The pandemia caused by SARS-CoV-2 (COVID-19) has been a diagnostic challenge in which chest X-rays have had a key role. This study aimed to determine whether the Radiological Scale for Evaluating Hospital Admission (RSEHA) applied to chest X-rays of patients with COVID-19 when they present at the emergency department is related with the severity of COVID-19 in terms of the need for admission to the hospital, the need for admission to the intensive care unit (ICU), and/or mortality.
Material and methodsThis retrospective study included 292 patients with COVID-19 who presented at the emergency department between March 16, 2020 and April 30, 2020. To standardize the radiologic patterns, we used the RSEHA, categorizing the radiologic pattern as mild, moderate, or severe. We analyzed the relationship between radiologic severity according to the RSEHA with the need for admission to the hospital, admission to the ICU, and mortality.
ResultsHospital admission was necessary in 91.4% of the patients. The RSEHA was significantly associated with the need for hospital admission (p = 0.03) and with the need for ICU admission (p < 0.001). A total of 51 (17.5%) patients died; of these, 57% had the severe pattern on the RSEHA. When we analyzed mortality by grouping patients according to their results on the RSEHA and their age range, the percentage of patients who died increased after age 70 years in patients classified as moderate or severe on the RSEHA.
ConclusionsChest X-rays in patients with COVID-19 obtained in the emergency department are useful for determining the prognosis in terms of admission to the hospital, admission to the ICU, and mortality; radiologic patterns categorized as severe on the RSEHA are associated with greater mortality and admission to the ICU.
La pandemia por SARS-CoV-2 (COVID-19) ha sido un desafío diagnóstico en el que la radiografía de tórax ha tenido un papel muy relevante. El objetivo de este estudio es determinar si la escala radiológica de valoración de ingreso hospitalario (ERVI), aplicada a las radiografías de tórax de pacientes con COVID-19 a su llegada al servicio de urgencias, se relaciona con la gravedad de la COVID-19 en términos de necesidad de ingreso hospitalario, ingreso en unidad de cuidados intensivos (UCI) o la mortalidad.
Materiales y métodosSe ha realizado un estudio retrospectivo a 292 pacientes enfermos de COVID-19 que consultaron en el servicio de urgencias, en un período de mes y medio (del 16 de marzo al 30 de abril de 2020). Para estandarizar los patrones radiológicos, hemos utilizado la escala ERVI, categorizando el patrón radiológico en leve, moderado y grave. Se ha analizado la relación entre la gravedad radiológica según la escala ERVI y la necesidad de ingreso hospitalario, en UCI y la mortalidad.
ResultadosEl 91,4% de los pacientes precisaron ingreso. Existe una asociación estadísticamente significativa entre la escala ERVI y la necesidad de ingreso hospitalario (p = 0,03). El ingreso en UCI presenta una asociación significativa con la escala ERVI (p < 0,001). Han fallecido 51 (17,5%) pacientes, de los cuales el 57% presentaba una escala ERVI grave. Cuando estudiamos la mortalidad agrupando a los pacientes según su resultado en la escala ERVI y su rango de edad, el porcentaje de fallecidos aumenta a partir de los 70 años en los pacientes con una escala ERVI moderada y grave.
ConclusionesLa radiografía de tórax en pacientes con COVID-19 a su llegada al servicio de urgencias es una herramienta pronóstica en cuanto a la decisión de ingreso hospitalario, en UCI y mortalidad, de manera que las escalas ERVI graves tienen una mayor mortalidad e ingreso en UCI con una diferencia estadísticamente significativa.
In late 2019, several cases of pneumonia of unknown origin were recorded in Wuhan (China). Initially, the disease appeared to be restricted to neighbouring areas only, but in early 2020, the first cases outside of Asia were confirmed. On 30 January 2020, the World Health Organization (WHO) declared that the COVID-19 outbreak represented a public health emergency of international concern. On 11 March 2020, the WHO officially declared it a pandemic. The WHO has reported that Spain was one of the main European and global foci of the infection from mid March to April, the period during which this study was conducted.1
The coronavirus causes lung involvement that can be visualised as findings in radiological tests. Whereas computed tomography (CT) of the chest was used as a technique to diagnose COVID-19 infection in China,2,3 the Radiological Society of North America (RSNA), the American College of Radiology (ACR) and the Sociedad Española de Radiología Médica [Spanish Society of Medical Radiology] (SERAM) affirmed that, although CT is more sensitive, it should not be used as a first-line technique for COVID-19 diagnosis, given the technical and organisational complexities that it entails. These organisations instead recommended the use of chest X-ray for this purpose in patients with suspected COVID-19 due to symptoms of acute respiratory failure and/or fever.4,5 Radiology imaging was essential in supporting the diagnosis of the disease at a time when access to reverse transcription polymerase chain reaction (RT-PCR) for SARS-CoV-2 and access to serology tests were very limited due to their low availability.6
There are various scales for assessing SARS-CoV-2 infection on chest X-ray, as compiled by Wasilewski et al.7 in their review article.
The system for scoring the seriousness of radiological findings on chest X-ray reported by Taylor et al.8 was created in the pre-COVID-19 era, and its objective was to simplify radiological reports by grouping findings into five categories according to seriousness in patients hospitalised with acute respiratory infection.
Wong et al.9 adapted and simplified the Radiographic Assessment of Lung Edema (RALE) scale10 in order to describe the course and seriousness of radiological findings in the chest in COVID-19 and correlate them with RT-PCR test results.
The scoring system in chest X-ray proposed by Borghesi et al.11 is the only method to date designed specifically for evaluating chest X-rays in patients with COVID-19.
In addition, the British Society of Thoracic Imaging was behind the development of a standardised chest X-ray report in view of the need to use common language when assessing radiological findings in patients with COVID-19. The report uses the terms "possible pattern", "indeterminate" and "alternative diagnosis" but makes no mention of the prognostic value of X-ray.12
This study used the Escala Radiológica de Valoración de Ingreso Hospitalario [Radiological Scale for Assessment of Hospital Admission] (ERVI) proposed by Dr Catalá in his revised ERVI SCALE tutorial13 to assess the seriousness of COVID-19 based on the opacities visible on chest X-ray. The objective of this study is to determine whether the ERVI scale applied to chest X-rays in patients with COVID-19 on arrival in the accident and emergency department is related to the seriousness of the disease in terms of need for hospital admission, intensive care unit (ICU) admission and death.
