Fractures of the petrous part of the temporal bone are a common lesion of the base of the skull; most of these fractures result from high-energy trauma. In patients with multiple trauma, these injuries can be detected on CT scans of the head and neck, where the direct and indirect signs are usually sufficient to establish the diagnosis. It is important to these fractures because the temporal bone has critical structures and the complexity of this region increases the risk of error unless special care is taken. This article reviews the key anatomical points, the systematisation of the imaging findings, and the classifications used for temporal bone fracture. We emphasise the usefulness of identifying and describing the findings in relation to important structures in this region, of looking for unseen fractures suspected through indirect signs, and of identifying anatomical structures that can simulate fractures. We point out that the classical classifications of these fractures are less useful, although they continue to be used for treatment decisions.
La fractura de peñascos constituye una lesión común de la base del cráneo, y la mayoría son el resultado de traumatismos de alta energía. Su reconocimiento en politraumatizados puede realizarse en las tomografías computarizadas de cráneo y cervicales. Los hallazgos directos e indirectos suelen ser suficientes para establecer el diagnóstico. Su identificación es importante debido a que el hueso temporal contiene estructuras críticas, y es posible errar debido a la complejidad de esta región, y su insuficiente vigilancia. Este trabajo revisa los puntos clave anatómicos, la sistematización de los hallazgos radiológicos y las clasificaciones usadas en fracturas de hueso temporal. Cobra relevancia la identificación y descripción de los hallazgos relativos a estructuras importantes de esta región, la búsqueda de fracturas no visibles sospechadas por signos indirectos, y la identificación de estructuras anatómicas que pueden simular fracturas. Pierden valor las clasificaciones clásicas, aunque siguen condicionando el manejo terapéutico.
Fracture of the petrous portion of the temporal bone is a common base of skull fracture and usually the result of high-energy trauma. In patients with multiple trauma, these injuries can be detected on computed tomography (CT) scans of the head and neck, where the direct and indirect signs are usually sufficient to establish the diagnosis. Except in specific situations, performing other specific imaging tests is not usually necessary. It is important to identify these fractures because the temporal bone contains critical structures and the complexity of this region increases the risk of error unless special care is taken in the radiological examination.
Our aim was to review the key anatomical points and the systematisation of radiological findings, and verify the validity of the different classifications used in temporal bone fractures. We carried out a systematic search in scientific article search engines, taking publications from the last eight years into account, and a non-systematic consultation of classic articles and chapters of well-known books.
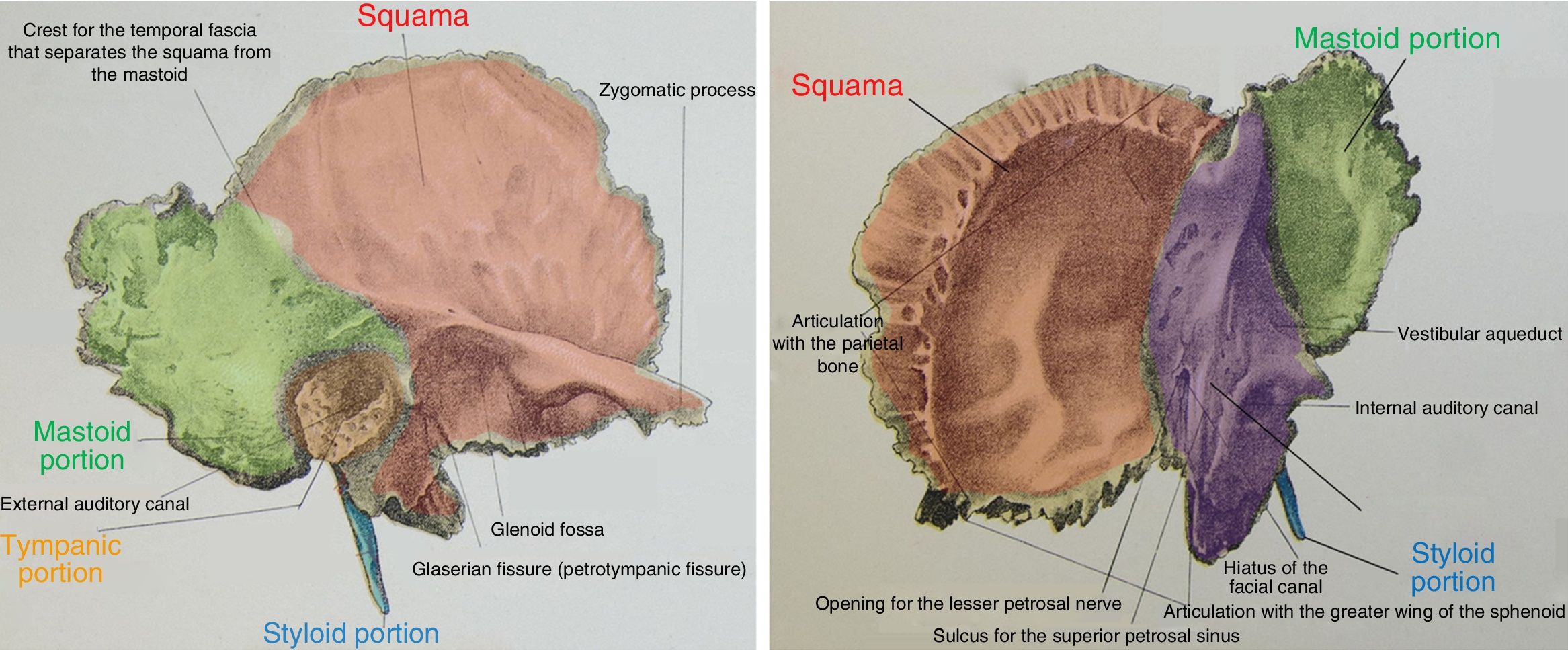
AnatomyComponents of the temporal boneThe vestibulocochlear organ is embedded in the temporal bone, which has complex anatomy. The temporal bone is formed of five portions: the squama, which forms the lateral wall of the middle cranial fossa; the mastoid, which is the aerated posterolateral portion, and most frequently affected by trauma; the petrous, which is the medial triangular portion that houses the inner ear, the internal auditory canal (IAC) and the petrous apex; the tympanic, which forms the U-shaped bony external auditory canal (EAC); and the styloid (Fig. 1).1–5
Illustration of the temporal bone, lateral (A) and superior (B) views.
The ear is in turn divided into the three parts, the outer ear, middle ear and inner ear.
