Pseudotumor cerebri is a disorder characterised by increased intracranial pressure that predominantly affects obese young women. This paper aims to define the concepts of primary pseudotumor cerebri, in which the cause cannot be identified (also known as idiopathic intracranial hypertension), and secondary pseudotumor cerebri, in which the cause can be identified. We review the current role of imaging techniques in diagnosing pseudotumor cerebri and describe and illustrate the most characteristic imaging findings of the disorder, some of which are included in the diagnostic criteria proposed in 2013. We also consider the fundamental role of interventional radiology in the treatment of pseudotumor cerebri because placing a stent in stenosed venous sinuses is a novel treatment option in patients who are refractory to classical treatment. Finally, we describe the imaging biomarkers that have been evaluated for diagnosing primary pseudotumor cerebri and predicting the response to treatment.
El síndrome de pseudotumor cerebral (SPTC) es una alteración caracterizada por el aumento de presión intracraneal que afecta predominantemente a mujeres jóvenes obesas. El objetivo del trabajo es definir los conceptos de SPTC primario, sin causa identificable y denominado también hipertensión intracraneal idiopática (HII), y de SPTC secundario, con etiología identificable. Se revisa el papel actual de las pruebas de imagen en su diagnóstico y los hallazgos por imagen típicos del SPTC, algunos de los cuales se incluyen entre los criterios diagnósticos propuestos en 2013. También se remarca el papel fundamental de la radiología intervencionista en el tratamiento, puesto que la colocación de stent en las estenosis de senos venosos constituye una alternativa terapéutica novedosa en pacientes resistentes al tratamiento clásico. Por último, se describen aquellos biomarcadores de imagen que han sido evaluados para aproximar el diagnóstico de la HII y predecir la respuesta al tratamiento.
Pseudotumor cerebri syndrome (PTCS) comprises a set of signs and symptoms deriving from increased intracranial pressure (ICP) in the absence of focal lesions, hydrocephaly, infection and underlying malignancy. Cases in which no aetiology is identified are called idiopathic intracranial hypertension (IIH).1 This condition predominantly affects obese women of reproductive age. Its pathophysiology is complex and multifactorial; one probable cause is alteration of the homoeostasis of the cerebrospinal fluid (CSF). Imaging tests are essential in diagnosis as they enable causes of increased ICP to be ruled out and as some imaging findings are among the diagnostic criteria for PTCS proposed in 2013.2 In addition, neuroradiology plays an important role in the treatment of PTCS, since the intravascular approach via the percutaneous route to transverse vessel stenosis using angioplasty and stent placement constitutes a novel therapeutic alternative in patients resistant to classic treatment.3 Finally, various imaging biomarkers have been proposed to diagnose IIH and to measure treatment response.
The objective of this article is to review the current state of knowledge with regard to PTCS, discuss the imaging findings currently accepted as signs of IIH and describe the role of interventionist neuroradiology in treatment.
DefinitionPTCS is a syndrome defined by signs and symptoms derived from increased ICP in the absence of focal lesions and other identifiable causes.
It was formerly known as benign intracranial hypertension. Today, this nomenclature should be avoided, as 1%–2% of patients will go blind in the first year following diagnosis and up to 24% of patients present permanent vision loss.4 Currently, the terms used are idiopathic intracranial hypertension and pseudotumor cerebri. In 2013, the new term PTCS was proposed and a distinction was made between primary PTCS, with no identifiable cause (also called IIH), and secondary PTCS, with an identifiable aetiology.1
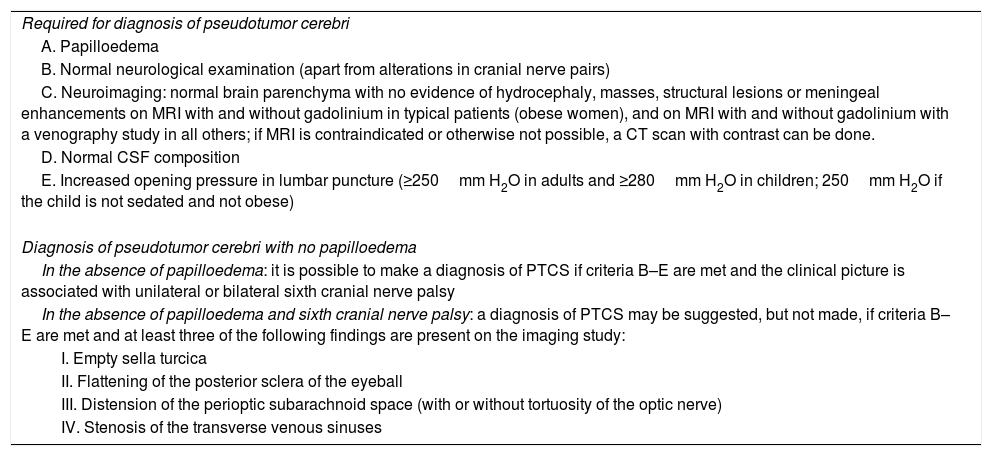
Diagnostic criteria in pseudotumor cerebri syndromeThe diagnostic criteria for PTCS have evolved between the first report of the corresponding clinical findings, by Dandy in 1937, and the proposal of the latest criteria, by Friedman et al. in 2013.1 The essential role of imaging tests is to rule out identifiable causes of intracranial hypertension. However, radiological findings are included among the most recently proposed diagnostic criteria. In the absence of papilloedema and sixth cranial nerve palsy, a diagnosis of IIH may be suggested based on a combination of imaging findings and clinical criteria1 (Table 1).
Diagnostic criteria for pseudotumor cerebria
| Required for diagnosis of pseudotumor cerebri |
| A. Papilloedema |
| B. Normal neurological examination (apart from alterations in cranial nerve pairs) |
| C. Neuroimaging: normal brain parenchyma with no evidence of hydrocephaly, masses, structural lesions or meningeal enhancements on MRI with and without gadolinium in typical patients (obese women), and on MRI with and without gadolinium with a venography study in all others; if MRI is contraindicated or otherwise not possible, a CT scan with contrast can be done. |
| D. Normal CSF composition |
| E. Increased opening pressure in lumbar puncture (≥250mm H2O in adults and ≥280mm H2O in children; 250mm H2O if the child is not sedated and not obese) |
| Diagnosis of pseudotumor cerebri with no papilloedema |
| In the absence of papilloedema: it is possible to make a diagnosis of PTCS if criteria B–E are met and the clinical picture is associated with unilateral or bilateral sixth cranial nerve palsy |
| In the absence of papilloedema and sixth cranial nerve palsy: a diagnosis of PTCS may be suggested, but not made, if criteria B–E are met and at least three of the following findings are present on the imaging study: |
| I. Empty sella turcica |
| II. Flattening of the posterior sclera of the eyeball |
| III. Distension of the perioptic subarachnoid space (with or without tortuosity of the optic nerve) |
| IV. Stenosis of the transverse venous sinuses |
PTCS: pseudotumor cerebri syndrome. CSF: cerebrospinal fluid.
The diagnosis is definitive if the patient meets criteria A–E.
The diagnosis is probable if the patient meets criteria A–D but the CSF pressure measured is lower than that specified for a definitive diagnosis.
The pathophysiology of this syndrome is multifactorial and not well-defined. Most current theories are centred on altered CSF homoeostasis due to increased resistance to CSF outflow/reabsorption and on altered venous haemodynamics.4
CSF absorption depends on the pressure gradient between the venous system and the subarachnoid space, such that increased brain venous pressure requires increased CSF pressure to maintain the absorption rate.4 The altered venous haemodynamics hypothesis is backed by the fact that dural venous sinus thrombosis causes signs and symptoms similar to those identified in patients with IIH.5
Other proposed factors are increased brain volume, increased brain arterial pressure transmitted to capillaries and increased CSF production.
