancement of the peripheral cortical region was seen with hypointensity in the central region. On diffusion-weighted sequences with a high b value, both adnexal lesions showed a low peripheral signal and a central area of high signal intensity. The findings reported were highly suggestive of ovarian fibromatosis. None of the imaging tests showed associated findings raising suspicion of malignancy (lymphadenopathy, peritoneal carcinomatosis, etc.).
A) Axial image from abdominal and pelvic computed tomography with intravenous contrast identifying two parauterine masses with a hypodense centre and a peripheral margin with a density similar to muscle (hollow arrows). They are associated with scant free fluid at the base of the Pouch of Douglas (white arrow). B) Coronal T2-weighted magnetic resonance imaging (MRI) of the pelvis showing that both ovaries are enlarged, with follicles in the central region (white arrows). Thickened, well-delimited and markedly hypointense ridges consistent with the “black garland sign” (asterisks) can be observed. C) Axial T1-weighted MRI of the pelvis with no intravenous contrast identifying enlarged ovaries with a slightly lesser intensity on their periphery (arrow tips) compared to the central stroma (white arrows). D) Axial T1-weighted MRI with fat suppression acquired following administration of intravenous contrast showing weak peripheral uptake by the fibrous part of both ovaries (arrow tips) with hypointensity of the central part (hollow arrow). Scant free fluid is identified at the base of the Pouch of Douglas (white arrow). E) Axial diffusion-weighted MRI (b 800). Both adnexal lesions show a low peripheral signal (arrow tips), with central hyperintensity corresponding to areas of stromal oedema (white arrow), subsequently confirmed in the pathology analysis.
As the patient suffered from prolonged amenorrhoea and was experiencing discomfort, in accordance with her wishes, surgical removal was chosen. The operation consisted of a bilateral salpingo-oophorectomy, yielding an intraoperative finding of bilateral pearly, very firm ovarian masses.
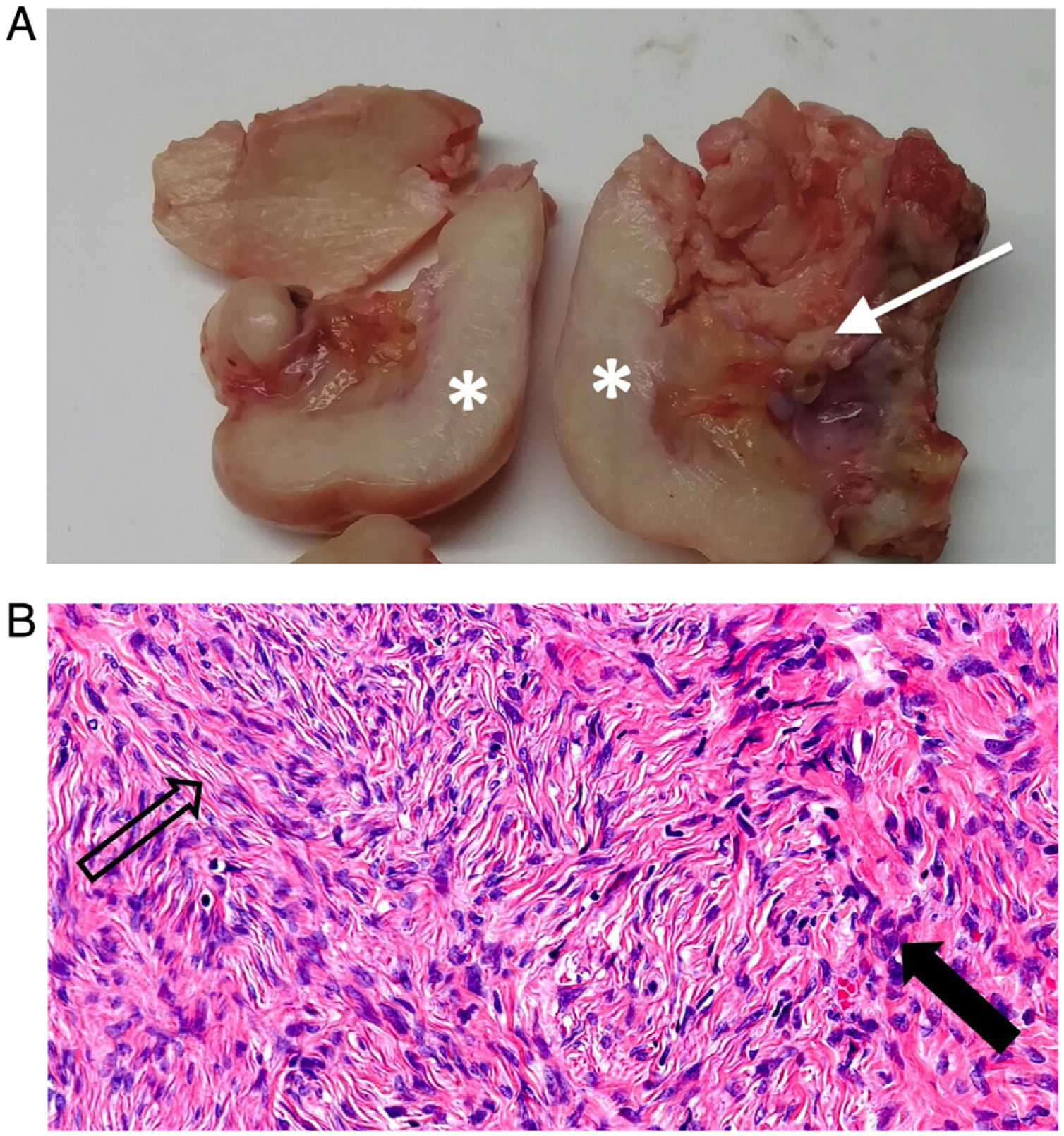
The macroscopic anatomopathological analysis (Fig. 3A) of the surgical specimens showed ovaries with a peripheral ridge of whitish tissue exhibiting an elastic consistency, consistent with fibrotic tissue, and a yellowish centre with vessels inside in relation to preserved ovarian stroma. The microscopic analysis (Fig. 3B) showed replacement of the peripheral ovarian parenchyma featuring fusocellular proliferation with areas of collagen and a central stromal oedema. All this confirmed the diagnosis of bilateral ovarian fibromatosis.
