To evaluate the association of posterior tibial tendon dysfunction and lesions of diverse ankle structures diagnosed at MRI with radiologic signs of flat foot.
Materials and methodsWe retrospectively compared 29 patients that had posterior tibial tendon dysfunction (all 29 studied with MRI and 21 also studied with weight-bearing plain-film X-rays) with a control group of 28 patients randomly selected from among all patients who underwent MRI and weight-bearing plain-film X-rays for other ankle problems.
In the MRI studies, we analyzed whether a calcaneal spur, talar beak, plantar fasciitis, calcaneal bone edema, Achilles’ tendinopathy, spring ligament injury, tarsal sinus disease, and tarsal coalition were present. In the weight-bearing plain-film X-rays, we analyzed the angle of Costa-Bertani and radiologic signs of flat foot. To analyze the differences between groups, we used Fisher's exact test for the MRI findings and for the presence of flat foot and analysis of variance for the angle of Costa-Bertani.
ResultsCalcaneal spurs, talar beaks, tarsal sinus disease, and spring ligament injury were significantly more common in the group with posterior tibial tendon dysfunction (p<0.05). Radiologic signs of flat foot and anomalous values for the angle of Costa-Bertani were also significantly more common in the group with posterior tibial tendon dysfunction (p<0.001).
ConclusionWe corroborate the association between posterior tibial tendon dysfunction and lesions to the structures analyzed and radiologic signs of flat foot. Knowledge of this association can be useful in reaching an accurate diagnosis.
Valorar la asociación entre Disfunción del Tendón Tibial Posterior (DTTP) y lesiones de diversas estructuras del tobillo diagnosticadas por RM, y los signos radiológicos de Pie Plano.
Material y métodoRealizamos un estudio retrospectivo comparando 29 pacientes con DTTP, todos examinados por RM y 21 de ellos con estudio radiológico en carga, con un grupo control de 28 pacientes elegidos aleatoriamente entre aquellos estudiados por otras patologías del tobillo mediante RM y estudio radiológico en carga.
En los estudios de RM revisamos la existencia de espolón calcáneo, pico talar, fascitis plantar, edema óseo calcáneo, tendinopatía del Aquiles, lesión del ligamento Spring, patología del seno del tarso y coalición tarsiana. En los estudios radiológicos en carga se valoraron el ángulo de Costa-Bertani y signos radiológicos de Pie Plano.
Analizamos las diferencias entre grupos en los hallazgos en RM y presencia de Pie Plano mediante el test exacto de Fisher y del ángulo de Costa-Bertani mediante el análisis de la varianza.
ResultadosLa presencia de espolón calcáneo, pico talar, patología del seno del tarso y del ligamento Spring fue más frecuente en el grupo con DTTP, de forma estadísticamente significativa (p<0,05). También existieron diferencias significativas en la presencia de Pie Plano radiológico y valores anómalos en el ángulo de Costa-Bertani, más frecuentes (p<0,001) en el grupo con DTTP.
ConclusiónCorroboramos la asociación entre lesión de estas estructuras diagnosticada por RM y los signos de Pie Plano radiológico con DTTP. El conocimiento de esta asociación puede ser de utilidad para establecer un diagnóstico preciso.
Posterior tibial tendon dysfunction (PTTD) is the painful process of progressive deformation and flattening of the adult foot. It is also referred to as posterior tibial tendon insufficiency (PTTI); or acquired adult flat foot (AAFF). The latter might be the most correct terminology since it allows a broader spectrum of causes and risk factors.
PTTD is a progressive complex process studied since the late 1960s,1 but it was not until the 1980s that the first in-depth descriptions of this pathology were published.2–4 In 1989 Johnson and Strom published the world's first fundamental categorization of PTTD.5
From the beginning its etiology was believed to be secondary to the injury of the PTT in turn associated to the progressive final development of AAFF. At the time it was thought that a failure of the PTT caused the excessive overloading of other ligament and articular structures leading to the flattening of the longitudinal plantar arch.
Unlike architectonic arches the medial longitudinal plantar arch does not have a “key stone” proving it with stability. Such instability can be seen in the astragalo-scaphoid joint and in the anterior sub-astragaloid joint where the astragalus behaves like a “meniscus bone” (the only bone of the lower limb not receiving muscle-tendon insertions) transmitting gravitational forces through the tragalo-scaphoid joint and the anterior sub-astragaloid joint toward the calceneal tuberosity and the base of metatarsals.
These joints make up the bone section of a complex called “acetabulum pedis” or “coxa pedis”6 responsible for keeping the stability of the plantar arch through dynamic and static elements.
Pisani introduced the idea of peritalar instability defined as the individual defect or most commonly the combined defects of at least one of the stabilizing mechanisms like for instance the loss of intrinsic joint structural stability; the loss of active stability due to mydiotendinous affection of PTT; or passive stability due to ligament failure–particularly the spring ligament.6 Any of these mechanisms would eventually affect sooner or later the remaining components leading to a condition called “degenerative glenopathy”.
Today it is generally accepted that these other ankle structures–particularly the spring ligament and the ligaments of the tarsal sinus play a more important role in this complex process than it was originally thought in such a way that the PTTD can be both the cause and the consequence of damage in these structures–particularly in the spring ligament.7
We should probably be thinking of AAFF and PTTD as more inter-related entities rather than a sole pathological entity. As a matter of fact many of the patients presenting with symptoms at the PTT already had a flat foot before or they only have pain in one of their feet with bilateral flat foot.8 There are also cases of development of AAFF that present without damage to the PTT.9 Recently Tryfonidis et al. published a series of 9 patients with AAFF with isolated rupture of the spring ligament as the only pathological finding.10 Scientific literature usually considers PTTD as the most probable cause of AAFF even though it requires other stabilizing structures of the medial longitudinal plantar arch to be damaged as well.
Lab studies with cadavers show that the rupture of the PTT is not enough to develop a plano-valgus foot (PVF).11,12 This is why some authors claim it also requires the excision of the plantar fascia, and the involvement of the short and long plantar ligaments and the ligament complex made up of the anterior superficial components of the deltoid ligament complex and the spring ligament (from now own we will refer to this complex as the spring ligament only).11 However in a recent study on cadavers they confirmed that the isolated section of the spring ligament causes rearfoot instability that the PTT simply cannot compensate. The injury causes significant variations in the rotations of scaphoid, astragalus and calcaneus bones13 which speaks of the paramount importance of this structure.
Several traumatologists believe than in most cases the flattening of the medial longitudinal plantar arch comes before the damage at the PTT level8,14; this is why paying attention to tendon affectation only is not very useful as long as the deformity of these other structures is not reversed to reinstate the natural biomechanics of the foot.
With this scientific scenario in mind we have done a retrospective study of cases and controls in an effort to study the link between the PTTD and damage to other structures of the ankle and the radiological PVF.