The outer ear (OE) is composed of the pinna and the EAC.5 The wall of the lateral third of the EAC is formed by fibrocartilage, and that of the medial two thirds by the tympanic portion of the temporal bone. The medial limit of the EAC is the tympanic membrane, which is inserted into the scutum (bony spur in the superior/medial portion of the bony EAC) and the tympanic ring. Its anterior limit is the posterior wall of the glenoid fossa.1–3
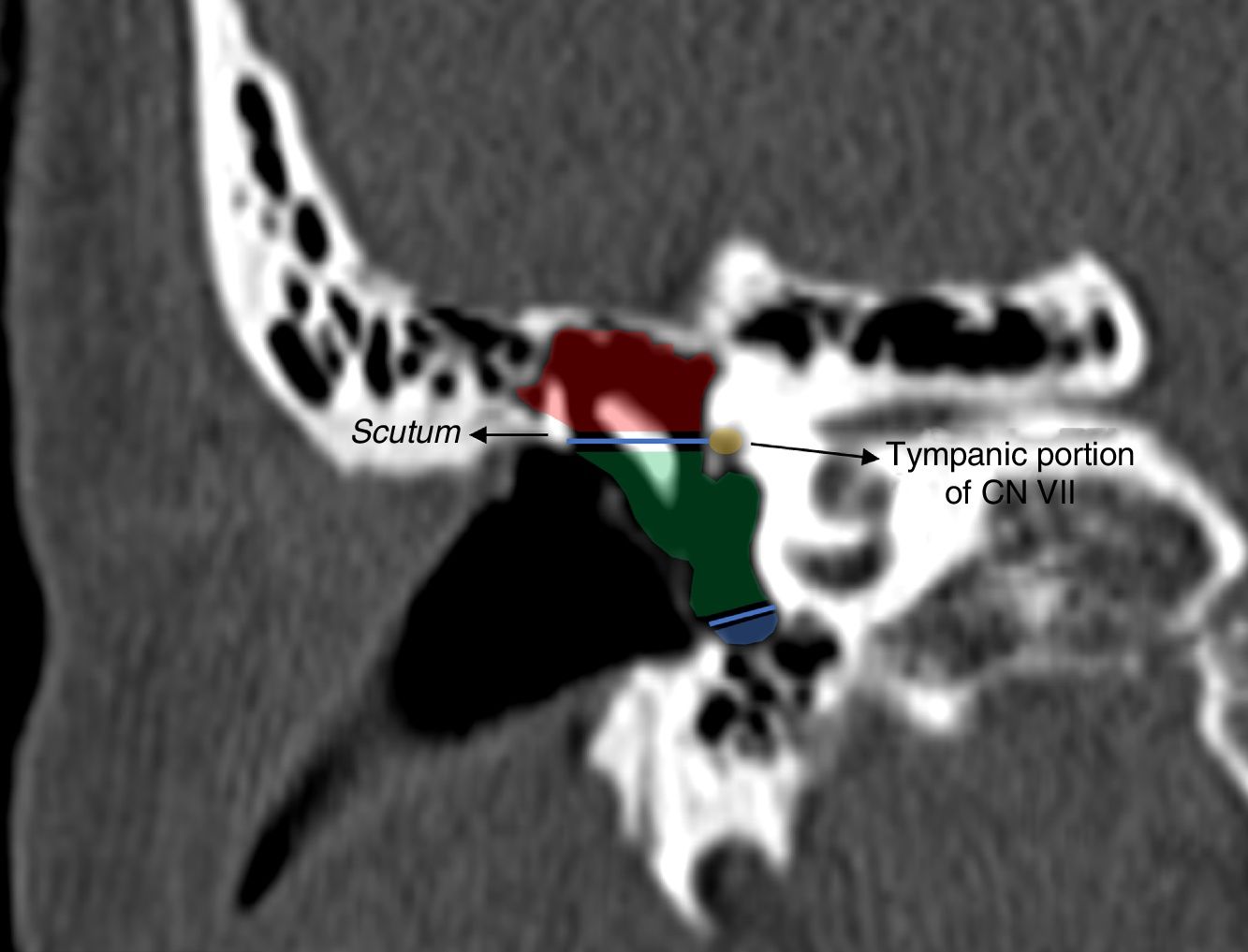
The middle ear (ME) is composed of the tympanic cavity (in the petrous portion of the temporal bone) and the mastoid antrum. In turn, the tympanic cavity is formed by the epitympanum, the mesotympanum and the hypotympanum (Fig. 2).1–3
Coronal computed tomography of petrous portion in which the division of the tympanic cavity is represented: the epitympanum (red), whose inferior limit is formed by an imaginary line drawn from the scutum to the tympanic portion of CN VII; the mesotympanum (green); and the floor, the hypotympanum (blue).
The lower limit of the epitympanum is an imaginary line from the scutum to the tympanic portion of the seventh cranial nerve (CN VII), and its roof is the tegmen tympani. The epitympanum has the following important structures:
- •
The tegmen tympani, which forms the bony roof of the ME and separates it from the dura mater in the middle cranial fossa.
- •
The head of the malleus, and the body and short branch of the incus, with the incudomalleolar joint which, in the absence of pathology, has a similar shape to an ice-cream cone.3–6
- •
The aditus ad antrum, which communicates the tympanic cavity with the mastoid antrum.
- •
Prussak's space, a lateral epitympanic recess, relevant in cases of cholesteatomas as it is often involved.
The mesotympanum is below the epitympanum and above the hypotympanum and also has important structures. On its posterior wall are the pyramidal eminence, from whose vertex the stapedius muscle arises; the sinus tympani, the most hidden recess in the middle ear; and the mastoid segment of the facial nerve. In its medial wall are the oval window, which connects to the base of the stapes, the round window, and the tympanic segment of the facial nerve.1–3
The hypotympanum forms the floor of the tympanic cavity and does not contain any structures of interest.
The chain of ossicles is located in the tympanic cavity and is formed by the malleus, the incus and the stapes. The handle of the malleus is attached to the tympanic membrane. The head of the malleus articulates with the short apophysis of the incus, lateral to the malleus, in the epitympanum (shaped like an ice-cream cone). Lastly, the incus’ lenticular process articulates with the head of the stapes, and the footplate of the stapes, with the oval window.3,5 The incus is the heaviest of the three bones and has less ligamentous support, which makes it the most vulnerable in the chain in the event of trauma.3–5,7
The inner ear is located in the petrous portion of the temporal bone and contains the labyrinth, which in turn has two parts, the bony labyrinth or otic capsule, and the membranous labyrinth.
The bony labyrinth is divided into the vestibule, the cochlea and the three semicircular canals: the superior, which forms the arcuate eminence on the roof of the petrous bone; the lateral, caudal to which runs the tympanic portion of CN VII1,2; and the posterior.
