Perinatal testicular torsion, defined as torsion occurring in the prenatal period or in the first month after birth, accounts for 10% of all cases of testicular torsion in pediatric patients. Most are extravaginal, and intravaginal torsion is rare. Its management is controversial, due to the low viability of the testis and the possibility of bilateral torsion. Ultrasonography is the method of choice to study testicular torsion. Combining B-mode and power Doppler imaging facilitates a fast reliable diagnosis. We review the ultrasonographic appearance of neonatal testicular torsion for each presentation, the differential diagnosis with other causes of increased scrotal volume in neonates, and its treatment.
La torsión testicular perinatal constituye el 10% de las torsiones testiculares en la edad pediátrica y se produce en el periodo prenatal o neonatal durante el primer mes de vida. La mayoría son extravaginales, siendo improbable la torsión intravaginal. Su manejo es controvertido debido a la baja viabilidad del testículo y a la posibilidad de torsión bilateral. La ecografía es el método de elección para su estudio. La combinación del modo B con el Doppler color o el power Doppler facilita el diagnóstico de forma rápida y segura. Revisamos la apariencia ecográfica de la torsión testicular neonatal en cada una de sus formas de presentación, el diagnóstico diferencial con otras causas de aumento de la bolsa escrotal en el neonato, y finalmente su tratamiento.
In the perinatal testicular torsion (PTT) the testis rotates around its vascular pedicle affecting venous and arterial flows causing ischemias, infarctions and necrosis.
The tunica albuginea that stems from the vaginal process of the peritoneum surrounds the testicle and the epididymis and meets the tunica vaginalis in the posterior-lateral side of the testis and is anchored to the scrotal wall.
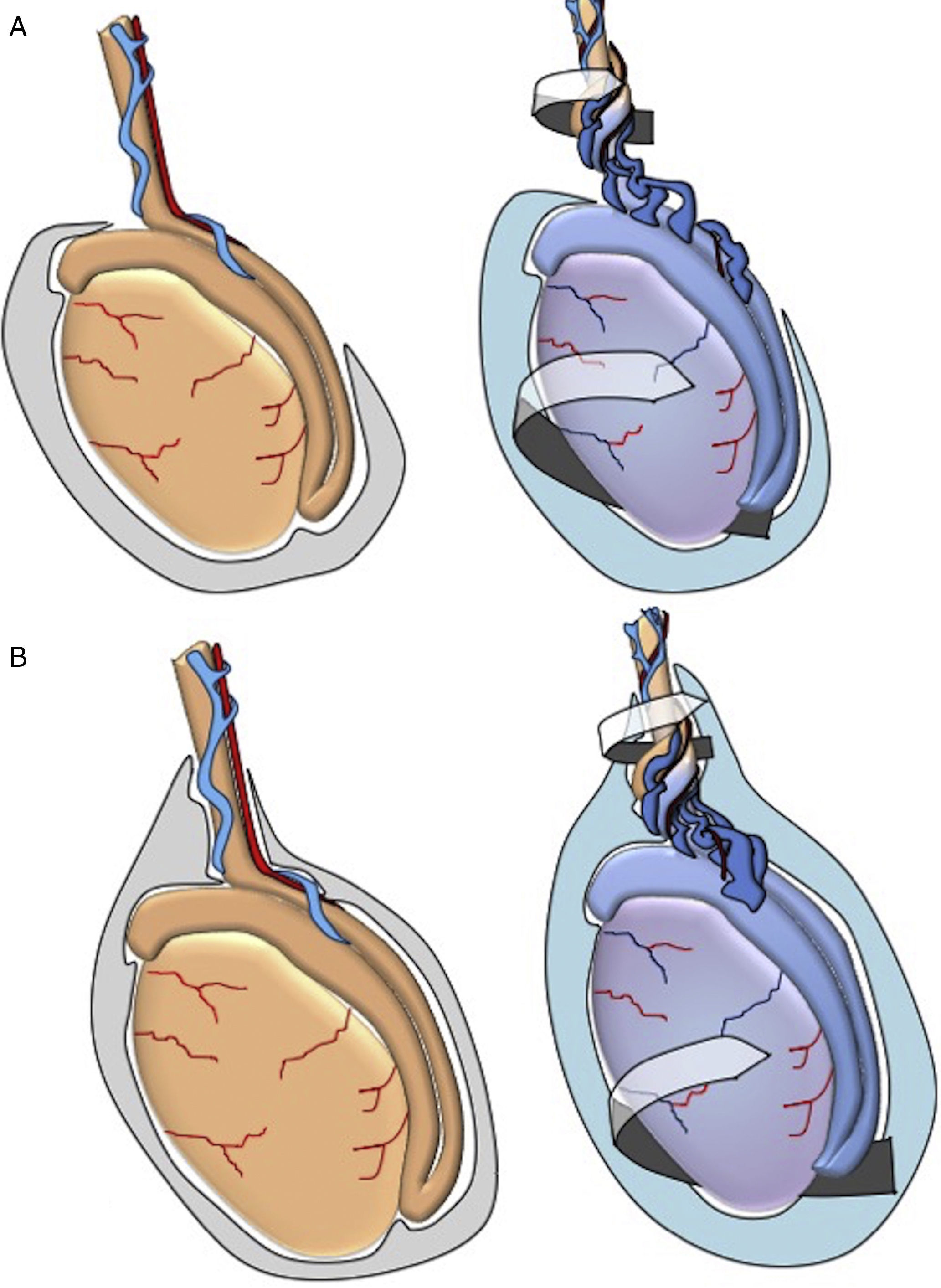
The lower pole of the testis with its tunica vaginalis fixes into the scrotal wall through the scrotal ligament or gubernaculum testis. Extravaginal torsion occurs in fetuses and newborn babies due to weak anchoring between the tunica vaginalis and the scrotal wall that allows the tunica vaginalis and its content to rotate together around the axis of the spermatic cord (Fig. 1). Normally the gubernaculum testis se acaba fully develops during the first three months of life and extravaginal torsion is rare beyond that age. It is more common in newborn babies after term pregancies, breech births and after long or traumatic deliveries.1,2
Scheme showing the testicular anatomy and the different mechanism of extravaginal torsion so typical of the perinatal age when the loose anchoring between the tunica vaginalis and the scrotal wall allows the tunica vaginalis and its content to rotate around the spermatic cord (A). The (B) figure shows the tunica vaginalis totally covering the testis which in turn explains the intravaginal torsion that is so typical of teenagers.
Around 70 per cent of all PTTs are intrauterine and the remaining 30 per cent happen during the 1st month of life.1–3 There is no preference for one side or the other, and PTTs are bilateral in 10 per cent of all case – usually synchronic.4
The PTT clinical presentation is that of a large, edematous scrotal sac that is painful when it is of postnatal establishment while it appears hard, painless and bluish when the torsion is prenatal. The assessment of the crematesric reflex is not significant since only 48 per cent of all healthy babies have it at birth being of low clinical utility under two and a half years of age.5,6
While a bilateral PTT is regarded as a surgical emergency due to high-probability anorchia, the management of unilateral PTTs remains controversial.1,7
The ultrasound is the modality of choice for the study of PTTs and there is a clear correlation between the ultrasound findings and the time to progression ratio of PTTs.8,9
We assessed the ultrasound appearance of PTTs in each and every single clinical presentation, and the differential diagnosis with other causes scrotal sac enlargement in the newborn infant and ultimately we assessed the appropriate therapy.
Image findingsPTTs have two well-differentiated clinical presentations: prenatal and neonatal.
Most prenatal testicular torsions occur during the 34th and 36th weeks of pregnancy whether intra-uterus or during delivery and they become evident at birth.10 Based on the time elapsed between torsion and birth, the clinical exploration varies ranging from no palpation of the testicle inside the sac to that same testicle being atrophic or finding one enlarged scrotal sac with indurated mass and no pain.
Neonatal testicular torsion is clinically similar to the sight late: the newborn infant shows a normal scrotal sac and in acute phases inguinoscrotal swelling, skin decoloration and, above all, pain.
Ultrasounds in mode B and Doppler help us assess both the testicular morphology and perfusion – something more correlated with the chronology of torsion.