Materials and methodsStudy populationWe have retrospectively analyzed the MRI studies of ankles done at our center between January 2008 and February 2009. For our study we chose all patients who came to the hospital due to PTTD and among which damage to the PTT could be confirmed at the MRI. Final sample was made up of the studies of 29 patients.
Twenty-one of these patients underwent foot loading studies with a difference between the radiological loading studies in charge and the MRI below 15 days in all cases.
Among all of the remaining patients studied through ankle MRI and loading radiological study between these dates we excluded those whose consultations were about PTTD and/or who showed PTT damage. The remaining patients without exclusion criterion we aleatorized and a paired sample of 28 individuals could be obtained regarding the group of cases by criteria of age and gender in an effort to avoid bias in these demographic variables.
MRI assessed the existence of the calcaneal spur, talus peaks, plantar fasciitis, calcaneal edema, tendinopathy of the Achilles tendon, spring ligament damage, tarsal sinus affectation and tarsal coalition.
The calcaneal spur was defined as the exophytic bone growth of the calcaneal tuberosity; the talus peaks as the exophytic bone growth or osteophytosis of the dorsal margin of the head of the astragalus in the astragalo-scaphoid joint; plantar fasciitis was defined as the focal (>4mm) or continuous thickening of the central fasciculus of the plantar fascia in its proximal insertion regardless of hypersignal spotted on the T2-weighted sequences (acute plantar fasciitis) or hyposignal in both sequences (chronic or fibrotic fasciitis); the calcaneal edema was defined as a hypersignal on the T2-weighted sequences at the bone marrow of the adjacent calcaneus to the insertion of the plantar fascia; tendinopathy of the Achilles tendon was defined as tendon thickening (>8mm in the anteroposterior plane) with or without alteration of the inter-substance signal, peritendinosis or partial or complete tear of the tendon–the inter-substance longitudinal tear included; spring ligament damage was defined as at least one of the following abnormalities: thickening, irregularity or wave-like contour, alteration of the inter-substance signal or solution of continuity15 including damage to the anterior superficial components of the deltoid ligament; tarsal sinus affectation was defined as the replacement of the fat signal by hypointensity of signal on T1-weighted sequences with hyperintensity or hypointensity of signal on T2-weighted sequences and/or discontinuity or irregularity of cervical and interbone ligaments; tarsal coalition was defined as both bone and fibrous links among any of the tarsal bones.
Lastly damage to the PTT was defined as any of the following clinical manifestations: tendinosis and/or tenosynovitis, partial tear (hypertrophic type 1 or atrophic or typ2) or complete tear (type 3).
Those patients with loading radiological studies available were analyzed to calculate the Costa-Bertani angle and determine the radiological PVF.
The Costa-Bertani angle defines 2 longitudinal arches even though it is the medial longitudinal arch the one that is commonly used – which is the arch used in this study. Such arch is defined by 2 lines that connect the calcaneal tuberosity to the inferior point of the astragalo-scaphoid joint and from this joint to the inferior point of the head of the first metatarsal or medial sesamoid bones. The normal values defined in this medial longitudinal arch range between 120° and 130°.
Due to the retrospective nature of the study and after doing all the examinations according to the routine protocol and always under the supervision of the specialist, without any extraordinary uncommon explorations and under the supervision of the hospital ethical and scientific committee we did not need any informed consents from patients or special permits from the ethical committee for the realization of this study.
Acquisition of dataPatients were studied according to the study protocol of our center in 1.5 T MRI (Signa HD 1.5T MR, GE Medical Systems, Milwaukee, WI, USA) and 3.0T (Signa HD 3.0T MR, GE Medical Systems, Milwaukee, WI, USA).
In all patients we used the following sequences in the axial, sagittal and coronal axes: 1.5T MR, T1 spin echo (400–500/15–25 [TR/TE]; 256×224 matrix; of 14–18cm FOV; 2–3 NEX, 3–4mm thick; 0.4–0.5mm spacing), and T2 fast spin echo with fat saturation (2150–2860/90–110 [TR/TE]; 256×224 matrix; 14–18cm FOV; 4–6 NEX; 3–4mm thick and 0.4–0.5mm spacing); RM 3.0T; T1 spin echo (460–560/18–28 [TR/TE]; 256×224 matrix; de 14–18cm FOV; 2 NEX; 3mm thick and 0.8mm spacing), and T2 fast spin echo with fat saturation (4400–4860/90–100 [TR/TE]; 256×224 matrix; 14–18cm FOV; 3 NEX, 3mm thick and 0.5mm spacing).
Two radiologists (CAJ and RRM) with 9 and 14 years of experience in musculoskeletal radiology, respectively interpreted the MRIs under consensus and the foot loading radiological studies of both groups without knowing the previous diagnosis.
The evaluation of the foot loading radiological studies included the anteroposterior (AP) and lateral projections of both feet as well as the AP frontal projections of both ankles showing the deformity of the foot under maximal load. Both radiologists diagnosed or excluded PVF under consensus after taking into consideration the radiological signs of the AP projection of the foot like the greater angle between the astragalus and the first metatarsal bone, the greater angle of the calcaneum-astragalus divergence or the uncovered joint surface of the head of the astragalus or the medial subluxation of the astragalus; on the lateral projection of foot, signs like the increase of the calcaneum-astragalus angles and between the astragalus and the first metatarsal bone the presence of dorsal subluxation of the scaphoid and plantar flexion of the astragalus with descent of the longitudinal arch; on the AP projection of the ankle the valgus rotation of the rear foot could be determined.
They also measured the Costa-Bertani angle of the pathological feet studied through MRI.
Statistical analysisThe distribution by age and sex was studied in a binary logistic regression analysis in an effort to determine the odds ratio for a 95% interval of confidence for every variable to confirm the absence of significant differences.
The variables defined in the MRI findings were analyzed through the Fisher's exact test for each and every variable as well as the radiological PVF defined under consensus by both radiologists. They did not do a multivariate analysis.
The Costa-Bertain angle was analyzed between both groups using the Analysis Of Variance (ANOVA) by comparison through binary logistic regression analysis.
We used the statistical software SPSS® version 17.0 (SPSS Inc., Chicago, IL, USA) in this analysis.
ResultsAge ranged from 26 to 76 years of age (average=55.72 years) including 19 women (65.52%) and 10 men (34.48%).
In the control group age ranged from 31 to 78 years of age (average=51.69 years) including 18 women (64.28%) and 13 men (35.82%). There were no significant differences in these parameters.
Among the 29 patients of the PTTD group the MRI showed 12 tendinosis with no defined tear, 3 tenosynovitis, 6 hypertrophic partial tears or type I, 2 atrophic partial tears or type II and 4 complete tears.
In the case group we found these frequencies of occurrence: calcaneal spurs (51.72%), damage to the tarsal sinus (44.83%), plantar fasciitis (41.38%), talus peaks (41.38%), damage to the spring ligament (31.03%) and tendinopathy of the Achilles tendon (24.14%).