The IAC is a canal on the medial side of the petrous bone that contains CN VII and CN VIII, and its lateral portion shares a border with the labyrinth.5
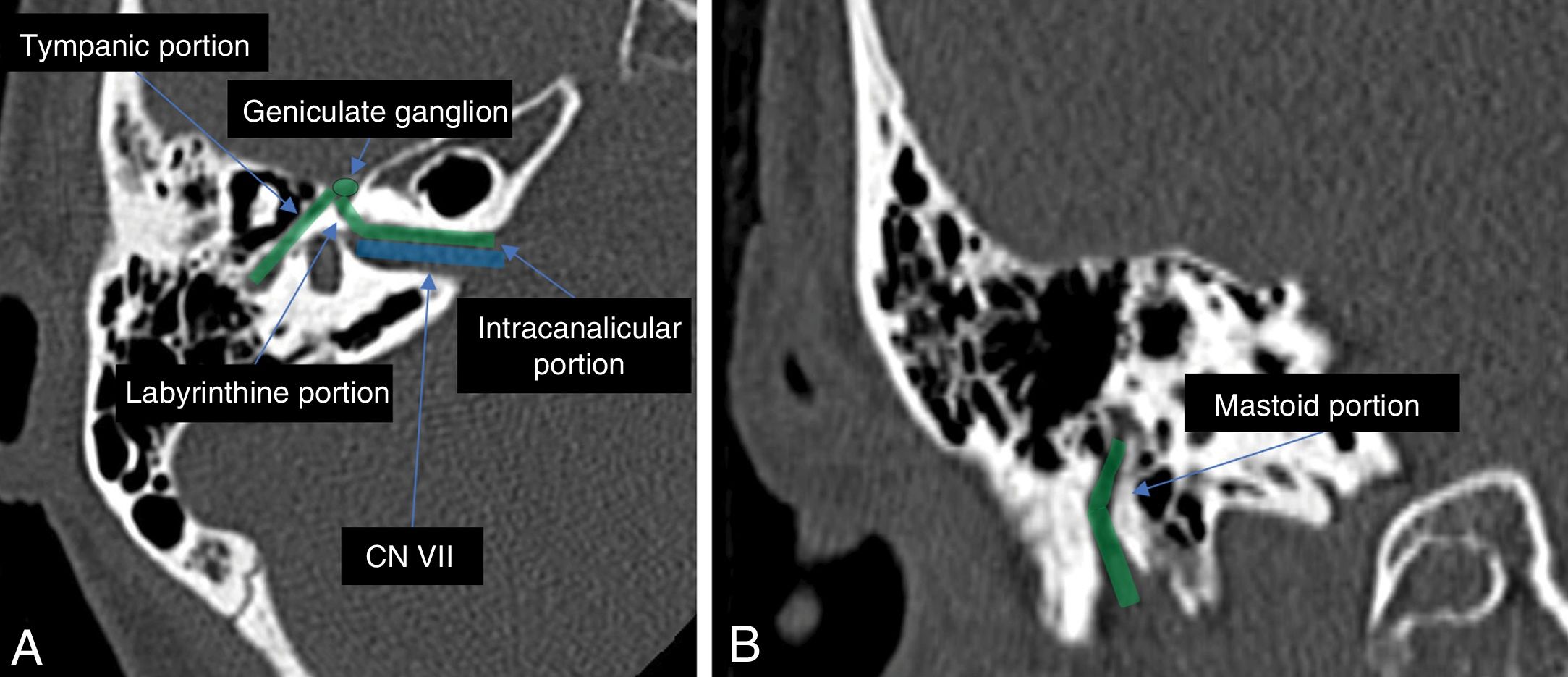
The facial nerve (CN VII)In traumatic injury to the petrous portion, it is essential to understand the anatomy of the path of the facial nerve. It has six segments: the cisternal, from the pons to the IAC; the intracanalicular, along the IAC; the labyrinthine, from the entrance to the aqueduct of Fallopius or facial canal to the geniculate ganglion; tympanic, from the geniculate ganglion to the pyramidal eminence of the facial; the mastoid, from the pyramidal eminence to the stylomastoid foramen; and the extracranial/parotid foramina.1,3
The segments that cross the petrous portion are the labyrinthine, the tympanic and the mastoid (Fig. 3), and the easiest way to locate the facial nerve in the temporal bone is to look for the stylomastoid foramen between the styloid and the mastoid and follow it cephalically. The labyrinthine and tympanic segments are practically in the same axial plane.
Traumatic injuryTemporal bone injuries can be caused by a number of mechanisms of action, such as penetrating (shots, branches, etc.), bruising (traffic accidents, etc.) or barotrauma.
The most common fractures of the base of the skull,8 present in 14–22% of all cases of skull fractures, are temporal bone or laterobasal fractures resulting from high-energy blunt-force trauma, and are most often caused by road traffic accidents (45–47%), falls (31–33%) and assault (11%).3,8–12 According to the 2016 Schub series, the most common cause now would be falls, with the change being explained by improvements in road safety.13
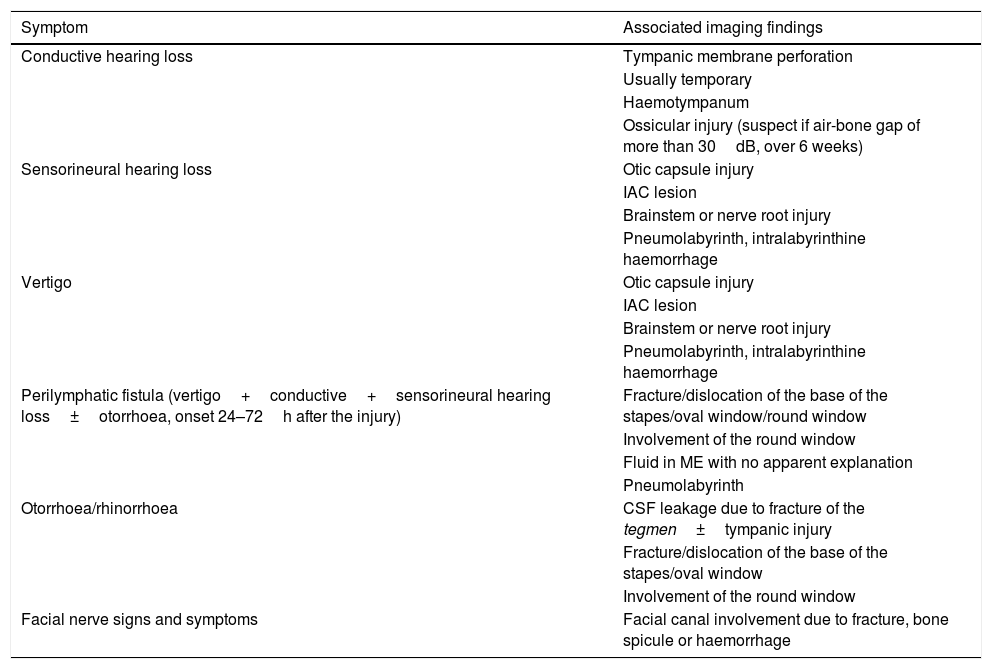
The clinical manifestations can be very diverse and may be masked by the critical condition and low level of consciousness of many patients on arrival at hospital. The manifestations are listed in Table 1 along with possible associated imaging findings. These findings will be discussed later.
Radiological findings according to symptoms.
| Symptom | Associated imaging findings |
|---|---|
| Conductive hearing loss | Tympanic membrane perforation |
| Usually temporary | |
| Haemotympanum | |
| Ossicular injury (suspect if air-bone gap of more than 30dB, over 6 weeks) | |
| Sensorineural hearing loss | Otic capsule injury |
| IAC lesion | |
| Brainstem or nerve root injury | |
| Pneumolabyrinth, intralabyrinthine haemorrhage | |
| Vertigo | Otic capsule injury |
| IAC lesion | |
| Brainstem or nerve root injury | |
| Pneumolabyrinth, intralabyrinthine haemorrhage | |
| Perilymphatic fistula (vertigo+conductive+sensorineural hearing loss±otorrhoea, onset 24–72h after the injury) | Fracture/dislocation of the base of the stapes/oval window/round window |
| Involvement of the round window | |
| Fluid in ME with no apparent explanation | |
| Pneumolabyrinth | |
| Otorrhoea/rhinorrhoea | CSF leakage due to fracture of the tegmen±tympanic injury |
| Fracture/dislocation of the base of the stapes/oval window | |
| Involvement of the round window | |
| Facial nerve signs and symptoms | Facial canal involvement due to fracture, bone spicule or haemorrhage |
CSF: cerebrospinal fluid; IAC: internal auditory canal; ME: middle ear.
Translated and adapted from Kennedy TA et al.14
In most cases, as the fractures are caused by high-energy trauma, the temporal bone is studied by CT as part of the serious or potentially serious trauma protocol, which includes thin slices (<1mm) of the cervical spine, and sometimes skull, in which the petrous portion can be included in the case of suspected fracture, and this is usually sufficient for diagnosis.3,14 Multiplanar reconstructions are important, and it is not necessary to perform specific CT of the temporal bone.3,13,15
However, there are specific situations in which it is necessary to perform a CT angiography or high resolution CT of the petrous portion, whether as an emergency or planned3,10,13,14:
- •
Suspected carotid canal injury.
- •
High clinical suspicion of fracture, not seen in initial images.
There are also situations where magnetic resonance imaging is necessary4,9,16:
- •
Some cases of paralysis of CN VII with normal CT.
- •
Persistent sensorineural hearing loss without abnormalities on CT.
- •
Suspected intra-labyrinthine bleeding (important finding due to the legal repercussions in identifying this, rather than due to possible changes in associated therapeutic approach).