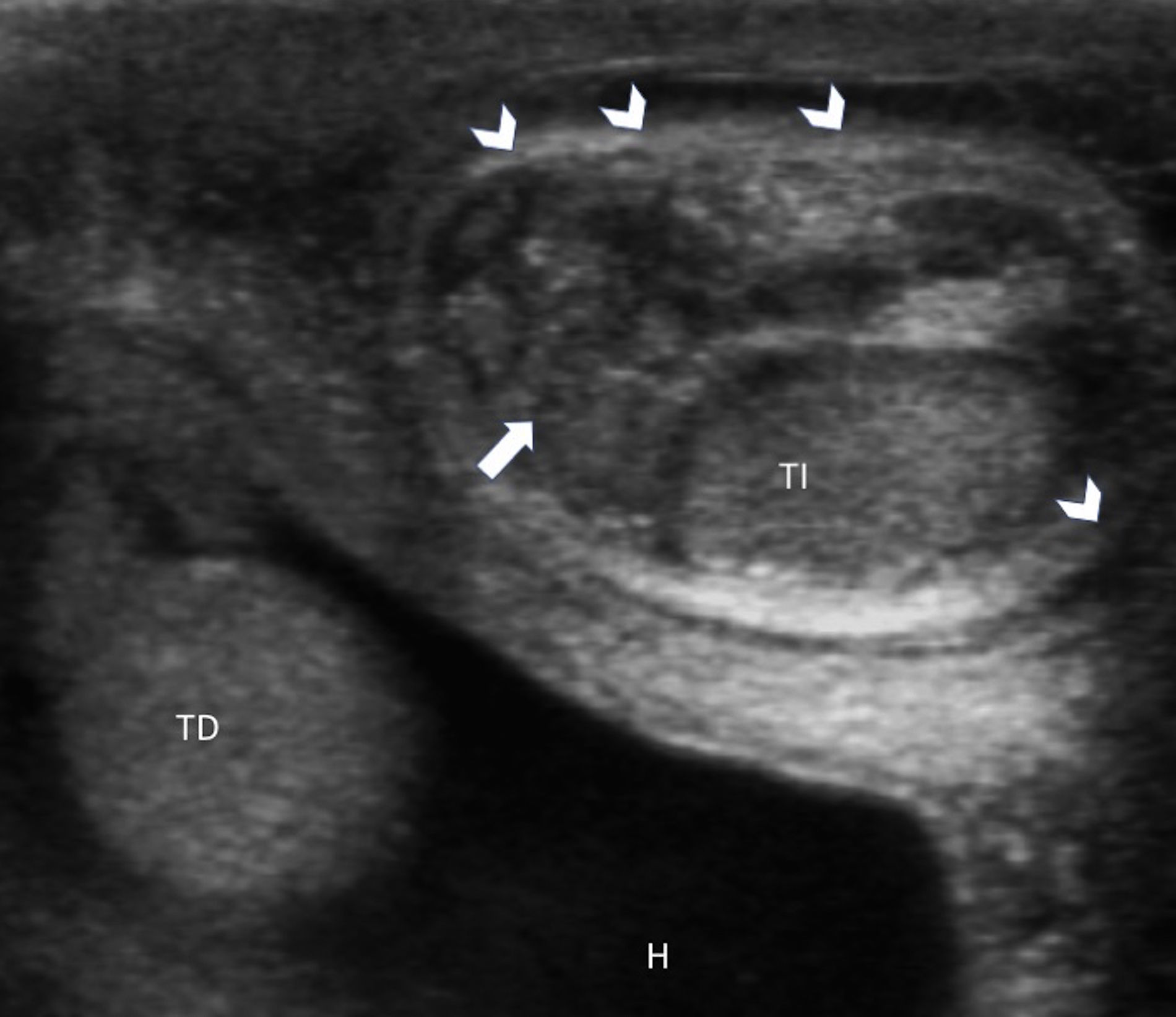
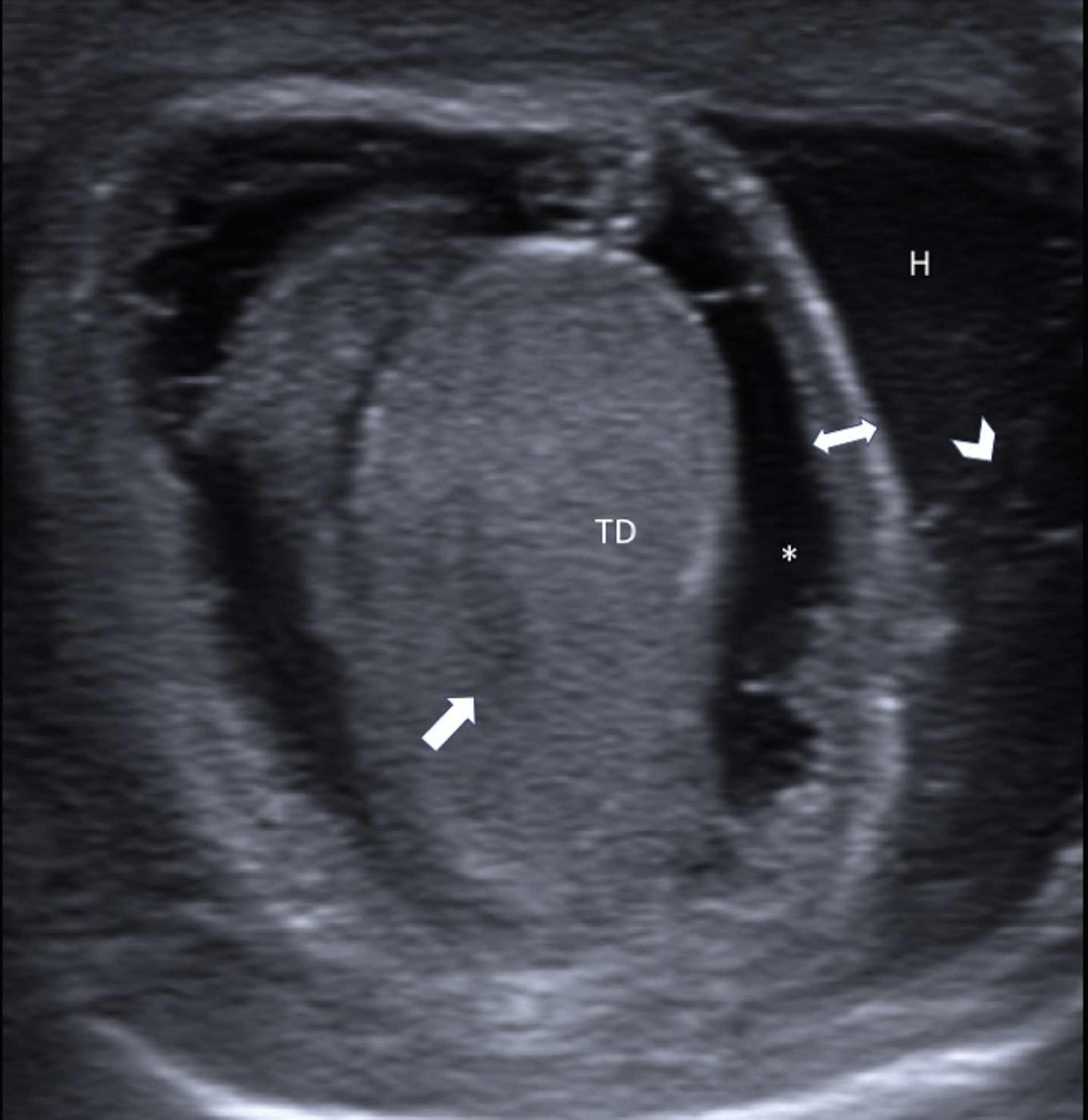
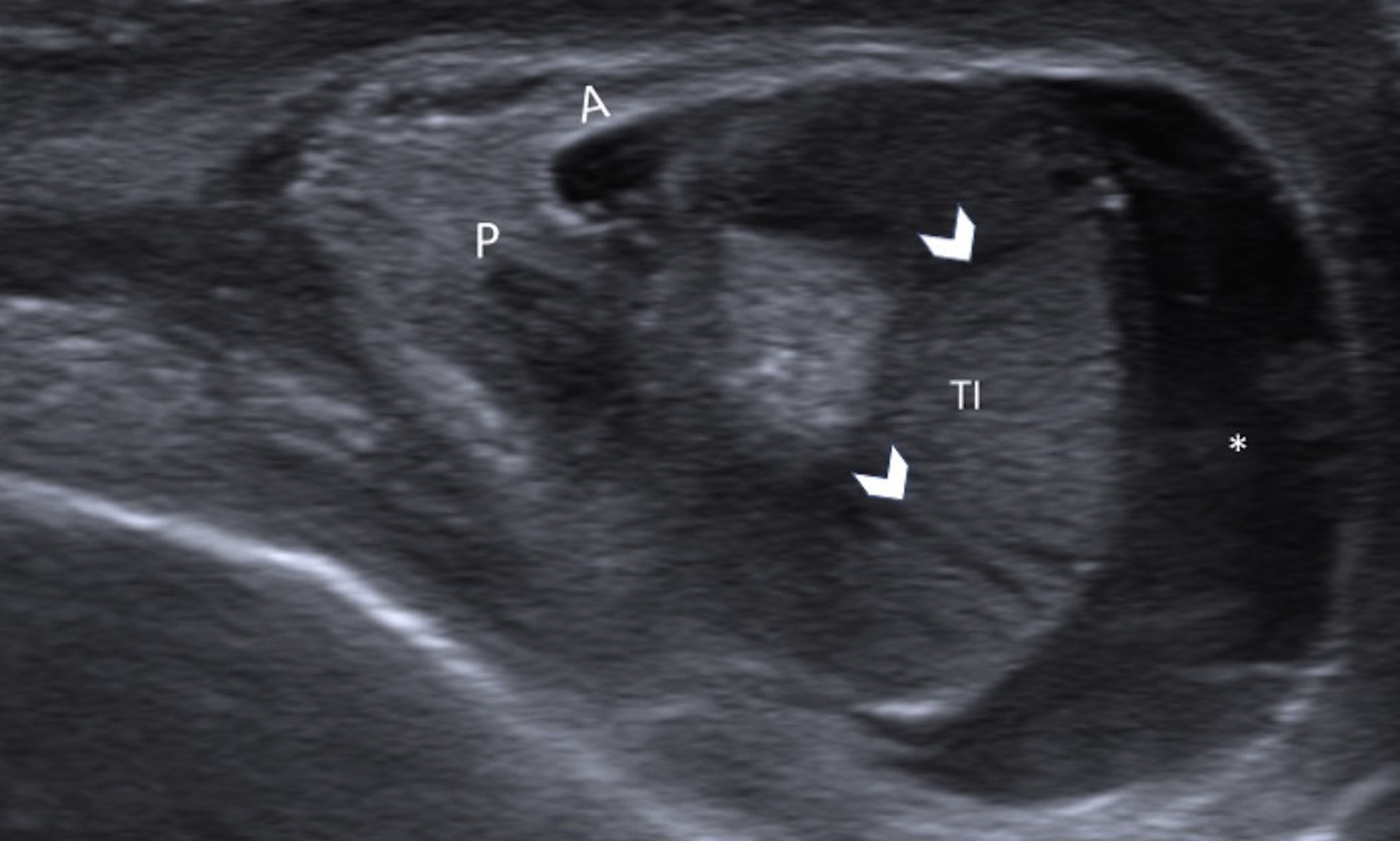
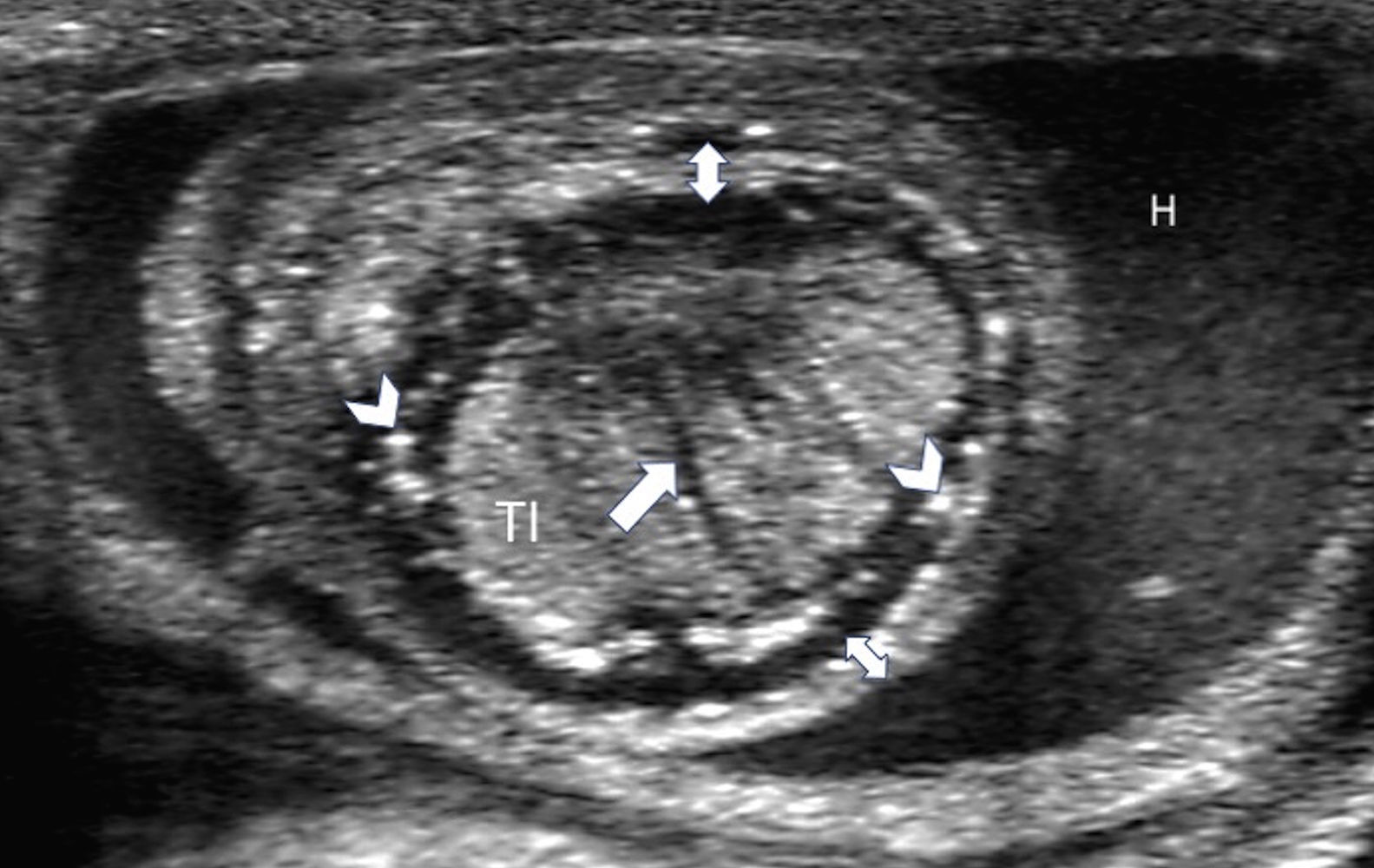
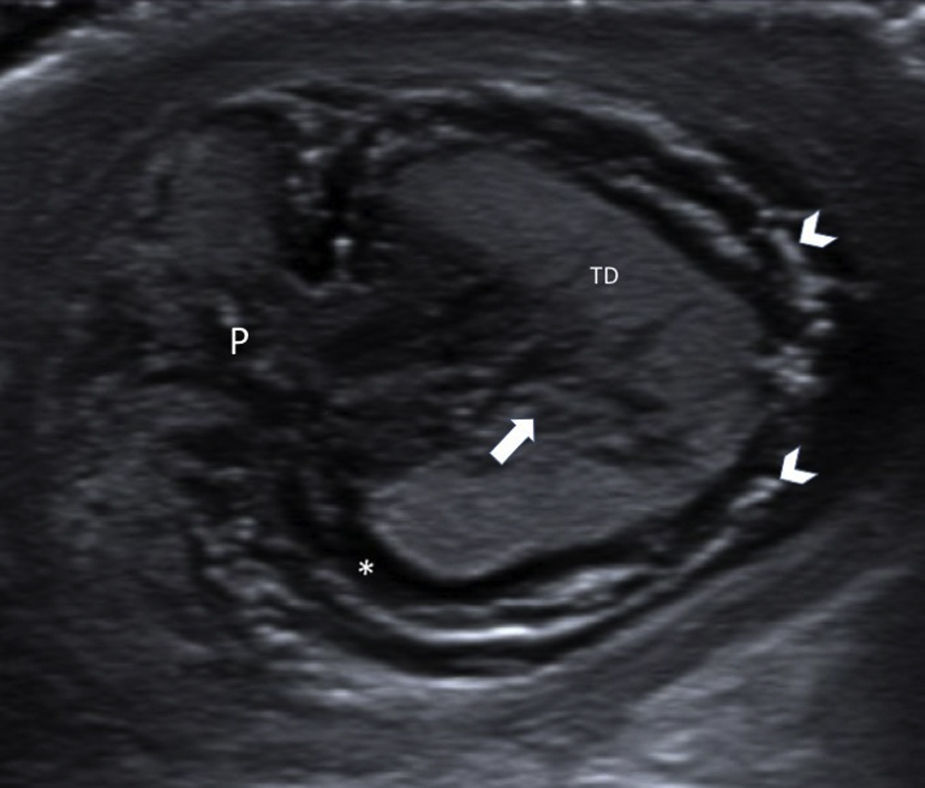
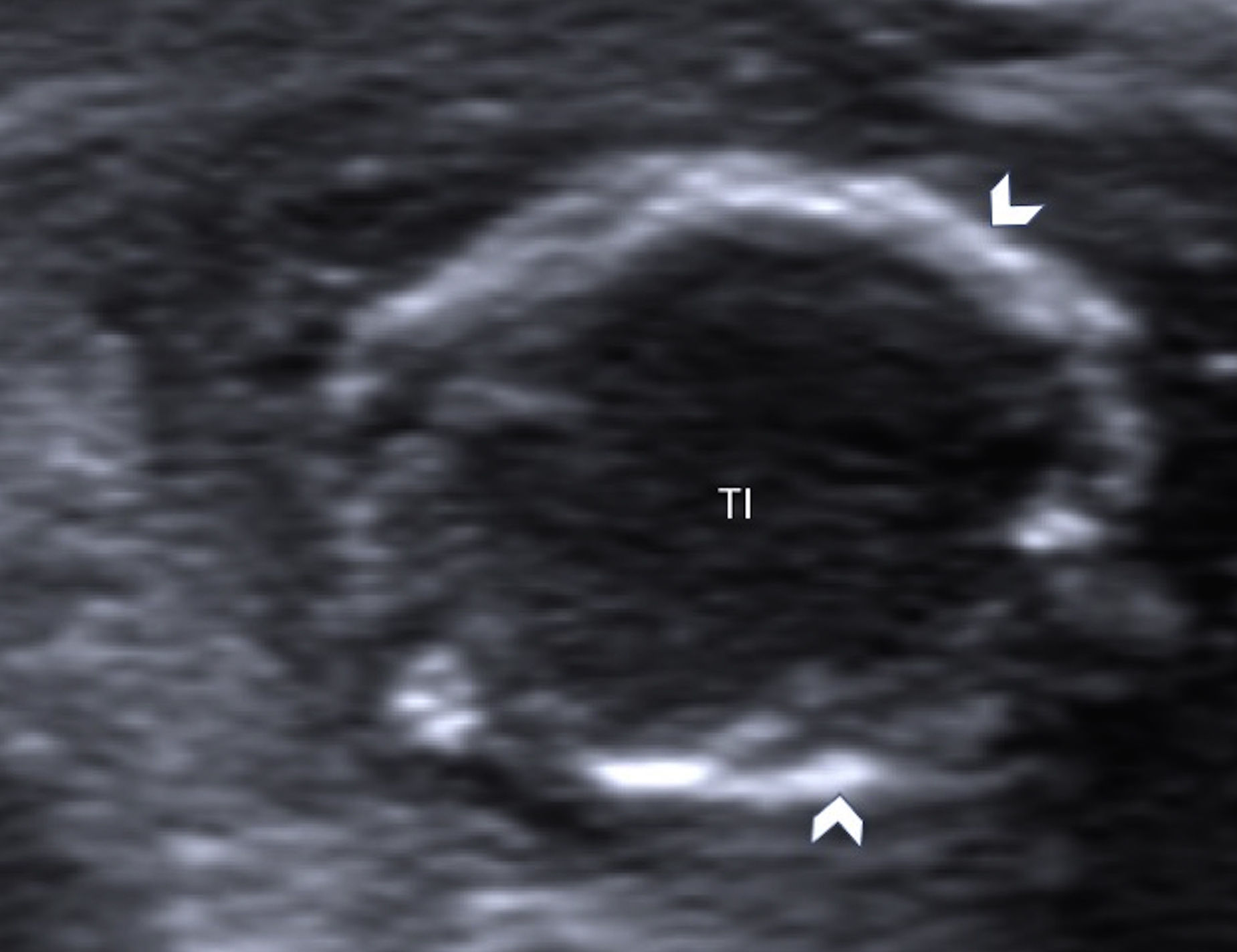
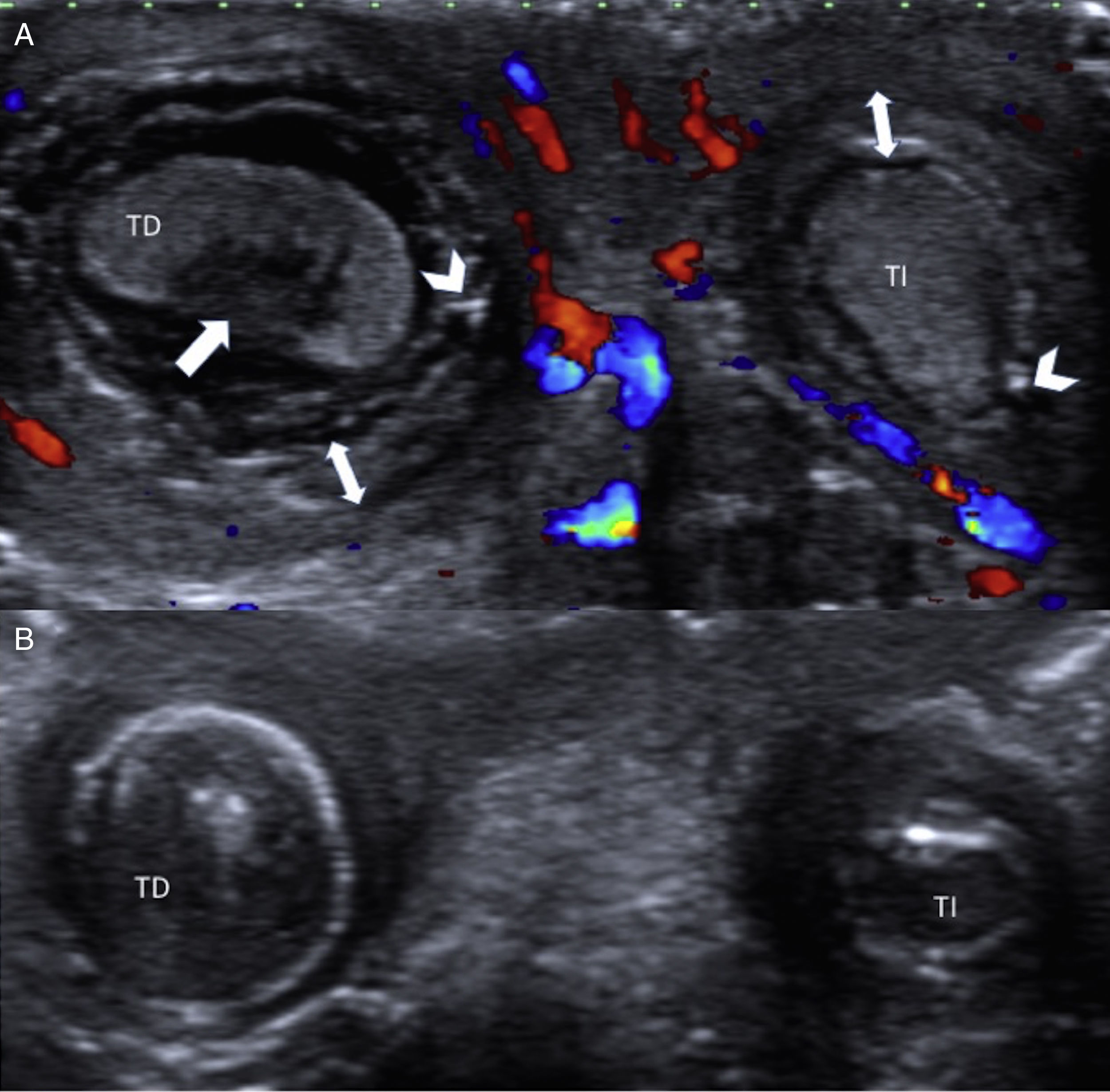
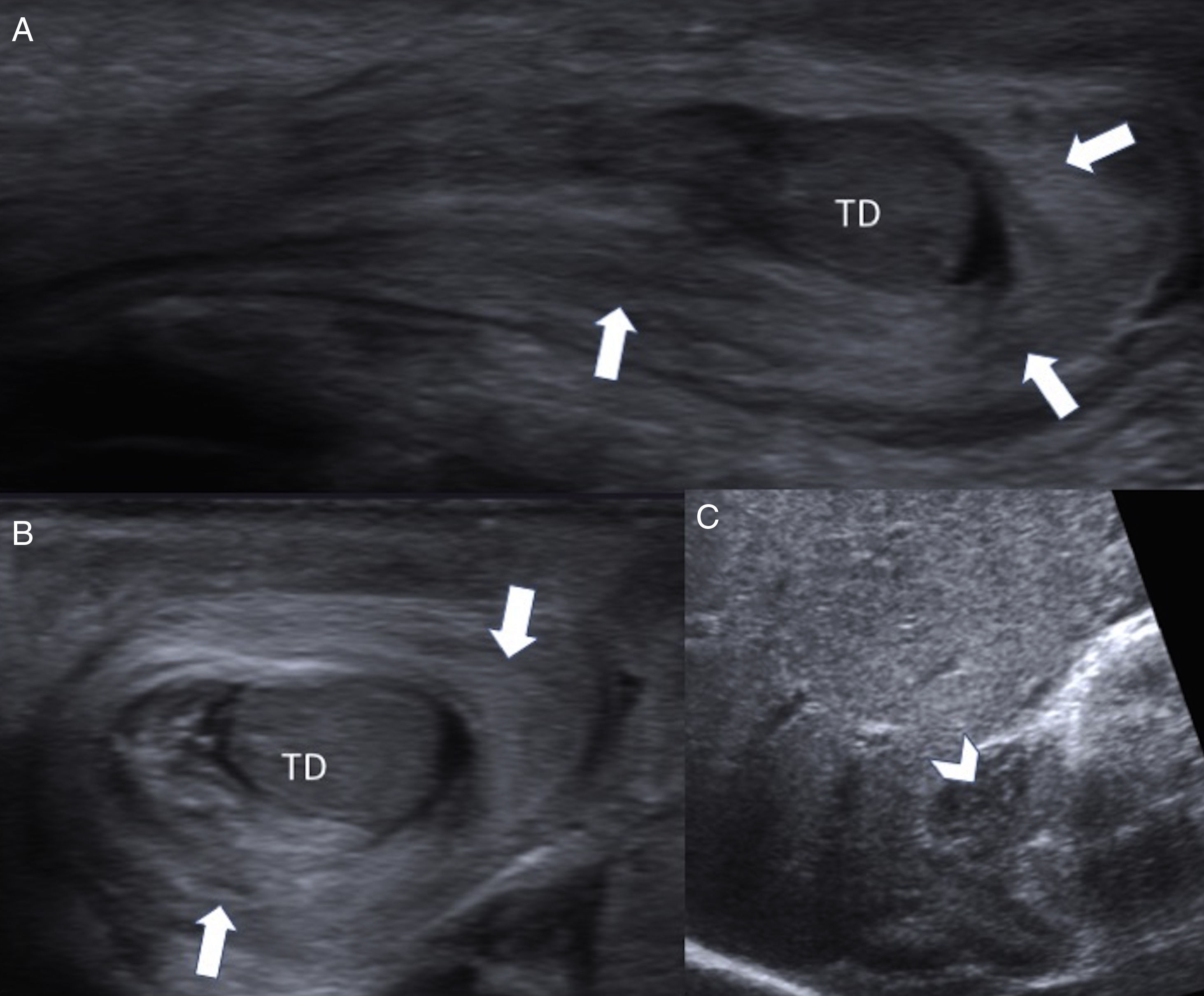
In the acute phase the ultrasound shows enlarged testis and epididymis, surrounded by hematocele arranged in two concentric compartments (‘double ring hemorrhage’ image). The external ring is slightly echogenic and shows an enlarged and edematous tunica albuginea (Figs. 2 and 3). The testis shows lobular edema and hemorrhagic extravasation secondary to venous occlusion (Fig. 4). This is followed by hypoxic-ischemic damage with a progressively heterogeneous testis with hypoechoic central area and hypoechoic peripheral ring (Fig. 5). These areas histologically correspond to infarction and necrosis. PTTs