In the control group we found these frequencies of occurrence: calcaneal spurs (21.43%), damage to the tarsal sinus (10.71%), plantar fasciitis (28.57%), talus peaks (3.57%), damage to the spring ligament (7.14%) and tendinopathy of the Achilles tendon (28.57%).
We only found one case of tarsal coalition in the control group (and none in the case group). This is the reason why this variable was not analyzed. We did not do any statistical analyses of the calcaneal edema due to its low frequency of occurrence (3 cases and 2 controls).
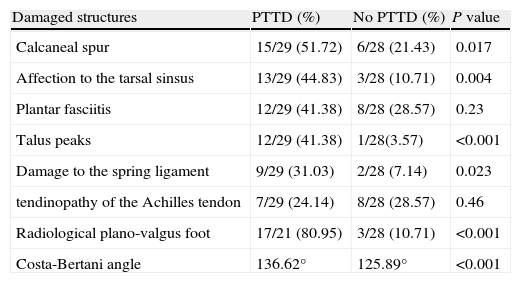
Using the Fisher's exact test for every independent variable and considering one statistical significance for p<0.05 we found significant differences for the calcaneal spur (p=0.017), for the affectation of the tarsal sinus (p=0.004), for the talus peaks (p<0.001) and for the damage to the spring ligament (p=0.023). Neither plantar fasciitis (p=0.23) nor the tendinopathy of the Achilles tendon (p=0.46) were significant (Table 1).
Statistical comparison of damaged structures and plano-valgus foot.
| Damaged structures | PTTD (%) | No PTTD (%) | P value |
| Calcaneal spur | 15/29 (51.72) | 6/28 (21.43) | 0.017 |
| Affection to the tarsal sinsus | 13/29 (44.83) | 3/28 (10.71) | 0.004 |
| Plantar fasciitis | 12/29 (41.38) | 8/28 (28.57) | 0.23 |
| Talus peaks | 12/29 (41.38) | 1/28(3.57) | <0.001 |
| Damage to the spring ligament | 9/29 (31.03) | 2/28 (7.14) | 0.023 |
| tendinopathy of the Achilles tendon | 7/29 (24.14) | 8/28 (28.57) | 0.46 |
| Radiological plano-valgus foot | 17/21 (80.95) | 3/28 (10.71) | <0.001 |
| Costa-Bertani angle | 136.62° | 125.89° | <0.001 |
Radiological PVF was diagnosed in 80.95% (17/21) of cases with foot loading radiological studies and an average Costa-Bertani angle of 136.62 degrees. In the control group the Costa-Bertani angle was 125.89 degrees. Three of the 28 controls had radiological PVF (10.71%).
The analysis through the Fisher's exact test of the radiological PVF was statistically significant (p<0.001). Comparison analysis through the ANOVA with binary regression of the Costa-Bertain angle was also significant (p<0.001) (Table 1).
DiscussionOur results confirm the link between PTTD and radiological PVF and some altered values of the Costa-Bertain angle bearing in mind though that the diagnosis of PVF is eventually clinical.
The PTT is the tendon of the ankle most usually damaged in middle-aged and elderly women16–18 mainly in a spectrum of injuries ranging from peritendonitis to tendinosis, then tio partial focal tear and eventually leading to complete tear17,19,20. The degeneration and tear of the PTT usually occurs in the tarsal tunnel or the perimalleolar region due to the relative hypovascularization of this area21–23 and pressure exerted on the tendon.4,14,24 The second most common location is insertional. The PTT inserts into the scaphoid tuberosity mainly though it shows secondary projections for virtually all tarsal bones except for the astragalus (Fig. 1).
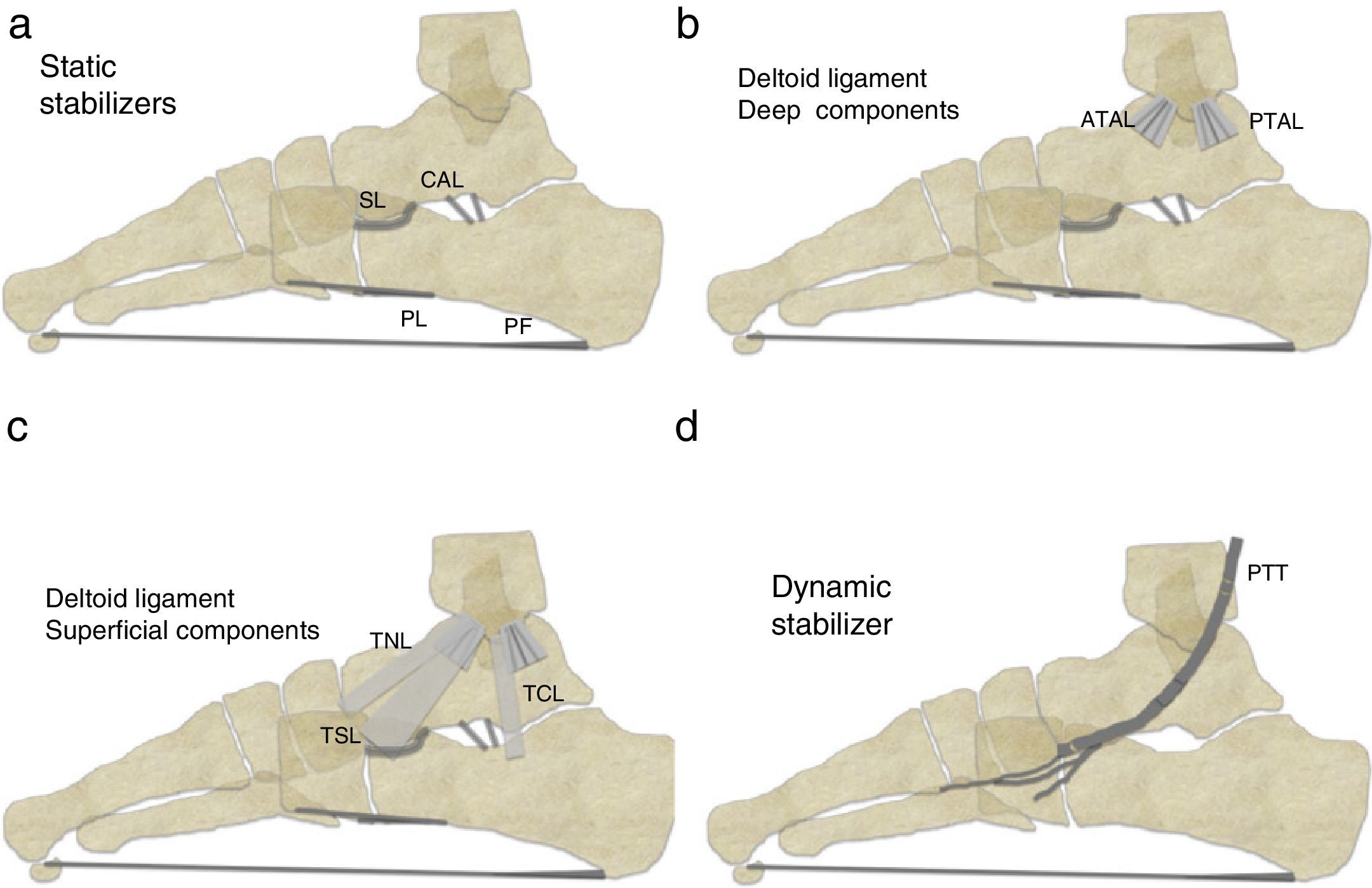
Schematic chart on sagittal plane showing the main stabilizers of the medial longitudinal plantar arch: (a) static stabilizers. PF: plantar fascia; CAL: calcaneal-astragalar ligament (of the tarsal sinus); PL: plantar ligaments (short and long); SL: spring ligament; (b) deep components of the deltoid ligament–ATAL: anterior tibio-astragalar ligament; PTAL: posterior tibio-astragalar ligament; (c) superficial components of the deltoid ligament: TCL: tibio-calcaneal ligament; TNL: tibio-navicular ligament; TSL: tibio-spring ligament, and (d) dynamic stabilizer: PTT: posterior tibial-tendon.