Primary PTCS is linked to other factors such as obesity and recent weight gain; approximately 70% of patients with IIH are obese and approximately 90% are overweight.6 Secondary PTCS, meanwhile, has been linked to identifiable causes and aggravating factors: venous and/or cerebral alterations (thrombosis of venous sinuses or jugular veins and right heart overload), drugs (antibiotics such as tetracycline, vitamin A and retinoids), anaemia and endocrine alterations (Addison's disease and hypoparathyroidism).1
EpidemiologyThe concept of the typical patient is rooted in IIH, since more than 90% of affected individuals are women of reproductive age who are obese or have experienced recent rapid weight gain.4 The incidence rate is 12–20 cases/100,000 people in this group, whereas in the general population it is 1–2/100,000 people.4
Less often, PTCS may affect thin people, children, males and the elderly.1,7 Lower rates of obesity are identified in paediatric patients with IIH so, while the syndrome is more common in overweight adolescents, this does not constitute a risk factor in children under 10 years of age.7 There is also no difference between sexes prior to the onset of puberty.8 Less than 10% of affected adults are men; they are typically obese and have a worse prognosis with regard to vision than women.9
Signs and symptomsClassically, a diagnosis of IIH is considered for a symptom triad of headache, visual changes and papilloedema.10
The most common symptom is headache. More than 90% of patients experience this symptom, which is generally described as oppressive and appearing after waking up. Other patients have reported experiencing a throbbing migraine.2
Transient visual alterations, specifically vision loss lasting less than 60 seconds or following postural provocation, constitute the second most common symptom, reported in 70% of patients.2 Permanent loss of vision is the most serious complication in IIH, and in fulminant cases may occur less than a month from the onset of symptoms.11 Other reported visual alterations are reduced visual acuity or visual field and diplopia due to sixth cranial nerve palsy.10
Up to 95% of patients may present papilloedema, which may entail permanent vision loss in up to 1%-2% of patients without early treatment.4
Other commonly reported symptoms are tinnitus, throbbing, neck or back pain, nausea, and vomiting.11
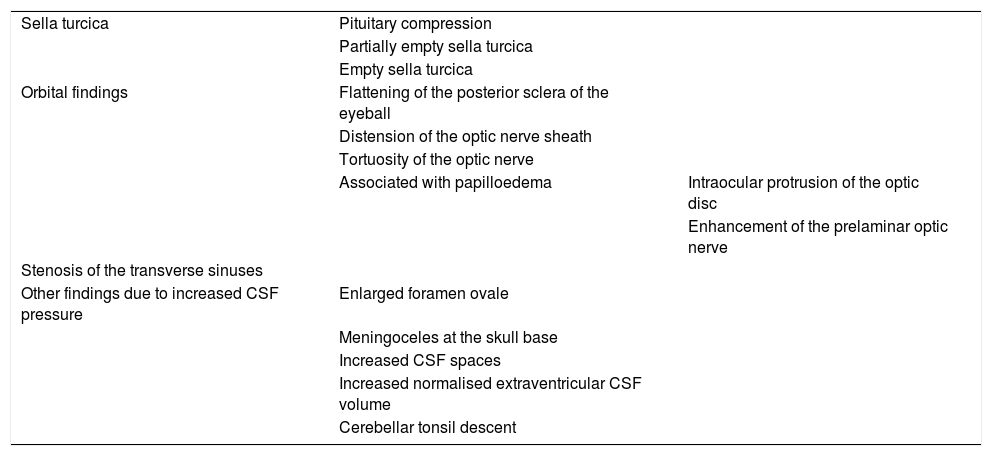
Radiological findings in pseudotumor cerebri syndromeThe primary purpose of imaging tests in IIH is to rule out diseases causing intracranial hypertension. However, various radiological findings have been reported in IIH with advances in neuroimaging, and some have been accepted as diagnostic criteria, as seen above. Radiological findings in PTCS are mainly characterised by their high specificity (>90%) and low sensitivity (Table 2).
Summary of radiological findings in pseudotumor cerebri syndrome.
| Sella turcica | Pituitary compression | |
| Partially empty sella turcica | ||
| Empty sella turcica | ||
| Orbital findings | Flattening of the posterior sclera of the eyeball | |
| Distension of the optic nerve sheath | ||
| Tortuosity of the optic nerve | ||
| Associated with papilloedema | Intraocular protrusion of the optic disc | |
| Enhancement of the prelaminar optic nerve | ||
| Stenosis of the transverse sinuses | ||
| Other findings due to increased CSF pressure | Enlarged foramen ovale | |
| Meningoceles at the skull base | ||
| Increased CSF spaces | ||
| Increased normalised extraventricular CSF volume | ||
| Cerebellar tonsil descent |
CSF: cerebrospinal fluid.
This is one of the most prevalent signs, seen in up to 80% of cases, with a specificity of approximately 70% and a low value if an isolated finding, as it is common in the general population.12
This radiological finding is secondary to prolonged pulsatility of high-pressure CSF filling the sella turcica and causing arachnoidocele through the sellar diaphragm.13 Some morphometric studies have suggested that the enlargement and remodelling of the sella turcica is the cause of the appearance of an empty sella.14
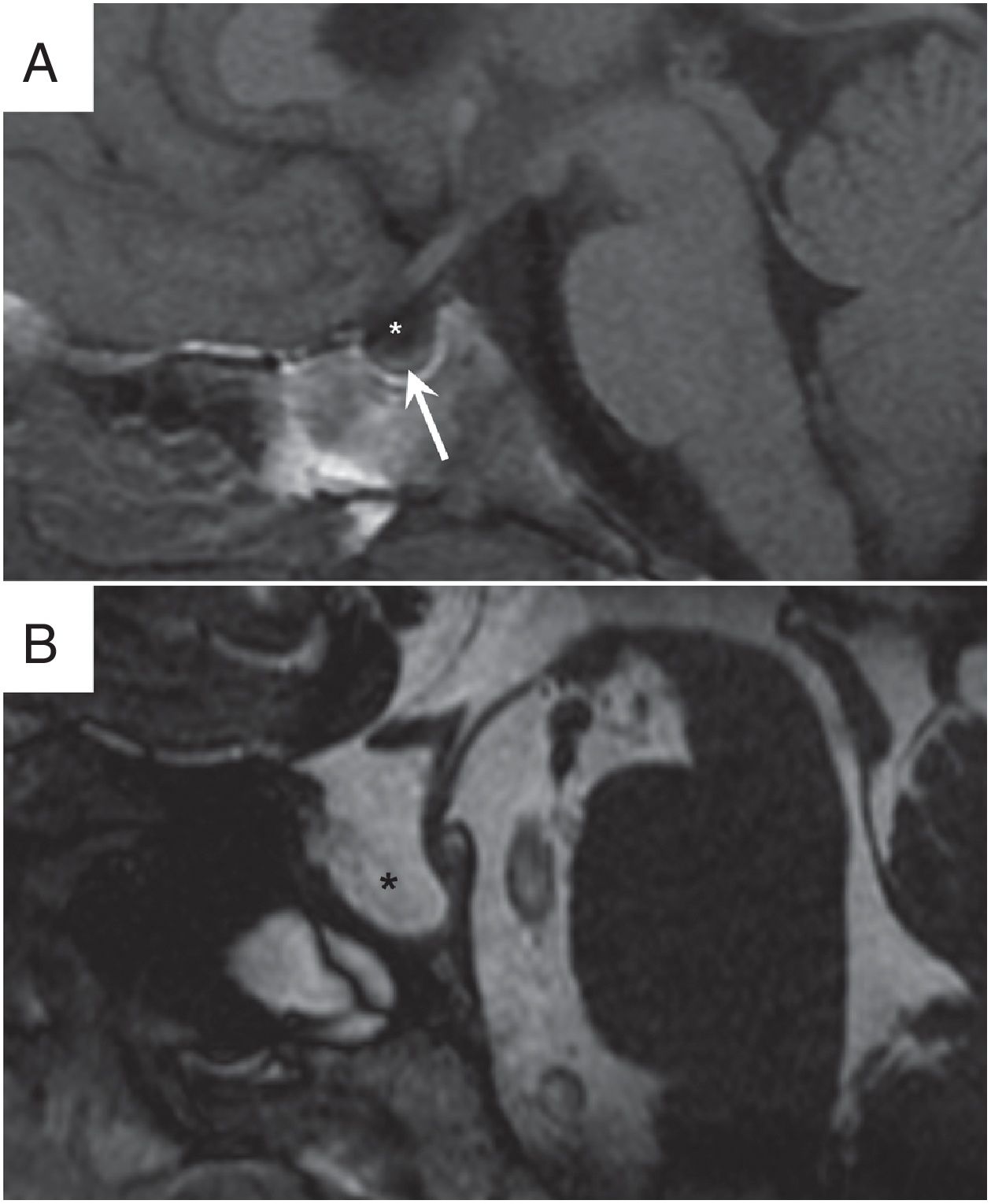
It may be seen, to varying degrees, on sagittal slices in magnetic resonance imaging (MRI) along the midline. The sella turcica is considered to be empty if it is found to be completely filled with CSF with the pituitary gland not visible, and to be partially empty when the majority is filled with CSF and the base of the pituitary gland is narrowed (Fig. 1).12,15
Radiological findings in the sella turcica.(A) Partially empty sella turcica, seen in sagittal turbo spin echo (TSE) T1 sequence. The typical characteristics are seen with the sella turcica almost completely filled with cerebrospinal fluid (CSF) (*) and the pituitary gland narrowed (arrow). (B) Empty sella turcica visualised in sagittal TSE T2 sequence. The sella turcica is seen to be remodelled, expanded and completely filled with CSF (*), with the pituitary gland not visible.
