The radiological evaluation of the postsurgical middle ear is complex due to the intricate anatomy of this region and the wide variety of procedures and materials used iin middle ear surgery. Knowledge of these factors will enable normal postsurgical changes to be differentiated from complications. This article describes the most common surgical procedures in the middle ear, their indications, and the normal radiological appearance after these procedures. It reviews the most common causes of failure in stapes surgery, in surgery for chronic otitis media, and in surgery for cholesteatoma, suggesting the best imaging method to assess the middle ear in each case.
ConclusionComputed tomography enables the evaluation of prostheses and the aeration of the cavities, whereas magnetic resonance imaging makes it possible to characterize the possible occupation of the cavities and is the technique of choice for the follow-up of closed mastoidectomy for cholesteatomas.
La valoración radiológica del oído medio operado es compleja por su intrincada anatomía y la amplia variedad de procedimientos quirúrgicos y materiales utilizados. Su conocimiento permitirá diferenciar los cambios posquirúrgicos normales de las complicaciones. En este artículo se describen los procedimientos quirúrgicos más comunes, sus indicaciones y su apariencia radiológica normal. Se revisan las causas más frecuentes de cirugía fallida en la cirugía del estribo, la otitis media crónica y en el colesteatoma, y se sugiere en cada caso la técnica de imagen de elección para su valoración.
ConclusiónLa tomografía computarizada permite la valoración de las prótesis y comprobación de la aireación de las cavidades, mientras que la resonancia magnética posibilita la caracterización de la posible ocupación de las cavidades y es la técnica de elección en el seguimiento del colesteatoma operado mediante mastoidectomía cerrada.
Radiological evaluation of the postoperative middle ear (ME) is particularly demanding. To the already complex anatomy of the temporal bone is added the wide variety of existing surgical techniques. Imaging plays an increasingly important role in the follow-up and management of patients who undergo ME surgery. In most cases, clinicians familiar with the different types of surgery and their radiological appearance will be able to distinguish between normal postoperative changes in recurrent disease and possible complications.
The most common surgical procedures can be classified as: operations for access and removal (mastoidectomies) and operations for functional reconstruction of the conduction system (tympanoplasties and ossicular chain reconstruction techniques).
In general, computed tomography (CT) is useful in assessing prostheses and confirming cavity aeration, while magnetic resonance imaging (MRI) is capable of characterising possible cavity occupation. The most established indication for MRI is the monitoring of cholesteatoma after closed mastoidectomy.
This article describes the most common surgical procedures, their indications and their normal radiological appearance. It reviews the most common causes of surgical failure in stapes surgery and surgery for chronic otitis media (COM) and surgery for cholesteatoma, and proposes the imaging technique of choice for assessment in each case.
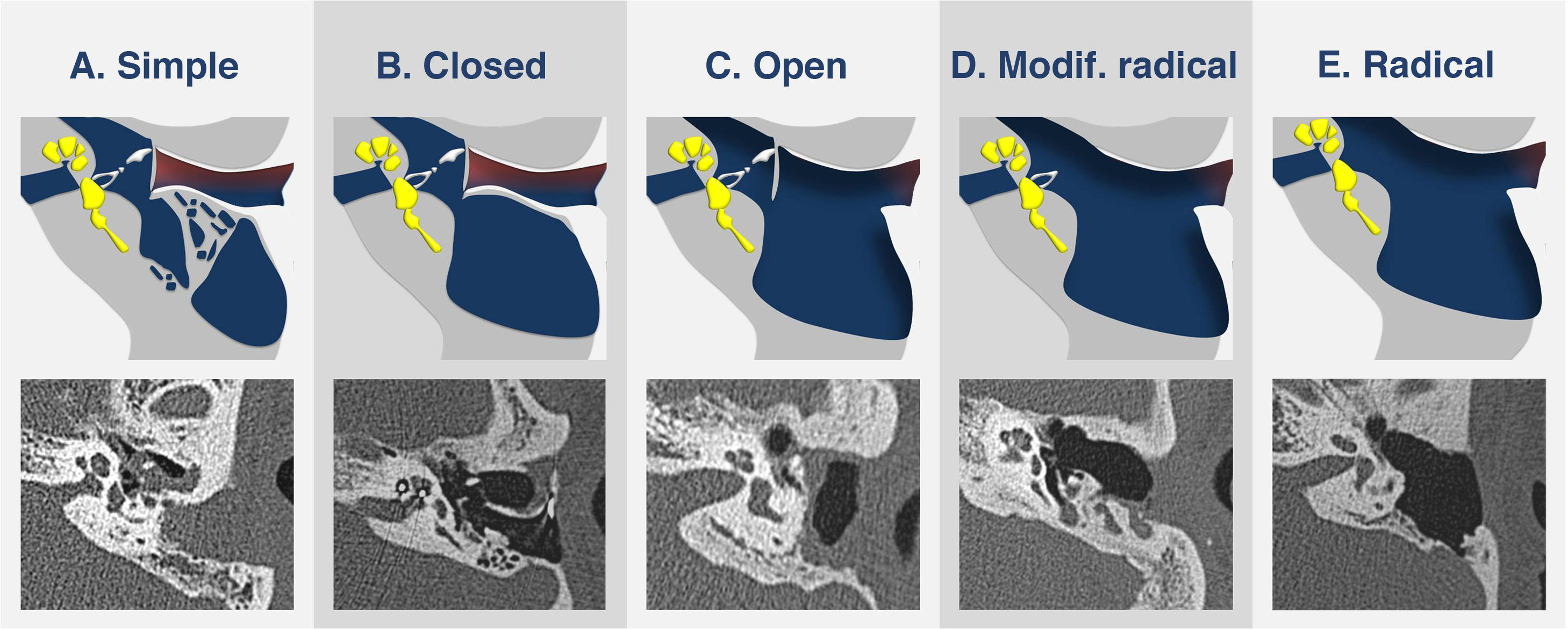