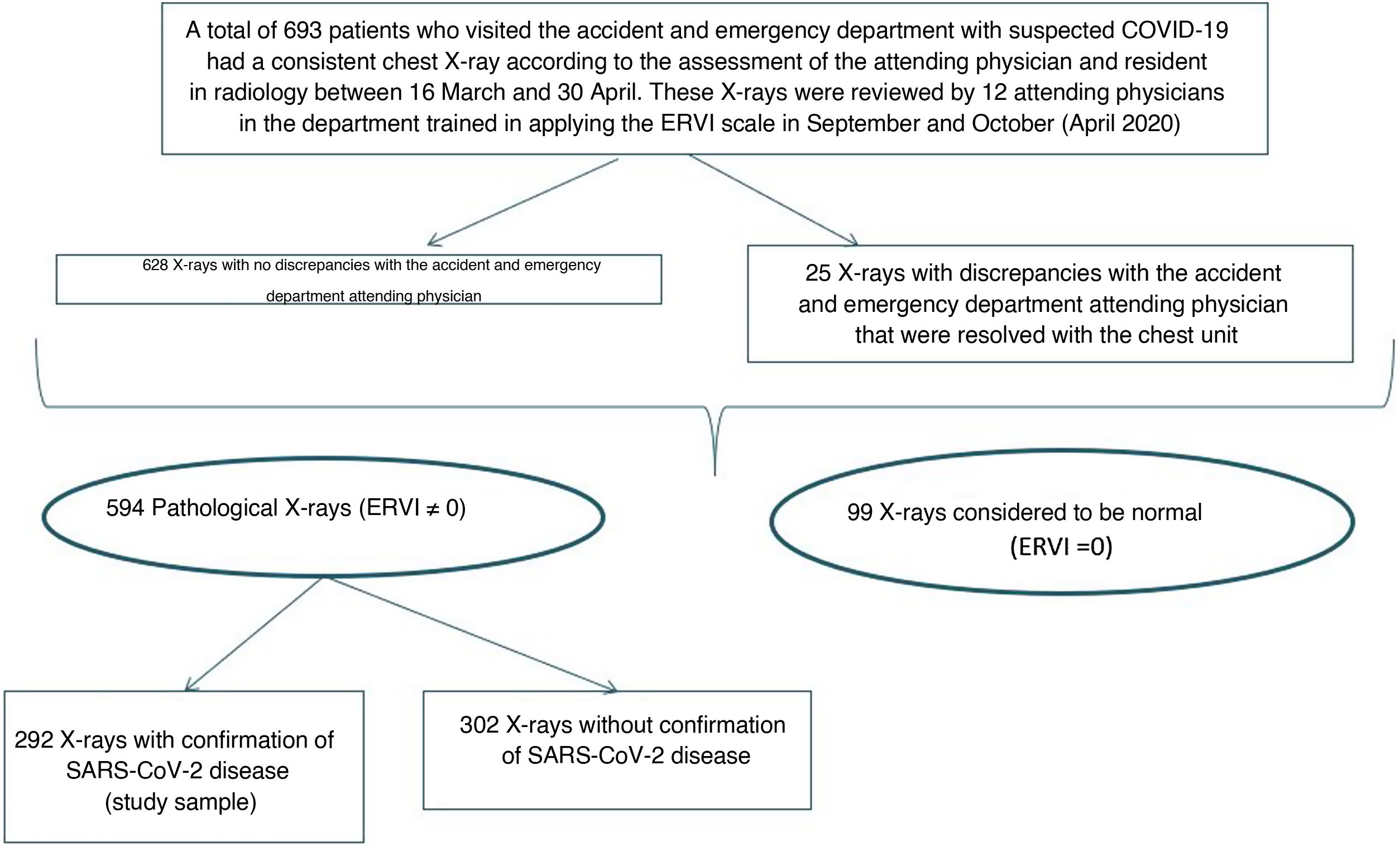
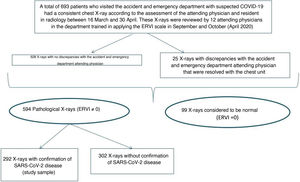
Material and methodsWe conducted a retrospective observational study of patients who consecutively visited the accident and emergency department at our hospital with signs and symptoms consistent with COVID-19 between 16 March and 30 April 2020. Patients underwent a posteroanterior and lateral or anteroposterior chest X-ray, in those cases that required it (patients unable to remain standing and X-rays taken with portable equipment). During that period, 693 patients were recorded to have signs and symptoms consistent with COVID-19 and undergo a chest X-ray; their chest X-rays were reported by the resident and the attending physician on duty. Later on, in September and October 2020, all the chest X-rays included in the database were reviewed by a second radiologist in the department, who applied the ERVI scale. In cases of discrepancies between the initial chest X-ray report and the review by the second radiologist, a third radiologist from the chest unit was asked to conduct an assessment. Just 25 X-rays (8.6%) required an assessment by the radiologist from the chest unit.
The ERVI scale developed by Dr Catalá13 assesses the seriousness of the disease based on the characteristics of the chest X-ray. This scale only takes into account lesions consistent with COVID-19 on chest X-ray, i.e. opacities, increased focal or diffuse density, or an alveolar–interstitial pattern.