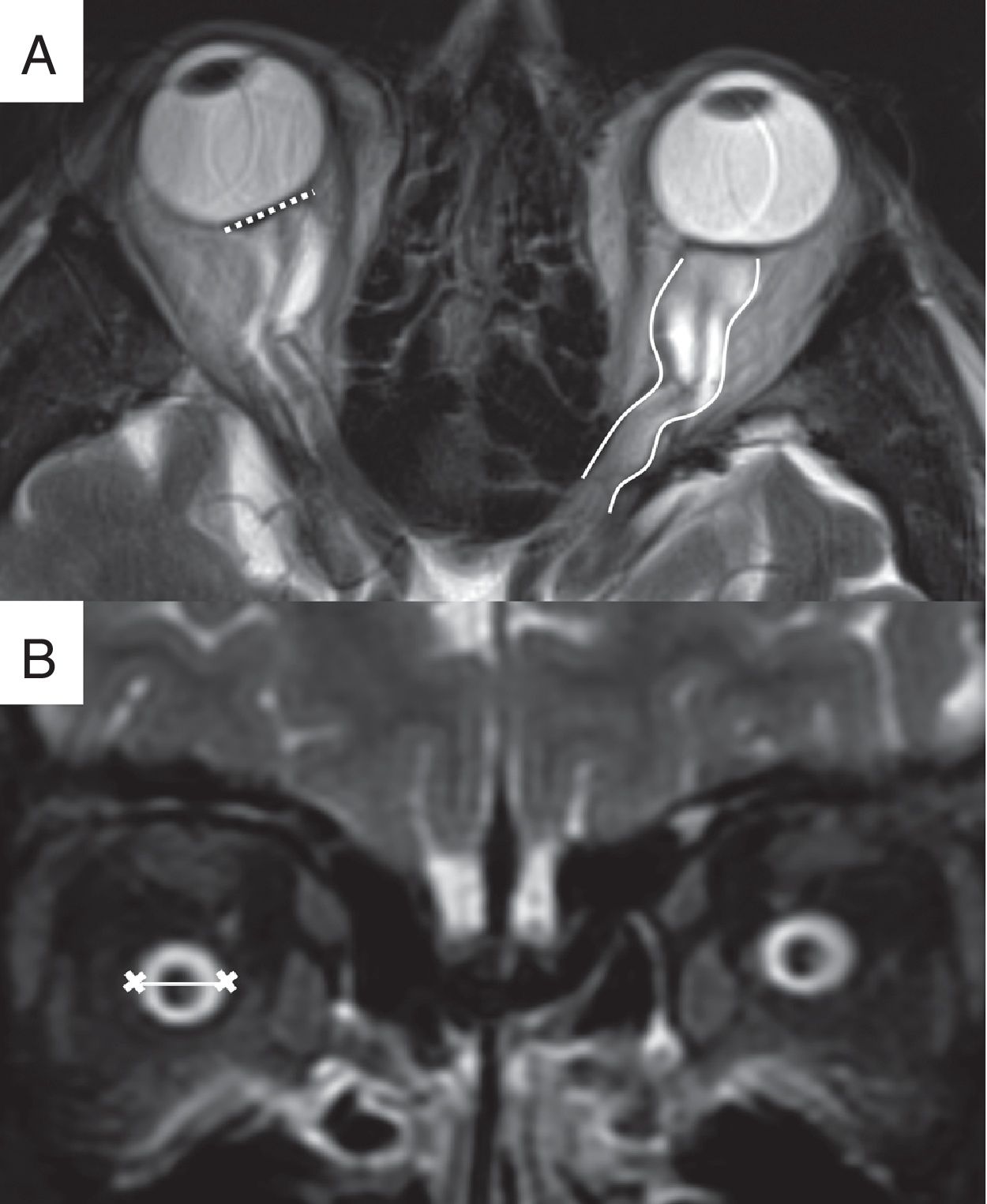
This is a very prevalent sign, with variable sensitivity and specificity close to 100% (Fig. 2).13,16 Determinations of the presence and degree of alteration of the eyeball are subject to marked inter-observer variability. Hence, automated measurement of eyeball distortion has been proposed to improve diagnostic precision.17
Orbital findings. (A) Magnetic resonance imaging (MRI), fast spin echo (FSE) T2 sequence on the transverse plane, showing distortion of the normal morphology of the eyeball with bilateral flattening of the posterior sclera (dotted line) as well as tortuosity of the optic nerves on the horizontal plane (solid lines). (B) MRI, short TI inversion recovery (STIR) sequence on the coronal plane, showing distension of the optic nerve sheath behind the eyeball (line).