Surgical proceduresMastoidectomyMastoidectomy comprises multiple procedures intended to eradicate ME disease and mastoid disorders, and access different portions of temporal bone. It is often associated with tympanoplasty. The most common indications are COM, cholesteatoma and procedures in which it is used as an access route.1 The different types of mastoidectomy can be assessed using imaging techniques, preferably CT. The anatomical structures that should be evaluated are: mastoid air cells, Koerner's septum, the wall of the external auditory canal (EAC) and the ossicular chain. They are classified in order of increasing complexity as follows (Fig. 1):
Types of mastoidectomy. Illustration and identification using transverse computed tomography imaging of each type of mastoidectomy. (A) Simple mastoidectomy: the cortex and the most external air cells are resected. (B) Closed mastoidectomy: the cortex, all air cells and Koerner’s septum are resected. (C) Open mastoidectomy: the posterior wall of the external auditory canal is also resected. (D) Modified radical mastoidectomy: part of the chain that is affected is also resected and reconstructed. (E) Radical mastoidectomy: all middle ear structures are resected and not reconstructed.
Simple mastoidectomy: the cortex and the most external air cells are resected (Fig. 1A). This is used in cases in which limited air cell resection is needed.
Closed or canal wall up mastoidectomy: the cortex, all air cells and Koerner’s septum, which forms the lateral wall of the mastoid antrum, are resected. The posterior wall of the EAC is preserved, hence the name “canal wall up” (Fig. 1B). It is used in cases of cholesteatoma, COM, access for cochlear implant placement and facial nerve disorder.1,2 This type is preferable to open mastoidectomy because it spares more of the patient’s anatomy, avoids the potential need for lifelong ear care and improves the fit of hearing aids.3 However, it is associated with higher rates of residual and recurrent disease in the treatment of cholesteatoma.4,5
Open or canal wall down mastoidectomy: in addition to the structures mentioned in closed mastoidectomy, the posterior wall of the EAC is also resected such that the mastoid cavity is externalised to the external auditory canal (Fig. 1C). It is used in cases of cholesteatoma having spread to the petrous apex or the inner ear and in cases in which patient follow-up is not reliable.1,6 It includes two subtypes: modified radical, in which the affected part of the ossicular chain is resected and reconstructed (Fig. 1D), and radical, which involves resection but not reconstruction of all ME structures and externalisation of the ME and the Eustachian tube, which is freely connected to an epithelialised mastoid cavity (Fig. 1E). At present, the radical version is usually not used; the potential indications are extensive cholesteatoma and tumours.1
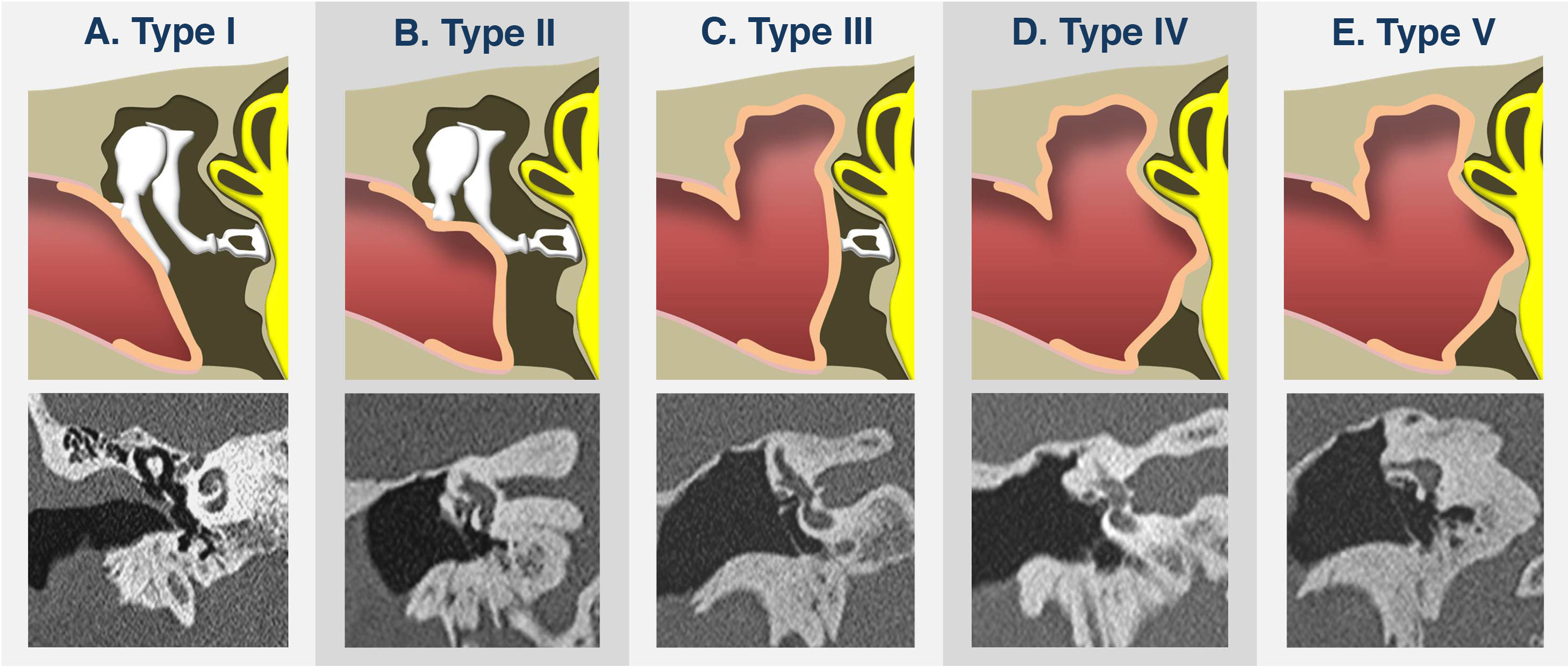
Reconstruction techniquesTympanoplastyThis is the surgical procedure for the repair of the tympanic membrane and the reconstruction of the ossicular chain. Its complexity will depend on the impairment caused by the disease and the potential for functional recovery.7 The most commonly used classification is the Wullstein classification, which distinguishes five recognisable types by CT (Fig. 2):8
- •
Type I or myringoplasty: this consists exclusively of tympanic membrane (TM) repair using a graft (Fig. 2A).
