The tensor fascia lata is a muscular structure that forms part of the lateral portion of the pelvis and proximal thigh. Because conditions affecting this muscle have not been widely reported and are relatively unknown, hypertrophy and pseudo-hypertrophy of the tensor fascia lata, although relatively common imaging findings, often go undiagnosed; instead, radiologists perform the differential diagnosis with more complex and more dangerous conditions. This article aims to review the anatomic and functional characteristics of the tensor fascia lata, going into detail about the radiological description of this muscle and pathological conditions that can affect it, as well as reviewing the relevant literature.
El músculo tensor de la fascia lata es una estructura muscular que forma parte de la porción lateral de la pelvis y del muslo proximal. La patología de este músculo no es bien conocida y descrita en la literatura. Por el contrario, la hipertrofia y la seudohipertrofia del músculo tensor de la fascia lata son hallazgos por imagen relativamente frecuentes que a menudo no se diagnostican y entran en un diagnóstico diferencial con patologías más complejas y peligrosas. En este artículo, nuestro objetivo es describir las características anatómicas y funcionales del músculo tensor de la fascia lata, profundizando en la descripción del músculo en radiología, su patología y un resumen de la literatura sobre el tema.
The differential diagnosis of a palpable tumour on the anterolateral aspect of the thigh is broad and includes neoplastic processes of varying lineage and potential for malignancy,1 focal fat deposits, collections, haematomas or abscesses, as well as abnormalities in the fascia or muscle groups present in that area. Within this last category is selective hypertrophy of the tensor fasciae latae (TFL) muscle, which can be focal or diffuse.
It is important that we take this possibility into account, include it in our differential diagnoses, and learn to recognise it based on the imaging features, the aetiological context and associated findings, to avoid incorrect diagnoses or unnecessary invasive procedures.
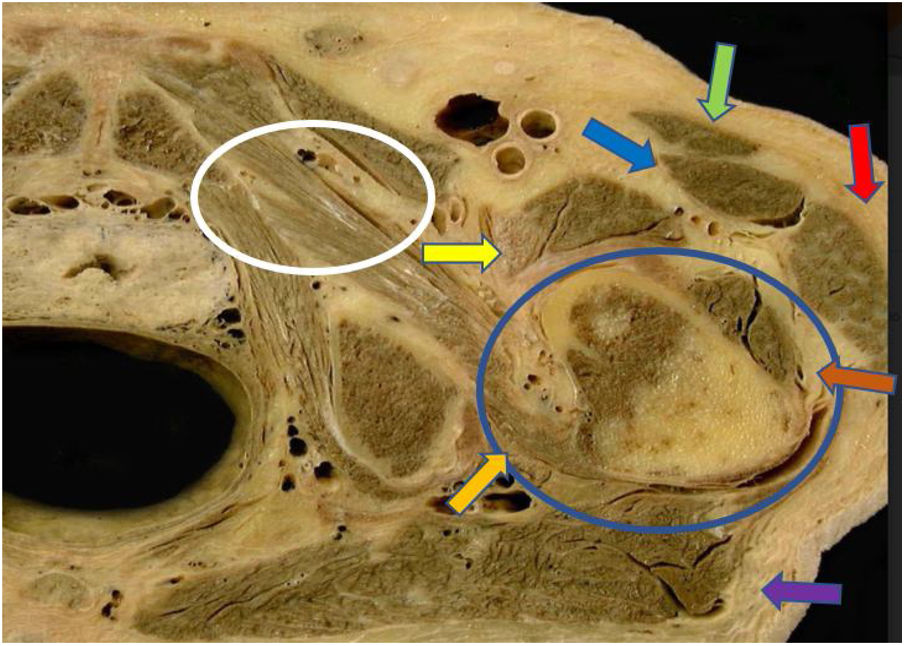
Anatomy and functionThe TFL is a skeletal muscle located over the anterior-lateral aspect at the root of the thigh (Fig. 1). The insertion site is in the lateral margin of the iliac crest, along its anterior segment, in the lateral margin of the anterior-superior iliac spine, and of the more superficial fibres, is the deep surface of the fascia lata.2,3
Anatomical cross-section in the transverse axis of the proximal region of the left thigh, at the proximal metaphyseal region of the right femur. Various muscle structures can be seen around the proximal femur (blue circle): the sartorius muscle (green arrow); the proximal rectus femoris (blue arrow); the vastus intermedius (brown arrow); the distal psoas muscle (yellow arrow); the quadratus femoris (orange arrow); the gluteus maximus (violet arrow); adductor muscles (white circle); and the tensor fasciae latae muscle (red arrow). Courtesy of Dr Alfonso Rodríguez Baena (Universidad Autónoma de Barcelona).