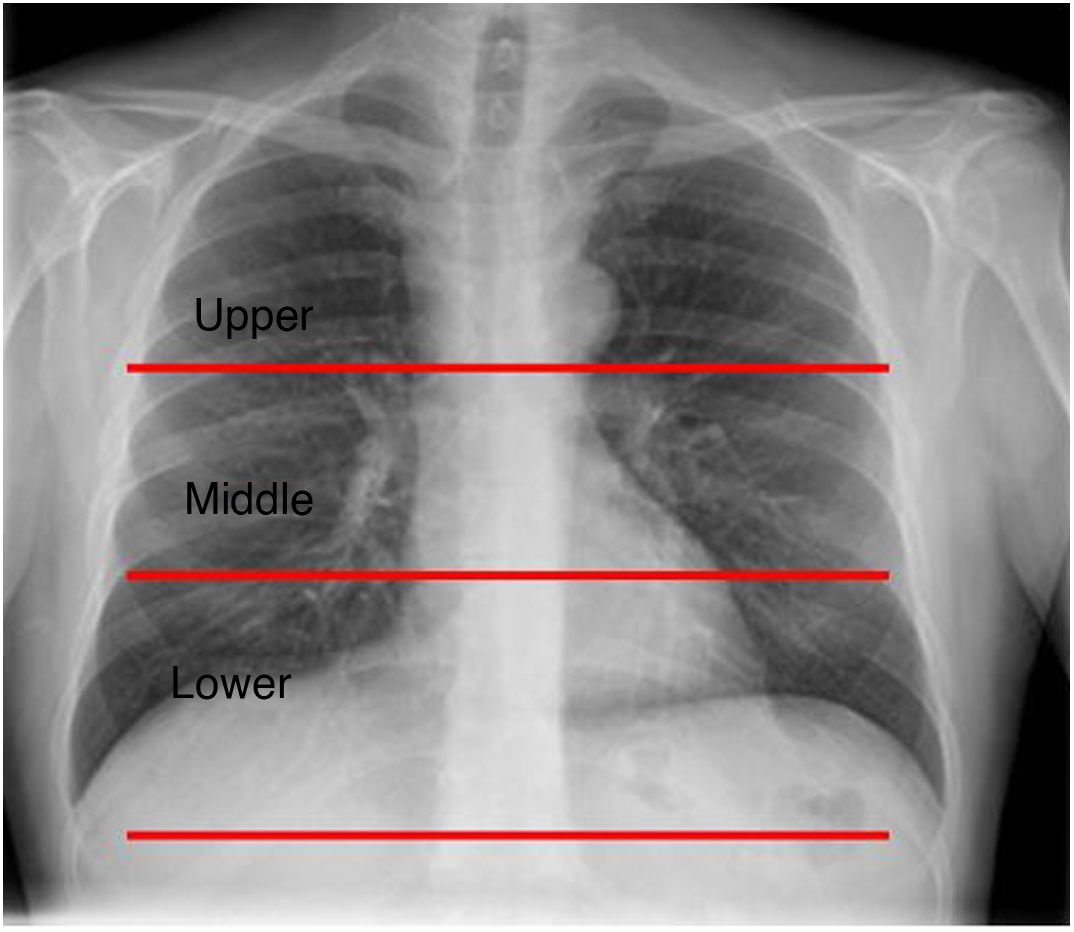
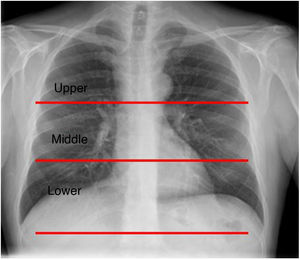
Each anteroposterior or posteroanterior X-ray was divided into three lung fields (upper, middle and lower) (Fig. 1).
Lung division on posteroanterior chest X-ray. This image illustrates the delimitations of the upper, middle and lower fields required to apply the ERVI scale. The upper field is above a horizontal line that passes through the carina, the lower field is below a horizontal line that passes through the lower pole of the right hilum, and the middle field is the space between the two lines.
The ERVI scale assigns a score in the following manner:
- a
No lesions (0 points).
- b
Unilateral with fewer than 3 lesions of any type or fewer than 3 lung fields affected. a + b (1 point).
- c
Unilateral with 3 or more lesions of any type or all 3 lung fields affected (3 points).
- d
Bilateral: lung fields with opacities or lesions as described in section b would be b + b (2 points); a lung field with an opacity as in section b and another opacity as in section c would be b + c (4 points).
- e
Add 1 additional point if three or more lung fields are affected between both lungs.
- f
Add 1 additional point if there is consolidation (this may indicate bacterial pneumonia or concomitant infection), lymphadenopathy or pleural effusion, or progression to acute respiratory distress syndrome (ARDS) in follow-up.
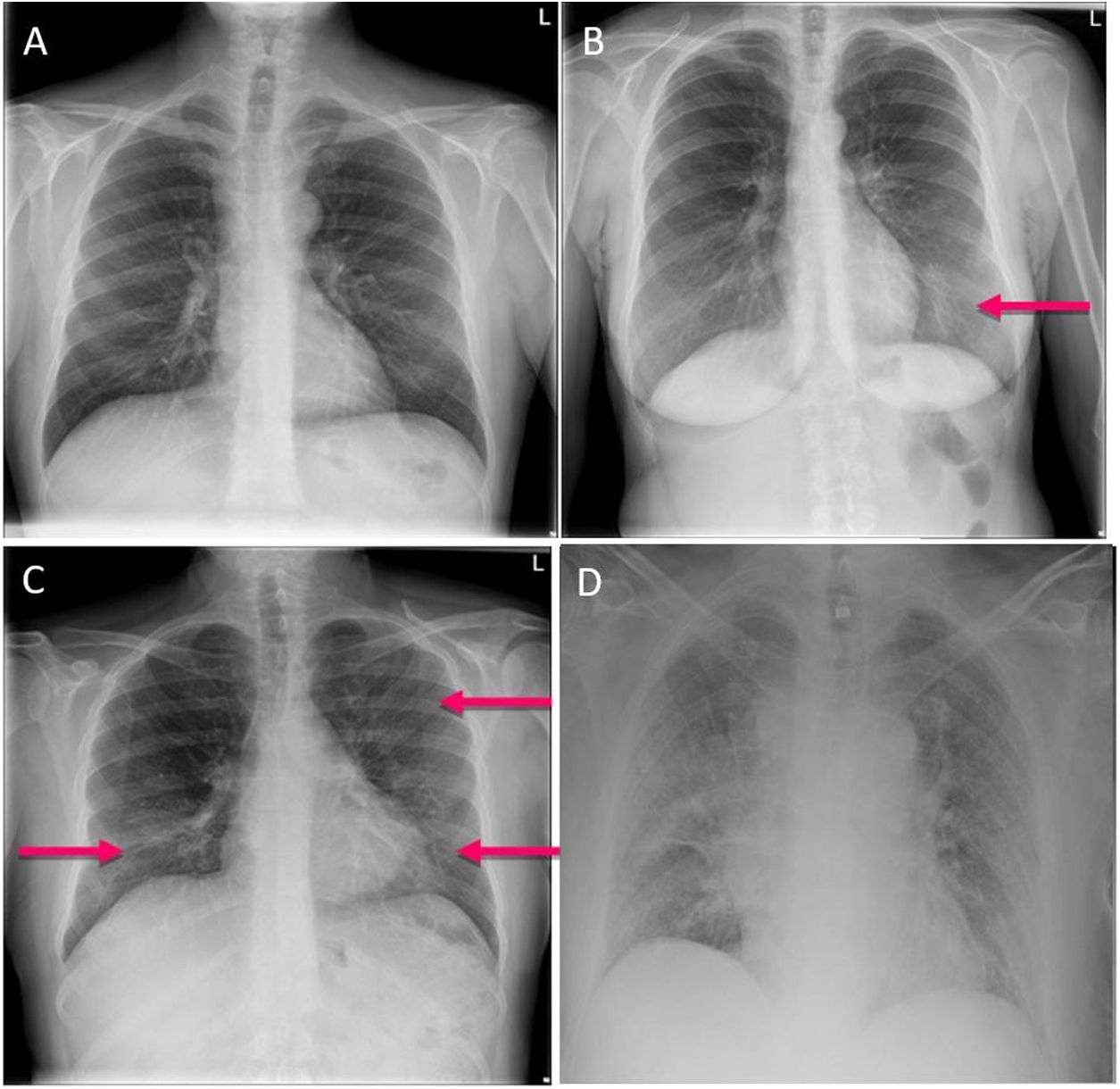
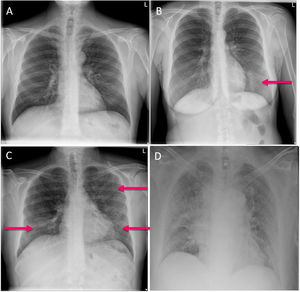
The total score ranges from 0 to 8. A score on the ERVI scale of 1–2 is considered mild, a score of 3–5 is considered moderate and a score of 6–8 is considered serious (Fig. 2).
Of the 693 patients with clinically suspected COVID-19, 99 had a score of 0 on the ERVI scale; these patients were not included in this study. Among the 594 remaining patients, a total of 302 patients in whom the disease was not confirmed were excluded. Patients with a positive RT-PCR test or serology testing positive for immunoglobulins (IgG or IgM) were considered COVID-19 patients. Our study focused on the 292 patients with confirmed SARS-CoV-2 infection with a score higher than 0 on the ERVI scale (Fig. 3).