In MRI, T2 sequences with fat saturation enable proper evaluation of the optic nerve (ON) sheath in the orbit.18 Patients with papilloedema present a mean ON sheath diameter, measured behind the eyeball, higher than in healthy patients (7.54±1.05mm versus 5.52±1.11mm) (Fig. 2).19,20 This finding has a sensitivity of 45%–66.7% and a specificity of 82.1%–95%, with a prevalence of 65%.14,21
Tortuosity of the optic nerveIn IIH, the attachment of the ON to the annulus of Zinn and the posterior sclera of the eyeball cause elongation and intraorbital tortuosity of the ON. Displacement may occur along the nerve's vertical or horizontal plane. Visualisation of the tortuosity of the ON has higher specificity on the vertical plane than on the horizontal plane (Fig. 2).18 This finding has a sensitivity of 40% and a specificity of 91%.21
Orbital findings associated with papilloedemaPapilloedema is characterised in the eye fundus by optic disc elevation, blurring of the optic disc margins, the presence of a peripapillary halo and venous distension, among other findings. It may be asymmetrical or unilateral.18
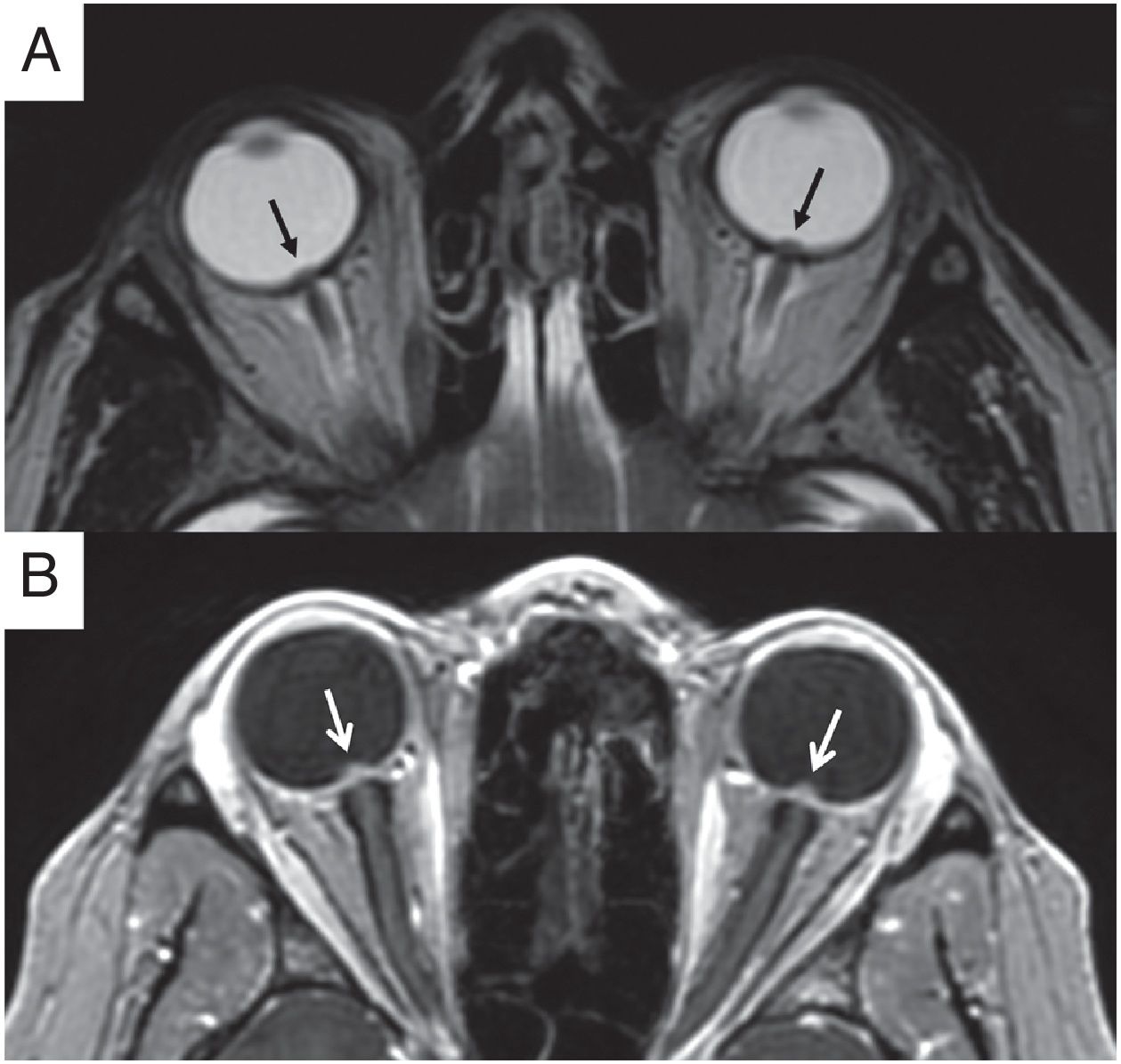
Intraocular protrusion of the optic discProtrusion of the optic disc has been seen in up to 67% of patients with PTCS (Fig. 3).22 It has a high positive predictive value for assessing papilloedema and the clinical grade thereof.17
Orbital findings associated with papilloedema. (A) Magnetic resonance imaging (MRI), FSE T2 sequence on the transverse plane. Bilateral intraocular protrusion of the optic disc (black arrows) is identified. (B) Same patient as in Image A. MRI, transverse 3D gradient T1 sequence with fat saturation following administration of intravenous contrast, showing bilateral, symmetrical enhancement in the prelaminar region of the optic nerves (white arrows).
The prelaminar region of the ON is a part of the intraocular portion of the head of the nerve supplied by the choroid vascular system. Its enhancement following contrast administration in MRI has a low sensitivity (50%) and a specificity of 100% (Fig. 3). It has been postulated that this enhancement results from flow difficulty with venous stasis in the choroid system due to intraocular protrusion of the optic disc. However, in many patients with IIH and marked papilloedema, prelaminar enhancement cannot be identified.13
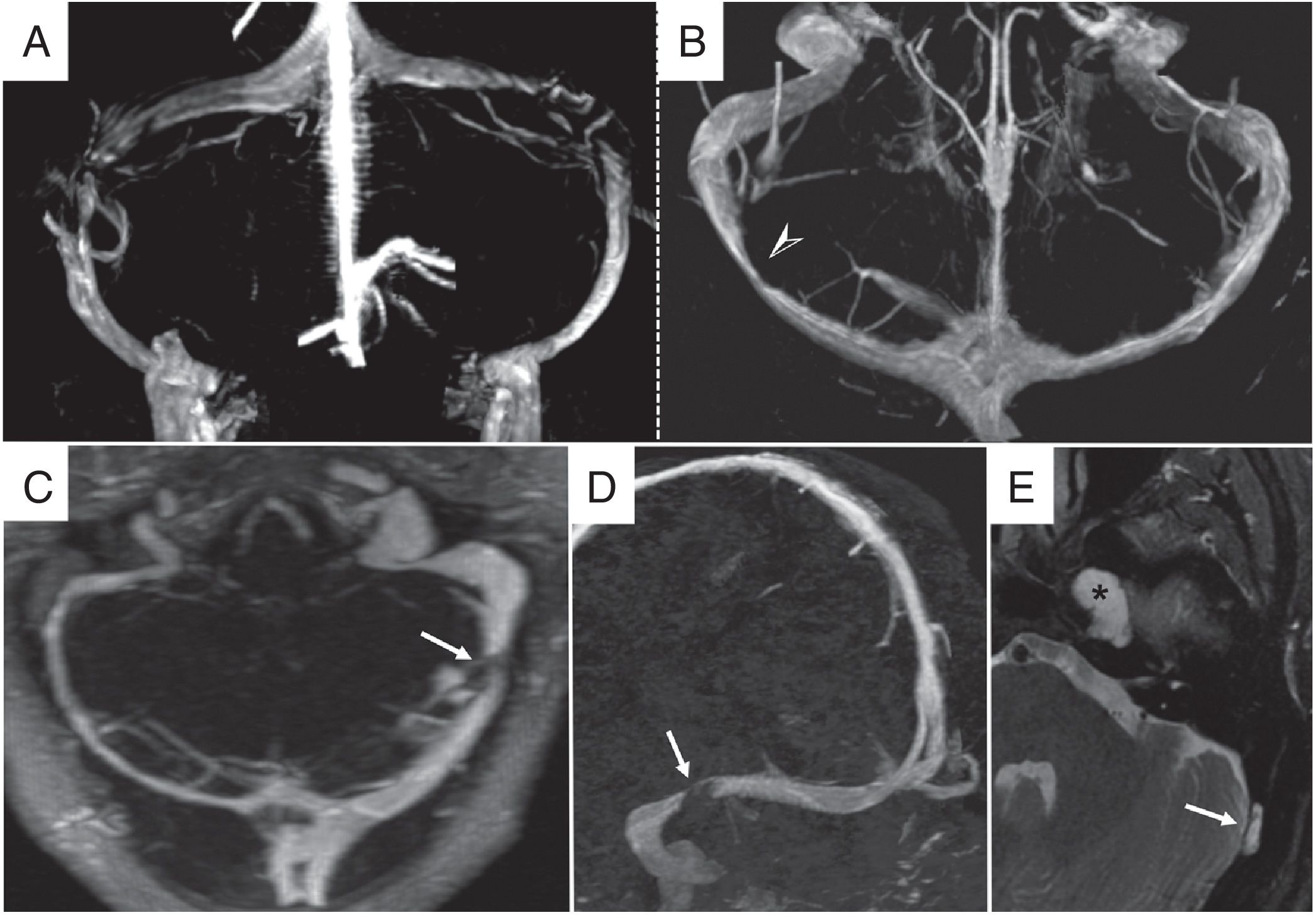
Stenosis of the transverse sinusesStenosis of the transverse sinuses has a prevalence of up to 90% in patients with IIH.5 The most common location is in the distal region of the transverse sinuses or at their junction with the sigmoid venous sinuses. It may be unilateral or bilateral (Fig. 4).23,24
Stenosis of the transverse sinuses. Venous MR angiography with contrast, coronal (A) and transverse (B) 3D volumetric reconstructions. (A, B) Extrinsic venous stenosis. A: typical bilateral stenosis in the distal region of the transverse sinuses. B: unilateral stenosis in the middle third of the right transverse sinus. (C–E) Intrinsic venous stenosis due to arachnoid granulation. C: venous MR angiography with contrast with maximum intensity projection (MIP) reconstruction on the transverse plane showing hypoplasia of the right transverse venous sinus and a significant small stenotic segment in the distal third of the left transverse sinus. D: MIP reconstruction on the parasagittal plane showing well-delimited stenosis borders (white arrow). E: transverse STIR sequence showing an arachnoid granulation causing stenosis (white arrow). A Meckel's cave meningocele (asterisk) associated with IIH can also be observed.