It consists of a single muscle belly, elongated and flattened, about 150 mm long2 and 20 mm in anterior-posterior diameter,4 which runs inferior to its distal insertion slightly below the greater trochanter, where it fuses with the iliotibial band, which descends laterally along the thigh until inserted into Gerdy’s tubercle in the lateral condyle of the tibia. Its innervation depends on the superior gluteal nerve (formed by the posterior roots of L4, L5 and S1), which in turn also innervates the lower and middle gluteal muscles. The TFL has several functions. First of all, it helps stabilise the pelvis when walking, preventing it from tilting to the other side during single-limb support. Along with the gluteus minimus and medius muscles, the TFL participates in the abduction and internal rotation of the hip. Through its continuity with the iliotibial tract, it is an accessory knee flexor and also helps stabilise the knee in extension.3,5
Imaging featuresThe TFL is a muscle with an obvious fibrillar pattern, composed of parallel fibres arranged in a slightly oblique sagittal plane, in an inferior and slightly lateral direction.5 It has interfibrillar fat, which progressively increases from proximal to distal. On ultrasound, the TFL appears hypoechoic cranially, with an increase in echogenicity as it descends, to the extent that caudally, it may be slightly hyperechoic in relation to the adjacent musculature. This finding stems from the increase in interfibrillar fat and should not be misinterpreted.4
On magnetic resonance imaging (MRI), the TFL appears isointense in relation to the rest of the musculature, and small foci of increased signal can be seen in T1- and T2-enhanced sequences in relation to above-mentioned interfibrillar fat.
Lastly, in computed tomography (CT) images, the TFL is isodense in relation to the adjacent musculature, and its interfibrillar fat, slightly hypodense, is less evident than in other imaging techniques, with the TFL more homogeneous along its entire length.
Differential diagnosisAlthough a broad range of disorders can affect the TFL and adjacent structures, the presentation is usually distinctive, in the form of a palpable tumour on the anterior-lateral aspect of the thigh, which appears asymmetric compared to the other thigh, and with variable degrees of pain. A high percentage of patients are referred to Radiodiagnostics in the context of pain in the lateral aspect of the hip (greater trochanteric pain syndrome). The differential diagnosis should include the following:
Neoplastic processesAlthough they should be included in the differential diagnosis, the presence of a primary or metastatic neoplasm in that area is very rare. Review of the scientific literature reveals isolated cases, such as that reported by Wong of a pleomorphic hyalinising angiectatic tumour located in the TFL and iliotibial band6 or that by Mensah et al.7 of a giant cell tumour of soft tissue arising from the TLF.
Benign lesions and overuse injuriesSuch lesions and injuries can be located both within the muscle and in fascial or subcutaneous planes, and can include bruises, fluid collections and abscesses. This subgroup includes “proximal iliotibial band syndrome”, named by Sher et al., which consists of a lesion at the proximal insertion of the iliotibial band adjacent to the TFL. This can occur in relation to overloading and may be the result of trauma, associated or not with muscle herniations, mainly in female runners, or degenerative in nature, mainly in overweight women. MRI is the diagnostic technique of choice, with images showing thickening of the proximal portion of the iliotibial band, associated with oedema of surrounding soft tissues. Focal increases in signal in the iliotibial band in T2-enhanced sequences are associated with a partial or complete rupture of the band.
Ultrasound is also very useful as, in addition to corroborating the above imaging findings, it helps provide clinical correlation through ultrasound palpation in the affected area, and can also confirm the development of muscle herniations in a dynamic study with active muscle contraction by the patient. At the same time, it enables local ultrasound-guided treatment in certain cases.8–10 Proximal iliotibial band syndrome is an underestimated and underdiagnosed disorder so clear clinical guidance is required for diagnosis. If suspected, investigations should include the iliac tubercle.
