Few studies have evaluated the radiologic characteristics of the development of the anterior tibial tuberosity. This study aimed to evaluate the radiologic characteristics of the anterior tibial tuberosity in a pediatric population broken down into age groups.
Material and methodsWe assessed 210 plain-film X-rays of the knee from patients aged from 10 to 17 years, divided into groups according to age and sex, for the presence of ossification of the anterior tibial tuberosity, the distance between the anterior tibial tuberosity and the metaphysis, and fusion with the epiphysis.
ResultsAt 10 years of age, the anterior tibial tuberosity was ossified in 50% of the girls but in only 25% of the boys. In all the girls, the anterior tibial tuberosity was ossified at 11 years, fusion of the anterior tibial tuberosity with the epiphysis had started at 12 years, and fusion was complete by 17 years. In boys, the process is delayed by one year compared to girls. A single center of ossification was found in all cases.
ConclusionThe ossification of the anterior tibial tuberosity starts distally, then the proximal part fuses with the rest of the epiphysis, and finally the distal part fuses with the tibia. The results of this study help enable a better analysis of the anterior tibial tuberosity in cases of knee pain.
Existen pocos estudios que evalúen las características radiológicas del desarrollo de la tuberosidad tibial anterior (TTA). El presente trabajo tiene por objeto evaluar las características radiológicas de la TTA en una población pediátrica de acuerdo a grupos de edad.
Material y métodosEs un estudio llevado a cabo en 210 radiografías de rodillas de pacientes entre los 10 y 17 años, que fueron divididos por grupos de edad y sexo. Se evaluaron la presencia de osificación de la TTA, la distancia de esta a la metáfisis y la fusión con la epífisis.
ResultadosA los 10 años de edad, la TTA estaba osificada en el 50% de las mujeres y solo en el 25% de los hombres. A los 11 años todas las mujeres tenían osificada la TTA, a los 12 tenían fusión de la TTA y con la epífisis, y a los 17 años la fusión era completa. En los hombres este proceso se produce un año más tarde que en las mujeres. En todos los casos se encontró un solo núcleo de osificación.
ConclusiónLa osificación de la TTA se inicia distalmente, posteriormente se fusiona su parte proximal con el resto de la epífisis y finalmente se fusiona en su parte distal a la tibia. Este estudio ayuda a un mejor análisis de la TTA cuando nos enfrentamos a un dolor de rodilla.
Anterior tibial tuberosity (ATT) is the main insertion area of the patellar tendon on the anterior and posterior part of the tibia. This tendon stretches to the perichondrium of the physis and the periosteum of the adjacent metaphysic.1–3 Growth plates are divided in pressure and traction plates,4 with functional and histological differences between them. The ATT is a traction plate since the patellar tendon is inserted into it; it supports a large mechanical load during knee extension, and it is mostly fibrocartilaginous.4 Traction plates are located in the junction of the tendons to the bones and they are subjected to traction forces; they contribute to the development of bone morphology, but not to its longitudinal growth. Pressure plates are located on the ends of long bones, between the epiphysis and the metaphysis. Subject to pressure forces, they contribute to longitudinal growth and its ossification is endochondral. There are no clear radiographic differences between these types of growth plates. It is considered that traction plates take a little longer to ossify due to direct or indirect mechanical effects on them.
There are few studies about the development of ATT. Hughes and Sunderland5 described a fibrous tissue posterior to ATT. Lewis3 interpreted this zone as a “fibrous junction” between the epiphysis and diaphysis. Badi6 showed ATT plate fibrous structure in rats. In humans there are few anatomical studies about the development of the ATT growth plate.7 Ogden et al.7–10 conducted radiographic and histomorphologic studies claiming that the development of ATT has seven stages based on the age of the patient.
When X-rays of children with anterior knee pain are analyzed it can be puzzling to assess ATT because there are few descriptions about what the normal radiographic development really is.
The goal of this article is to evaluate the radiographic features of ATT in a pediatric population based on age groups.
Material and methodsThis study was conducted in compliance with the ethical principles based on the Helsinki declaration and it was approved by the hospital ethics committee. Since it is a study based on image archives and medical histories without any interventions on patients it did not require informed consent.
It is an observational, descriptive, retrospective study in which the information source used is digital anteroposterior and lateral X-rays of the knee taken without load using a Siemens Polymat Multix X-ray, on patients looking for medical assistance due to limb trauma, who according to the retrospective review of their medical history, did not have any clinical or radiographic compromises of the knee. The inclusion criteria were: X-rays of 10–17-year-old patients, without post-traumatic diseases or anomalies in the proximal third of the tibia and who in the lateral projection were at between 20° and 60° of flexion. The exclusion criteria were: X-rays taken with inadequate techniques, fractures of the patella, proximal tibia and/or distal femur, presence of osteosynthesis material in the proximal tibia, patients with a history of chronic pain in the knees in the previous 12 months, diagnosis of cerebral palsy, hemophilia, nephrotic syndrome, history of septic arthritis, presence of hemarthrosis, neoplasms around the knee and radiographic findings of anomalies in bone density.