In order to collect the required data, the patients' medical records were reviewed and the following variables were recorded: age (stratified by 10-year age groups), gender, date of visit to the accident and emergency department, ERVI score, need for hospital admission, need for ICU admission and mortality.
Statistical analysisThe Statistical Package for the Social Sciences (SPSS) computer program was used; associations were studied using the χ2 test (applied to age, ERVI score, need for admission, need for ICU admission and mortality). A p-value <0.05 was used for rejecting the null hypothesis, with the differences observed being significant with a probability of error less than 5% (type 1 error).
Ethical considerationsThe study was conducted in compliance with good clinical practice guidelines according to the recommendations of the Declaration of Helsinki and Spanish Law 41/2002 on patient autonomy. Sensitive data were anonymised to maintain patient privacy. The approval of the provincial independent ethics committee was sought. As this was a retrospective study, patients were not asked to grant their informed consent.
ResultsThe study sample consisted of 292 patients: 166 (56.8%) men and 126 (43.2%) women, with a mean age of 62.14 years (standard deviation [SD]: 15.12).
All the patients studied had been diagnosed with SARS-CoV-2 infection, either by RT-PCR testing of a nasal swab or by serology testing of antibodies in blood. In just seven patients (2.4%), PCR testing was negative and serology testing was positive for IgG.
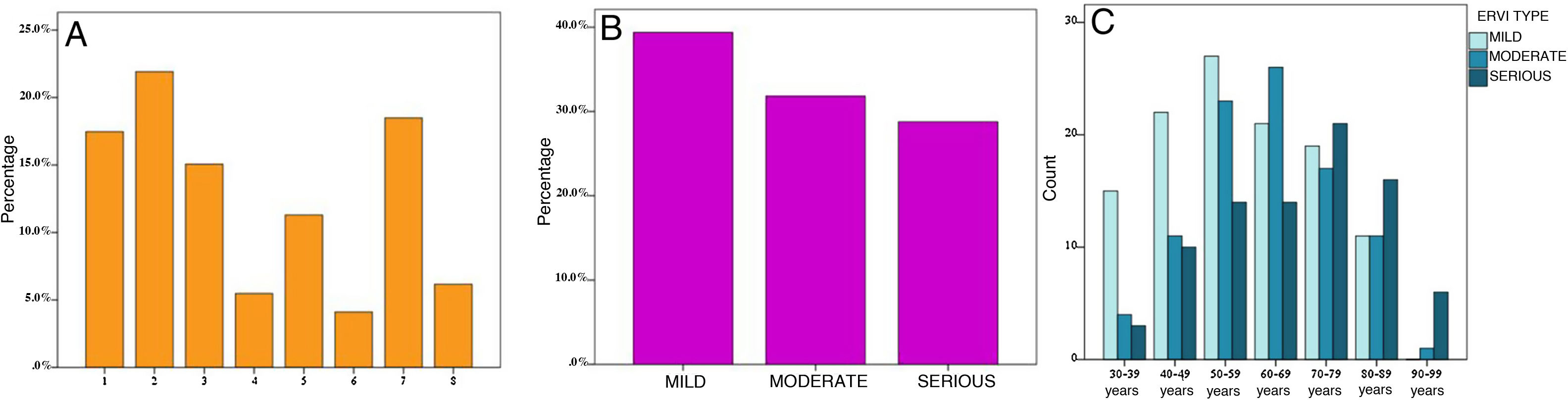
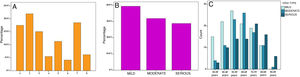
Opacities on chest X-ray were measured using the ERVI scale (Fig. 4A). When the ERVI scores for these patients were grouped according to the seriousness that they represented, it was determined that 115 (39.4%) patients had a mild ERVI score, 93 (31.8%) had a moderate ERVI score and 84 (28.8%) had a serious ERVI score (Fig. 4B). Analysis of ERVI scores by age revealed significant differences (p = 0.002); serious ERVI scores were more common in patients in the 70–79 and the 80–89 age groups, and mild ERVI scores were more common in those under 50 years of age (Fig. 4C).