- •
Type II: this is used in cases with malleus erosion; the TM graft is placed on the remaining malleus or the incus (Fig. 2B).
- •
Type III: this is used when the malleus and the incus are eroded; the TM graft is placed on the stapes head (Fig. 2C). If a graft or strut is placed between the TM and the stapes head, it is called minor columella tympanoplasty, and if it is placed between the TM and the stapes footplate, it is called major columella tympanoplasty.
- •
Type IV: this is used when the malleus, the incus and the superstructure of the stapes are eroded; the TM graft is placed on the stapes footplate (Fig. 2D).
- •
Type V: this is used when the stapes footplate is ankylosed; the TM graft is placed directly on a fenestration made in the lateral semicircular canal (Fig. 2E).
Types of tympanoplasty (Wullstein classification). Illustration and identification using coronal computed tomography reconstructions of each type of tympanoplasty. (A) Type I: myringoplasty. The tympanum is reconstructed with a graft. (B) Type II: the graft is placed over the remaining malleus or the incus. (C) Type III: the graft is placed over the stapes. (D) Type IV: the graft is placed over the footplate. (E) Type V: the graft is placed over a fenestration in the lateral semicircular canal.
This is reconstruction of the mechanism of sound transmission, consisting of placement of a graft or prosthesis between the TM and the inner ear to restore its continuity. There is a wide variety of prostheses of different designs and materials. The choice of prosthesis will depend on its properties, patient requirements, disease extent and surgeon experience.9 CT is the imaging technique of choice to assess it and evaluate prosthesis position. Techniques are classified based on the portion of the chain replaced (Fig. 3):
Types of ossicular chain reconstruction. Illustration and identification using coronal computed tomography reconstructions of each type of reconstruction. (A) Partial reconstruction prosthesis: the prosthesis is attached to the graft/tympanic membrane (TM) and to the stapes head. (B) Full reconstruction prosthesis: the prosthesis is attached to the graft/TM and to the footplate or oval window. (C) Stapes prosthesis: the prosthesis is attached to the incus and the piston is placed through an orifice in the footplate or over a graft in the oval window if the footplate is resected.
Prosthesis for partial reconstruction: this is used when the stapes is complete and mobile; the prosthesis replaces the malleus and incus and is attached to the TM or graft and the stapes head (Fig. 3A). It is often used in cholesteatoma and COM in which the malleus and the incus are more commonly affected.1,2 There is a subtype called incus interposition, currently in disuse, in which the affected incus is resected, remodelled and connected to the handle of the malleus and the stapes.
Prosthesis for full reconstruction: this is used when the stapes is affected; the prosthesis is attached to the TM or graft and to the footplate or oval window (Fig. 3B).
Stapes surgery: the main indication for this is otosclerosis. The superstructure of the stapes is resected, the prosthesis is attached to the incus or the footplate is resected and the piston is placed on a graft over the oval window (stapedectomy) or a hole is made in the footplate through which the piston is placed (stapedotomy) (Fig. 3C).