The variables studied were: sex, laterality and age in years and months. The age groups were defined in the following manner. 10-year-old group: individuals who were between 10 years and 10 years and 11 months, 29 days, and so on with the following groups until the final group of 17-year-olds.
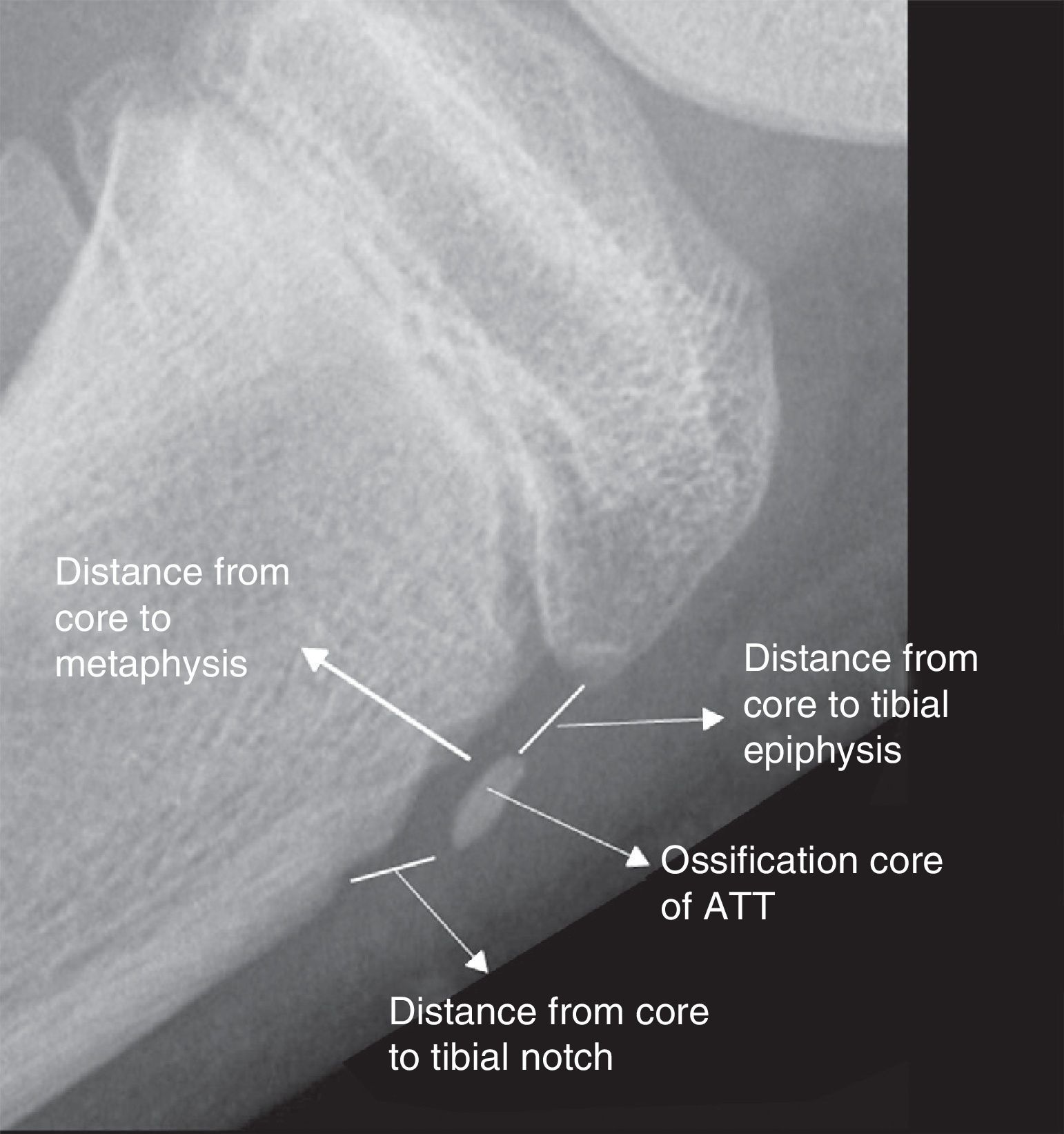
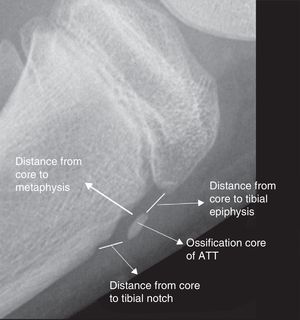
The radiographic variables determined for the study were: presence, number and size of the ATT ossification center, distance between the ossification center and the metaphysis as measured from the posterior edge of the nucleus in its central zone up to the anterior edge of the metaphysis; distance between the ossification center and the superior epiphysis of the tibia as measured from the superior edge of the nucleus to the inferior edge of the epiphysis of the tibia, and the distance between the inferior edge of the nucleus and the metaphyseal notch of the tibia (Fig. 1).