LymphadenopathyIn routine clinical practice, lymphadenopathy is one of the most common causes of focal lesions on the anterior-lateral aspect of the thigh. However, from an imaging point of view, they are not problematic in terms of diagnosis.
Selective hypertrophy of the tensor fasciae lataeAlthough compensatory hypertrophy of a skeletal muscle is widely described in the literature,11 the first step should be to differentiate true muscle hypertrophy from pseudohypertrophy.
True muscle hypertrophy consists of an increase in muscle volume based on an increase in the number and size of muscle fibres, while in pseudohypertrophy, the increase in volume occurs due to infiltration of fat and connective tissue into the muscle.12 In both conditions there is an increase in the dimensions of the affected muscle and imaging techniques are required as they cannot be distinguished by physical examination.
In cases of hypertrophy of the TFL, imaging techniques would show an increase in the overall size of the muscle, with preservation of its structure and normal fibrillar pattern, with echogenicity, density or signal intensity similar to a normal muscle on ultrasound, CT or MRI respectively.
In cases of pseudohypertrophy of the TFL, the images would show an increase in overall muscle size, with a decrease in the normal fibrillar pattern and its replacement by fat component. On ultrasound, this would appear as marked hyperechogenic trabeculation between normal isoechoic muscle fibres; on MRI, as an increase in intramuscular multifocal signal in T1/T2-weighted sequences, corresponding to a decrease in signal intensity in fat saturation sequences resulting from intermuscular fat between normal muscle fibres with a normal MRI signal; and on CT, as increased hypodense intramuscular fat component.
The most common cause of compensatory hypertrophy is a selective overloading of the muscle in question as a result of mechanisms causing biomechanical redistribution of the loads it is subjected to.11 This redistribution of loads can be caused by three major aetiological groups:
- 1.
Postoperative disorders: particularly after arthroplasty and iliac or femoral osteotomy.
- 2.
Serious structural alterations regardless of their cause: this section includes post-traumatic sequelae and deforming joint diseases.
- 3.
The dysfunction of the agonist muscle in the affected muscle13 regardless of the cause.
Less common causes of selective hypertrophy of the TFL muscle include selective denervation,12 caused by a root or nerve plexus injury,14 or a postoperative iatrogenic injury,15 which although primarily manifested in the form of muscle atrophy, is also described as compensatory hypertrophy or pseudohypertrophy of the affected muscle.12,15
The most common cause of muscle pseudohypertrophy is muscular dystrophy.12
The literature review shows that there are few articles that analyse selective hypertrophy of the TFL. In 2003, Llaslan et al. reported on a series of eight cases of unilateral hypertrophy in the context of screening for soft tissue tumours in the thigh. They described their imaging findings, and the previous history some patients had (hip surgery or neuropathy), which might have caused the hypertrophy. In three of their cases, a tumour biopsy was performed for diagnosis, the results being compatible with TFL muscle hypertrophy.16
In 2013, Sutter et al. published a study analysing the association between TFL hypertrophy and abductor tendon tears in 35 patients. They performed comparative TFL measurements, using the dimensions of the sartorius muscle in healthy patients and in those affected by tendon tears as reference. They concluded that TFL hypertrophy occurred in those with abductor tear,13 with a significant increase in the TFL/sartorius ratio on the side affected by the abductor tear compared to the other side.
In 2016, Rodríguez-Roiz et al. conducted a retrospective study of patients with hip replacement surgery, in which they analysed the presence of TFL hypertrophy in postoperative follow-up, collecting additional data such as the type of surgical approach, the symptoms and atrophy of the glutaeus minimus and medius. They identified five cases with TFL hypertrophy, using the sartorius muscle as reference, and in all five they also found atrophy or tendon tear in the glutaeus minimus and medius muscles, suggesting an association between painful hip replacement with gluteal muscle dysfunction and development of TFL hypertrophy.17
In 2012, Douglas et al. studied alterations in the TFL in relation to lesions in the superior gluteal nerve after total hip arthroplasty using the anterior-lateral approach. They had 26 cases, and TFL atrophy occurred in 16, but in another three, TFL hypertrophy was found.15
Meijer et al. in 2017 and Mosquera Morales et al. in 2018 published case reports on patients investigated for anterior-lateral tumour of the thigh with TFL hypertrophy, with associated atrophy and glutaeus medius tendon tear18,19; and in 2008, Chang et al. reported a case of TFL hypertrophy associated with denervation by ipsilateral lumbosacral radiculopathy.14
The fact that certain patients with glutaeus muscle tears or weakness develop hypertrophy, and others do not, suggests this factor is one of the many aetiopathogenic factors in the development of this condition.