- •
Suspected meningocele or associated encephalocele.
They should provide indications on the mechanisms of production, the extension, severity and prognosis, but in practice no classification meets all these requirements.3,9
Apart from the traditional classification, new classifications have recently emerged, such as otic capsule violating/sparing, petrous portion violating/sparing3,7,10 and involvement of the four components of the temporal bone.17
Traditional classificationThe traditional classification is still the most used by clinicians.9 It divides fractures into longitudinal (the most common3,5,9,13,14), transverse and oblique or mixed.
Longitudinal fractures are parallel to the long axis of the petrous bone3,14 and, depending on their location with respect to the labyrinthine structures (or the EAC4), may be either anterior or posterior.5,7,9
Transverse fractures are perpendicular to the long axis of the petrous bone3,14 and, depending on their location with respect to the arcuate eminence, may be either lateral or medial.4,5,7,9
The oblique or mixed category is because many fractures include both components and so cannot be classified as strictly longitudinal or transverse.
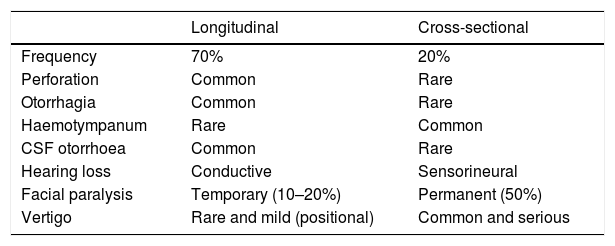
The traditional classification has good correlation with the production mechanisms and certain clinical signs (Table 2), but is poor for predicting complications and prognosis and is not therefore representative of the fractures seen in daily clinical practice.3,4,9,10 This is because it was developed from experiments in the first half of the 20th century on cadaveric skulls hit with blunt objects.3,4,14,18 It is also considered arbitrary, as it only takes into account the axial plane of the fracture and not the other planes of the space for assessment.3,14
Findings associated with the traditional classification. After several reassessments of the classification, these findings were found not to be so related.
| Longitudinal | Cross-sectional | |
|---|---|---|
| Frequency | 70% | 20% |
| Perforation | Common | Rare |
| Otorrhagia | Common | Rare |
| Haemotympanum | Rare | Common |
| CSF otorrhoea | Common | Rare |
| Hearing loss | Conductive | Sensorineural |
| Facial paralysis | Temporary (10–20%) | Permanent (50%) |
| Vertigo | Rare and mild (positional) | Common and serious |
The new classifications, described below, seem to show better correlation with the development of serious sequelae.3,14
In the classification according to violation/sparing of the otic capsule or bony labyrinth there are two situations3:
- •
Fractures involving the otic capsule, which represent 2–7% of fractures and are associated with a higher rate of complications such as sensorineural hearing loss, leakage of cerebrospinal fluid (CSF), vascular injury and facial nerve paralysis.11,14
- •
Fractures sparing the otic capsule, which represent 93–98% of fractures and are more commonly associated with intracranial lesions (epidural haematomas, subarachnoid haemorrhage, etc.).
In the classification according to violation/sparing of the petrous bone, there are3:
- •
Fractures involving the petrous bone, i.e. the otic capsule and the petrous apex have greater correlation with sensorineural hearing loss, facial nerve paralysis and CSF leakage.
- •
Fractures sparing the petrous bone but involving the OE, the ME, and/or the mastoid: due to their greater tendency to extend to the ME, they are more prone to causing conductive hearing loss.10
Classification of fractures according to involvement of the four components of the temporal bone divides it into four portions (squama, tympanic, mastoid and petrous), and classifies the fractures according to whether they involve one, two, three or more of the components. Unlike the other new classifications, no good correlation has been shown with the development of clinical symptoms and sequelae.17
In conclusion, the new classifications seem to provide better guidance in terms of predicting the clinical prognosis and choosing the most appropriate therapeutic approach, with the otic capsule-violating/sparing classification being the most relevant for these purposes.3–5,9,10 Despite this, not all authors agree with the new classifications,9 and it is still important to include the direction of the traditional classification in the report, as it provides the otorhinolaryngology specialist with a conceptual idea of the fracture pattern.3,14
More important than classifying the fractures are identification and description of the findings and possible complications, and multiplanar reconstructions are very useful for that purpose. Including that information increases the clinical relevance of our report, helping improve the management and prediction of the patient's prognosis.3,10,14
Structures to be reviewedBecause of the different possible repercussions, there are a series of elements which have to be studied in cases of injury of the temporal bone, and these are explained below.
External auditory canalIt is important to detect fractures in this area (Fig. 4), as if they are not detected and treated, they can lead to stenosis of the EAC; a situation which can be prevented by temporary tamponade.3 Patient follow-up is also important, in order to assess potentially treatable long-term complications.19
The relationship of the anterior wall of the EAC with the glenoid fossa explains the different fracture mechanisms; by impaction of the mandibular condyle at the posterior portion of the temporomandibular joint or direct extension of the fracture to the EAC.3,19
It is important to assess the axial and coronal slices of the EAC along its entire length, as well as its relationship with the temporomandibular joint.3
Ossicular chainThe continuity of the ossicular chain can best be assessed from axial slices.3,4 Dislocation of the ossicles is more common than fracture3,4,6,9 and the incus is the element of the chain most frequently affected in both types of injury, because it is the largest and heaviest ossicle and, as mentioned previously, it has less ligamentous support.