The X-rays were assessed by a radiologist with over 10 years of experience in pediatrics and a pediatric orthopedician who both reached consensus of the findings. Data collection and statistic analysis were performed on an Excel 2010 table. The authors declare that they do not have any conflicts of interests in the present study and they did not have any sources of funding.
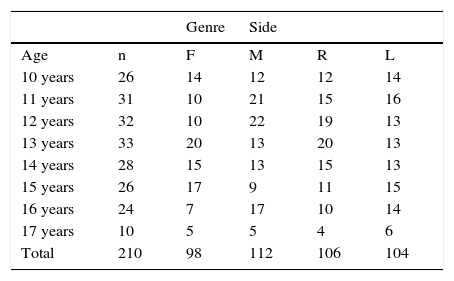
Results210 X-rays were obtained, which were distributed based on age, sex and side of the knee analyzed; 46.6 per cent were women and 53.3 per cent, men. Although there was a smaller number of 17 year-old cases the distribution by age can be considered homogeneous (Table 1).
Distribution based on genre, sex and side groups.
| Genre | Side | ||||
|---|---|---|---|---|---|
| Age | n | F | M | R | L |
| 10 years | 26 | 14 | 12 | 12 | 14 |
| 11 years | 31 | 10 | 21 | 15 | 16 |
| 12 years | 32 | 10 | 22 | 19 | 13 |
| 13 years | 33 | 20 | 13 | 20 | 13 |
| 14 years | 28 | 15 | 13 | 15 | 13 |
| 15 years | 26 | 17 | 9 | 11 | 15 |
| 16 years | 24 | 7 | 17 | 10 | 14 |
| 17 years | 10 | 5 | 5 | 4 | 6 |
| Total | 210 | 98 | 112 | 106 | 104 |
R: right; F: feminine; L: left; M: masculine.
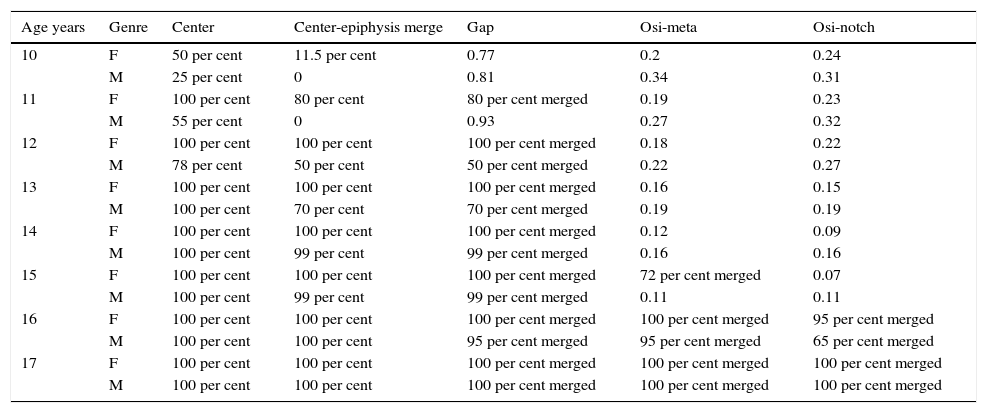
When analyzing in each age range the presence of the ATT ossification center its fusion with the epiphysis determined by the distance between the latter and proximal epiphysis of the tibia (Gap), its fusion with the metaphysis (osi-meta distance) and its fusion with the tibial notch (osi-notch), the following was found (Table 2):
Overall results.