At our centre, from January 2017 to October 2020, we collected a series of eight patients who attended with a palpable mass in the anterior-lateral region of the thigh and were diagnosed with TFL hypertrophy. Figs. 2–5 show the images of four of them, with these being the most representative cases. All the patients in our series had different degrees of atrophy of the gluteus minimus and medius muscles on the same side as the TFL hypertrophy, which corroborates the associations between these two characteristics described in the scientific literature (Figs. 3–5).
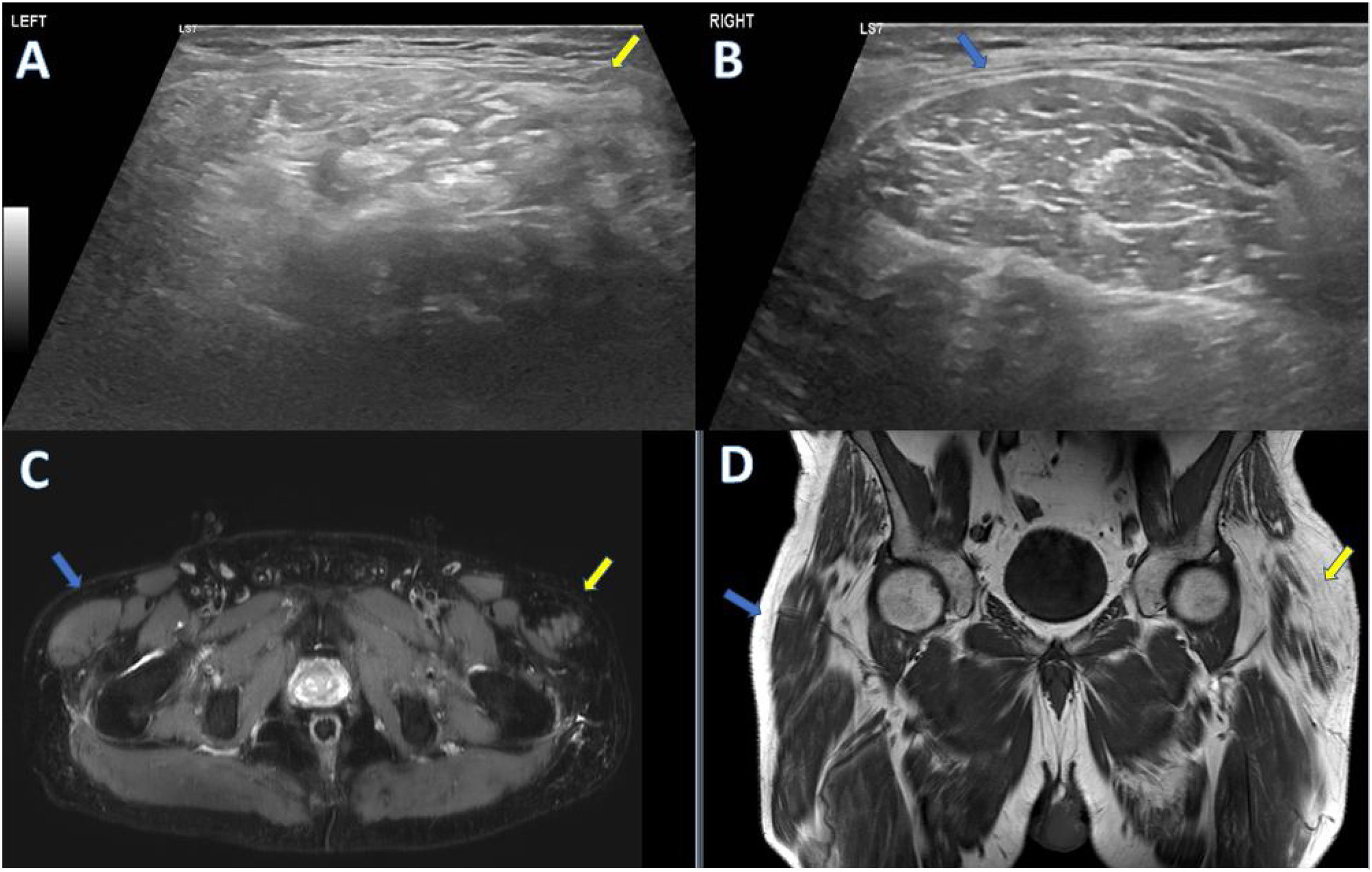
67-year-old man who consulted for tumour in anterior-lateral aspect of his left hip. As relevant previous medical history, the patient has left L5-S1 radiculopathy diagnosed by electromyography. Ultrasound shows asymmetry in size with enlargement of the left tensor fasciae latae (TFL) muscle (image A, yellow arrow) compared to the right (image B, blue arrow), with hyperechoic trabeculation between muscle fibres, related to fat