The most common causes of conductive hearing loss after traumatic injury of the temporal bone are haemotympanum and rupture of the tympanic membrane. Persistence of the hearing loss for more than six weeks after healing of the tympanic membrane and/or resorption of the haemotympanum is suspicious of ossicular injury.3,4,6,10,14,15
The different types of dislocation include the following3,6,9,14:
- •
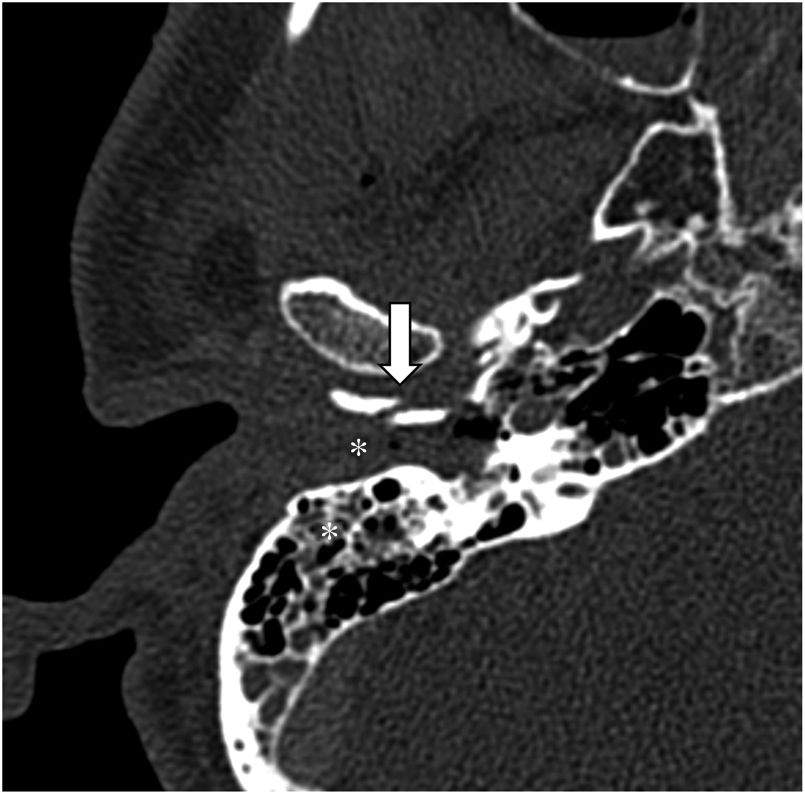
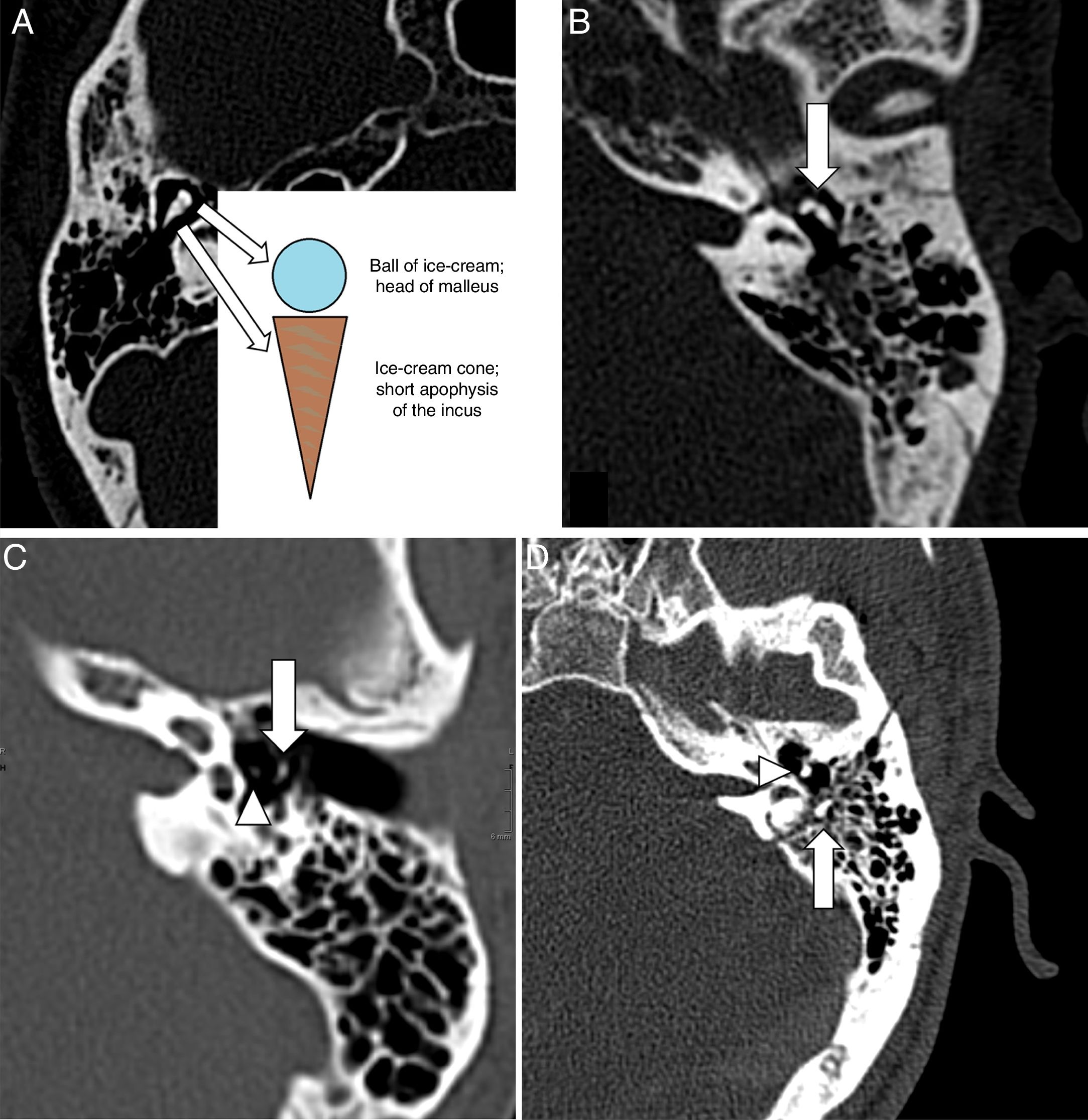
Separation of the incudomalleolar joint. The incus usually becomes displaced from the malleus, which is more fixed, and the joint loses its ice-cream cone shape (Fig. 5A and B). It is easy to visualise in axial slices, although coronal slices are useful in cases of slight lateral displacement of the incus, which can lead to the broken heart sign.
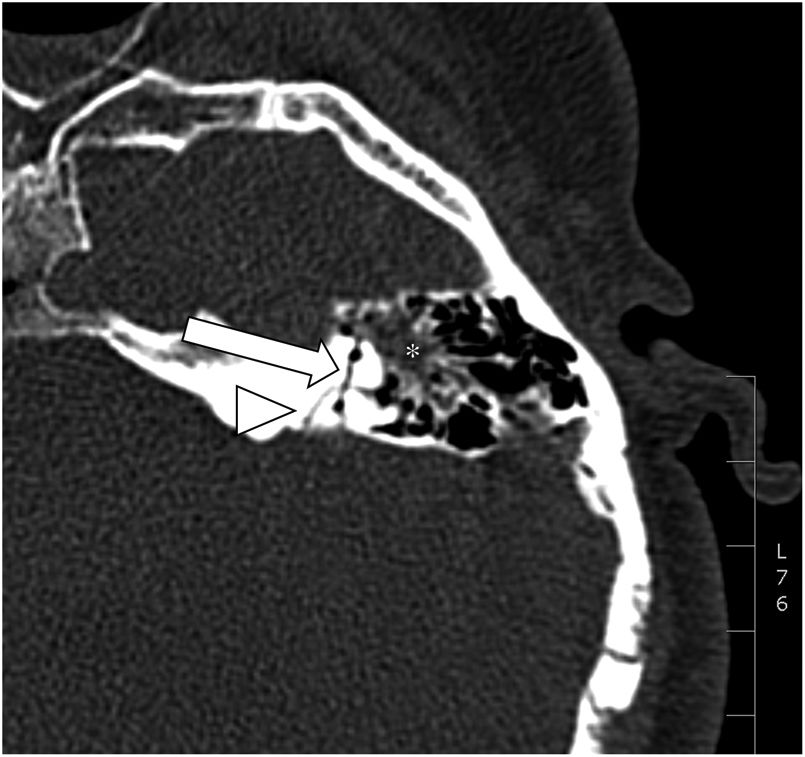
Figure 5.(A) Axial CT showing the incudomalleolar joint with the shape of an ice-cream cone. (B) The loss of this typical shape suggests incudomalleolar separation (arrow). (C) Delayed oblique axial CT after a road traffic accident, which shows incudostapedial separation. Lenticular apophysis of the incus (arrow). Head of the stapes (arrowhead). (D) Axial CT with dislocation of the incus from both the malleus (arrowhead) and the stapes (arrow), lodged in the aditus ad antrum/mastoids.
(0.38MB). - •
Separation of the incudostapedial joint. The lentiform process of the incus becomes separated from the head of the stapes, and it is difficult to visualise at the acute post-traumatic stage due to haemotympanum (Fig. 5C). It shows up well in axial slices.
- •
Incus dislocation. Involves simultaneous separation of the incus from the malleus and the stapes (Fig. 5D). The incus may remain in the epitympanum, prolapse to the lower part of the tympanic cavity or the EAC, or even disappear. This needs to be assessed in axial and coronal slices in order to identify the exact position of the incus with respect to the other two ossicles.
- •
Dislocation of the malleoincudal complex. Block displacement with sparing of the incudomalleolar joint outward, inward or downward, which may also involve displacement of the incudostapedial joint.