| Age years | Genre | Center | Center-epiphysis merge | Gap | Osi-meta | Osi-notch |
|---|---|---|---|---|---|---|
| 10 | F | 50 per cent | 11.5 per cent | 0.77 | 0.2 | 0.24 |
| M | 25 per cent | 0 | 0.81 | 0.34 | 0.31 | |
| 11 | F | 100 per cent | 80 per cent | 80 per cent merged | 0.19 | 0.23 |
| M | 55 per cent | 0 | 0.93 | 0.27 | 0.32 | |
| 12 | F | 100 per cent | 100 per cent | 100 per cent merged | 0.18 | 0.22 |
| M | 78 per cent | 50 per cent | 50 per cent merged | 0.22 | 0.27 | |
| 13 | F | 100 per cent | 100 per cent | 100 per cent merged | 0.16 | 0.15 |
| M | 100 per cent | 70 per cent | 70 per cent merged | 0.19 | 0.19 | |
| 14 | F | 100 per cent | 100 per cent | 100 per cent merged | 0.12 | 0.09 |
| M | 100 per cent | 99 per cent | 99 per cent merged | 0.16 | 0.16 | |
| 15 | F | 100 per cent | 100 per cent | 100 per cent merged | 72 per cent merged | 0.07 |
| M | 100 per cent | 99 per cent | 99 per cent merged | 0.11 | 0.11 | |
| 16 | F | 100 per cent | 100 per cent | 100 per cent merged | 100 per cent merged | 95 per cent merged |