infiltration due to pseudohypertrophy of the muscle. MRI also showed, both in an axial STIR sequence slice (image C) and in a T1-weighted FSE sequence coronal slice (image D), the increase in size of the left TFL (yellow arrows) compared to the right (blue arrows), with increased interfibrillar signal intensity in T1 and decreased signal intensity in STIR, related to fat infiltration due to pseudohypertrophy.
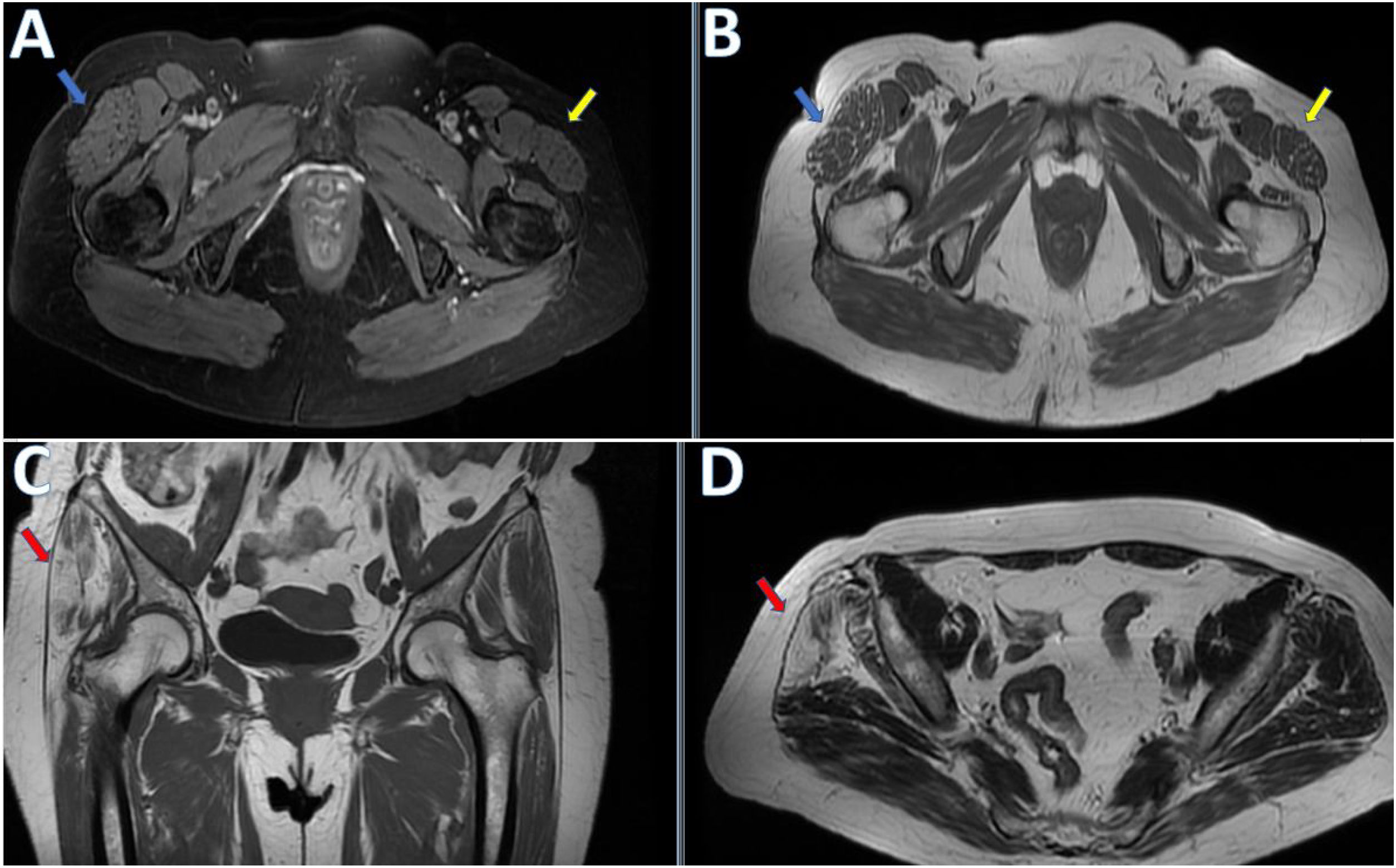
66-year-old woman who consulted for tumour in anterior-lateral aspect of her right hip. On magnetic resonance imaging (MRI), axial slice of STIR sequence (image A) and axial slice of T1-weighted FSE sequence (image B) show an increase in the size of the right tensor fasciae latae muscle (TFL) (blue arrow) compared to the left (yellow arrow), in this case with normal muscle fibrillar pattern, related to hypertrophy. Diffuse fat atrophy/infiltration of the right glutaeus minimus and medius muscles can also be seen, with associated changes due to insertional tendinopathy, which could potentially be the trigger for ipsilateral TFL muscle compensatory hypertrophy (red arrows in C and D, coronal and axial T1-weighted FSE MRI sequence images).