MRI venography with contrast and the auto-triggered elliptic centric-ordered imaging (ATECO) technique decreases signal loss due to artefacts compared to the classically used technique (time-of-flight MRI venography) and enables better detection of stenosis of the venous sinuses, with a sensitivity and a specificity of 93%.5 Stenosis of the venous sinuses may be intrinsic or extrinsic.
Intrinsic stenosis of the transverse sinusesThere have been reports of alterations in the venous sinuses that cause focal defects in intraluminal filling, result in intrinsic stenosis and could contribute to the onset of intracranial hypertension. These alterations include septa, arachnoid granulations and projections of the arachnoid matrix and the subarachnoid space in the wall of the dural venous sinuses.24 Arachnoid granulations have been reported in 24% of computed tomography (CT) scans and 13% of MRI studies with contrast in normal populations, and increase in number with age. They are often seen in the transverse and sigmoid sinuses.24,25
Extrinsic stenosis of the transverse sinusesThis consists of a stenosis of the lumen of the venous sinuses due to compression secondary to increased ICP, which causes a state of self-sustained venous collapse.2 This state is considered a cause and consequence of the increased ICP. CSF is passively reabsorbed through the perivenular spaces and in the arachnoid granulations towards the intracranial venous sinuses. Dominant transverse sinus stenosis or bilateral stenosis may impede venous drainage and cause venous hypertension. This hypertension impedes and reduces CSF absorption, causing increased ICP and even greater compression of the venous sinuses.2,3,26
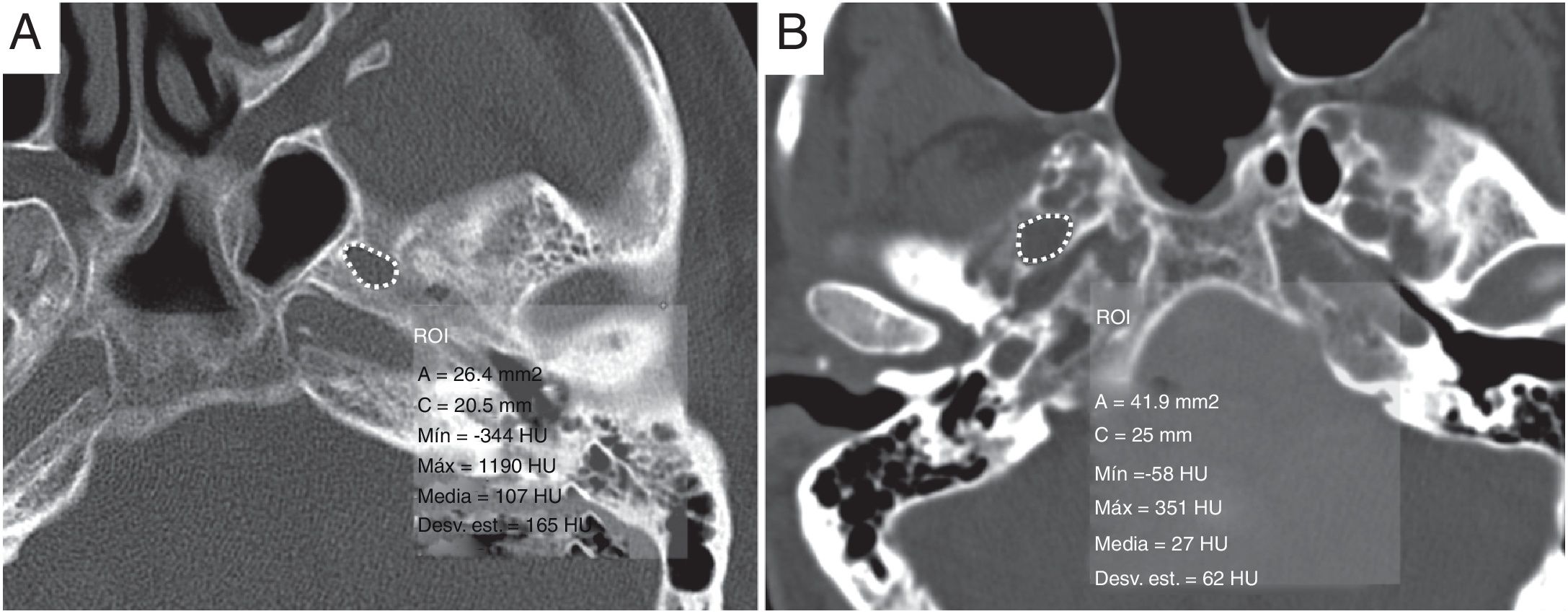
Other radiological findings associated with increased CSF pressureEnlarged foramen ovaleChronically high CSF pressure may cause bone remodelling and erosion. This finding is seen in cases of enlarged foramen ovale (FO). Mean FO area is greater in patients with IIH (Fig. 5). For a cut-off value of 30mm,2 the sensitivity of the FO area for detecting IIH is 50%, with a specificity of 81%. For a cut-off value of 40mm,2 the specificity and positive predictive value are 100%.15
Increased area of the foramen ovale. (A) Area of the foramen ovale on a computed tomography scan of the head without contrast in a healthy patient, with a value of 26.4mm.2 Compare this to a patient with idiopathic intracranial hypertension (B) in which the mean area of the foramen ovale is 41.9mm,2 exceeding 40mm.2
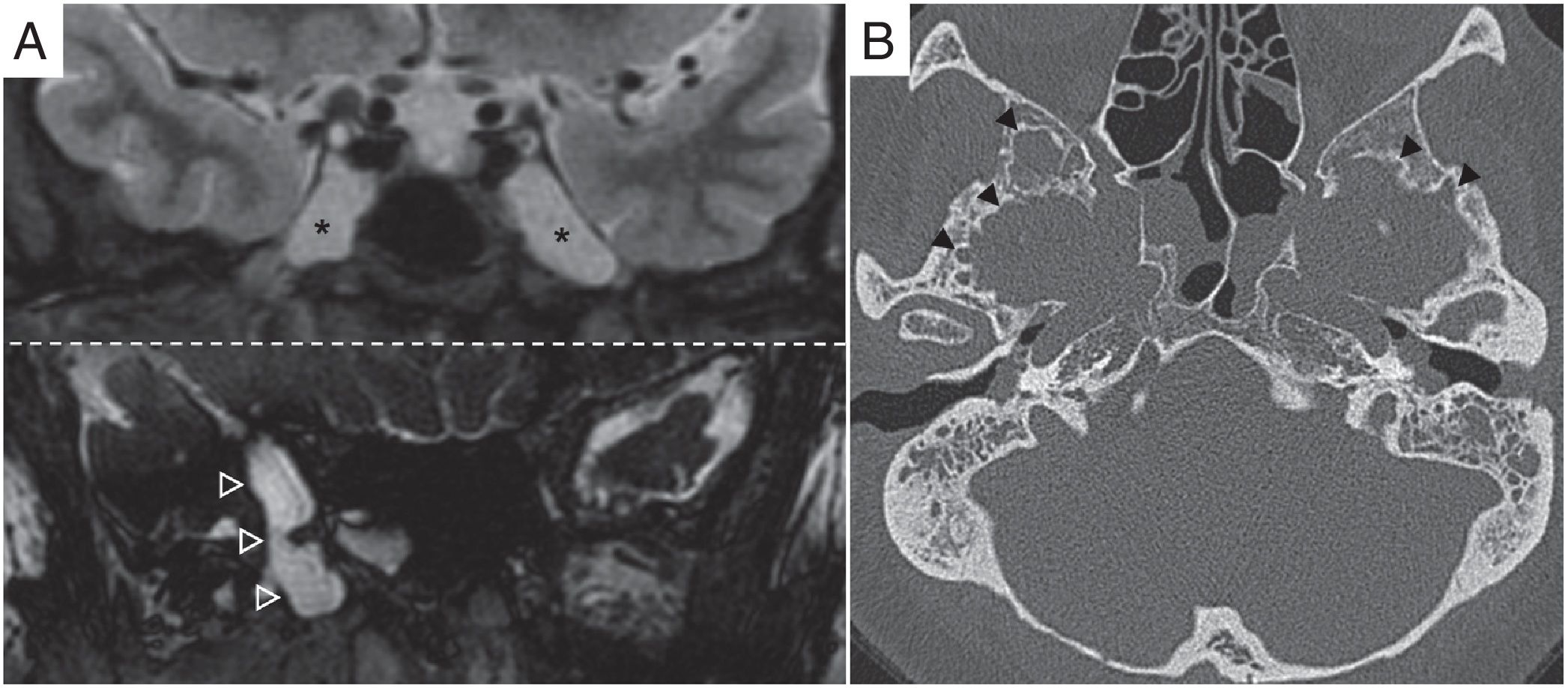
These may represent an additional sign of IIH on imaging.27 In 11% of patients with IIH, meningoceles have been identified in Meckel's cave or the petrous apex, and in 9%, increased Meckel's cave diameter has been identified (Fig. 6).28 Intraosseous arachnoid granulations in the rest of the skull base, predominantly in the sphenoid wings, have also been reported.29 CSF may leak through bone erosions and osteodural defects into the middle ear or the paranasal sinuses.12
Meningoceles and arachnoid granulations at the skull base. (A) Coronal STIR and coronal fast imaging employing steady-state acquisition (FIESTA) sequences showing Meckel's cave meningoceles (asterisks) and a meningocele located in the medial area of the right greater wing of the sphenoid bone (hollow arrow tips). (B) Computed tomography of the petrous apices, transverse image, showing multiple bone defects affecting the inner table of both sphenoid wings corresponding to intraosseous arachnoid granulations (black arrow tips).