Surgical failureAcute and serious surgical complications are those common to all skull base procedures and include bone dehiscence, bleeding, abnormal cerebrospinal fluid (leak, infection or hydrocephaly), infection and vascular injury.1 This article will focus on the non-emergency complications that usually present with persistent or recurrent hearing loss and will classify them according to the initial disease that motivated the surgical procedure.
Surgical failure in COMThe main indication for surgery in COM is disease that persists or recurs despite mastoidectomy and/or tympanoplasty with or without ossicular chain reconstruction. Initially, the imaging technique of choice is CT. The most common reasons for failure are:
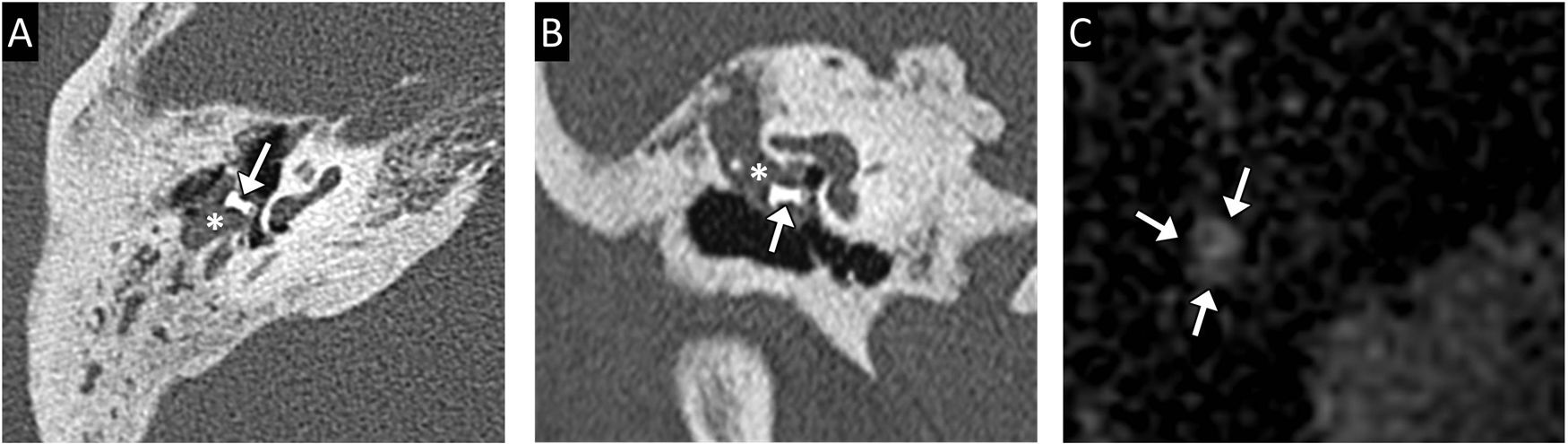
ME opacification: the ME may become occupied by inflammatory fluid or granulation tissue, usually in relation to lack of ventilation.10 Granulation tissue has a non-specific appearance on CT as soft tissue with no bone erosion; on MRI it does not restrict diffusion and exhibits late uniform contrast uptake (Fig. 4).11 In cases in which cholesteatoma is suspected, non-echo-planar diffusion-weighted imaging (DWI) enables characterisation of cavity-occupying tissue.
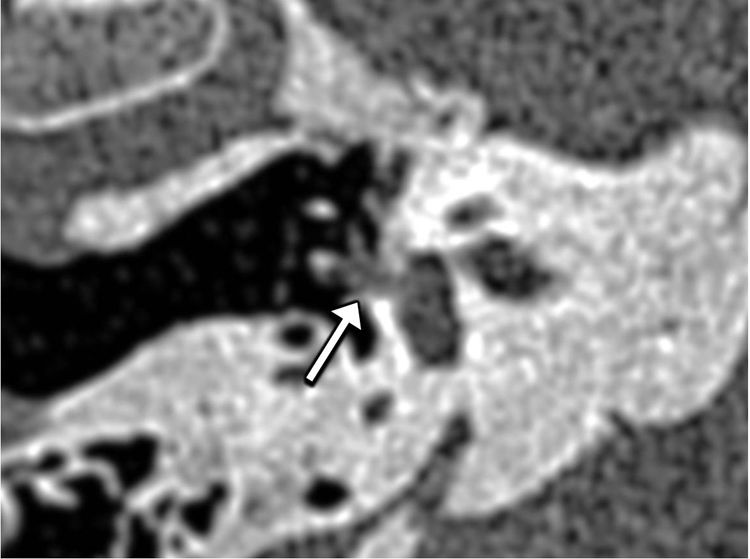
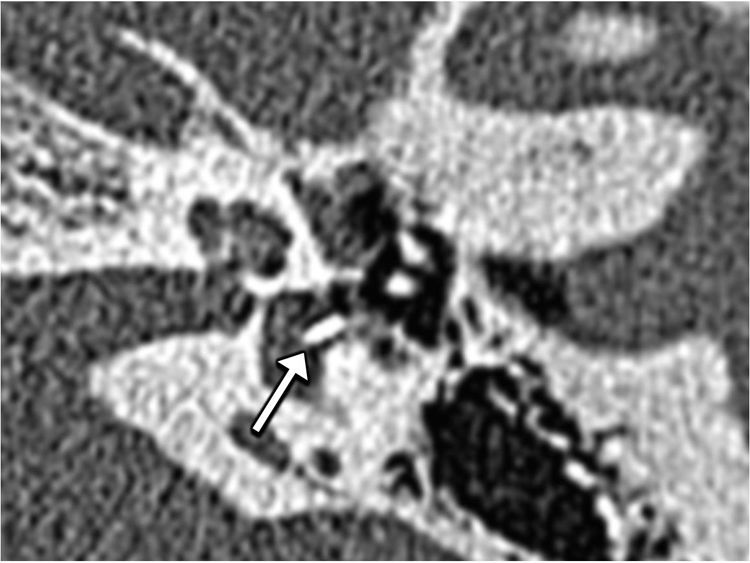
Granulation tissue. Transverse computed tomography imaging (A) and coronal reconstruction (B) in a patient who underwent tympanoplasty and partial ossicular chain reconstruction (arrow) showing dense soft tissue partially occupying the mesotympanum and epitympanum (asterisk) encompassing the prosthesis. Transverse magnetic resonance imaging in a non-echo-planar DWI sequence (C) shows no diffusion restriction (arrows).