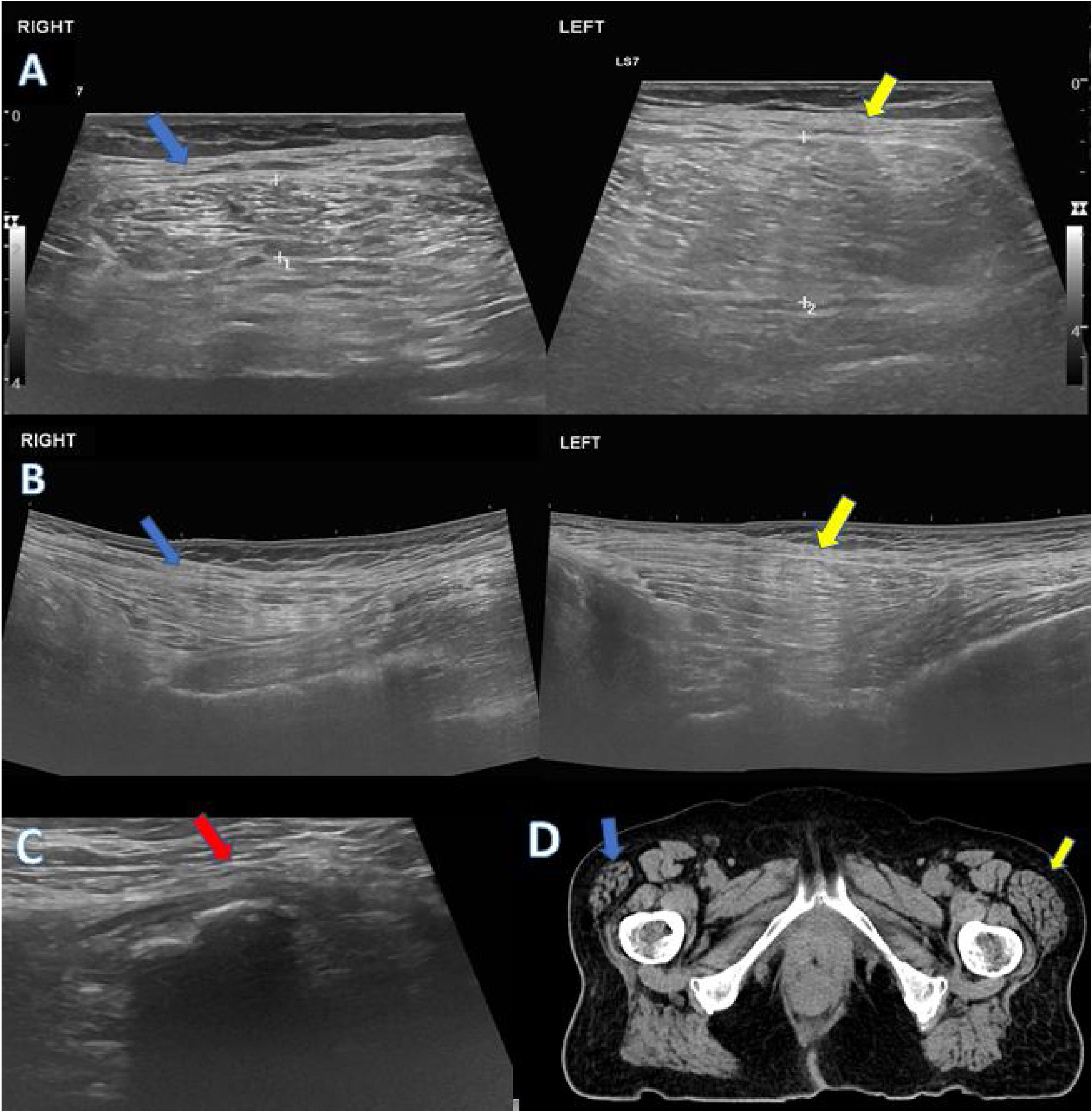
78-year-old woman who consulted for pain and tumour in anterior-lateral aspect of her left hip. Ultrasound showed an increase in the volume of the left tensor fasciae latae muscle (TFL) (images A and B; the yellow arrows indicate axial and longitudinal slices of the left TFL respectively), compared to the right (images A and B, blue arrows indicate axial and longitudinal slices of the right TFL respectively) reaching twice the anterior-posterior diameter. The left gluteus minimus and medius tendons cannot be seen due to chronic tear (image C, red arrow). All this points to compensatory hypertrophy of the left TFL. The axial slice from the computed tomography scan (image D) confirms the increase in size of the left TFL (yellow arrow) compared to the right (blue arrow).
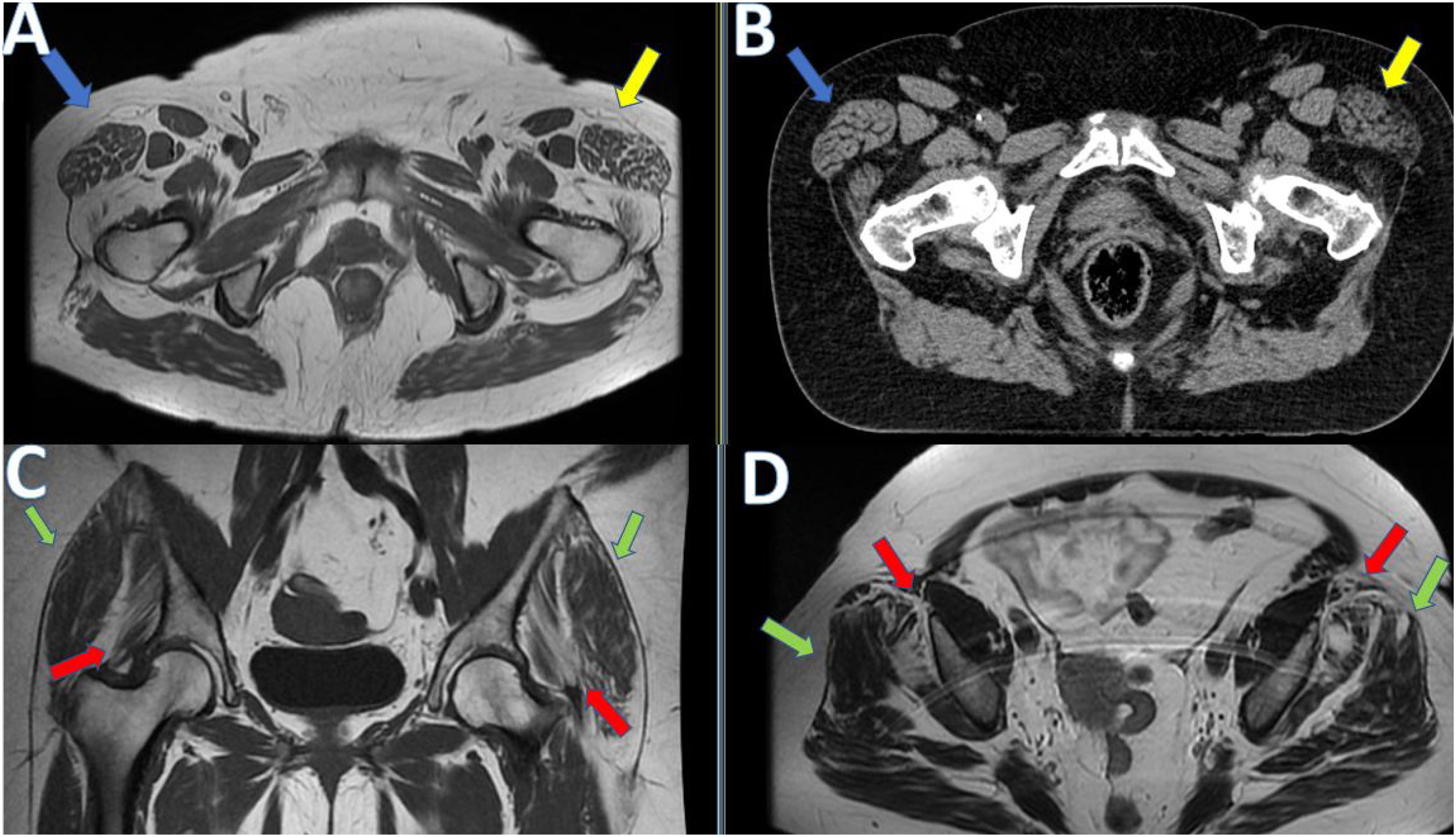