| M | 100 per cent | 100 per cent | 95 per cent merged | 95 per cent merged | 65 per cent merged | |
| 17 | F | 100 per cent | 100 per cent | 100 per cent merged | 100 per cent merged | 100 per cent merged |
| M | 100 per cent | 100 per cent | 100 per cent merged | 100 per cent merged | 100 per cent merged |
F: feminine; Gap: measurement in centimeters between the ossification center and the upper tibial epiphysis; M: masculine; center: percentage of patients with a presence of ossification center; osi-meta: measurement in centimeters between the posterior side of the center and the anterior edge of the tibial metaphysis; osi-notch: measurement in centimeters between the ossification center ant the metaphyseal notch.
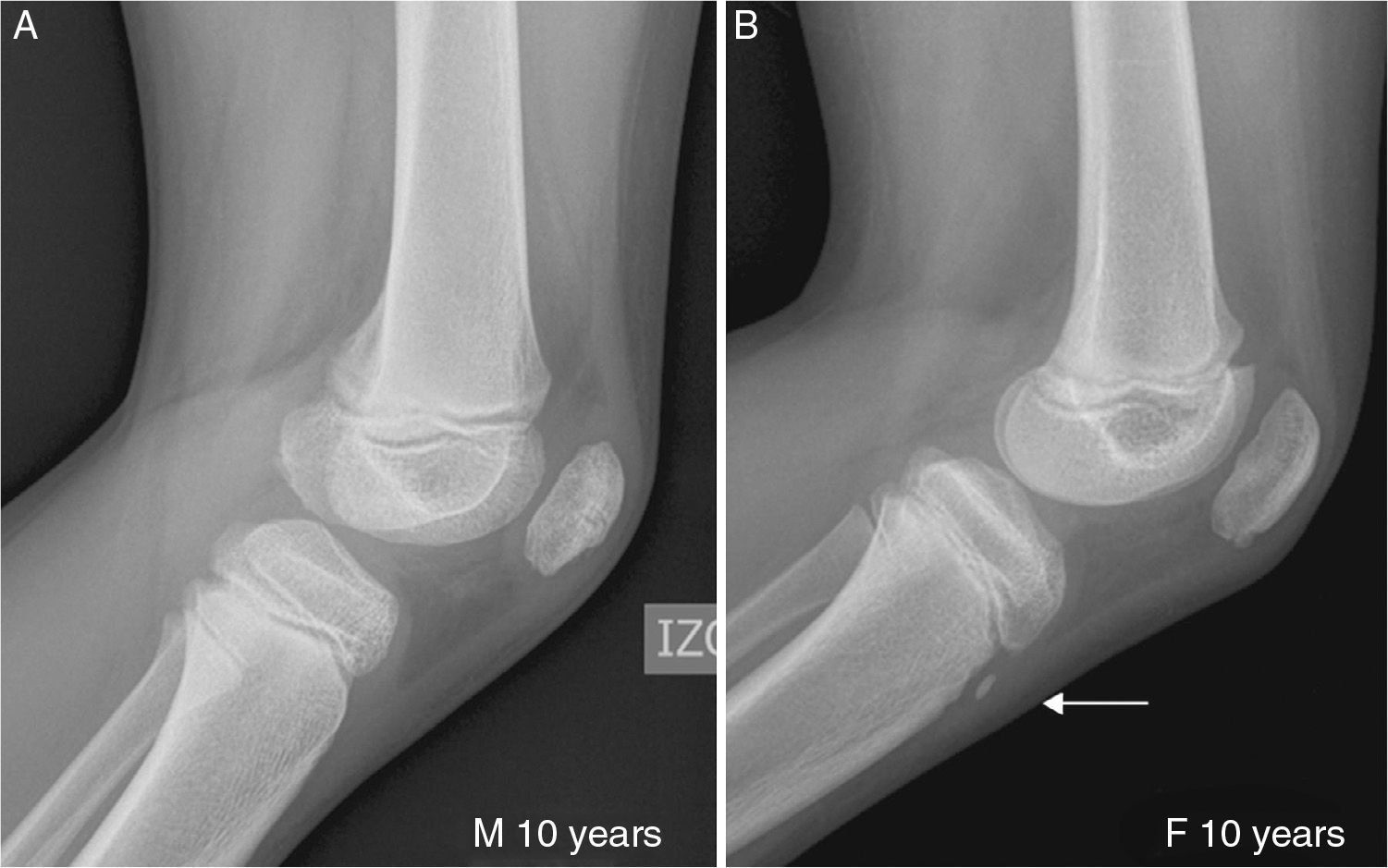
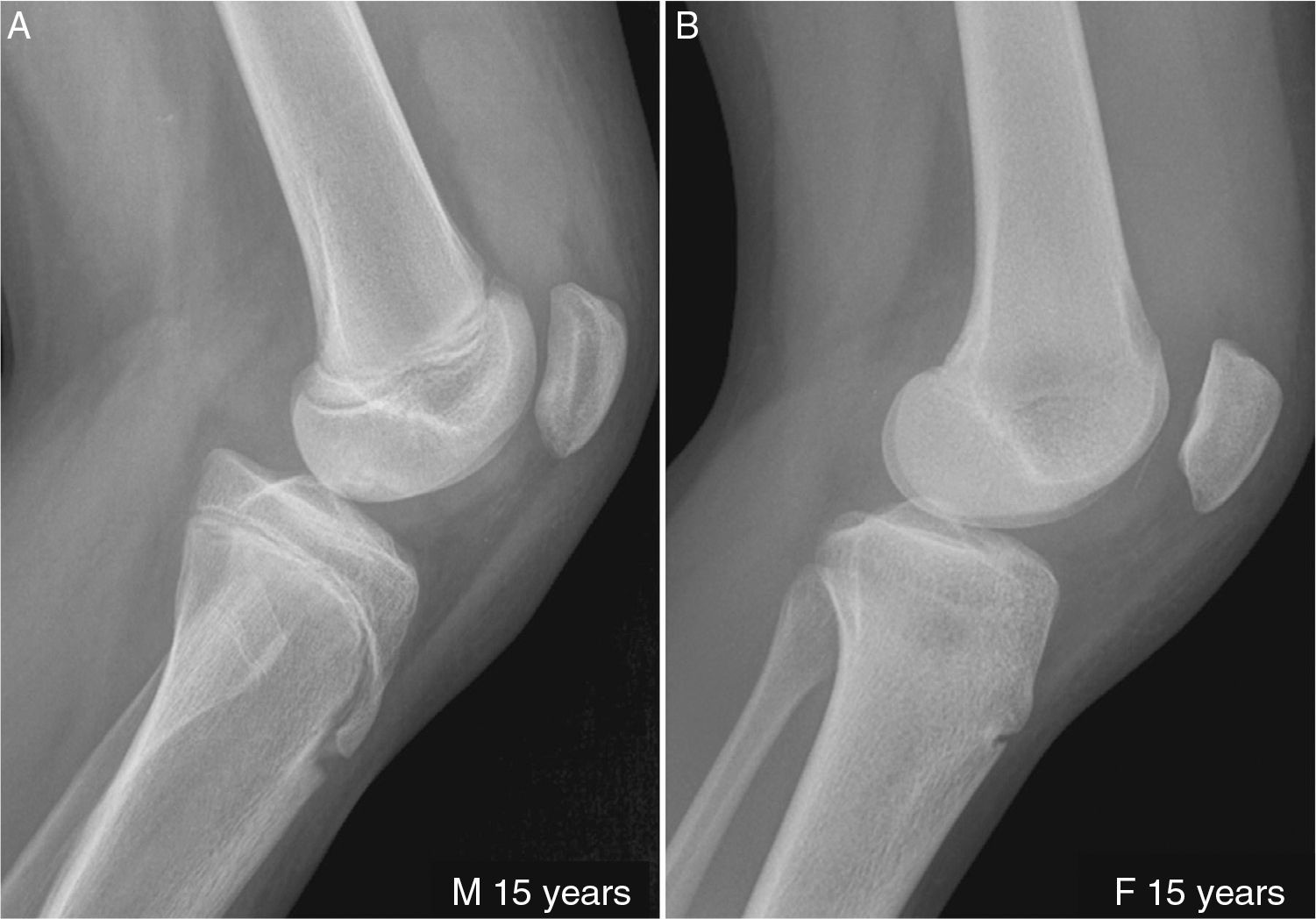
At 10 years of age, the ATT nucleus was observed in 50 per cent of the females and 25 per cent of the males. Three females showed junction between the latter and the epiphysis of the tibia (11.5 per cent). None of the males had this junction (Fig. 2).