ERVI score on admission in the patients in the sample. A) Bar chart representing percentages of patients with each ERVI score (1–8). B) Bar chart representing percentages of patients with mild, moderate and serious ERVI scores. C) Bar chart representing numbers of patients with mild, moderate and serious ERVI scores according to age groups.
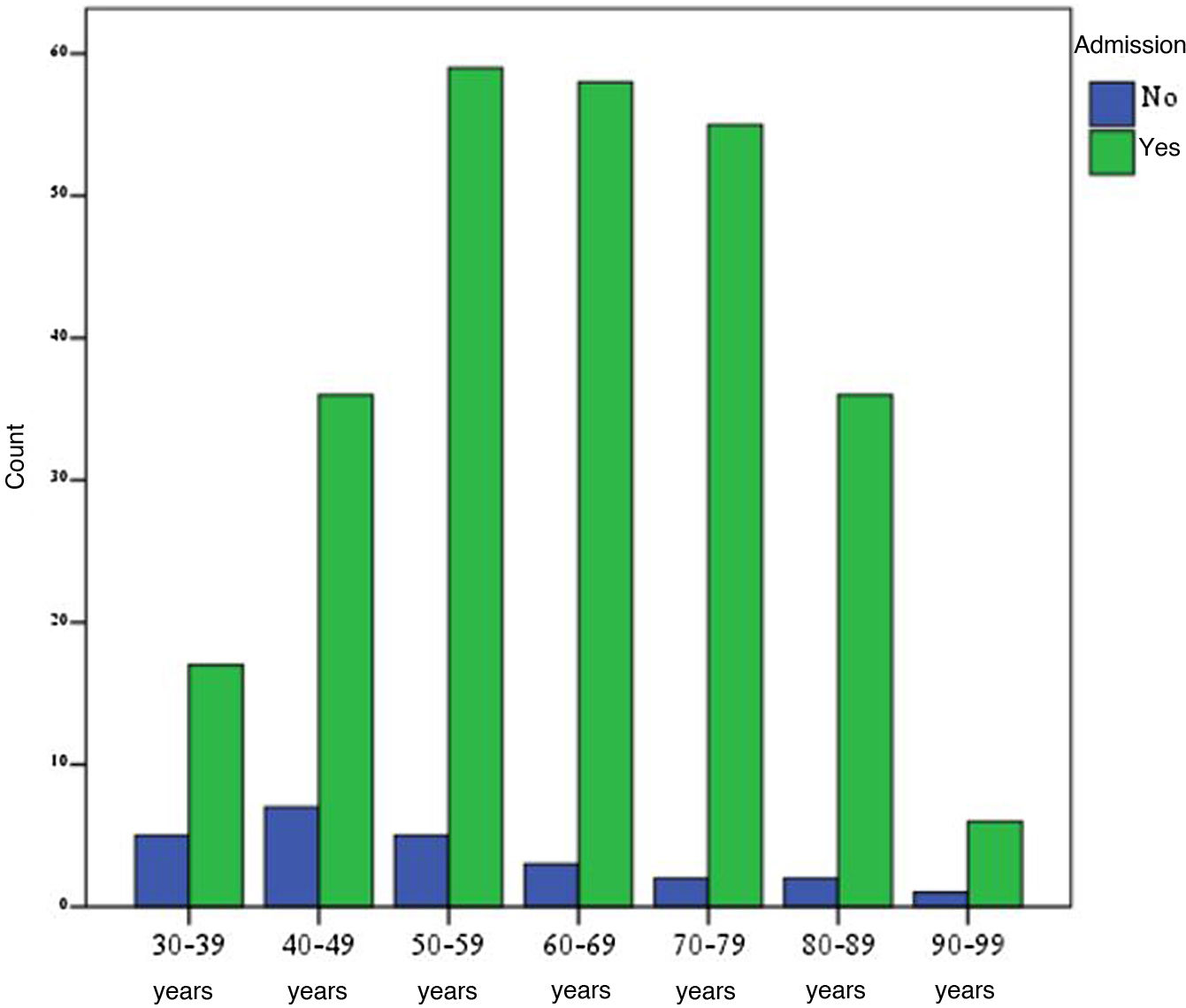
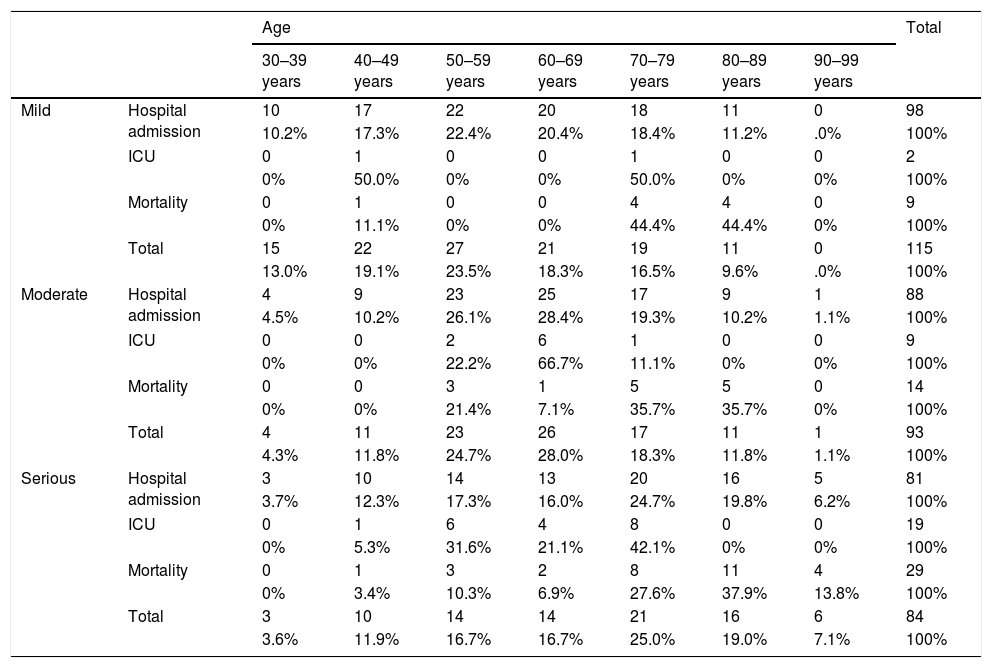
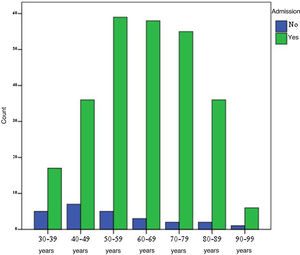
A total of 267 (91.4%) patients required hospital admission; of them, 58.8% were men, with a statistically significant difference (p = 0.028). There was also a statistically significant relationship between ERVI score and need for hospital admission (p = 0.003). Hospital admission was required for 85.2% of patients with a mild ERVI score, 94.6% with a moderate ERVI score and 96.4% with a serious ERVI score. The majority of admitted patients were 50–79 years of age (64%) (Fig. 5). Patients in the 50–59 age group had a higher percentage of mild ERVI scores than patients in the 70–79 and 80–89 age groups, who had higher percentages of serious ERVI scores (Table 1).