give rise to hemorrhagic infarctions causing alterations in the echostructure of the testis that is more evident than in intravaginal torsions of the teenager where the parenchima remains more homogeneous. The presence of hydrocele may be an early sign of testicular torsion due to an alteration of the vascularization or due to the inflammation.9–12
Five-day-old newborn infant showing one palpable left scrotal mass. The scrotal linear ultrasound probe shows a normal echogenicity-right testis (TD) surrounded by the hydrocele (H). The left testis (TI) seems to be wrapped by an external echogenic ring (arrowhead) with presence of hematocele (arrow). Findings of left neonatal testicular torsion.
Six-day-old newborn infant showing referred to due to an oversized righ scrotal sac of hard consistency and purple color of 24-hour duration. The linear ultrasound probe shows right testis (TD) with an impaired echostructure (arrow), external ring (double arrow) and subalbugineous fluid (asterisk). In the outside we can see hydrocele (H) with septa inside (arrowhead). Findings of left neonatal testicular torsion.
A few-hours-old newborn infant with an oversized left scrotal sac. The linear ultrasound probe shows volume increase of left testis (TI) with lubular edema (arrowheads) and sub-albugineous fluid (asterisk). Visible thickening of vascular pedicle (P) and tunica albuginea (A). Findings of perinatal testicular torsion.
A few-hours-old newborn infant with palpable mass in left scrotal sac. The linear ultrasound probe shows left testis (TI) with lobular edema and linear striations in the testicular parenchyma (arrow). We can see peripheral hyperechogenic foci (arrowheads) and external echogenic ring (double arrow) showing a thickened tunica albuginea. Complex hydrocele (H). Findings of testicular torsion of prenatal onset.
Little by little the testicle grows smaller in size while a peripheral echogenic ring shows up that on the histological level corresponds with calcifications of the transitional zone between the testis and the tunica albuginea (Fig. 6). As the torsion becomes chronic the testis becomes atrophied and the calcifications are more prominent12 (Fig. 7).
One-day-old newborn infant with right scrotal edema. The linear ultrasound probe shows volume increase of right testicle (TD) with significant pedicle (P) thickening and heterogeneity of parenchyma (arrow). Minimal sub-albugineous fluid (asterisk) and calcifications (arrowheads) in the transitional zone between the testis and the tunica albuginea. Findings of prenatal testicular torsion.
Same patient from Fig. 5 after six weeks. The linear ultrasound probe shows atrophic, hypoechoic left testis (TI) surrounded by a thick echogenic layer compatible with dystrophic calcifications.