At 11 years of age, the females had ossified ATT, 80 per cent of them with fusion with the epiphysis of the tibia. Only 55 per cent of the males had an ossification center and none of them had merged into the proximal tibia.
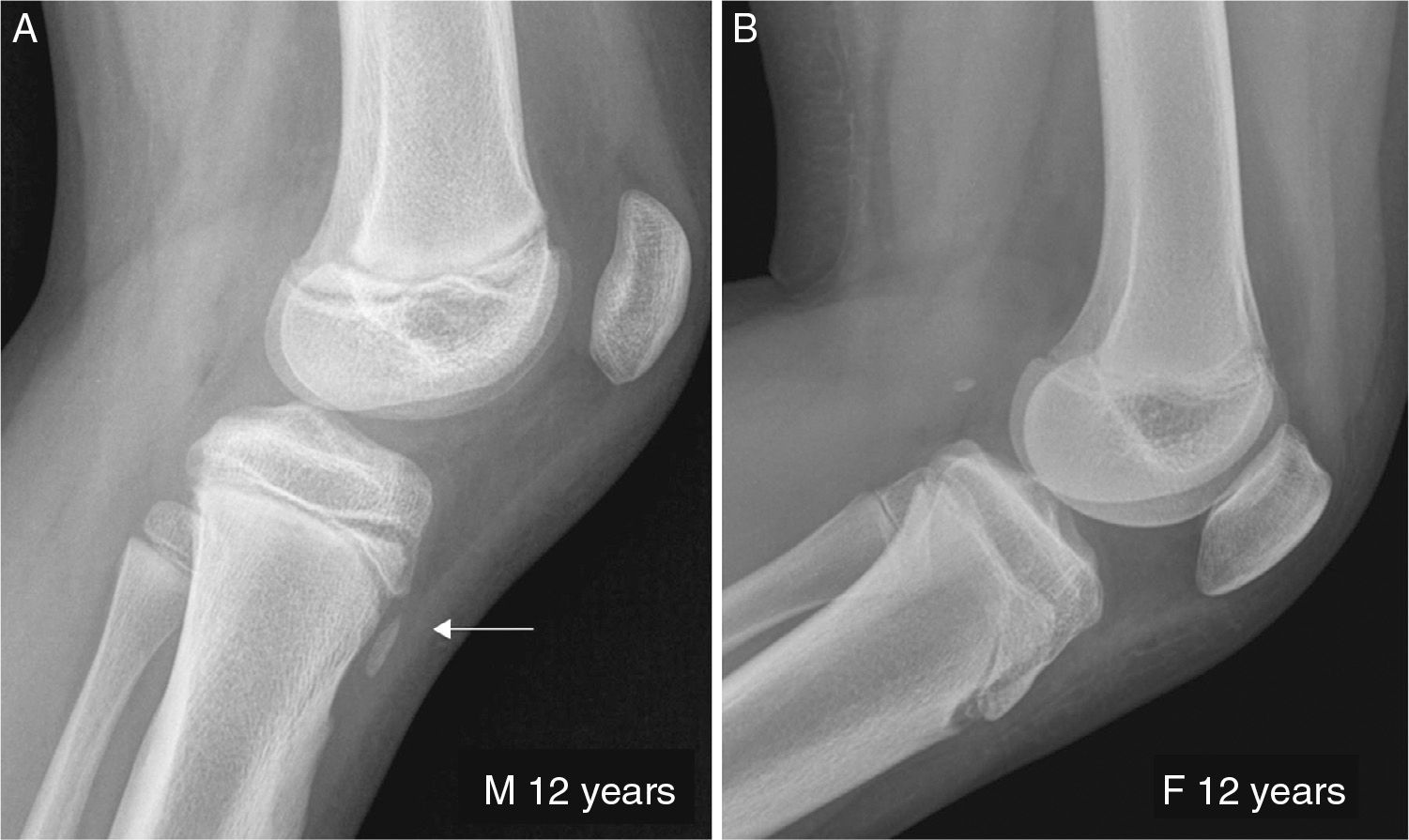
At 12 years of age all the females showed fusion of the nucleus with the tibia in the shape of a tongue; 22 per cent of the males did not show ossification centers (Fig. 3).