Classification of patients by ERVI score and age, assessing need for hospital admission, need for ICU admission and mortality.
| Age | Total | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| 30–39 years | 40–49 years | 50–59 years | 60–69 years | 70–79 years | 80–89 years | 90–99 years | |||
| Mild | Hospital admission | 10 | 17 | 22 | 20 | 18 | 11 | 0 | 98 |
| 10.2% | 17.3% | 22.4% | 20.4% | 18.4% | 11.2% | .0% | 100% | ||
| ICU | 0 | 1 | 0 | 0 | 1 | 0 | 0 | 2 | |
| 0% | 50.0% | 0% | 0% | 50.0% | 0% | 0% | 100% | ||
| Mortality | 0 | 1 | 0 | 0 | 4 | 4 | 0 | 9 | |
| 0% | 11.1% | 0% | 0% | 44.4% | 44.4% | 0% | 100% | ||
| Total | 15 | 22 | 27 | 21 | 19 | 11 | 0 | 115 | |
| 13.0% | 19.1% | 23.5% | 18.3% | 16.5% | 9.6% | .0% | 100% | ||
| Moderate | Hospital admission | 4 | 9 | 23 | 25 | 17 | 9 | 1 | 88 |
| 4.5% | 10.2% | 26.1% | 28.4% | 19.3% | 10.2% | 1.1% | 100% | ||
| ICU | 0 | 0 | 2 | 6 | 1 | 0 | 0 | 9 | |
| 0% | 0% | 22.2% | 66.7% | 11.1% | 0% | 0% | 100% | ||
| Mortality | 0 | 0 | 3 | 1 | 5 | 5 | 0 | 14 | |
| 0% | 0% | 21.4% | 7.1% | 35.7% | 35.7% | 0% | 100% | ||
| Total | 4 | 11 | 23 | 26 | 17 | 11 | 1 | 93 | |
| 4.3% | 11.8% | 24.7% | 28.0% | 18.3% | 11.8% | 1.1% | 100% | ||
| Serious | Hospital admission | 3 | 10 | 14 | 13 | 20 | 16 | 5 | 81 |
| 3.7% | 12.3% | 17.3% | 16.0% | 24.7% | 19.8% | 6.2% | 100% | ||
| ICU | 0 | 1 | 6 | 4 | 8 | 0 | 0 | 19 | |