The PTT is the main dynamic stabilizer restricting the abduction of the medial foot through eccentric contraction during the propulsion phase of walking. It flexes and inverts the rear foot giving a stable configuration to the plantar arch while blocking the displacement of the astragalus and calcaneus into the astragalo-scaphoid joints and secondarily into the calcaneal-cuboid joints. It strengthens the action of spring and deltoid ligaments too. The PTT is however inactive during bipedalism.
The fundamental static stabilizers of the plantar longitudinal arch are the plantar fascia, the spring ligament, the anterior superficial components of the deltoid ligament, the short and long longitudinal plantar ligaments and the ligaments of the tarsal sinus (Fig. 1).
During bipedalism the main support of the plantar arch is plantar fascia25 followed by the short and long plantar ligaments and the spring ligament. Also it is the fundamental static stabilizer during the first stance phase while walking. It spreads from the calcaneal tuberosity to the bases of the proximal phalanges of the toes.
However despite the high frequency of occurrence of injuries described both in our outcomes and in Balen's26 and Deland's27 outcomes there is no link statistically significant between damages to the plantar fascia or the Achilles tendon and PTTD.
In our study we found a frequency of occurrence of plantar fasciitis of 41.38% in the case group–very similar to the percentage found in the articles aforementioned (32% and 26%, respectively).