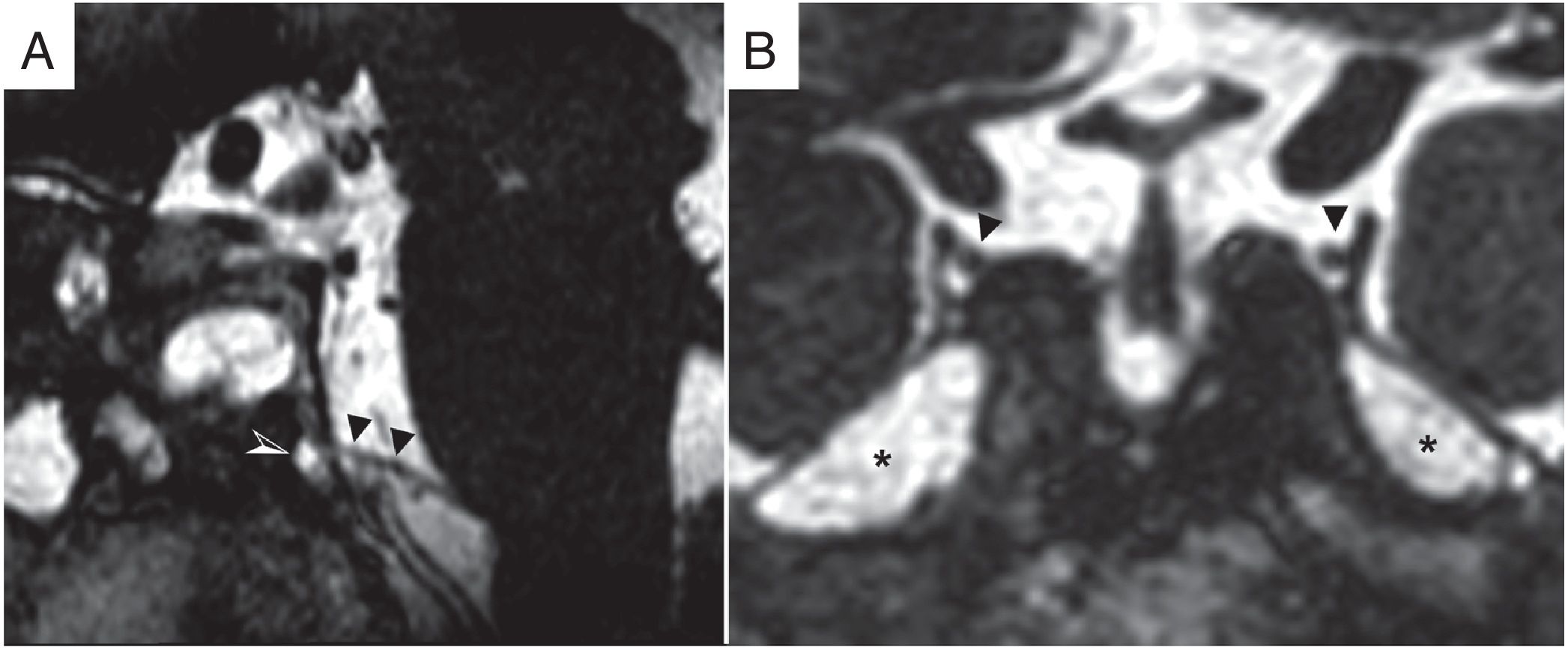
A bilateral and symmetrical increase in CSF spaces around cranial nerve pair III in the lateral wall of the laterosellar space or cranial nerve pair VI at the entrance to Dorello's canal have been documented (Fig. 7).27 More studies are needed to evaluate its actual diagnostic value.
Increased cerebrospinal fluid (CSF) spaces. (A) Fast imaging employing steady-state acquisition (FIESTA) balanced sequence on the sagittal plane in a patient with IIH. The filling of the dural canal of the sixth cranial nerve (Dorello's canal) with CSF is seen (white and black arrow tip). (B) FIESTA sequence coronal image with a bilateral and symmetrical increase in CSF spaces (asterisks) around the dural canals of the third cranial nerve (black arrow tips) in the lateral wall of the laterosellar space. A Meckel's cave meningocele (asterisk) associated with IIH was also identified.