| 0% | 5.3% | 31.6% | 21.1% | 42.1% | 0% | 0% | 100% | ||
| Mortality | 0 | 1 | 3 | 2 | 8 | 11 | 4 | 29 | |
| 0% | 3.4% | 10.3% | 6.9% | 27.6% | 37.9% | 13.8% | 100% | ||
| Total | 3 | 10 | 14 | 14 | 21 | 16 | 6 | 84 | |
| 3.6% | 11.9% | 16.7% | 16.7% | 25.0% | 19.0% | 7.1% | 100% | ||
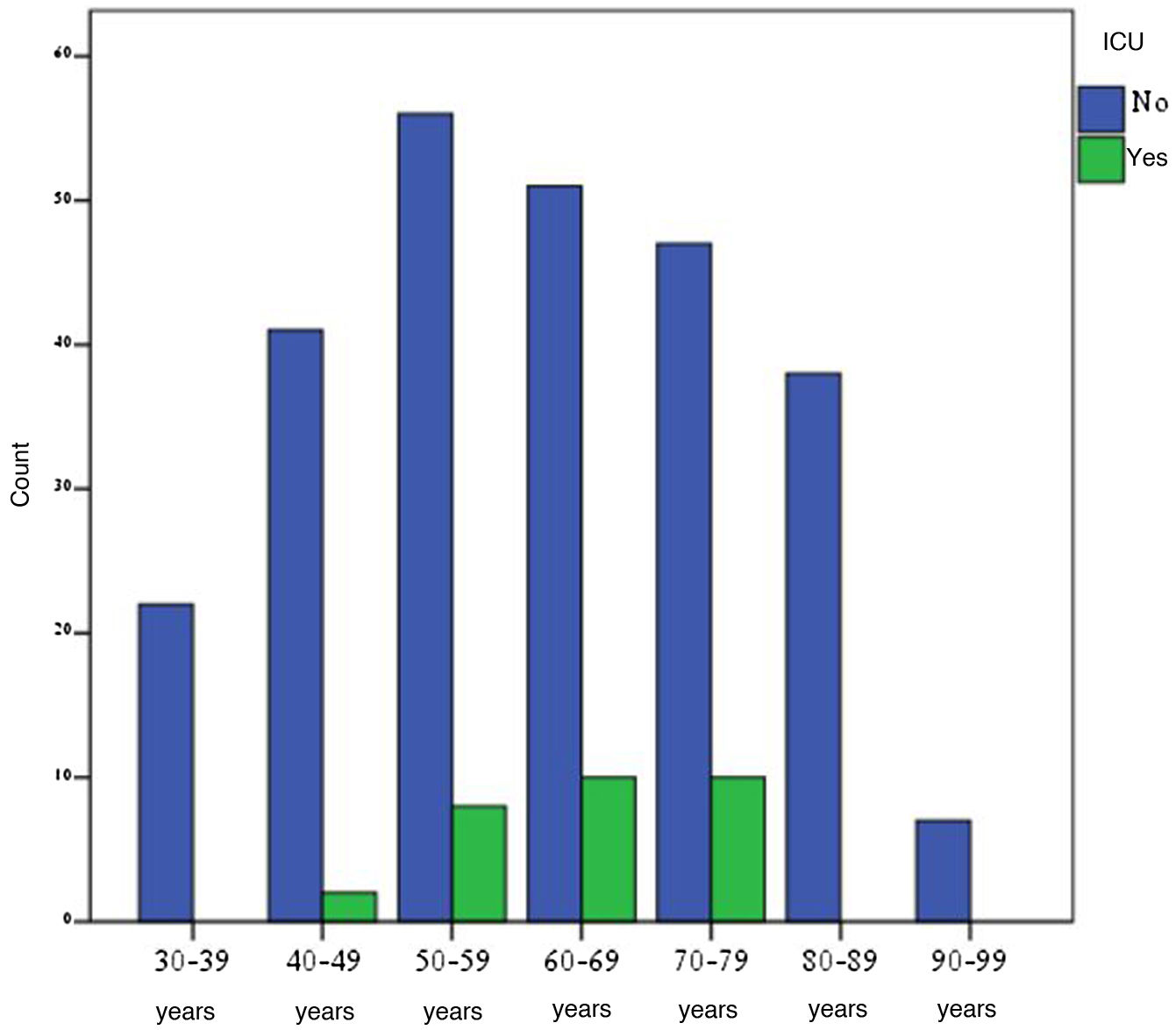
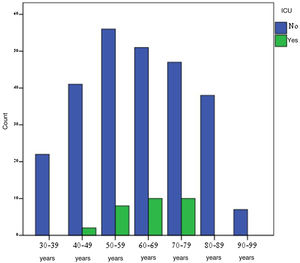
A total of 30 (10.3%) patients required ICU admission; of them, 76.7% were men, with a statistically significant difference (p = 0.028). When this hospital admission was stratified by age group, statistically significant differences were found between ERVI score and ICU admission (p < 0.001). The majority of ICU-admitted patients were 50–79 years of age (93.3%) (Fig. 6). Nineteen ICU-admitted patients (63.3%) had a serious ERVI score (Table 1).
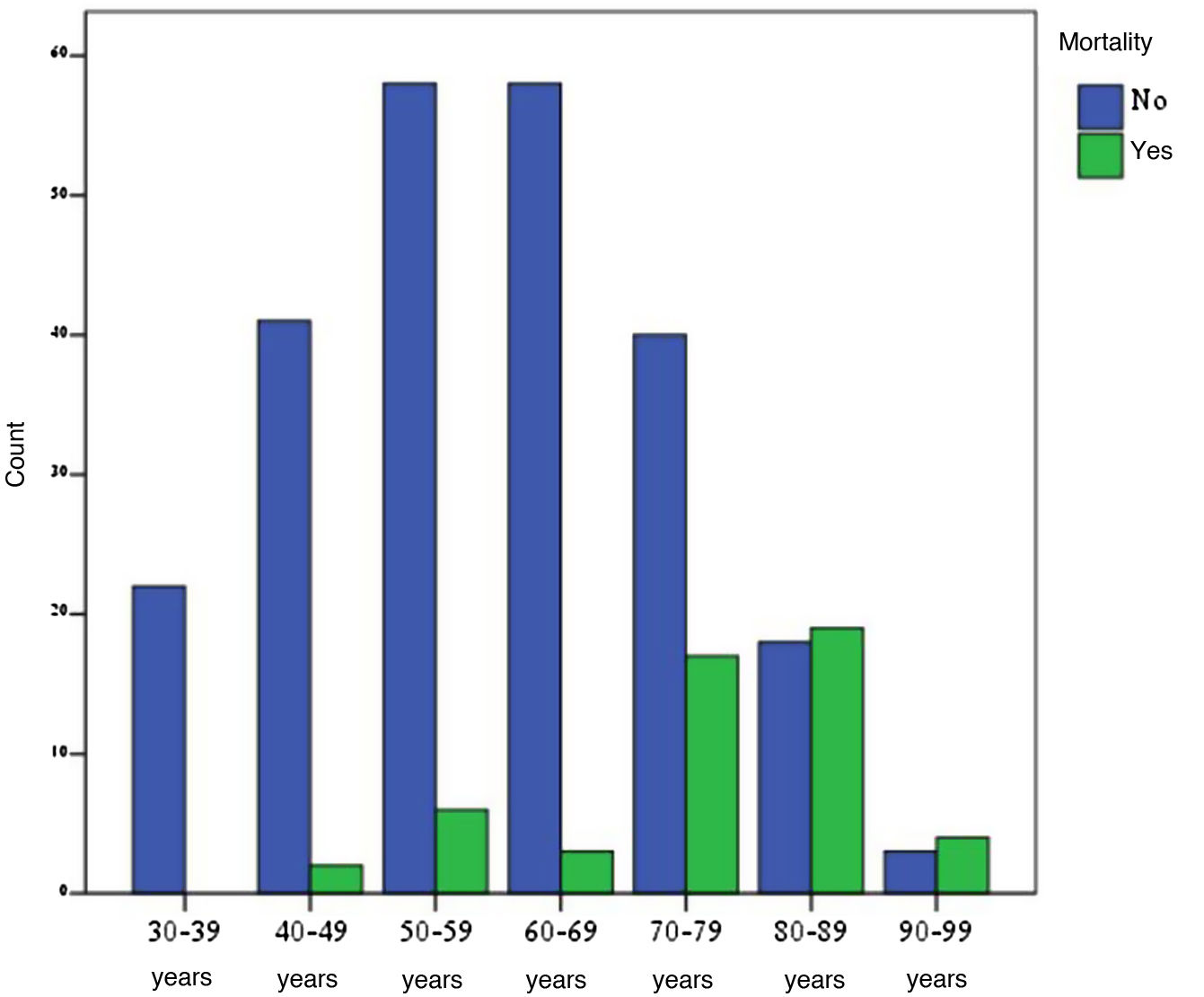
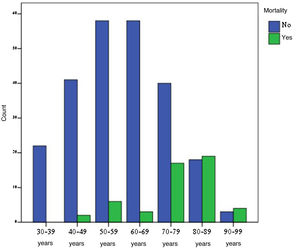
Fifty-one patients (15.5%) died; no statistically significant differences were found between mortality and gender. A breakdown of mortality by ERVI score revealed that the highest percentage of deaths (56.9%) had been given a serious ERVI score, 25.5% had been given a moderate ERVI score and the remaining 17.6% had been given a mild ERVI score. The association between mortality and the different degrees of seriousness of the ERVI scale was statistically significant in all groups (p < 0.001) (Table 1).