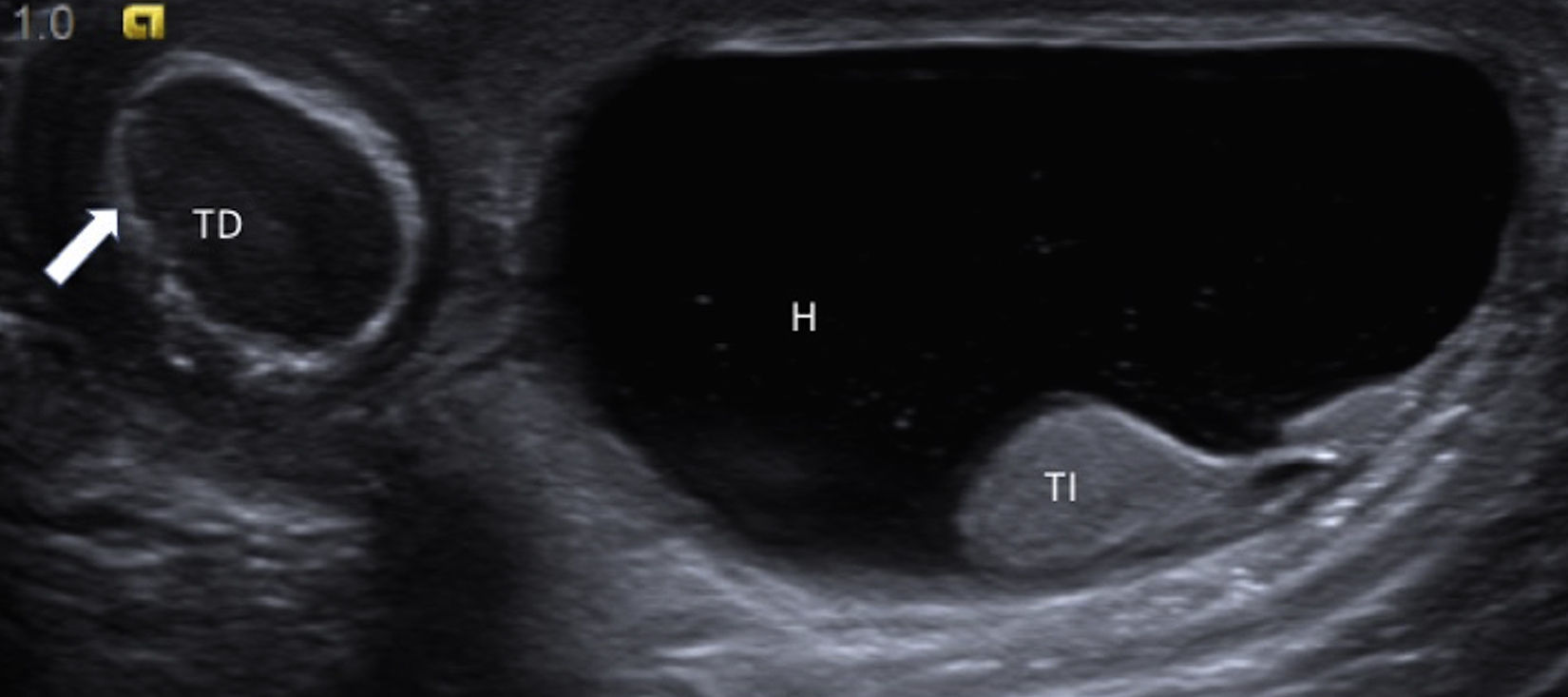
The healthy scrotal sac shows one homogeneous testicle with the tunica albuginea attached to it and often presence of hydrocele secondary to inflammatory changes due to contralateral torsion or due to a congenital defect of the peritoneo-vaginal duct closure also associated with the PTT (Fig. 8).
One and a half-month-old newborn infant with oversized left scrotal sac. The scrotal linear ultrasound probe shows a very hypoechoic right testis (TD) with hyperechogenic external ring secondary to chronic torsion (arrow) of possible prenatal onset misdiagnosed at birth. Left scrotal sac with hydrocele (H) surrounding the left testicle (TI).
The Doppler shows absence of vascular flow in all stages always with flow in the normal contralateral testis that can be extremely difficult in newborn babies if we do not make an adequate technical adjustment of the equipment.9 Even though the sensitivity of the absence of flow for the diagnosis of testicular torsion is high, its specificity is unknown in newborn babies.9,12
Asynchronic bilateral intrauterine torsions are the reason for the different appearance both clinically and in the ultrasound though both testes are nonviable testes (Fig. 9).
Fourteen-hour-old newborn infant with oversized scrotal volume. (A) The color Doppler ultrasound imaging with panoramic linear probe of the scrotum shows both an impaired echostructure of both tests (TD: right testis; TI: left testis) and an absence of vascularization between them. (B) Control ultrasound after four (4) weeks: peritesticular hyperechogenic ring typical of chronic infarction and bilateral testicular atrophy.
In addition to PTT the increased size of the scrotum in a newborn babie can be due to different causes; the most common are scrotal hematoma, orchiepididymitis, hydrocele, inguinal hernia, tumors, and meconium periorchitis.13,14
The B-mode and color Doppler ultrasound imaging help us in the diagnosis of each and every single one of these causes allowing us to distinguish them from PTT and facilitating therapeutic management.
HematomaThe scrotal hematoma in the newborn infant is rare and usually secondary to adenal hemorrhage and obstetric trauma. The skin can look bluish in appearance and unlike hydrocele translumination is negative. The Doppler ultrasound shows one homogeneous testicle with a preserved vascularization, presence of complicated hydrocele and covers of increased size (Fig. 10). An abdominal ultrasound should always be performed in order to discard any possible adjacent suprarenal hemorrhages. Therapy is conservative with clinical and ultrasound follow-up until recovery.15,16
Term four-day-old newborn infant with a history of dystocic delivery. Increased right hemiscrotum thickness. (A) The ultrasound imaging with linear probe and longitudinal slice shows inguinal-scrotal hematoma (arrows), with normal echostructure of right testis (TD). (B) Transverse slice showing the TD surrounded by one concentric hematoma (arrows). (C) Abdominal CT scan showing one right suprarenal hemorrhage (arrowhead).
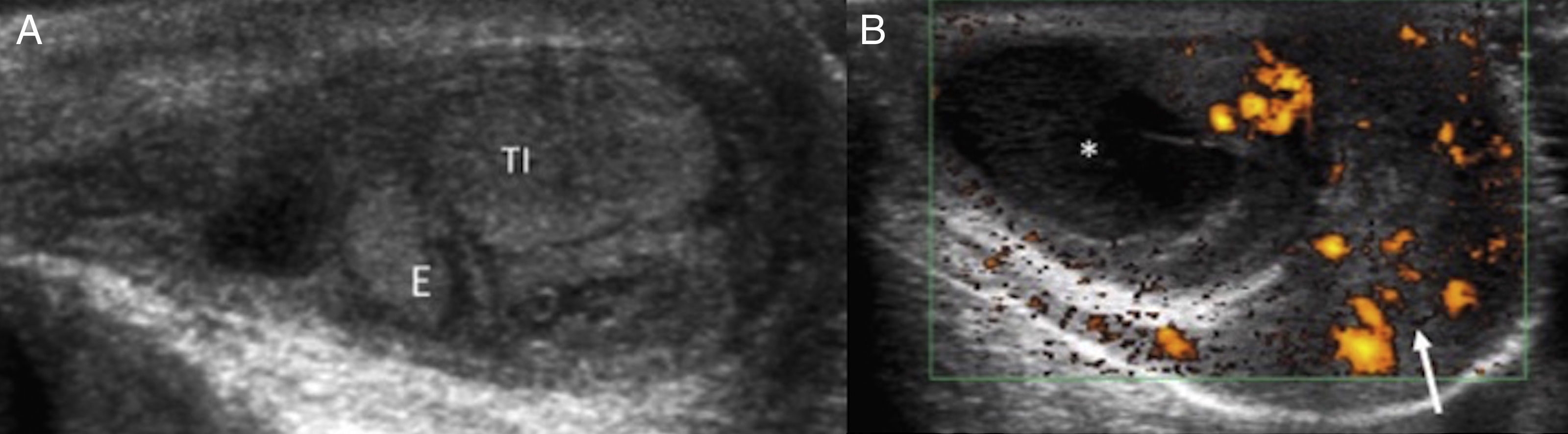
It is rare in the neonatal age. The causes are due to an ascending infection of the urinary tract through the deferent duct or to viral or bacterian hematogene dissemination and the most common responsible organisms are Escherichia coli and Klebsiella pneumoniae. Usually syndromes are fever, discomfort during the medical exam and leucocytosis. The ultrasound shows hyperemia both of the epididymis and the testicle that may have an impaired echostructured (Fig. 11). Therapy is conservative with antibiotics and ultrasound follow-up.17,18
Twelve-day-old newborn infant with septis due to rotavirus. The clinical exploration confirms the presence of left testis (TI) of an increased volume and inflammatory changes. (A) The ultrasound shows oversized TI and epididymis (E). (B) The Doppler ultrasound confirms thickening and hyperemia of covers (arrow) and pyocele (asterisk). Findings of neonatal orchiepididymitis.