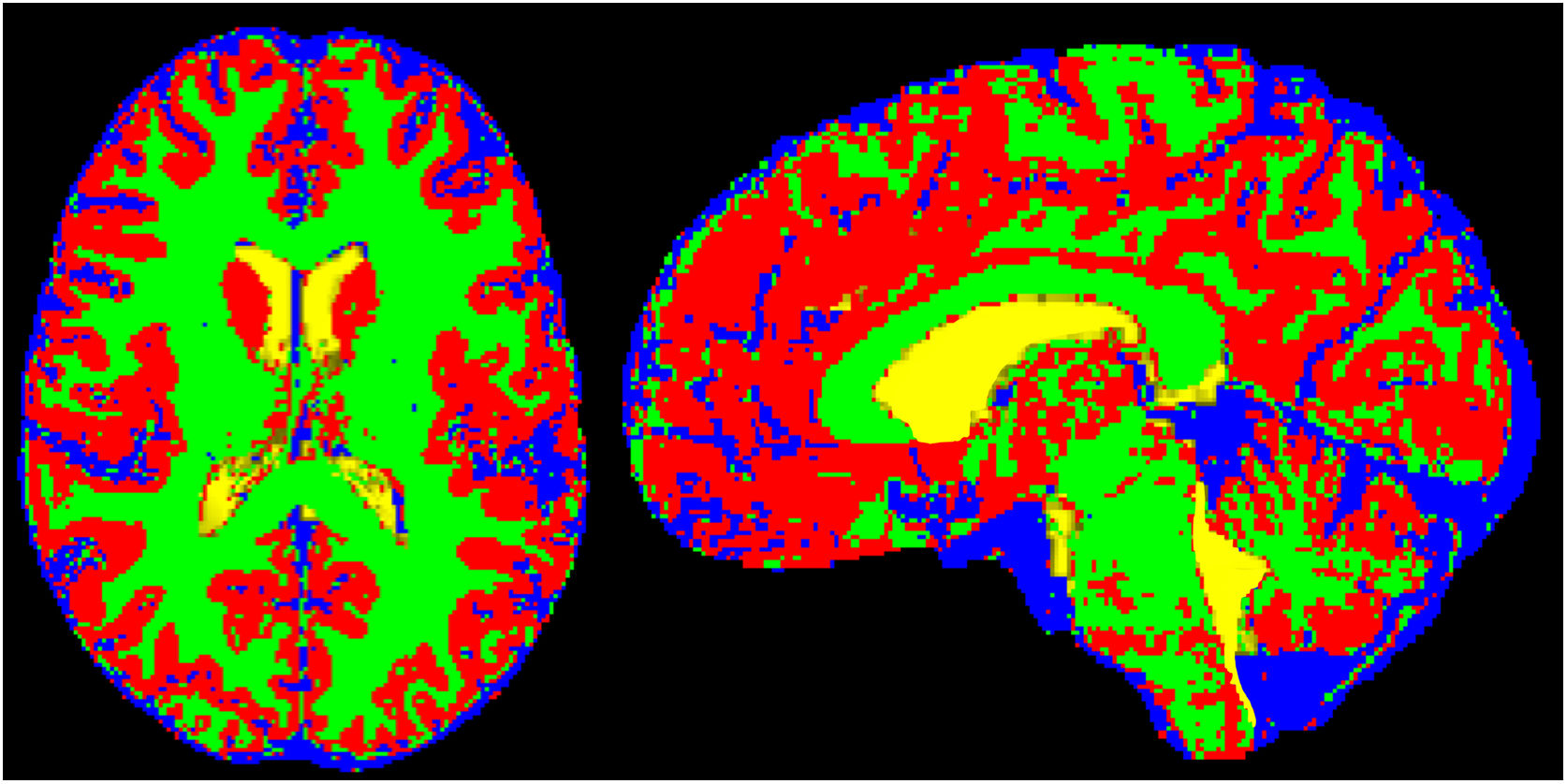
Measurement of extraventricular intracranial CSF volume has been proposed as a useful finding for establishing a diagnosis of IIH (Fig. 8). Alperin et al. identified an increase in this normalised volume compared to the total intracranial volume, with a cut-off point of more than 18%, as a radiological finding with a sensitivity of 73% and a specificity of 100%.30
Increased normalised extraventricular cerebrospinal fluid (CSF) volume. Example of semi-automated segmentation of intracranial extraventricular CSF distinguishing intraventricular CSF (yellow) from extraventricular CSF (blue). Grey matter and white matter segmented and distinguished using other colours (red and green, respectively).
Cerebellar tonsil descent or ectopia through the foramen magnum, defined as a descent greater than 5mm, has a significant incidence of between 10% and 21% in patients with IIH. Given this radiological finding in an appropriate clinical context, other radiological signs of IIH should be assessed to rule out conditions characterised by cerebellar tonsil descent, especially a type 1 Chiari malformation (there is also scientific evidence of concomitance of this and IIH) and intracranial hypotension syndrome.31
Imaging biomarkersVarious imaging biomarkers for diagnosing and treating IIH as well as predicting treatment response have been reported. Most studies have analysed markers that categorically determine the presence or absence of IIH, such as increased sella turcica area,14,32 increased foramen ovale area15 and increased extraventricular CSF.28,33 Various studies have advocated for automated measurements, such as making maps of the distance from the eyeball to measure the flattening of the posterior sclera17 and semi-automated quantitative assessment on MRI venography of the degree of stenosis of the transverse sinuses.34 However, studies published to date have low levels of scientific evidence, and the imaging biomarkers proposed have been neither shown to be clinically useful nor validated. Changes on imaging following treatment (acetazolamide or lumbar puncture) have also been evaluated in three of the proposed biomarkers: increased pituitary gland area, flattening of the posterior sclera and decreased extra-cerebral space. At present, none of them enables prediction of treatment response and none aids in deciding whether or not to treat, or in selecting the best treatment option.
TreatmentPTCS is a syndrome in which signs and symptoms vary widely from patient to patient. Thus, there is no single therapeutic approach. Each patient's management should be personalised according to that patient's clinical signs and symptoms, and each patient should be cared for by a multidisciplinary team. The main objective of IIH treatment is to relieve symptoms, restore visual acuity and prevent the progression of vision loss.33
LifestyleThe initial treatment measure in IIH is weight loss (5%-10%) for reversal of signs and symptoms.6 Treatment may range from strict dieting to bariatric surgery.35
Medical treatmentAcetazolamide is the most commonly used drug in medical treatment, and the only one with level A evidence for the treatment of patients with IIH and mild vision loss.33 It decreases CSF pressure and the degree of papilloedema as it inhibits expression of carbonic anhydrase by the choroid plexuses. It results in visual field improvements and better scores on quality of life scales compared to placebo.36 Multiple other drugs have been used, such as topiramate and furosemide.
SurgeryIn patients resistant to medical treatment of IIH with progressive acute vision loss (fulminant IIH), it may be necessary to resort to surgical treatment options intended to decrease ICP by shunting CSF. These options are optic nerve sheath fenestration, CSF shunting (lumboperitoneal or ventriculoperitoneal shunting) and stent placement in the venous sinuses. At present, there is no strong scientific evidence showing one of these techniques to be superior to the others.37
Optic nerve sheath fenestrationThis is the procedure of choice for patients with IIH resistant to medical treatment who present serious vision loss yet limited headache symptoms.11 It consists of fenestrating the retrobulbar ON sheath in order to drain CSF. However, complications have been reported in 26% of patients, and treatment failure with a need for repeat surgery has been reported in approximately 14.9%-31% of cases.38
Cerebrospinal fluid shuntingRepeat lumbar punctures may decrease ICP and reduce symptoms. This treatment is usually a temporary measure until a definitive procedure is performed to decrease CSF pressure, such as ventriculoperitoneal shunting (VPS) or lumboperitoneal shunting (LPS).39 In recent years there has been a trend towards greater use of VPS, although there is still uncertainty as to which is the better of these two techniques. Both procedures yield good percentages of improvement in visual field and acuity, headache and papilloedema.38 However, there are high failure rates with a need to review the procedure and perform repeat surgery in around 38% of cases of LPS and 41% of cases of VPS.38
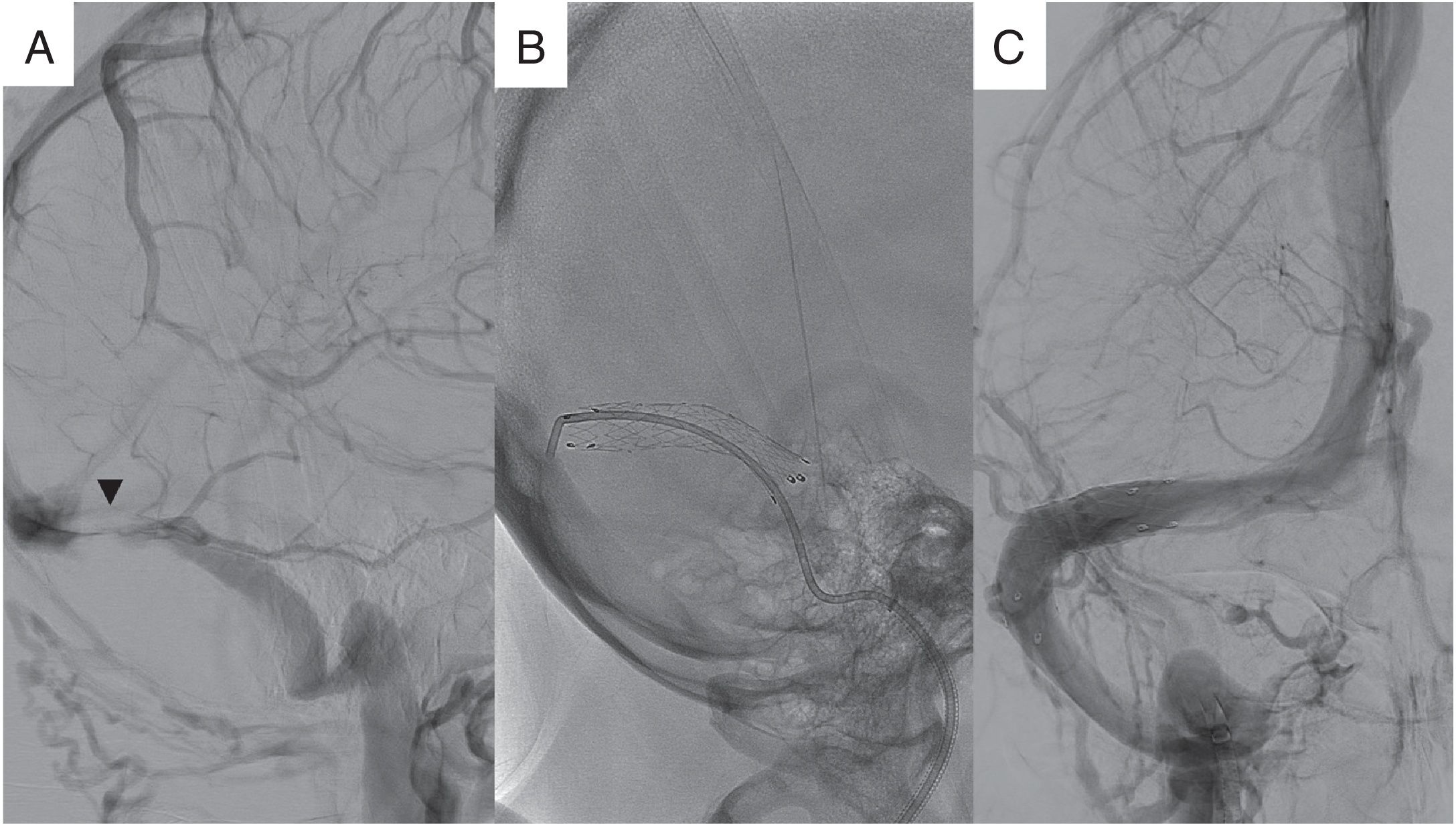
Stent placement in brain venous sinusesTreatment with a stent in IIH to resolve stenosis of the venous sinuses is based on the vascular/venous theory of its pathophysiology. Opening of the stenosis by the stent would disrupt the state of self-sustained venous collapse by reducing intracranial venous hypertension and improving CSF absorption (Fig. 9).33 It has demonstrated a high level of technical success and good clinical outcomes, with improvement of headache, papilloedema and visual acuity.9