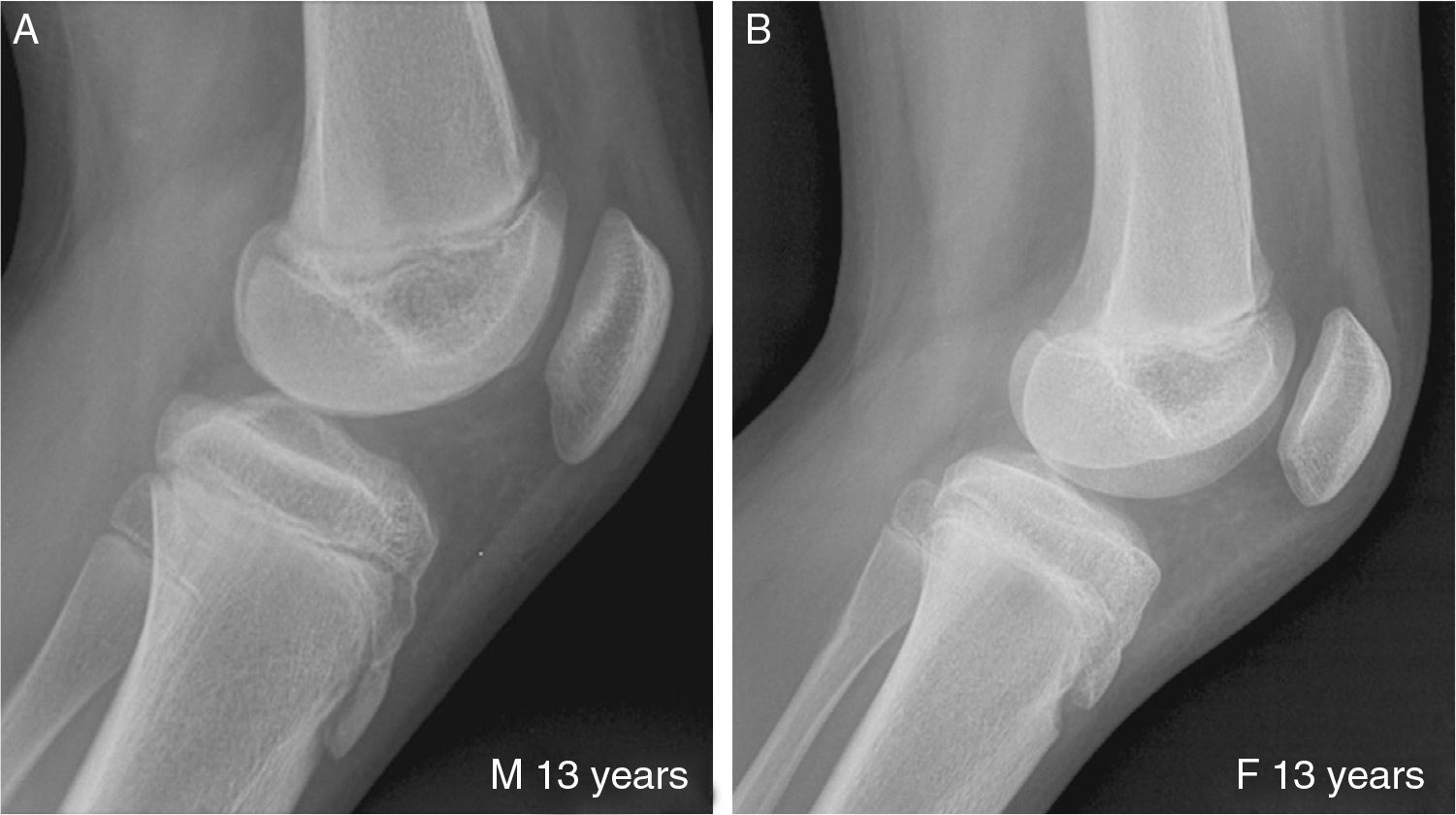
At 13 years of age, all the males had an ATT nucleus while 70 per cent of them had merged into the epiphysis of the tibia (Fig. 4), which was observed in 99 per cent of the males at 14 years of age. In this age group, 53 per cent of the females showed fusion of the posterior part of the nucleus with the tibial metaphysis.
At 15 years of age 72 per cent of the females showed fusion of the nucleus with the metaphysis and in males, the radiographic conditions were similar to those of the 14-year-old group (Fig. 5).
(A) Fifteen year old boy showing total merge and thickening of the upper side of the ossification center merge and in process of ossification in the posterior side. (B) Fifteen year old girl showing total merge of the ossification center both in upper and posterior sides. Lower side compatible with fibrocartilage area (traction zone).
At 16 years of age, 95 per cent of the females showed complete fusion of the ATT nucleus with the tibial metaphysis, and the radiologic notch had disappeared in this location, while in 95 per cent of males it had merged into the superior and posterior part of the tibia while only 65 per cent of them showed fusion with the inferior part of the tibial metaphysis remaining this notch in 35 per cent of the cases (Fig. 6).
At 17 years of age, 100 per cent of the females and the males showed complete ATT ossification with fusion with the tibial proximal epiphysis and metaphysis.
DiscussionThe radiographic findings of this study show a distal to proximal ATT ossification pattern with subsequent fusion with the epiphysis and finally the metaphysis that is more premature in females than in males starting at 10–12 years of age.