- •
Stapediovestibular dislocation. This is very rare due to the strong ligament attachment between the stapes and the oval window. The dislocation may be internal (the stapes displaced towards the vestibule) or external (the base of the stapes displaced towards the tympanic cavity), and it is a possible cause of perilymphatic fistula.
Of these injuries, the most common are dislocations of the incudostapedial joint and the incudomalleolar joint.3,5,6,8,10,14,20
The most common fractures of the ossicular chain are of the long branch of the incus, which show up well in axial and coronal slices, and of the branches of the stapes, especially the posterior branch. In the malleus, the most common fracture is of the neck, and this is studied in axial and coronal slices, oblique to the long axis of the malleus.3
The carotid canalThe line of the fracture involves the carotid canal (Fig. 6), which increases the risk of damage to the internal carotid artery. This needs to be assessed in the axial, coronal and sagittal planes.3 Approximately 24% of skull base fractures involve the carotid canal, 11% of which have associated vascular complications. CT angiography is therefore indicated if skull base fracture is identified or suspected.3,9,14
There are different types of vascular injury associated with these fractures depending on which layers of the vessel wall are affected, including: dissection; pseudoaneurysm formation; complete vascular occlusion; vascular section; or the formation of a carotid-cavernous fistula.3,4,10,14
Venous drainageThe fracture line affects venous sinuses and/or jugular foramen, which increases the risk of vascular injury in the form of transections or thrombosis.3 If identified or simply suspected, venous CT angiography or venous MR angiography is indicated.14
According to some authors, the identification of fracture lines that affect the jugular foramen is very rarely accompanied by venous complications.9
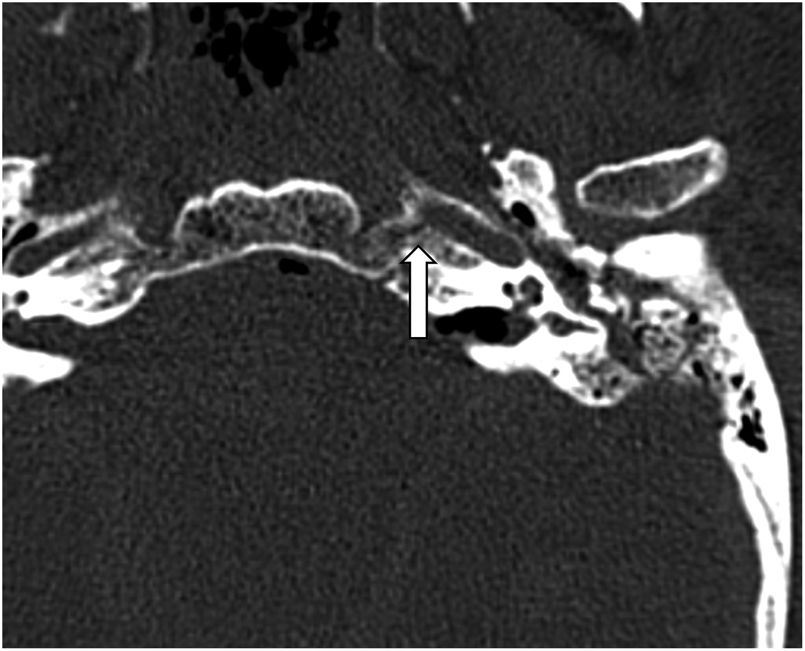
Facial nerveFacial nerve injury occurs in 5–10% of temporal bone fractures, and the portion most commonly affected is the geniculate ganglion3,4,7,8,14,21,22 (Fig. 7). The facial nerve canal has to be examined along its entire length in the axial plane, using oblique sagittal reconstructions to assess the integrity and continuity of the tympanic and mastoid segments in a single image.3
Immediate post-traumatic onset of symptoms usually indicates a serious injury to the facial nerve, by transection or compression by a bone fragment, and may indicate the need for urgent surgical exploration. In contrast, delayed symptom onset, i.e. 1–16 days after the injury, usually occurs due to oedema, swelling or intra- or peri-neural haematoma, and can be managed with observation and corticosteroids, considering surgical exploration if there is a clear bone fragment invading the facial canal.3–5,10,14
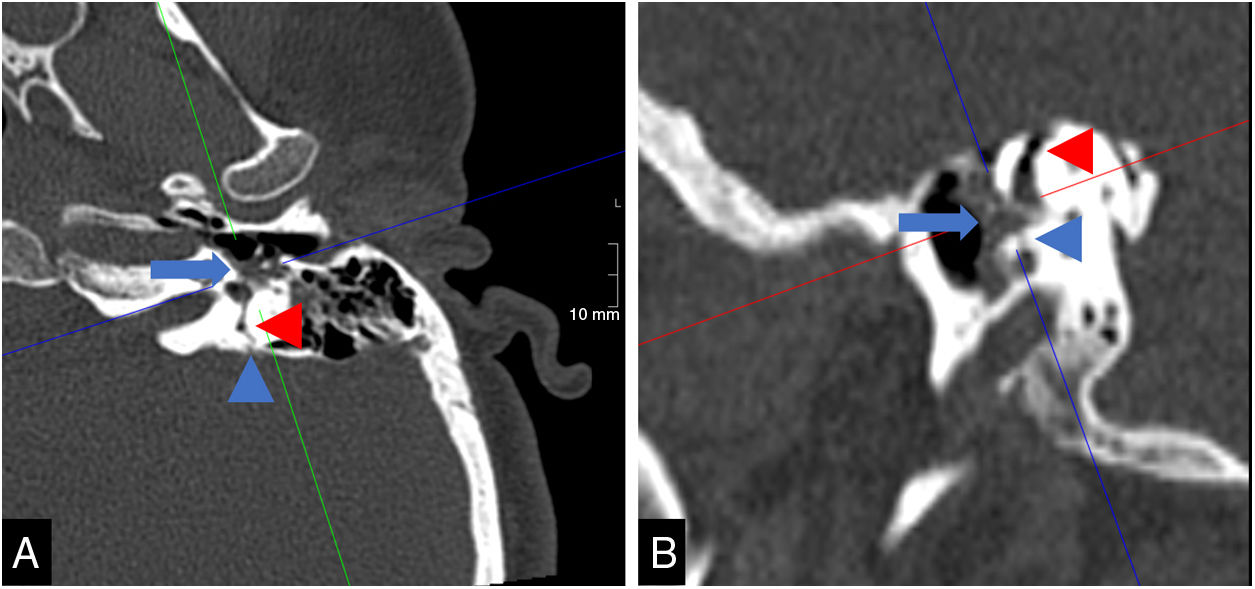