A) Macroscopic specimens from both ovaries following surgery. The right ovary (left side of image) and the left ovary (right side of image), previously fragmented, enabling visualisation of a peripheral ridge of homogeneous whitish tissue exhibiting an elastic consistency, consistent with fibrotic tissue (asterisks). The centre is composed of yellowish stroma with vessels (arrow). The macroscopic findings are consistent with bilateral ovarian fibromatosis. B) Haematoxylin-eosin staining at 40x magnification of the ovary showing replacement of more than 90% of the parenchyma with fusocellular proliferation (black arrow) forming intertwined bundles with variable areas of collagen and stromal oedema (hollow arrow).
Ovarian fibromatosis is a very uncommon benign condition, first described by Scully and Young2 in 1984, which usually affects young women, with a mean age of 25 years. It presents with menstrual abnormalities as well as abdominal pain in most cases, although it may also be asymptomatic. Its involvement is predominantly unilateral, although there are some examples of bilateral involvement, as in our case.
Histologically, ovarian fibromatosis is characterised by proliferation of collagen-producing fusiform cells around normal ovarian structures. Although its pathophysiology is not entirely clear, it seems that the lesion could be secondary to partial or intermittent torsion leading to venous and lymphatic obstruction. The disease bears resemblances to massive ovarian oedema, since both involve enlarged ovaries with preservation of internal ovarian structures. However, they differ in terms of the nature of the abnormal tissue, which is fibrotic in fibromatosis and oedematous in massive ovarian oedema.3 However, as seen in the microscopic analysis in our case, it is possible to detect foci of stromal oedema in ovaries with fibromatosis. In fact, there are reports in the scientific literature of foci of stromal oedema similar to foci of massive ovarian oedema in up to 50% of cases of ovarian fibromatosis. This would point to a possible link between the two conditions.4
In 2003, Bazot et al.5 reported the case of homogeneous, low-signal bilateral ovarian masses on T2-weighted sequences corresponding to fibrous infiltration of the ovary. They stressed that partial preservation of normal ovarian structures distinguishes this from other ovarian masses. However, this characteristic image of markedly hypointense fibrous tissue on T2-weighted sequences around the residual ovary was finally described by Takeuchi et al.1 as the “black garland sign” (Fig. 2B). Although it is not always present, the “black garland sign” is very specific to ovarian fibromatosis and was subsequently reported by other authors.6,7
The differential diagnosis based on its hypointensity on T1 and T2 sequences should be made with other entities that also show it, such as fibromas, fibrothecomas, Brenner tumours and Krukenberg tumours.8 However, imaging of preserved central ovarian structures surrounded by fibrous tissue is not observed in these lesions and may reflect the specific characteristics of ovarian fibromatosis. In addition, Krukenberg tumours show strong contrast uptake on both CT and MRI imaging,8 whereas reported cases of ovarian fibromatosis show weak uptake on post-contrast T1-weighted sequences.1 Aggressive pelvic fibromatosis secondarily affecting the ovaries is another differential diagnosis that must be considered, but it is distinguished by extraovarian involvement which is not typical in ovarian fibromatosis.9 In addition, an association with other diseases such as abdominal fibromatosis, sclerosing peritonitis and Meigs syndrome has been reported.10
In conclusion, ovarian fibromatosis is a disease with a low prevalence, which may interfere with radiological interpretation and cause it to be initially omitted from the differential diagnoses of solid ovarian masses. Visualisation of the “black garland sign” on MRI, given its specificity, should lead to it being considered as a possible diagnosis.
Authorship- 1
Responsible for study integrity:
- 2
Study concept: MSU, CGE, LCA.
- 3
Study design: MSU, CGE, LCA.
- 4
Data collection: MSU, CGE, LCA.
- 5
Data analysis and interpretation: CGE, LCA.
- 6
Statistical processing: N/A.
- 7
Literature search: N/A.
- 8
Drafting of the article: MSU.
- 9
Critical review of the manuscript with intellectually significant contributions: CGE, LCA.
- 10
Approval of the final version: MSU, CGE, LCA.
The authors declare that they have no conflicts of interest.
Please cite this article as: Santos Urios M, García Espasa C, Concepción Aramendía L. Fibromatosis ovárica: “signo de la guirnalda negra”. Radiología. 2022;64:164–168.