Prosthesis displacement: this is one of the main causes of hearing loss relapse;12 the position of the prosthesis is suitably assessed by CT (Fig. 5).
Full prosthesis displacement and granulation tissue. Transverse computed tomography imaging (A) and coronal reconstruction (B) in a patient who underwent a modified radical mastoidectomy and full ossicular chain reconstruction (arrow) showing displacement of the prosthesis which is at an inferior angle and is not in contact with the oval window. There is also granulation tissue occupying the mastoidectomy cavity and partially occupying the middle ear (asterisk).
Remember: CT is the initial imaging technique of choice in assessing surgical failure in COM. The aeration of the middle ear and the position of the prosthesis should be assessed.
Surgical failure in cholesteatoma and role of DWI in its follow-upApart from the complications associated with mastoidectomy and tympanoplasty that it has in common with surgery for COM, the main complication is residual and recurrent cholesteatoma.
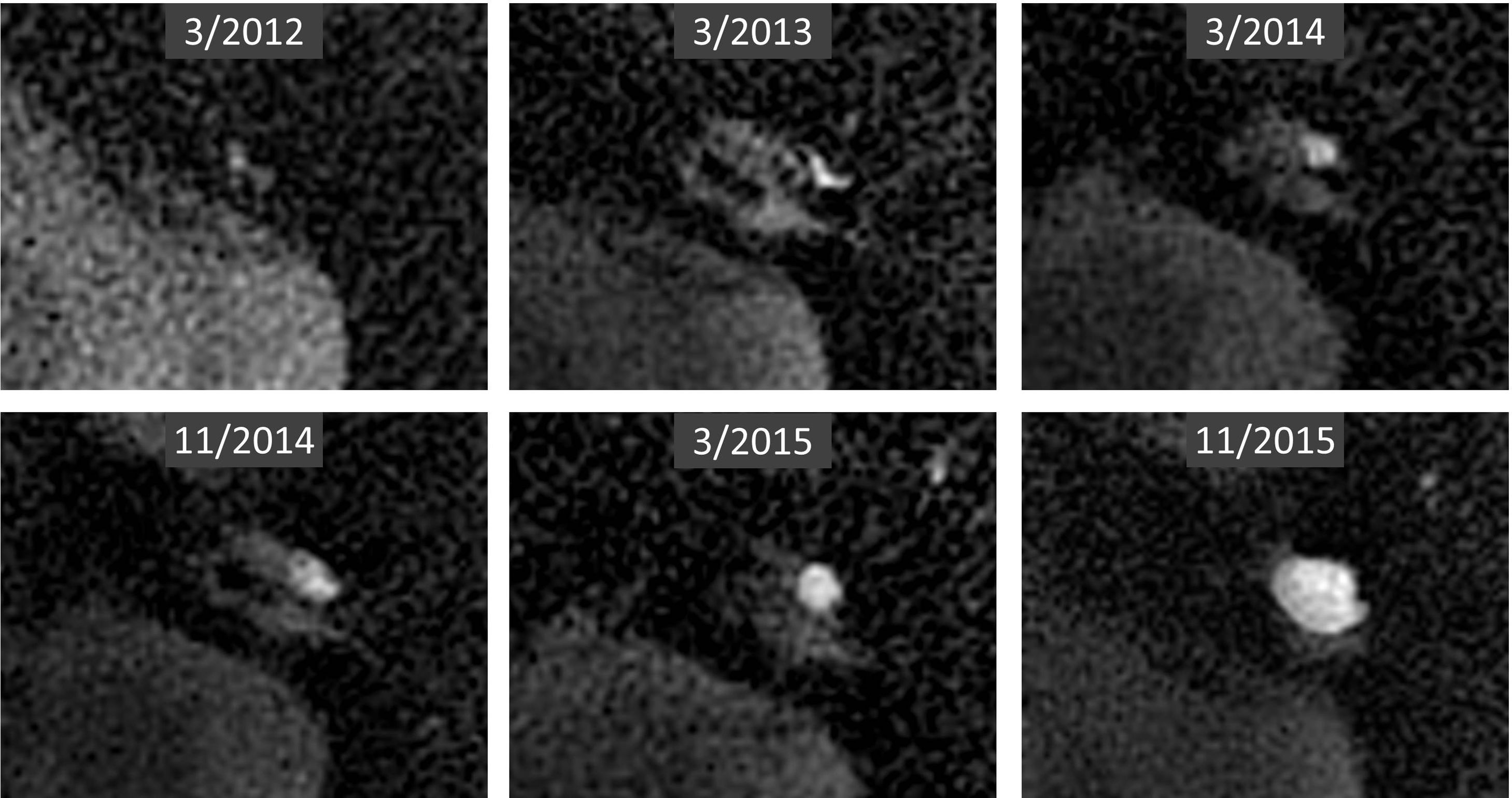
Closed mastoidectomy is associated with rates of residual and recurrent disease of 36% and 18%, respectively.4,5 This used to require surgery for review purposes 9–12 months later. That has been replaced with follow-up using non-echo-planar DWI, which enables detection of postoperative and recurrent disease, and surgery is now reserved exclusively for cases in which it is necessary.13
Remember: non-echo-planar DWI has replaced surgery for review purposes in the follow-up of patients who undergo surgery for cholesteatoma using a closed technique.