However we have found significant differences in the frequency of occurrence of calcaneal spur in the control group. We know that the calcaneal spur is more prevalent in patients with pain in their heels but it is also proved to be more common in patients with flat feet. Prichasuk et al. showed a high statistical significance in the link between pain in the heel, the calcaneal spur and the flattening of the plantar longitudinal arch.28 Over-weight, advanced age and women are factors associated with this condition as well.28
On the other hand in his study Deland27 did not find significant differences in damages to the short and long plantar ligaments with a rare frequency of injuries. We have not studied this possible relation due to the great variability of ligament images coming from the MRIs and due to its limited repercussions and interest in traumatological literature.
As in prior studies26,27 data from our study seem to indicate that both the spring ligament and the ligaments from the tarsal sinus are key structures associated to the affectation of the PTT.
Surgically Gazdag and Cracchiolo29 showed a great incidence of spring ligament tears (18 cases in 22 patients) in PTT surgical reconstructions in patients with major failures in their tendons.
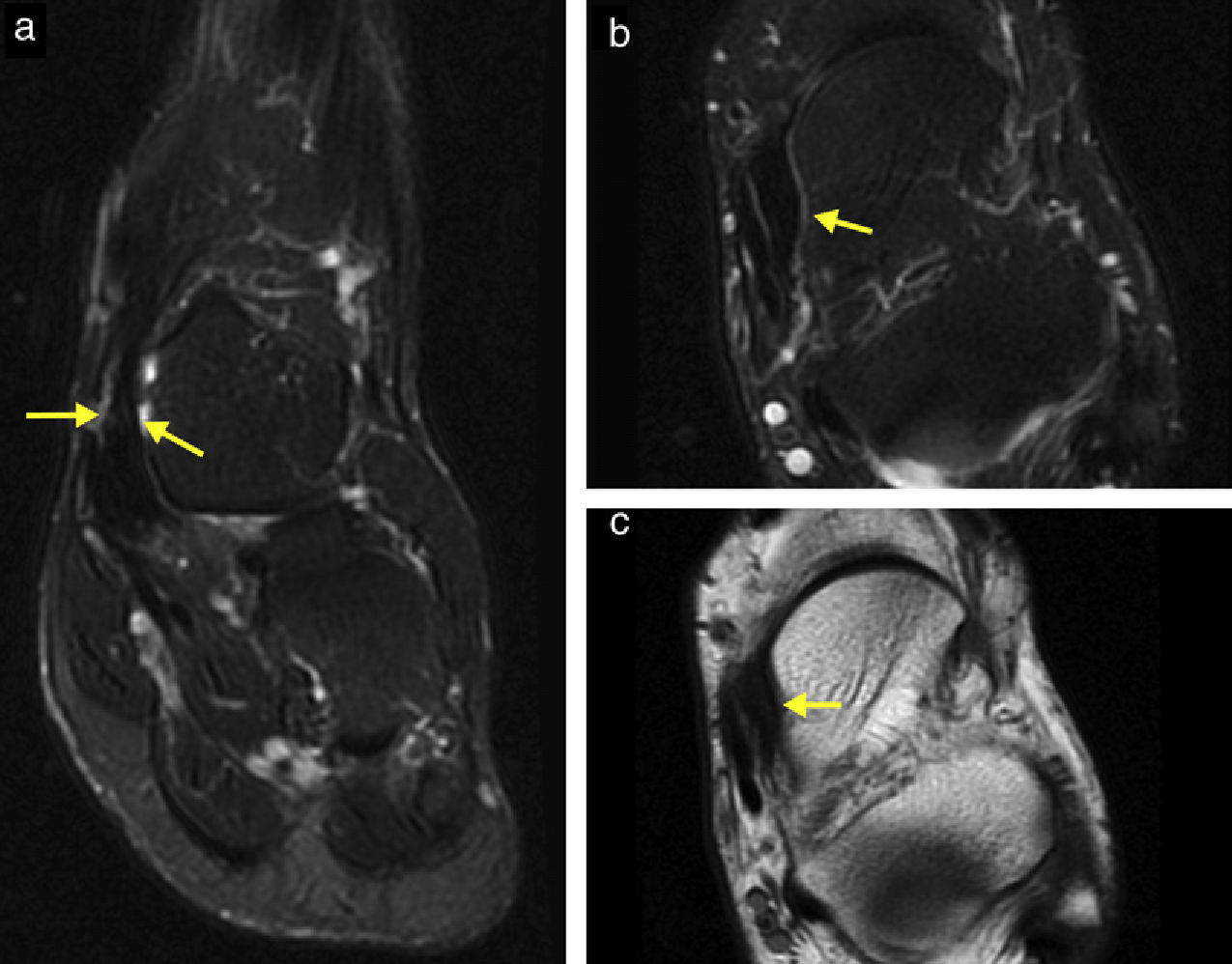
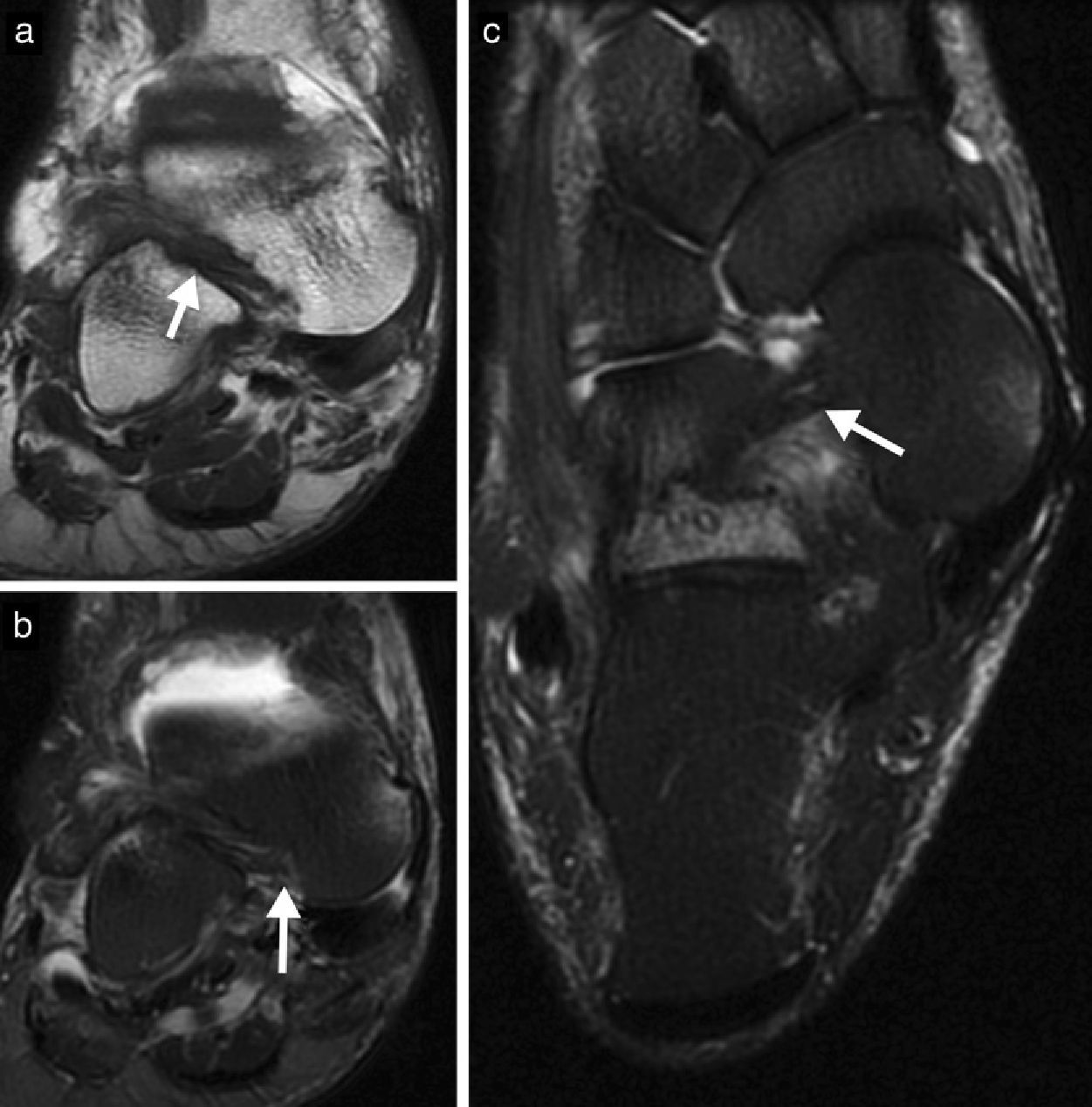
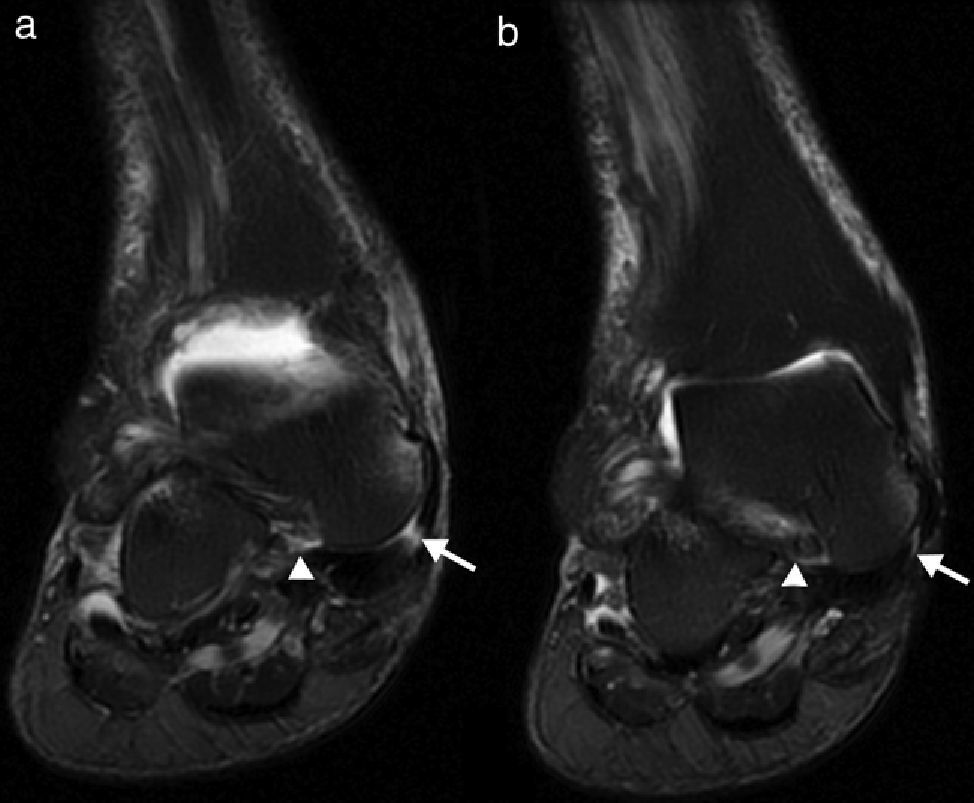
Afterwards MRI studies on PTTD like Balen's26 and Deland's studies27 have been published where the connection between damage to the spring ligament (Fig. 2) and dame to the ligaments of the tarsal sinus has been confirmed (Fig. 3).