ATT develops initially as an anterior cartilaginous extension of the proximal tibial epiphysis at weeks 12–15 weeks of fetal life, a moment in which an outside-inside growth of fibrovascular tissue starting at the zone of Ranvier.6,7
The ATT growth plate develops after birth as a structure separated from the proximal tibial growth plate. Histologically, there are three regions though the territory among them is progressive. Proximally the cellular architecture is analogous to the rest of the proximal tibial growth plate and it is the result of an endochondral ossification process, except that cell columns are short, with a greater degree of intercellular matrix and the lacunae are distorted due to elongation. This region is transformed distally into a fibrocartilaginous zone in which the hyaline cartilage forms fibrocartilage while morphing into bone due to membranous ossification. The third region shows a transition from hyaline cartilage to fibrous tissue and finally to bone due to membranous ossification.7,8
There are few studies on the development of ATT.7–10 In these studies it is concluded that its secondary ossification is not evident in patients under 10 years of age and in this age range, only a small anterior metaphyseal notch is observed marking the ATT distal point. The appearance of a well-formed secondary ossification center is evident between 11 and 12 years of age, it forms in the distal portion of the tuberosity. This ATT nucleus grows proximally toward the tibial epiphysis until only a small cartilage bridge is present between the two ossification centers, which will be replaced by bone in the next 2 years, ultimately closing the tuberosity. The physis of the proximal tibia closes first and then extends gradually in the ATT causing the physiological epiphyisiodesis in females between 13 and 15 years of age and males between 15 and 17 years of age.
The histologic data presented by Ogden et al.7 were collected from 7 specimens of between 11 and 13 years of age, and the radiographic features were analyzed in 66 corpses of newly-born up to 14 year-old children, without specifying groups or ages.
The progression of the development and fusion of ATT observed in the present work were very similar to those described by Ogden et al.,7–10 who describe the ATT secondary ossification that begins in the distal portion, growing toward the proximal one with subsequent merge into the proximal tibial epiphysis. Then the merge of the distal part of the nucleus into the tibial distal metaphysis occurs.
In the 10-year-old female group a secondary ossification nucleus was found in 50 per cent of the cases while it was found in 25 per cent of male cases only. When analyzing girls younger than 10 years 5 months old, 72 per cent already showed ATT nucleus and in up to 11.5 per cent of them there was merging between the nucleus and the proximal tibial epiphysis, while none of the boys in this age group showed this junction. This proves that early ATT ossification is common in girls younger than 10 years of age.
Some authors show isolated cases of ATT with fragmentation or with more than one ossification nucleus.11 This feature was not observed in this study, and only one secondary ossification nucleus was found in the 210 cases.
When it comes to the distance values from the ATT nucleus to the metaphysis and the proximal tibial epiphysis, which decreased as age increased, they indicate the direction and progression of ossification, first with merging into the epiphysis and then into the metaphysis.
The findings about the progressive development of ossification and ATT merge found into the different age groups are in agreement with the use of this feature as a partial way to determine skeletal maturity.12
Although some of the limitations of the work lie in the fact that the X-rays used were taken at different knee flexion angles, which could hypothetically alter some of the measurements taken, we believe that they do not alter the interpretation of our results.
This study allows us to characterize the development of ATT in a pediatric population. The radiographic findings allow us to establish a normal distal-to-proximal ossification pattern with subsequent merge into the epiphysis and ultimately into the metaphysis, a process that always begins at an earlier age in females than in males. Our results can be used as a model for subsequent studies seeking to describe abnormal patterns that compromise ATT, such as Osgood Schlatter disease or avulsion fractures in this same age group.8,13,14
Ethical responsibilitiesProtection of people and animalsThe authors declare that no experiments with human beings or animals have been performed while conducting this investigation.
Data confidentialityThe authors confirm that in this article there are no data from patients.
Right to privacy and informed consentThe authors confirm that in this article there are no data from patients.
Authors- 1.
Manager of the integrity of the study: EVA.
- 2.
. Study Idea: EVA.
- 3.
Study Design: EVA, DDH, LAM.
- 4.
Data Mining: EVA, DDH, LAM.
- 5.
Data Analysis and Interpretation: EVA, DDH, LAM.
- 6.
Statistical Analysis: EVA, DDH.
- 7.
Reference: EVA, DDH.
- 8.
Writing: EVA,DDH.
- 9.
Critical review of the manuscript with intellectually relevant remarks: EVA, DDH, LAM.
- 10.
Approval of final version: EVA, DDH, LAM.
The authors declare no conflict of interests associated with this article whatsoever.
Please cite this article as: Vergara-Amador E, Davalos Herrera D, Moreno LÁ. Características radiológicas del desarrollo de la tuberosidad tibial anterior. Radiología. 2016;58:294–300.