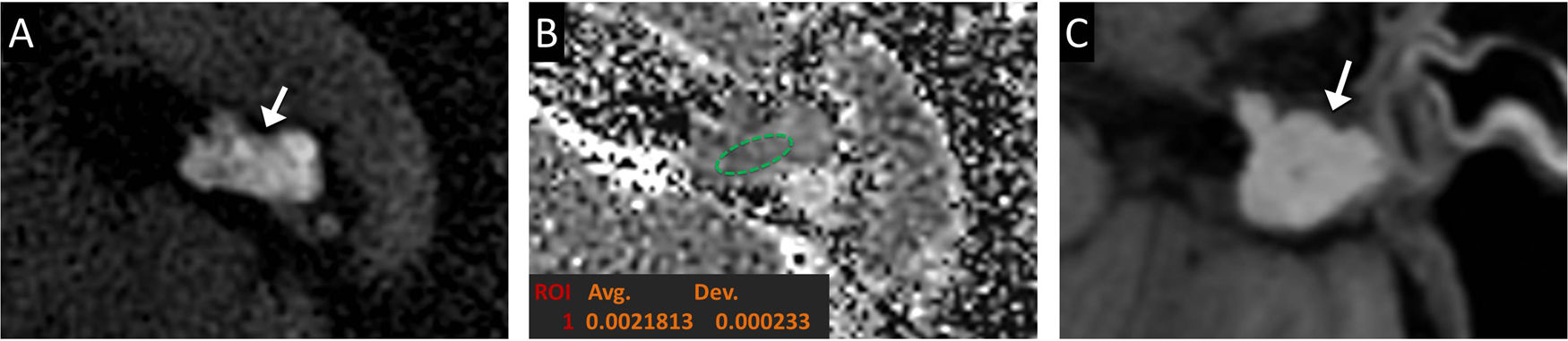
Due to its high keratin content, a cholesteatoma restricts diffusion, unlike other things that might occupy the postoperative cavity, such as granulation tissue, inflammation or fluid (Fig. 6). The non-echo-planar technique is used to reduce distortion due to air and bone susceptibility artefacts and increase spatial resolution.3 In addition, measuring the apparent diffusion coefficient improves specificity, with a sensitivity comparable to qualitative assessment.14 The main limitation of this technique is its ability to detect cholesteatomas measuring less than 3 mm, for which regular follow-up is recommended (Fig. 7).15 A wide variety of false positives have been reported; in order to improve diagnostic performance, the clinical context, surgery type and otoscopic findings should be assessed and the rest of the sequences should be evaluated (Fig. 8).15
Recurrent cholesteatoma. Transverse computed tomography imaging (A) in a patient who underwent a mastoidectomy for cholesteatoma showing full cavity occupation (asterisk). Transverse magnetic resonance imaging in a non-echo-planar DWI sequence (B) and apparent diffusion coefficient (ADC) map (C) showing a hyperintense focus of cholesteatoma (arrow) with diffusion restriction; ADC value 0.81 × 10−3 mm2/s.
Progressive growth of recurrent cholesteatoma. Transverse magnetic resonance imaging in a non-echo-planar DWI sequence over time (arrow in the upper part of each image) in a patient who underwent surgery for cholesteatoma using a closed technique showing progressive growth of recurrent cholesteatoma, with hyperintense tissue in DWI with diffusion restriction with low ADC values (not shown).
Cholesterol granuloma. Transverse magnetic resonance imaging in a non-echo-planar DWI sequence (A) and apparent diffusion coefficient map (B) in a patient who underwent surgery for cholesteatoma using a closed technique showing hyperintense tissue on DWI (arrow) with no diffusion restriction with ADC values of 2.18 × 10−3 mm2/s. A T1-weighted sequence (C) showing high signal intensity corresponded to a cholesterol granuloma.