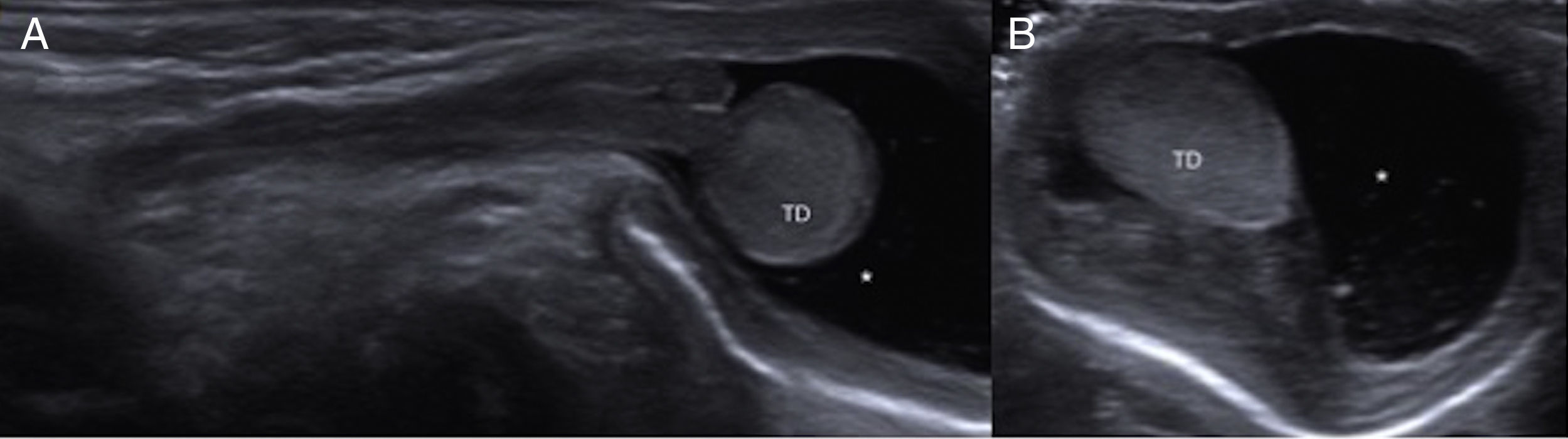
It is the most common cause for a increase in size in the scrotal sac due to an accumulation of liquid in the tunica vaginalis. As a contributor to its formation we find the scrotal skin weakness pressure that has less pressure than the abdominal wall. It can be communicating or not according to how patent the vaginal process is. In addition to the type of hydrocele the ultrasound also shows the characteristics of each hydrocele – whether it is simple or complicated with presence of dispersed echoes inside (Fig. 12). It tends to disappear through reabsorption during the first year of life and only if it persists longer than a year and a half surgery may be considered as an viable option.13
Newborn infant with oversized right hemiscrotum. (A) Ultrasound image (longitudinal section) of inguinal canal showing right testis (TD) with normal echostructure and size and surrounded by fluid (asterisk). (B) Transverse cut showing fluid (asterisk) surrounding the TD. Findings of right communicating hydrocele.
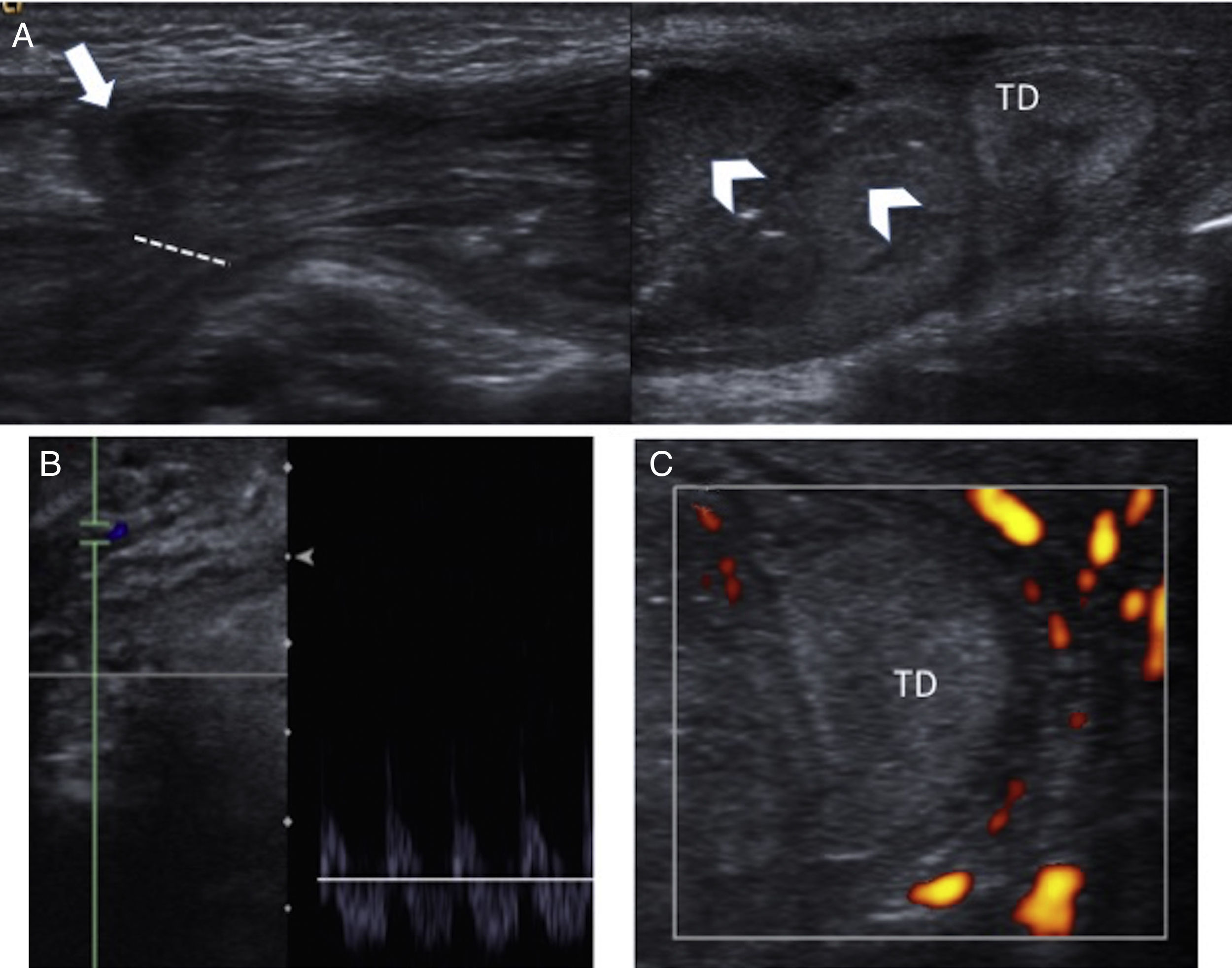
Inguinal hernias are common in newborn babies, especially in premature babies. The intestine, the omentum or both of them penetrate through the vaginal process – something that occurs more frequently on the right side. The ultrasound shows a patent inguinal duct with loops penetrating such duct while contacting, displacing and compressing the testicle. The Doppler assesses both the state of the loops to discard suffering due to incarceration like testicular vascularization that can be affected by loop compression on the cord which in turn can lead to testicular ischemia (Fig. 13). In cases of manual reduction it is useful to confirm whether it was successful or not.19
Premature three-week-old newborn infant with suspicion of incarcerated right inguinal-scrotal hernia. (A) The ultrasound shows presence of hernia (inguinal orifice indicated by the discontinuous line) with sac (arrow) containing intestinal loops of thick walls (arrowhead) with caudal displacement of right testis (TD). (B) The pulsed Doppler ultrasound of the herniated bowel loop vessels shows diastolic inversion as a sign of loop distress. (C) TD without vascularization in the power Doppler ultrasound secondary to compression.