Otic capsuleInvolvement of the cochlea due to fracture or contusion can cause sensorineural hearing loss. The otic capsule is examined with axial slices, and planes parallel to the long and short axis of the petrous portion of the temporal bone, to assess the integrity of the cochlea in its short and long axis respectively.3,14
Fracture or contusion of the vestibule or semicircular canals causes vertigo (Fig. 8). The vestibule is examined with axial and oblique coronal slices, to identify its relationship with the cochlea and the semicircular canals. The semicircular canals are assessed individually in coronal, axial and sagittal orthogonal planes.3 Despite that, we need to bear in mind that the most common form of imbalance after a head injury is benign paroxysmal positional vertigo, which is usually self-limiting in 6–12 months.3,14
However, labyrinthitis ossificans can be a serious after effect of otic capsule-violating fractures, leading to fibrosis and ossification of the labyrinthine structures.9,10
Tegmen tympani/mastoideumTraumatic perforation in the roof of the eardrum and the mastoid cells can be accompanied by CSF leaks, as well as meningoceles, encephaloceles and/or meningitis. It should be assessed with coronal slices, and it is important to describe the location and size of the fracture, as well as the presence and orientation of displaced fragments and the existence of encephalocele.4,9,10,14,16
Indirect imaging signs without visualisation of fracture linesIndirect radiological signs are independent imaging findings that may be present in a specific diagnostic context and can be useful clues in terms of suggesting the diagnosis, even though it is not plain to see23:
- •
Mastoid cell occupation of ME (Fig. 9A) and/or the EAC (Fig. 4).3,4,14
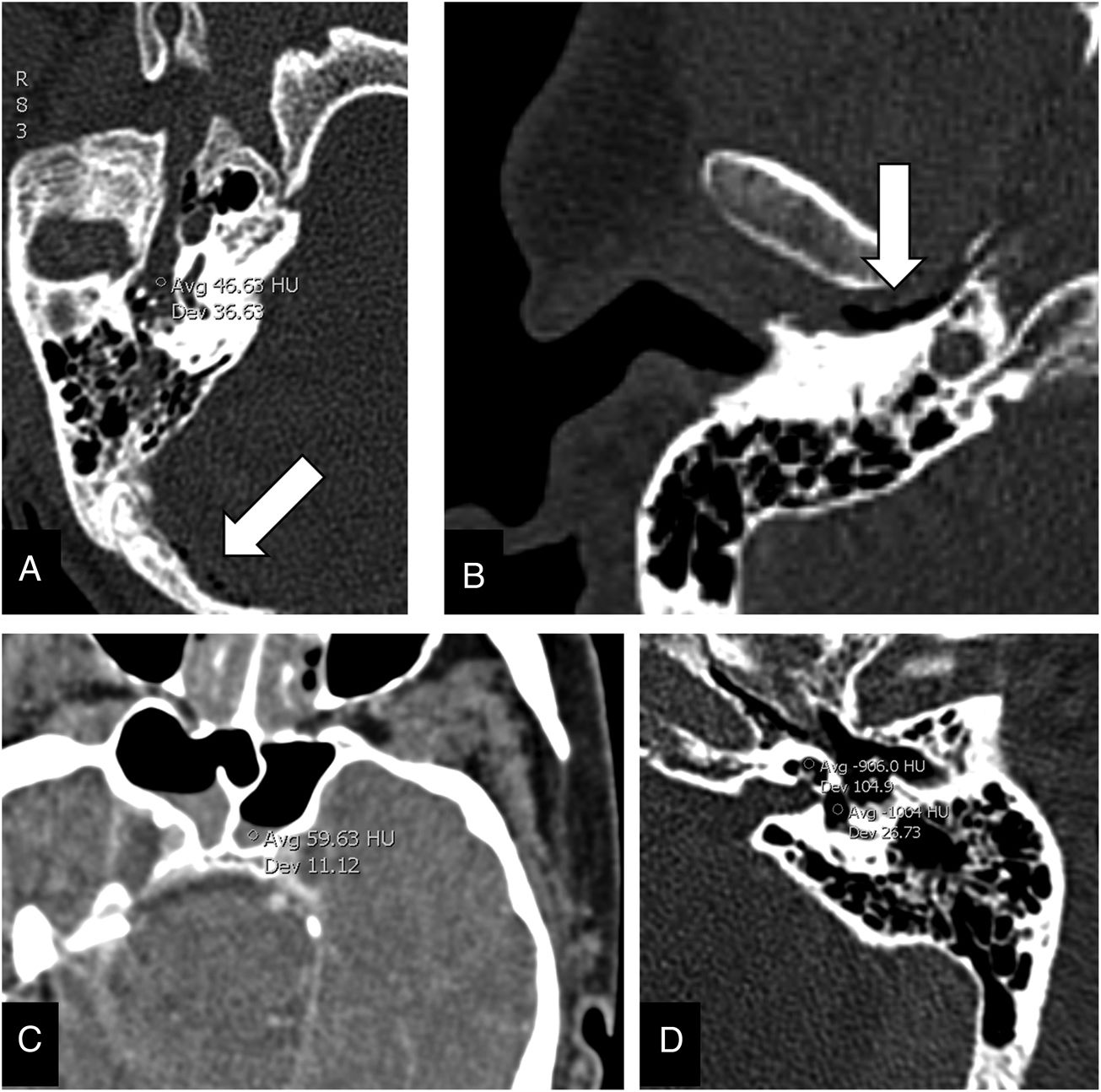
Figure 9.Indirect signs of fracture. (A) Axial computed tomography (CT) with evidence of high attenuation content in the middle ear and mastoid cells. Pneumocephalus bubbles can also be seen (arrow). (B) Axial CT showing air in the glenoid fossa (arrow). (C) Axial CT showing blood-air level (haemosinus) in the sphenoid sinus. (D) Axial CT showing pneumolabyrinth (ROI in cochlea and vestibule: −906HU and −1004HU, respectively) without clear evidence of fracture lines.
(0.18MB). - •
Pneumocephalus adjacent to the temporal bone (Fig. 9A).3,14 According to some studies, pneumocephalus is associated with a greater likelihood of a complex fracture.23
- •
- •
- •
Extra-axial collection of blood.3
- •
Brain injury.3
- •
Pneumolabyrinth (Fig. 9D). This is an indirect sign of perilymphatic fistula, even virtually pathognomonic according to some articles,4,9,24,25 which can occur as a result of stapediovestibular dislocation or extension of the fracture to the otic capsule.14 It is often transitory.24,26
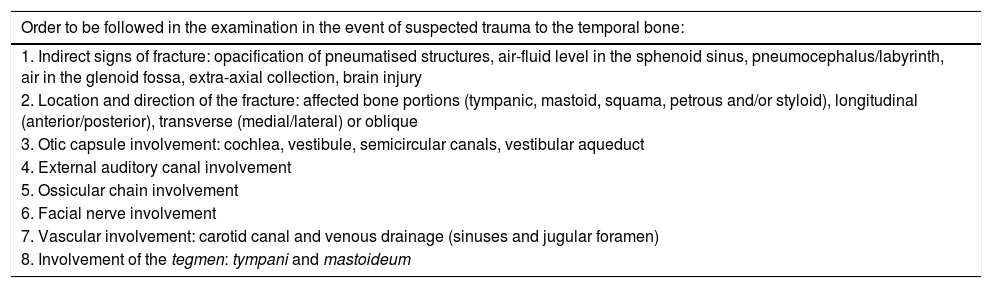
Table 3 shows a suggested order of investigation for suspected temporal bone injury.
Search systematics.