In open mastoidectomy, the risk of residual and recurrent disease is lower, and in the majority of cases the cavity is accessible to direct inspection.3 However, DWI can be useful in evaluating cholesteatomas that spread to regions that cannot be assessed, such as the petrous apex or the mastoid process, in obliterated cavities or in opaque reconstructed tympanums.16
Surgical failure in otosclerosisSurgical failure occurs in approximately 5%–6% of cases.17 It is assessed by CT. In all cases, the attachment of the prosthesis, the condition of the ossicular chain, the position of the piston and the inner ear should be evaluated.
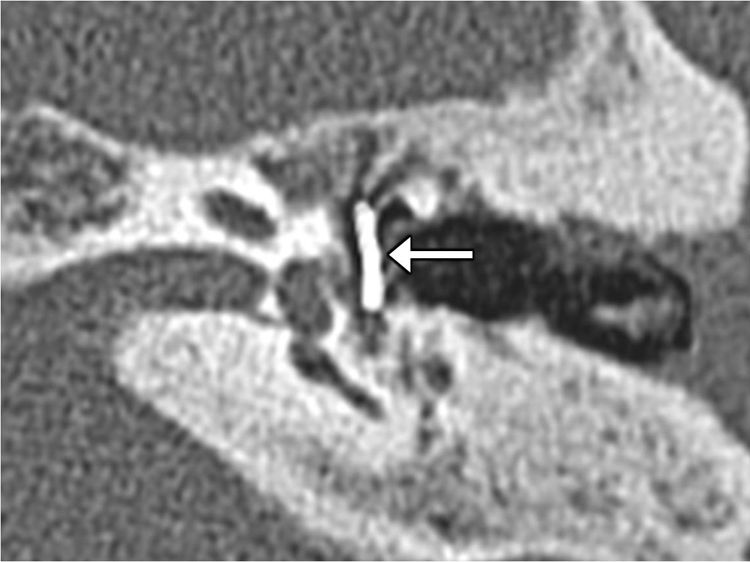
The most common cause is displacement of the prosthesis.18,19 It can luxate (Fig. 9), migrate or lateralise (lateralised piston syndrome) (Fig. 10). It should be borne in mind that the prosthesis need not be perfectly centred in the oval window and that slight insertion through the footplate is acceptable.1,20
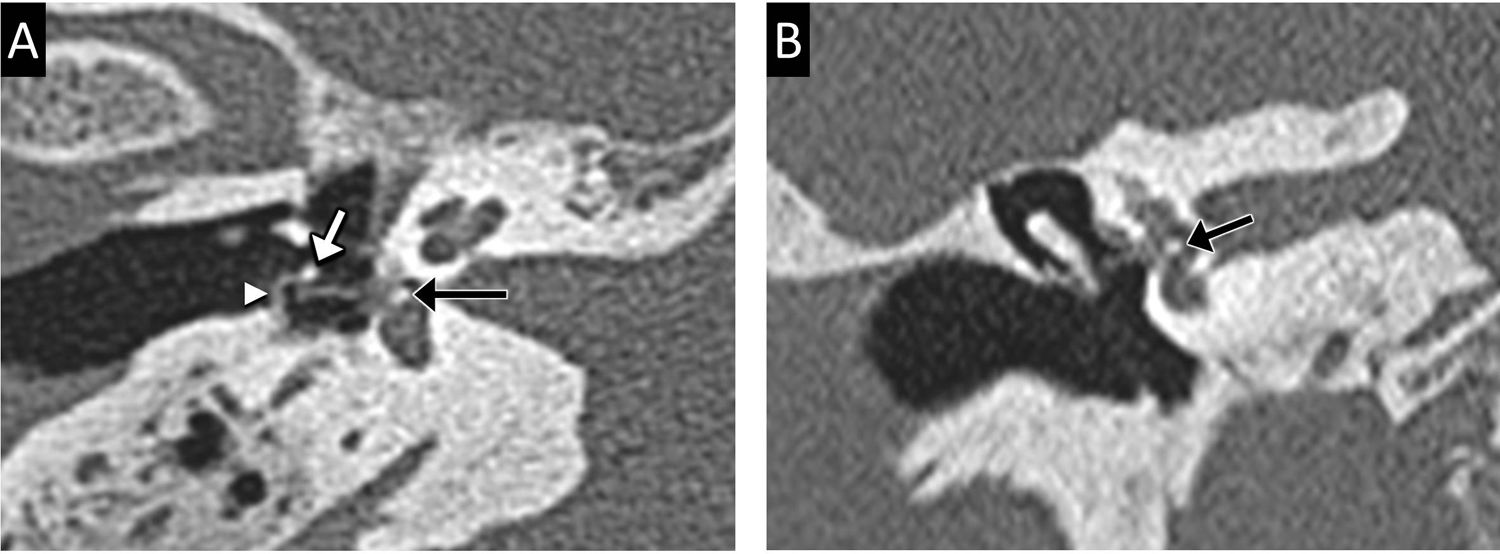
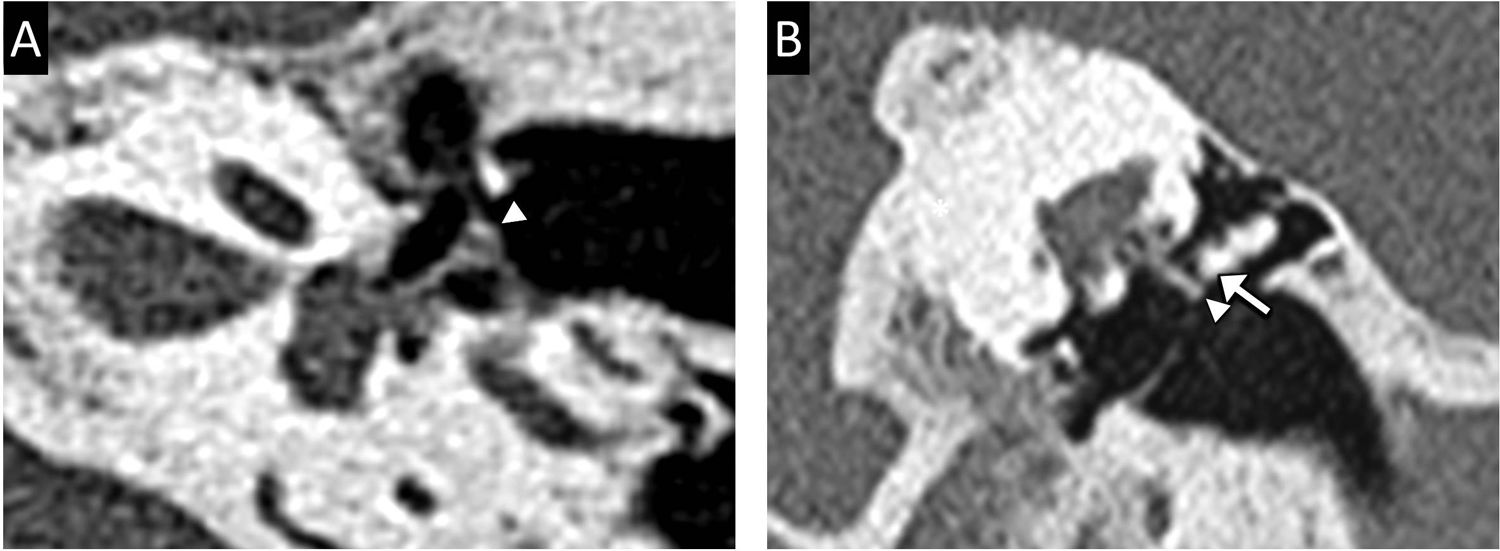
Other less common causes include detachment of the loop of the prosthesis from the long process of the incus (Fig. 11), necrosis of the long process of the incus due to an overly long prosthesis or insufficient mounting (Fig. 12), obliterative otosclerosis consisting of the formation of otospongiotic hypertrophic bone occupying the oval window niche and limiting prosthesis mobility (Fig. 13), and granulation tissue formation.18
Stapes prosthesis loop detachment and intravestibular foreign body. Transverse computed tomography imaging (A) and coronal reconstruction (B) showing a detachment of the loop of the prosthesis (arrow tip) from the long process of the incus (white arrow). An intravestibular foreign body of calcific density (black arrow) presumably corresponding to the footplate is also seen.