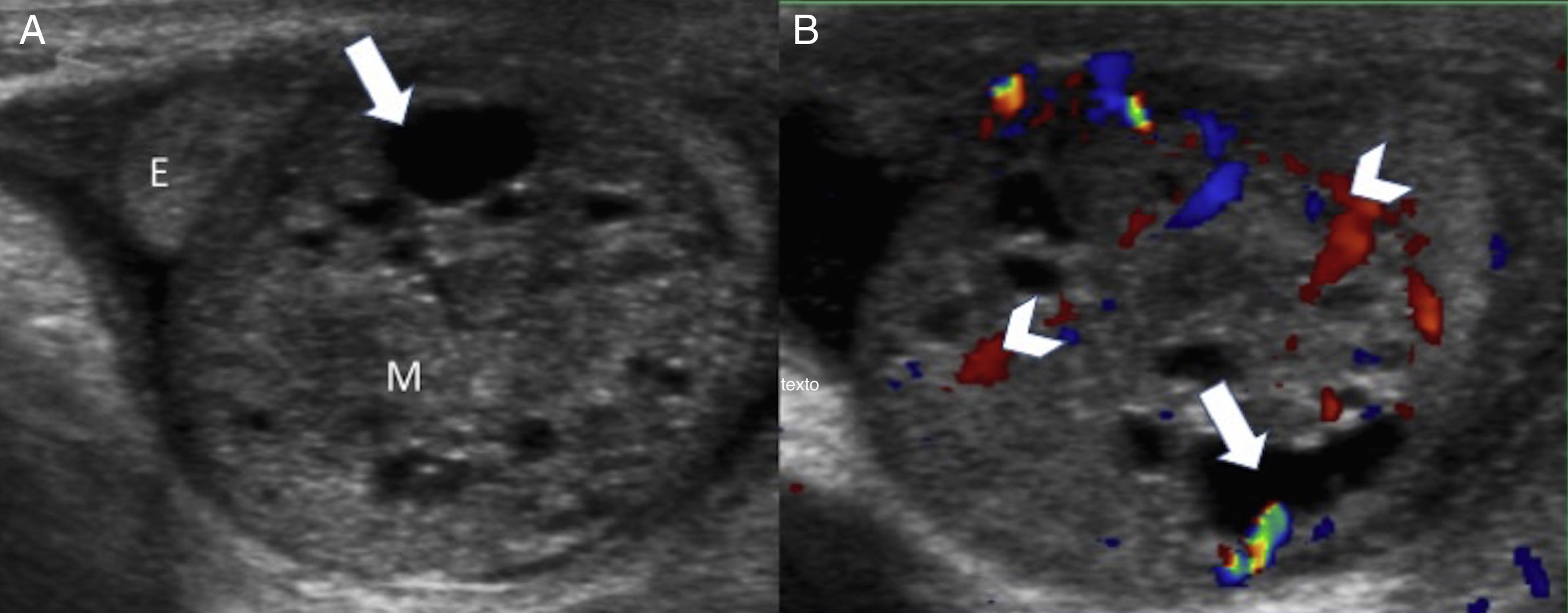
It is extremely rare when they are of neonatal presentation. They look like a scrotal mass. The most common of all occur in babies under 6 months of age and they are juvenile granulosa cell tumors (stromatous) with an ultrasound appearance of multicystic masses. Germinal tumors (endodermal sinus tumors, teratomss) appear in the ultrasound as heterogeneous intratesticular masses with solid and cystic areas and presence of vessels inside (Fig. 14). Surgical management is required with or without adjuvant therapy based on the definitive hystology.20–22
Newborn infant with oversized right testis hard on palpation. (A) The linear ultrasound probe confirms the presence of one heterogeneous testicular mass (M) with cystic zones inside (arrow). The epididymis (E) above the mass can be seen. (B) The color Doppler ultrasound confirms presence of one vascularized testicular tumor (arrowhead). After intervention, the ultrasound suspicion of congenital right testicular teratoma is confirmed.
The infant needs to have suffered fetal meconium peritonitis with meconium passage to the scrotal sac through the patent vaginal duct. The scrotal sac is enlarged and hard. The ultrasound shows a well-established scrotal mass wrapped around the testis and the epididymis with echogenic foci due to calcification. The testis shows normal ultrasound and Doppler characteristics. The correspondence between the clinical history and the ultrasound findings establishes the diagnosis and avoids exploratory surgery.23,24
TherapyThe management of PTT is controversial. According to most pediatric urologists, the clinical separation between prenatal and neonatal torsion is essential. Taken prenatal and neonatal torsions together, the percentage of salvageble testicles is low (3–6%).25 However if we take them separately the percentage goes from 0 per cent in prenatal torsions to 6.3 per cent in neonatal torsions,3 and up to 21 per cent if treated as a surgical emergency.
There is general consensus that bilateral torsion requires immediate surgical review in an attempt to avoid anorchia.
Certain authors suggest the need to distort the testes and perform a biopsy due to the lack of concordance between the testes macroscopic appearance and the testes potential viability due to the resistance of endocrine cells (Leydig cells) to ischemia.
Also in cases of neonatal unilateral torsion the consensus on the need for an immediate surgery is almost unanimous.10
We should remember that: the neonatal unilateral torsion requires urgent surgical review – the same as bilateral torsion. However in the prenatal testicular torsion, the indication of contralateral orchidopexy and the moment of surgery are controversial issues since any surgical interventions can be iatrogenic.1
There are two different viewpoints when it comes to management and both are based on the probability of occurrence of synchronic or asynchronic contralateral torsion. The fact that a few cases of contralateral torsion have been reported between 8 hours and 6 months after the onset of the first one validates the medical opinion of performing an early contralateral orchidopexy.26,27 Other justify the performance of orchidopexies by showing that the torsion may give rise to the development of cytokines with damage to the contralateral germinal epithelium.10 Detractors of this early exploration refer to the low percentage of testicles that are ultimately saved and the surgical risk involved.10,26,27
In this sense we can conclude that since asynchronic torsions are exceptional the right thing to do would be to wait and see and act only at the slightest sign of clinical suspicion.7
On the histological level, prenatal torsion has the appearance of a non-functioning testicular remnant or a fibrous lump without any visible testicular tissues; it is the so called «vanished testis».
Regardless of the moment chosen, this remnant should be surgically resected to prevent infection and any risks of malignancy reported in up to 10 per cent of all cases.28,29
There is general consensus that the surgical approach should be scrotal since it is technically easier, the risk is lower and the contralateral orchidopexy can be performed better.
Up to 60 per cent of all PTTs show hydrocele in the sac that is contralateral to the twisted testis.30 Treating it is also subject to discussion. The hydrocele compression on the testicle could produce ischemia so it seems reasonable to act.30
ConclusionsThe PTT is not very common and amounts to just 10 per cent of all testicular torsions in the pediatric age. The color Doppler ultrasound and the power Doppler imaging are the modalities of choice used for study. The ultrasound characteristics of the PTT are correlated with the longer or shorter time of progression of the PTT. Knowing these characteristics is another cause for an increased size of the neonatal scrotal sac with the corresponding therapeutical implications.
Ethical responsibilitiesProtection of people and animalsThe authors declare that no experiments with human beings or animals have been performed while conducting this investigation.
Confidentiality of dataThe authors confirm that in this article there are no data from patients.
Right to privacy and informed consentThe authors confirm that in this article there are no data from patients.
Authors- 1.
Manager of the integrity of the study: CSN, RLLS
- 2.
Study Idea: CSN, RLLS
- 3.
Study Design: CSN, RLLS
- 4.
Data Mining: N/A.
- 5.
Data Analysis and Interpretation: N/A.
- 6.
Statistical Analysis: N/A.
- 7.
Reference: CSN, RLLS
- 8.
Writing: CSN, RLLS
- 9.
Critical review of the manuscript with intellectually relevant remarks: CSN, RLLS
- 10.
Approval of final version: CSN, RLLS, SPA, EGI
The authors declare no conflict of interests associated with this article whatsoever.
Please cite this article as: Sangüesa Nebot C, Llorens Salvador R, Picó Aliaga S, Garcés Iñigo E. Torsión testicular perinatal. Valoración ecográfica y diagnóstico diferencial. Radiología. 2017;59:391–400.