| Order to be followed in the examination in the event of suspected trauma to the temporal bone: |
|---|
| 1. Indirect signs of fracture: opacification of pneumatised structures, air-fluid level in the sphenoid sinus, pneumocephalus/labyrinth, air in the glenoid fossa, extra-axial collection, brain injury |
| 2. Location and direction of the fracture: affected bone portions (tympanic, mastoid, squama, petrous and/or styloid), longitudinal (anterior/posterior), transverse (medial/lateral) or oblique |
| 3. Otic capsule involvement: cochlea, vestibule, semicircular canals, vestibular aqueduct |
| 4. External auditory canal involvement |
| 5. Ossicular chain involvement |
| 6. Facial nerve involvement |
| 7. Vascular involvement: carotid canal and venous drainage (sinuses and jugular foramen) |
| 8. Involvement of the tegmen: tympani and mastoideum |
Translated and adapted from Kennedy TA et al.14
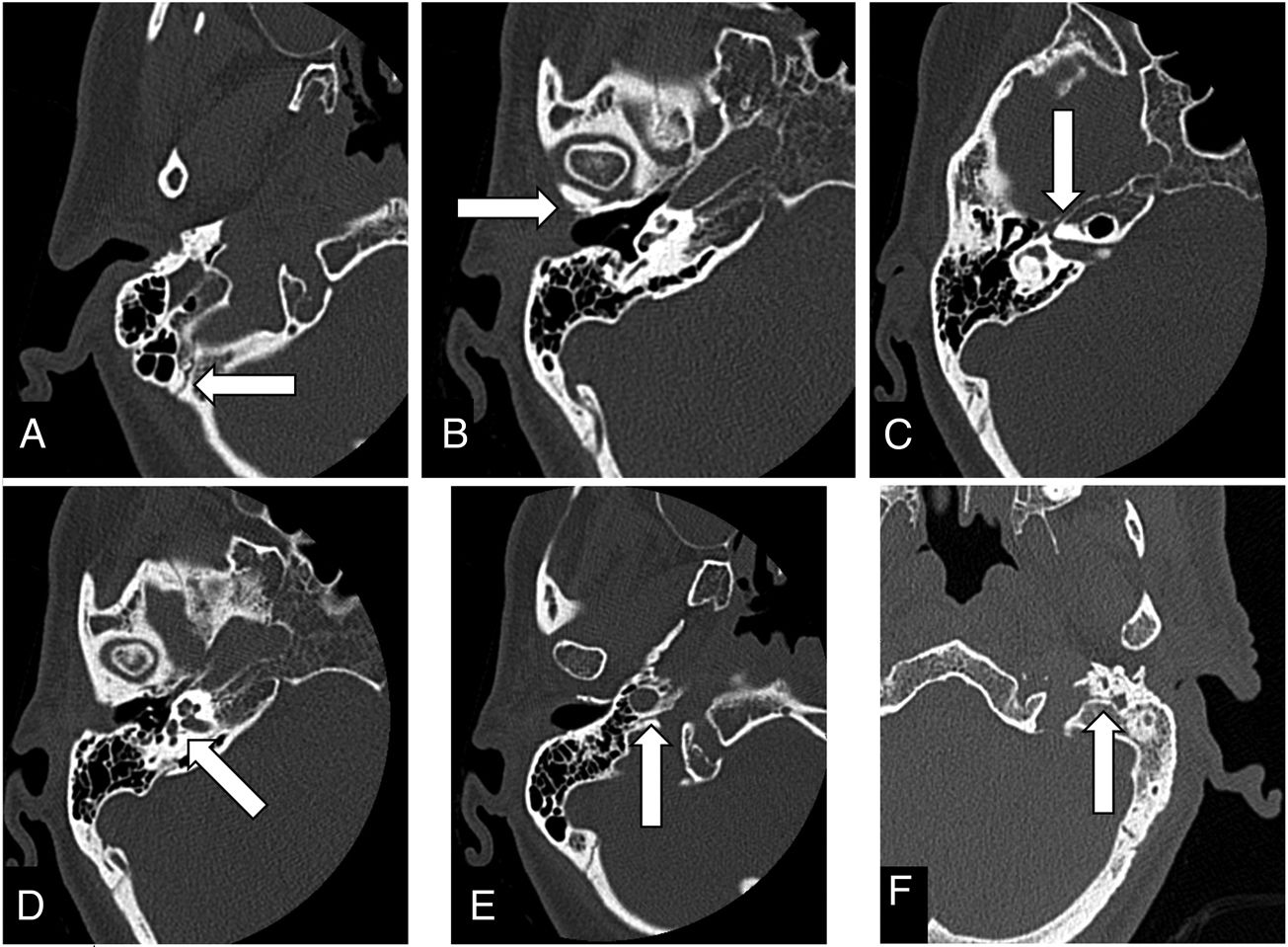
Anatomical structures or variants that can be confused with fracture lines, and which have to be recognised to avoid mistaken diagnoses. The most important are listed below4,5,8,27:
- •
Extrinsic suture lines of the temporal bone. These are between the temporal bone and the rest of the skull, and they differ from fractures in that they follow a non-linear course and have sclerotic borders (Fig. 10A).
- •
Intrinsic fissures of the temporal bone. These are in between the components of the temporal bone:
- –
Tympanosquamous suture: ventral to the EAC, it continues in the petrotympanic and petrosquamous fissures (Fig. 10B).
- –
Petrotympanic (or glaserian) fissure: provides the exit for the chorda tympani from the ME to the infratemporal fossa and also allows the passage of the anterior tympanic artery.
- –
Petrosquamous fissure: continuous with Koerner's septum. It is best seen in coronal slices as a small defect in the tegmen tympani, but in axial it is seen as a crack orientated anteromedially from the glenoid fossa.
- –
Tympanomastoid fissure: posterior to the EAC. Inconstant, Arnold's nerve, branch of the vagus nerve runs through it.
- –
- •
Petromastoid canal, connecting the mastoid antrum to the cranial cavity, which runs an anterior convex route between the arms of the superior semicircular canal, and has an approximate diameter of 0.5mm. This can be a route for the spread of mastoid infections towards intracranial components (Fig. 8).
- •
Hiatus of the facial canal (Fig. 10C). Its path is in the anterior surface of the petrous bone communicating with the geniculate ganglion, and the greater (superficial) petrosal nerve runs through it.
- •
Foramen singulare (Fig. 10D). Its trajectory goes from the IAC (from the vestibular nerve) to the posterior semicircular canal, and the posterior ampullary nerve (singular nerve) runs through it.
- •
Vestibular aqueduct. Contains the endolymphatic duct. Increases in size at its distal end, becoming the endolymphatic sac.
- •
Cochlear aqueduct. It connects the perilymph in the basal turn of the cochlea (close to the round window) to the subarachnoid space.
- •
Inferior tympanic canaliculus (Fig. 10E). Situated between the carotid canal and the jugular foramen. Jacobson's nerve runs through it (from CN IX in the pars nervosa of the jugular foramen) to the ME, along with the inferior tympanic artery.
- •
Mastoid canaliculus (Fig. 10F). Connects the pars vascularis of the jugular foramen and the mastoid portion of the facial canal, a few millimetres above the stylomastoid foramen. Arnold's nerve runs through the mastoid canaliculus.
Knowledge of the different classification systems for petrous portion fractures provides us with information about the characteristics of the fractures. The general trend among clinicians is to prefer the use of the new classifications because they are better at predicting the prognosis, while continuing to use the traditional nomenclature in our reports. Nonetheless, greater importance is given to identification and description of the findings and their possible complications.
The system of investigation we suggest begins with indirect signs, to then be guided towards and focus on the injuries with prognostic impact. There are radiological signs whose significance may be uncertain nowadays, such as pneumolabyrinth. However, examination of such signs in successive studies may be beneficial for predicting patient prognosis.
Authorship- 1.
Responsible for the integrity of the study: MVA.
- 2.
Study conception: MVA and CUC.
- 3.
Study design: MVA, CUC and ADT.
- 4.
Data acquisition: MVA.
- 5.
Analysis and interpretation of the data: MVA.
- 6.
Statistical processing: N/A.
- 7.
Literature search: MVA, CUC and PSGR.
- 8.
Drafting of the paper: MVA.
- 9.
Critical review of the manuscript with relevant intellectual contributions: MVA, CUC, ADT, PSGR and MMG.
- 10.
Approval of the final version: MVA, CUC, ADT, PSGR and MMG.
The authors declare that they have no conflicts of interest.Supplementary data
Supplementary data associated with this article can be found, in the online version, at doi:10.1016/j.rxeng.2019.03.007.
Please cite this article as: Varo Alonso M, Utrilla Contreras C, Díez Tascón Á, García Raya PS, Martí de Gracia M. Patología traumática de peñascos, un diagnóstico complejo. Claves para el informe. Radiología. 2019;61:204–214.