Analysis of patient mortality by age, irrespective of ERVI score, found a higher rate of mortality in the 70–79 and 80–89 age groups (exceeding 50%), with mortality being higher in patients 80–89 years of age with serious ERVI scores (68.75%) (Fig. 7). Among patients under 70 years of age, 21.2% died (accounting for 11 of the 52 patients who died); just one of them had a mild ERVI score (Table 1).
DiscussionThe purpose of this study was to determine whether chest X-ray has prognostic value in patients with COVID-19. To this end, we standardised chest X-ray results using the ERVI scale. All chest X-rays taken in COVID-19 patients who visited the accident and emergency department during the first wave of the pandemic, over a period of a month and a half, were analysed. Need for hospital admission, ICU admission and mortality were assessed as prognostic markers. According to our results, the ERVI scale had prognostic value with statistically significant differences in relation to ERVI score (mild, moderate and serious) and need for hospital admission, need for ICU admission and death. The group of patients over 80 years of age had the highest mortality rate and the highest percentage of serious ERVI scores.
One of the difficulties of comparing chest X-ray results is the lack of a common language, necessitating a standardised report to enable mutual understanding between radiologists and clinicians. Consequently, various scales that measure the seriousness of radiological findings have appeared in the scientific literature during times of pandemic; however, not all of them have prognostic value. Different scales have been used to assess the extent of pneumonia.7–11 A review of the literature did not turn up any article using the ERVI scale. The only scale specifically developed for COVID-19 is that of Borghesi et al.11 All the other scales cited in the introduction are adaptations of other scales to COVID-19. The ERVI scale was developed specifically for COVID-19, it is easy to administer, it has good interobserver concordance in preliminary studies, and the score obtained is useful for predicting mortality.13 Although we did not conduct concordance studies as such, the experience of the radiologists who participated in the review of the chest X-rays did differ greatly; despite this, there were discrepancies between the initial report and the review by the second radiologist in just 25 chest X-rays (8.6%).
However, during the first wave of the pandemic, the majority of hospitals used chest X-ray to aid in the diagnosis of SARS-CoV-2 pneumonia. As this study showed, a systematic assessment of this using the ERVI scale also offers prognostic value in relation to the disease. In a series of 104 patients with COVID-19 confirmed by RT-PCR, Kerpel et al. found that lung opacities on chest X-rays, measured using the RALE scale, were correlated with disease prognosis in terms of need for ICU admission, need for intubation and mortality.14 In China, CT has been used as a tool with prognostic value, in addition to diagnostic utility, as the extent of pneumonia on CT scans predicts mortality and may facilitate the screening of patients who require closer monitoring and more aggressive treatment.15
Patients with a serious ERVI score had higher rates of ICU admission; this difference was statistically significant. Authors such as Cozzi et al., who used the RALE scale to assess seriousness in patients with COVID-19, also found a statistically significant relationship between X-ray pattern and need for ICU admission in the most seriously ill patients, as in our series.17 The most affected patients in that series were in the 60–79 age group, and patients over 80 years of age had high percentages of hospital admission similar to ours. A total of 34 (15.3%) patients died in the 30-day period of that study. Its results were consistent with those of our series. However, mortality results differed: Cozzi et al.’s study found that mortality was higher in men, whereas our study did not find gender-based differences.
For Hui et al., a chest X-ray taken between the sixth and tenth day from the onset of symptoms was a good predictor of serious disease.16 In our series, we did not collect the symptoms onset date, although the chest X-ray taken in the accident and emergency department also proved a good predictor of serious disease.
Our results, consistent with those of other authors, demonstrated that chest X-ray is a prognostic tool, especially in cases of serious disease.16–22 Although our study did not evaluate the diagnostic utility of chest X-ray, several authors have emphasised that if serology testing for confirmation purposes is not available during the pandemic, chest X-ray may be useful for guiding diagnosis and clinical decision-making in patients with suspected COVID-19.10,11,14–17 We believe that the ERVI scale applied to chest X-ray is useful for predicting the prognosis of patients with COVID-19 as of their admission to the accident and emergency department and may help to guide their clinical management early on.
We feel that the limitations of our study had to do with the sample studied, since testing to confirm a diagnosis of COVID-19 was preferentially performed in the most seriously ill patients given its limited availability, thus running a risk of bias in studying only patients with confirmed disease. Another limitation of the study was that the X-rays were not assessed by radiologists with expertise in chest radiology, which might have influenced their appraisal of the findings. The study’s retrospective nature might also have posed a risk of selection bias, as it was known in advance that the patients were COVID-19 patients, while their ages were also known.
ConclusionsChest X-ray in patients with COVID-19 on arrival in the accident and emergency department was a prognostic tool in relation to hospital admission, ICU admission and mortality; serious ERVI scores showed a statistically significant association with higher rates of mortality and ICU admission.
FundingThis study received no specific grants from public agencies, the commercial sector or non-profit organisations.
Authorship- 1
Responsible for study integrity: AA, TD, DD.
- 2
Study conception: AA, TD, DD.
- 3
Study design: AA.
- 4
Data collection: EC, MMG, MLB.
- 5
Data analysis and interpretation: AA, TD.
- 6
Statistical processing: AA, TD, DD.
- 7
Literature search: EC, MMG.
- 8
Drafting of the article: AA, TD.
- 9
Critical review of the manuscript with intellectually significant contributions: AA, TD, EC, MMG, MLB, DD.
- 10
Approval of the final version: AA, TD.
The authors declare that they have no conflicts of interest.
We would like to thank all the professionals who helped to make our study possible.
Please cite this article as: Adarve Castro A, Díaz Antonio T, Cuartero Martínez E, García Gallardo MM, Bermá Gascón ML, Domínguez Pinos D. Utilidad de la radiografía de tórax para evaluar el pronóstico de pacientes con COVID-19. Radiología. 2021;63:476–483.