Ankle MRIs: (a) coronal fat-supressed T2-weighted sequences, (b) axial fat-supressed T2-weighted sequences and (c) axial T1-weighted sequences. Arrows indicate in (a) the thickening and irregularity of the tibiospring component with inter-substance hypersignal indicative of the sequelae of chronic tear. Arrows in (b and c) show irregular thickening of the supero-medial component of the spring ligament secondary to chronic tear and fibrosis.
Ankle MRIs: (a) coronal T1-weighted sequences, (b) coronal fat-supressed T2-weighted sequences and (c) axial T2-weighted sequences. Arrows indicate in (a and b) the irregularity of the fibers of the calcaneal-astragalar cervical ligament with edema in the tarsal sinus. In (c) arrows identify the horizontalization of the cervical ligament due to distal displacement and medial rotation of the head of the astragalus. The cervical ligament loses its competence with this anomalous angulation of its trajectory. Pay attention to the diffuse edema of the calcaneus on the floor of the tarsal sinus.
In our study the frequency of cases in which we find affectation of the tarsal sinus (41.38%) and the spring ligament (31.03%) (Fig. 4) though statistically significant it is significantly inferior to the frequency described in Balen's study26 (72% and 92% respectively) and Deland's study27 (48 and 87% respectively) and to the frequency found by Gazdag and Cracchiolo29 through surgery of damage to the spring ligament (82%). Such difference could be explained by the variability of case inclusion criteria in our study with serious affectation since Gazdag and Cracchiolo's study29 uses a surgical series with serious affectation while Balen's26 and Deland's studies27 include advanced cases of injury or PTT failure, respectively.
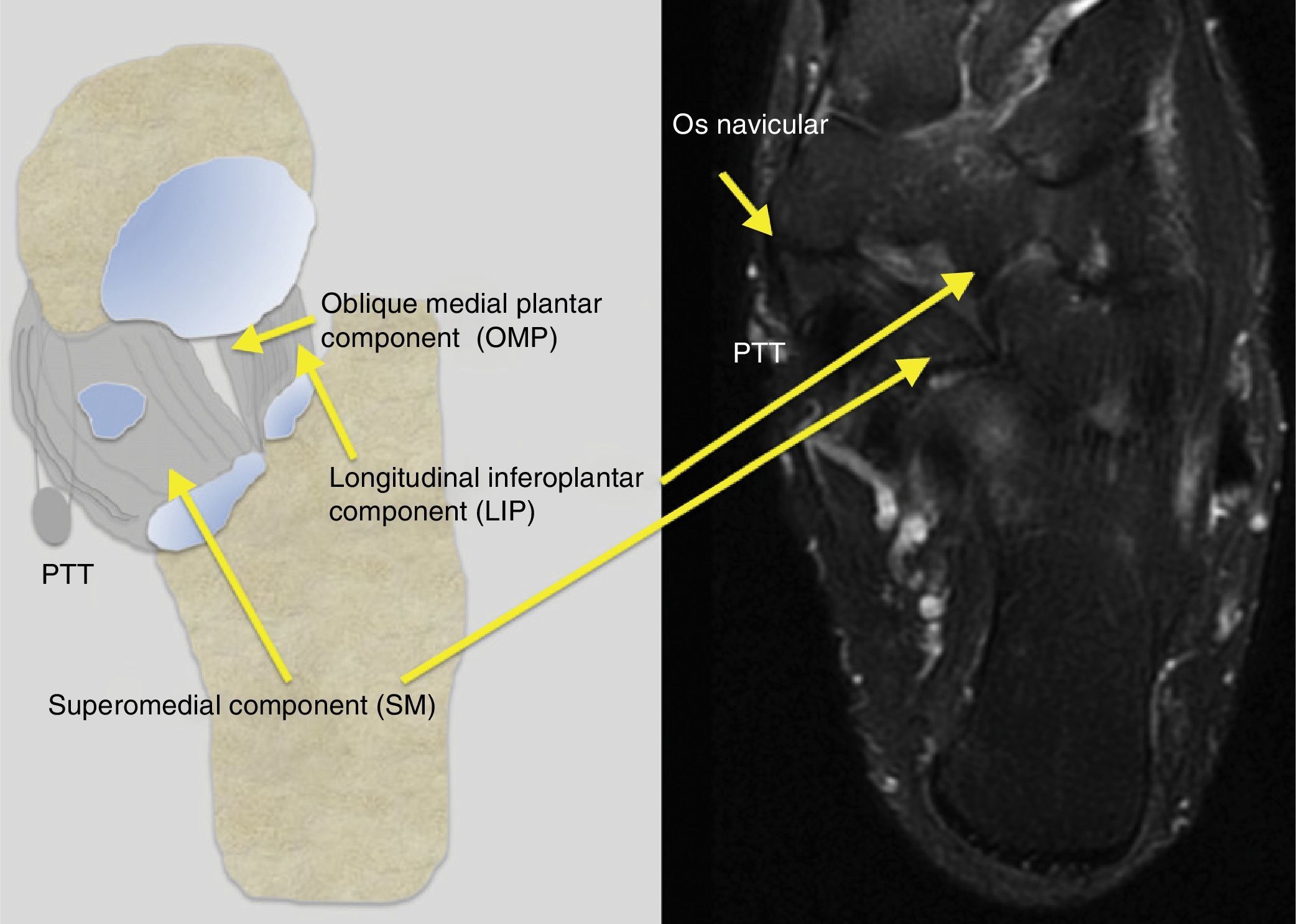
The spring ligament does not have elastic properties. It works as a medial and plantar contention structure of the head of astragalus. It seems to be the greater stabilizing component of the plantar arch during the middle stance phase.13 Despite the indication of its repair is not widely accepted including this structure in the surgical reconstruction of PVF12,13,30 is becoming more and more common. It is made out of two main fasciculi (superomedial ligament and inferoplantar longitudinal ligament)31 and other inconstant accessory fasciculus (oblique medial plantar ligament)32 (Fig. 5). Superomedial fasciculus is immediately located deep to the PTT, stems from the sustentaculum tali, inserts into the superomedial margin of tuberosity of scaphoid and merges to the anterior superficial fibers of deltoid ligament (the so-called tibiospring ligament33 as capsular medial reinforcement). It is the strongest thickest component and most of the times the only recognizable component during surgery–necessarily damaged when there is significant clinical affectation of the spring ligament. It is only this component that contains a fibrocartilaginous reinforcement suggesting it does not support tension forces only but also compression between the PTT and the head of the astragalus.12
On the left side of the schematic chart of the axial plane representing the components of the spring ligament: LIP: Longitudinal inferoplantar; OPML: oblique medial plantar ligament; SM: Superomedial; PTT: Posterior tibial-tendon. To the right axial fat suppressed T2-weighted sequences showing the corresponding components of the spring ligament.