Causes of surgical failure that present with sensorineural hearing loss or vestibular syndromes include excessive intravestibular insertion of the piston, labyrinthitis, labyrinthine fistula, intravestibular foreign bodies and semicircular canal dehiscence (Figs. 11 and 14).18
Remember: the most common cause of failed stapes surgery is prosthesis displacement. It is assessed by CT.
ConclusionsThere is a wide variety of ME surgical procedures. This article has reviewed and illustrated its normal appearance on imaging. Knowledge of them will enable detection of possible complications in the majority of cases. CT allows assessment of postoperative cavity aeration and prosthesis position. DWI enables characterisation of tissues occupying the middle ear and is the tool to be used for the follow-up of patients having undergone cholesteatoma using a closed technique.
Authorship- 1
Responsible for study integrity: MM, EP.
- 2
Article conception: MM, EP, JCM, OJT, JCP.
- 3
Article design: MM, EP.
- 4
Data collection: MM, EP, JCM, OJT, JCP.
- 5
Data analysis and interpretation: not applicable.
- 6
Statistical processing: not applicable.
- 7
Literature search: MM, EP, JCM, OJT, JCP.
- 8
Drafting of the article: MM, EP, JCM, OJT.
- 9
Critical review of the manuscript with intellectually significant contributions: MM, EP, JCM, OJT, JCP.
- 10
Approval of the final version: MM, EP, JCM, OJT, JCP.
The authors declare that they have no conflicts of interest.
Please cite this article as: Mazón M, Pont E, Castellá-Malonda J, Jacome-Torres O, Carreres-Polo J. Valoración radiológica del oído medio operado. Radiología. 2021. https://doi.org/10.1016/j.rx.2021.04.005