Stent treatment of stenosis of a venous sinus. Digital venography imaging. (A) Image on the sagittal plane and digital bone subtraction identifying a stenotic segment in the left transverse sinus (arrow head). (B) Venography image without digital subtraction showing the release of the stent in the stenotic region. (C) Venography with digital subtraction showing the end result. Transverse sinus of a preserved calibre identifying a normal calibre with passage of contrast through the stent. Courtesy of Dr Jordi Blasco Andaluz, Hospital de la Santa Creu i Sant Pau, Barcelona.
The aim of this technique is to normalise the pre- and post-stenosis pressure gradient. Initially retrograde cerebral venography must be done with manometry to evaluate this gradient. There is no consensus with regard to the pressure gradient value that must be present for this treatment to be indicated, although there is evidence that the greater the difference between the pre- and post-stenosis pressures, the better the clinical outcome. Following stent implantation, manometry is repeated to assess the extent to which the gradient has decreased. It has been reported that the greater the difference between the pressure gradients before and after stent implantation, the more favourable the clinical outcome.33 Balloon angioplasty has not yielded good outcomes, with high rates of recurrence of stenosis.11
The main indication for stent placement in the venous sinuses is IIH that is resistant to medical and surgical treatment. There have also been studies where the initial indication was intolerance to medical treatment, or fulminant IIH.40
Various studies have evaluated outcomes following this procedure. A systematic review of the literature conducted by Kalyvas et al.38 included 11 studies and a total of 155 patients, 80.3% of whom had been treated with stent placement as an initial treatment option. It found papilloedema improvement in 98% of cases, visual acuity improvement in 65% of cases and visual field improvement in 75% of cases. Headache, meanwhile, improved in 77% of cases and worsened in just 2% of cases. CSF pressure normalised in all patients studied. Recurrence of symptoms occurred in 8%.
Notable among complications was transient headache following treatment, with a frequency of 12%.38 Cases of stent restenosis, subdural haematomas and other complications deriving from the procedure, such as pseudoaneurysm at the puncture site, have been reported.11,34
Regarding prognostic factors, a worse clinical course has been reported in young patients (mean age 30 years) and elevated CSF opening pressure, with higher rates of stent revision in patients with obesity.34
ConclusionPTCS is characterised by signs and symptoms deriving from increased ICP in the absence of an identifiable aetiology. Imaging tests in diagnosis are aimed at identifying causes of increased ICP. However, some imaging findings are accepted as signs of IIH with a high specificity and a low sensitivity: findings in the sella turcica, orbital findings associated or not associated with papilloedema and stenosis of the transverse vessels, among others. The radiologist should be familiarised with the imaging of this syndrome, since some of these signs are included in the diagnostic criteria for PTCS proposed in 2013. Treatment objectives in PTCS are to preserve vision and manage symptoms such as headache in order to improve quality of life. Personalised management of each patient enables the treatment to be adapted. Neuroradiology plays an important role in the latter regard, since the intravascular approach via the percutaneous route to transverse vessel stenosis using angioplasty and stent placement constitutes a novel therapeutic alternative with good outcomes. Finally, various imaging biomarkers have been proposed to diagnose IIH and to measure treatment response with a low level of evidence at present. Therefore, the role of the radiologist is essential both for diagnosis and for interventionist management. In the future, it will be useful to conduct prospective studies so as to acquire more extensive experience with and knowledge of this disease.
Authorship1. Responsible for the study's integrity: DVC, JCP.
2. Study concept: JCP.
3. Study design: DVC, JCP.
4. Data acquisition: DVC, JCP.
5. Data analysis and interpretation: DVC, JCP.
6. Statistical processing: not applicable.
7. Literature search: DVC, JCP.
8. Drafting of the study: DVC, JCP.
9. Critical review of the manuscript with intellectually significant contributions: DVC, JCP.
10. Approval of the final version: DVC, JCP.
- 1.
PTCS comprises a set of signs and symptoms deriving from increased ICP in the absence of focal lesions, hydrocephaly, infection and underlying malignancy. Cases in which no aetiology is identified are called IIH.
- 2.
The essential role of imaging tests is to rule out identifiable causes of intracranial hypertension. However, radiological findings are included among the most recently proposed diagnostic criteria. In the absence of papilloedema and sixth cranial nerve palsy, a diagnosis of IIH may be suggested based on a combination of imaging findings and clinical criteria.
- 3.
Radiological findings in PTCS are primarily characterised by their high specificity and low sensitivity.
- 4.
Each patient's management should be personalised according to that patient's clinical signs and symptoms, and each patient should be cared for by a multidisciplinary team. The main objective of IIH treatment is to relieve symptoms and preserve vision.
- 5.
Stent placement in the transverse sinuses has demonstrated a high level of technical success and good clinical outcomes, with improvement of headache, papilloedema and visual acuity.
The authors declare that they have no conflicts of interest.
We would like to thank Dr Fernando Aparici Robles, Head of the Neuroradiology Unit at Hospital Universitari i Politècnic La Fe de València, for his role in the critical review of the manuscript, and Dr Juan Delgado Moraleda for his work on the semi-automated segmentation of cerebral extraventricular CSF.
Please cite this article as: Veiga-Canuto D, Carreres-Polo J. Papel de la radiología en el síndrome de pseudotumor cerebral. Radiología. 2020;62:400–410.