The inferoplantar longitudinal fasciculus originates at the coronoid fossa of the calcaneus and inserts into the navicular lateral plantar margin. The oblique medial plantar component (“third ligament”) has been described recently.32 It originates in the coronoid fossa too between the anterior and medial articular faces of calcaneus and inserts into the scaphoid tuberosity. These structures have been widely described in radiological literature and can be assessed through MRI and ultrasound.15,34–39
At tarsal sinus level we find two ligaments between the calcaneus and the astragalus. The cervical ligament is more anterior and lateral while the inter-bone or calcaneal-astragalar ligament is lateral and posterior-wise. They are indirect stabilizers excessive preventing the inversion of the rear foot and opposing (above all the cervical ligament) the distal glide and medial rotation of the head of the astragalus over the calcaneus.
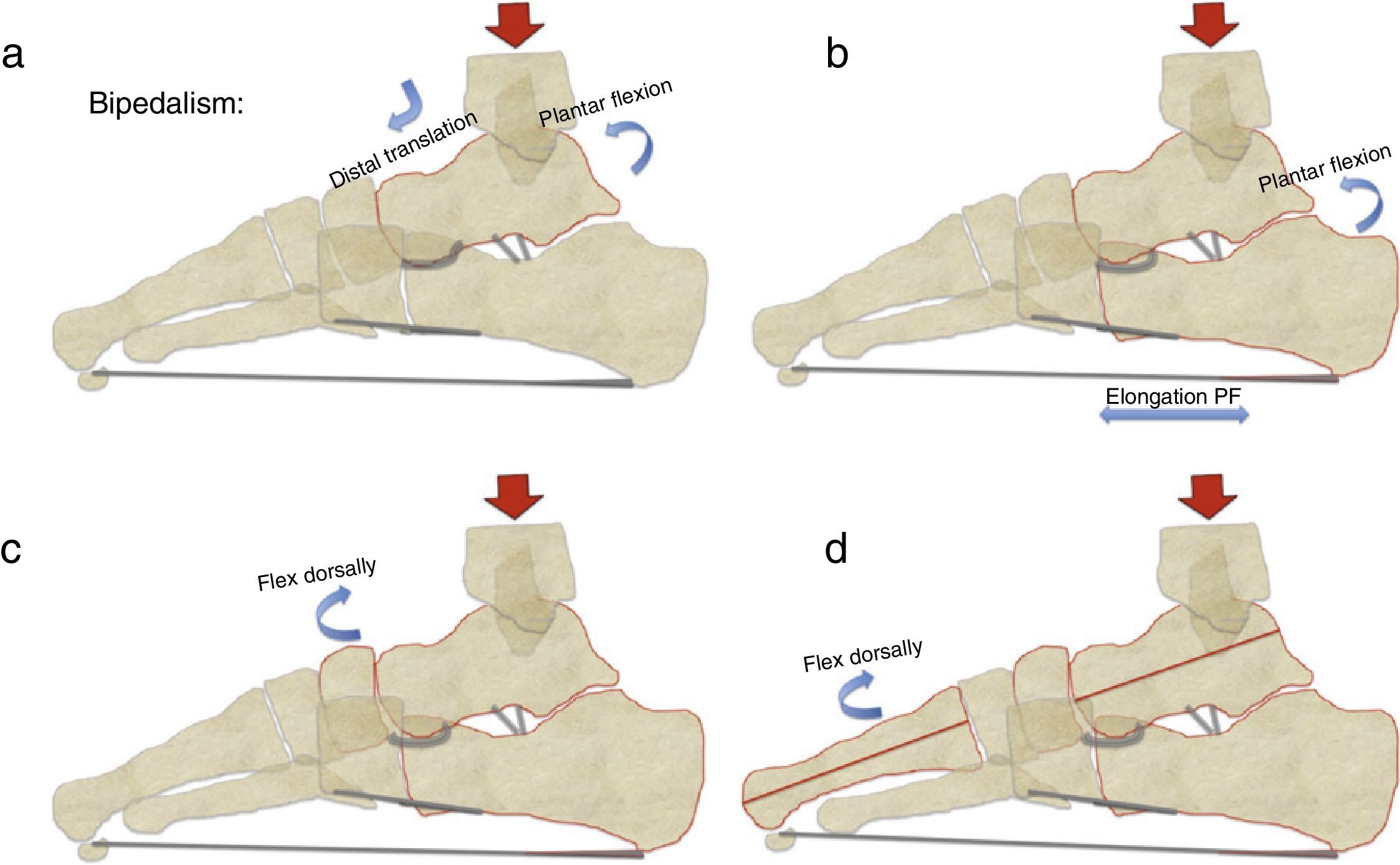
While loading the astragalus usually goes horizontal, rotates and glides distally over supastragalar joints. The inertia of plantar flexion on the astragalo-scaphoid joint causes descent and medial rotation of the head of the astragalus (Fig. 6a). The spring ligament restricts the medial rotation of the astragalus being the distal astragalar glide contained by the ligaments of tarsal sinus.
Chart on the schematic sagittal plane of forces that take place during bidedalism and against which the main stabilizers of the medial longitudinal plantar arch act upon: (a) the astragalus flexes plantarly toward a certain distal translation over the calcaneus, (b) plantar flexion of the calcaneus with elongation of the plantar fascia, (c) the scaphoid usually flexes dorsally, and (d) the metatarsal bones usually flex dorsally as well.
Calcaneus usually flexes plantar-wise too by lowering the plantar arch. This increase of pressure is mainly absorbed by the plantar fascia and to a lesser extent by the short and long plantar ligaments preventing the collapse of the arch while limiting the enlargement of its base (Fig. 6b). The scaphoid (as it happens with nails) goes for dorsal flexion, eversion and abduction as an inverse response to the medial rotation and plantar flexion of the astragalus (Fig. 6c)–movements restricted by the spring ligament and the eccentric contraction of PTT.