64-year-old woman who consulted for bilateral trochanteric pain. On magnetic resonance imaging with T1–T2-weighted FSE sequences in the axial and coronal planes (images A, C and D), and computed tomography in the axial plane (image B), we can see an increase in size of both tensor fasciae latae muscles (blue and yellow arrows in images A and B) with a slight left predominance, related to hypertrophy, with associated atrophy of the glutaeus minimus (images C and D red arrows) and glutaeus medius, bilaterally, but also predominantly on the left (images C and D green arrows).
These findings appear to corroborate one of the causal mechanisms of selective muscle hypertrophy, in which there is biomechanical redistribution of the loads, with overload of a muscle due to the dysfunction of its agonists; in our cases, of the abductor gluteal muscles. This produces an overload of the TFL, with all the load of the abduction of the hip falling on the TFL and causing compensatory hypertrophy.
We presented a case of pseudohypertrophy of the TFL, whose cause was an ipsilateral radiculopathy, corroborating another of the causal associations described in the literature, of muscular pseudohypertrophy caused by denervation (Fig. 2).
ConclusionTFL muscle hypertrophy should be included in the differential diagnosis of anterior-lateral thigh swelling, as although not a common finding, it is described and documented with its possible causal relationships. Consequently, taking the clinical context and the patient’s history in association with the imaging findings, this diagnosis can be made accurately and without having to resort to invasive procedures.
Authorship- 1.
Responsible for study integrity: SM.
- 2.
Study concept: MP.
- 3.
Study design: AS.
- 4.
Data collection: MP.
- 5.
Data analysis and interpretation: SM.
- 6.
Statistical processing: MP.
- 7.
Literature search: MP, AS.
- 8.
Drafting of the article: SM, MP.
- 9.
Critical review of the manuscript with intellectually significant contributions: AS, AB.
- 10.
Approval of the final version: AS, AB.
The authors declare that they have no conflicts of interest.