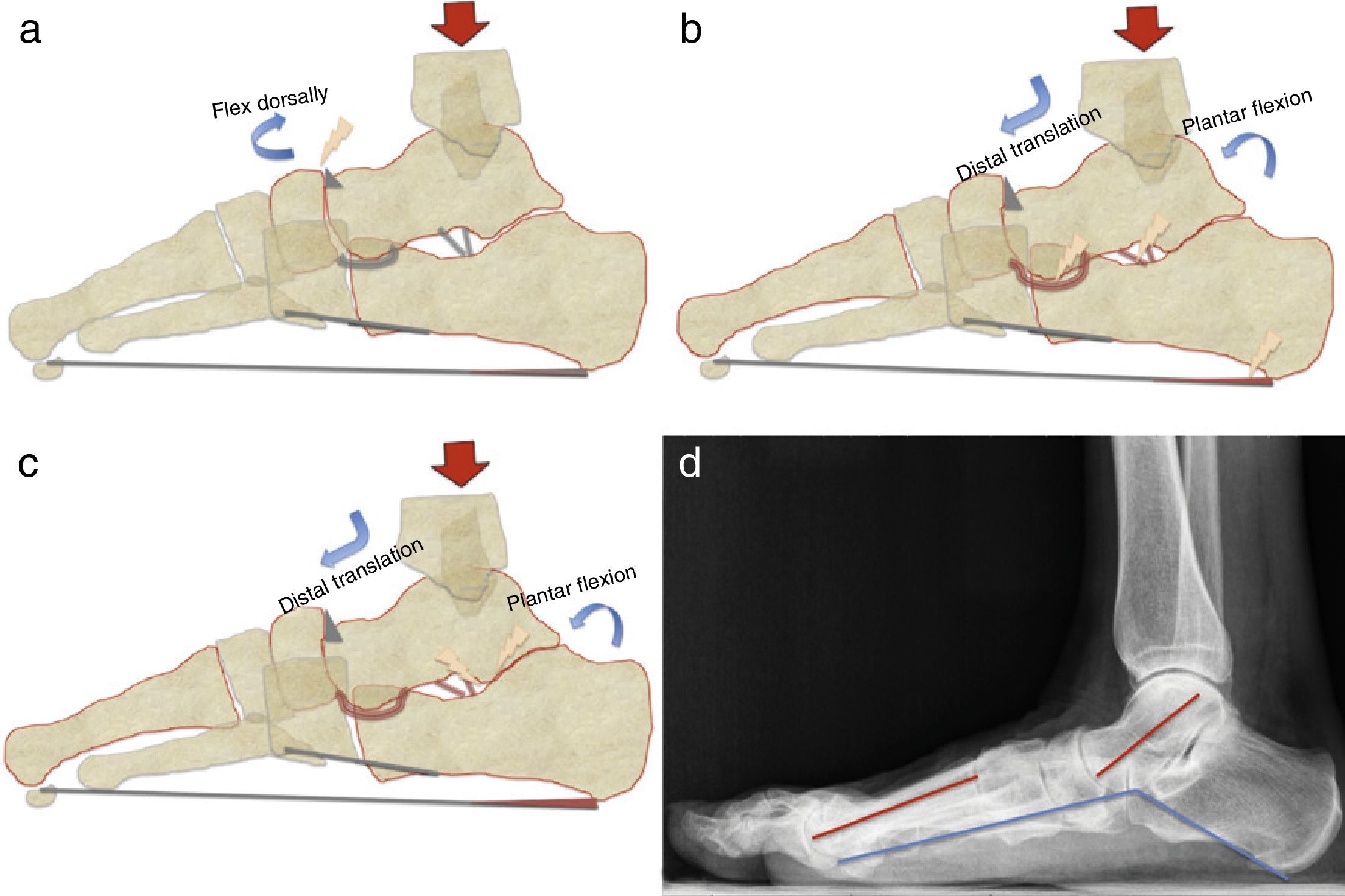
The talus peaks–an indicator of instability of the astragalo-scaphoid joint is also statistically significant in our study vs the control group and as far as we know this link had never been studied before.
Metatarsal bones usually flex themselves dorsally and abduct too (Fig. 6d).
The attempted most widely accepted explanation in scientific literature regards PTTD and AAFF as inter-related entities showing us that when any of these stabilizing mechanisms fails the plantar flexion of the astragalus cannot be counteracted efficiently by the spring ligament or the tarsal sinus ligaments (Fig. 7a) which in turn allows the medial rotation of the head of the astragalus and the distal impaction of astragalus on the calcaneus on the floor of tarsal sinus.40 The astragalus remains medially and plantarly rotated, the calcaneus remains in valgus rotation, there is abduction of the rear foot and the first metatarsal bone rotates dorsally (Fig. 7c and d). In turn this deformity of the plantar arch causes the progressive development of PTTD.14,24
Chart on the schematic sagittal plane representing the theoretical sequence of the morphological changes occurring when mechanical stabilizers fail: (a) instability at the astragalo-scaphoid joint secondary to the plantar flexion of the astragalus and the dorsal flexion of the scaphoid usually causes the development of dorsal ostephytosis (talus peaks); (b) both the plantar flexion and the distal unlimited translation of the astragalus over the calcaneus overload the calcaneal-astragalar ligaments and the spring ligament. The elongation of plantar fascia favors the appearance of the calcaneal spur; (c) the distal translation of the astragalus over the calcaneus ends with the impaction of the astragalus over the body of the calcaneus at the back of the tarsal sinus, and (d) Lateral Rx of loading foot with flat foot image, with plantar flexion of the astragalus. The blue line indicates the Costa-Bertain angle. The red lines show the impaired longitudinal axes of the astragalus and the first metatarsal bone.
Our study shows some possible flaws derived from the selection of case and control groups. It lacks a comparison group of healthy controls since we have adapted our analysis to our routine clinical context–this is why patients from the control group were exclusively selected due to the lack of damage to the PTT and for reasons for consultation different to PTTD. The use of “true” patients instead of healthy controls can lead to biases derived from the very condition of these patients or to the various subspecialties of our traumatologists. Be it as it may we wanted to come as close as possible to routine radiological clinical practice. As we said before it is very possible that this variability is also the cause for the differences found between our data and the data from scientific literature on the frequency of alteration-occurrence of some of the structures studied.
On the other hand there are some limitations as this is a retrospective study. If we would have done a prospective study we could have comparatively analyzed the contralateral foot or assessed the data from the flat foot before developing PTTD.
As a conclusion in our study we could confirm the statistically significant link between PTTD and injuries found on the MRI in key structures for the stabilization of plantar arch like the spring ligament and tarsal sinus ligaments. Similarly we found a high statistically significant frequency of calcaneal spur and talus peaks in patients with PTTD. This last finding–regarded as far as we know as a marker of astragalo-scaphoid instability has not been previously studied as associated to PTTD.
Finally we also found important differences vs the control group in the alterations of the Costa-Bertani angle and the frequency of radiological PVF even though it should be reminded that the ultimate diagnosis of PVF is totally clinical.
The link between these MRI-diagnosed structures and signs of radiological flat foot and PTTD and its possible physiopathological mechanisms can be especially useful for a precise diagnosis.
Authors- 1.
Responsible for the integrity of the study: LHH, JCA and VMF.
- 2.
Original idea of the study: LHH, MRR and JCA.
- 3.
Study design: LHH, RCA, JCA, EAM and MJP.
- 4.
Data mining: JCA, MRR, EAM, MJP and VMF.
- 5.
Data analysis and interpretation: JCA, RCA and LHH.
- 6.
Statistical analysis: LHH, EAM and RCA.
- 7.
Reference search: LHH, MJP and JCA.
- 8.
Writing: LHH.
- 9.
Manuscript critical review with intellectually relevant contributions: JCA, MRR and VMF.
- 10.
Final version approval: LHH, JCA, MRR, EAM, RCA and VMF.
Authors reported no conflict of interest.
Please cite this article as: Herráiz Hidalgo L, Carrascoso Arranz J, Recio Rodríguez M, Jiménez de la Peña M, Cano Alonso R, Álvarez Moreno E, et al. Disfunción del tendón tibial posterior: ¿qué otras estructuras están implicadas en el desarrollo del pie plano adquirido del adulto? Radiología. 2014;56:247–256.