Endovascular treatment with mechanical thrombectomy devices demonstrated high recanalization rates but functional outcome did not correlate with high rates of recanalization obtained. Patient selection prior to the endovascular treatment is very important in the final outcome of the patient. The primary aim of our study was to evaluate the prognostic value of posterior circulation Alberta Stroke Program Early CT Score (pc-ASPECTS) and Pons-Midbrain Index (PMI) scores in patients with Basilar Artery Occlusion (BAO) treated with successful angiographic recanalization after mechanical thrombectomy.
MethodsRetrospective single-centre study including 18 patients between 2008 and 2013 who had acute basilar artery occlusion managed with endovascular treatment within 24h from symptoms onset and with successful angiographic recanalization. The patients were initially classified into two groups according to clinical outcome and mortality at 90 days. For analysis we also divided patients into groups based on pc-ASPECTS (≥8 vs. <8) and PMI (≥3 vs. <3) on non-contrast CT (NCCT) and CT Angiography Source Images (CTASI). Imaging data were correlated to clinical outcome and mortality rate.
ResultsCTASI pc-ASPECTS, dichotomized at <8 versus ≥8, was associated with a favourable outcome (RR: 2.6; 95% CI: 1.3–5.2) and a reduced risk of death (RR: 6.5: 95% CI: 7.8–23.3). All patients that survived and were functionally independent had pc-ASPECTS score ≥8. None of the 5 patients with CTASI pc-ASPECTS score less than 8 survived.
ConclusionPC-ASPECTS on CTASI is helpful for predicting functional outcome after BAO recanalization with endovascular treatment. These results should be validated in a randomised controlled trial in order to decide whether or not to treat a patient with BAO.
El tratamiento endovascular con dispositivos de trombectomía mecánica demostró altos índices de recanalización, si bien el resultado funcional no guardó relación con los altos índices de recanalización obtenidos. La selección de los pacientes previa al tratamiento endovascular es muy importante en el resultado final de estos pacientes. El objetivo principal de nuestro estudio fue hacer una valoración del valor pronóstico de la escala ASPECTS (Escala Precoz por TC del Programa de ACV de Alberta) y del índice puente-mesencéfalo (IPM) en pacientes con oclusiones de la arteria basilar (OAB) sometidos, con éxito, a recanalización angiográfica tras trombectomía mecánica.
MétodosEste estudio retrospectivo de un único centro incluyó 18 pacientes entre los años 2008 y 2013 con oclusiones de la arteria basilar que fueron sometidos a tratamiento endovascular dentro de las 24 horas siguientes al inicio de los síntomas y con una exitosa recanalización angiográfica. Inicialmente, los pacientes fueron clasificados en dos grupos según el resultado clínico y la mortalidad a los 90 días. Para el análisis, los pacientes también fueron divididos en grupos de imágenes utilizando, para ello, la escala ASPECTS-CP (≥8 vs. <8) y el IPM (≥3 vs. <3) mediante tomografías computarizadas sin contraste (TCSC) e imágenes fuente de la angio-TC (IFATC). Los datos de las imágenes se compararon tanto con los resultados clínicos como con la tasa de mortalidad.
ResultadosLa escala ASPECTS-CP mediante IFATC, dicotomizada a <8 vs. ≥8, se asoció a un resultado favorable (riesgo relativo [RR]: 2,6; intervalo de confianza [IC] del 95%: 1,3–5,2), así como a un menor riesgo de mortalidad (RR: 6,5; IC del 95%: 7,8–23,3). La puntuación en la escala ASPECTS-CP de todos los pacientes que sobrevivieron y fueron funcionalmente independientes fue igual o superior a 8. Ninguno de los cinco pacientes con puntuaciones en la escala ASPECTS-CP mediante IFATC por debajo de 8 sobrevivió.
ConclusiónLa escala ASPECTS-CP mediante IFATC sirve de ayuda a la hora de predecir el resultado funcional tras recanalización de la OAB mediante tratamiento endovascular. Estos resultados deberían ser validados en un ensayo controlado aleatorizado para decidir si tratar, o no, a un paciente con OAB.
Basilar artery occlusion (BAO) is an extremely severe subtype of stroke with high mortality and disability rates.1,2 Recanalization has become one of the most important predictors of favourable outcomes in patients with BAO.2–6 Endovascular treatment with mechanical thrombectomy devices results in high rates of recanalization (64–100%).7–9 Nevertheless, the functional outcome continues to follow the pattern of the high rates of recanalization obtained through mechanical thrombectomy. Patient selection according to their clinical status prior to endovascular treatment is of great importance to the patient's eventual outcome. Clinical parameters such as confirmed ischaemic lesions, state of coma and its duration, and the need for endotracheal intubation have been found to be crucial factors in the eventual outcome of patients with acute BAO.2–5,10,11
Unlike in the anterior circulation,12 there is currently no consensus regarding which patients with acute BAO would benefit from endovascular treatment. Recent randomised controlled trials have demonstrated that victims of ischaemic stroke secondary to occlusion of a proximal vessel of the anterior circulation (internal carotid artery or middle cerebral artery) benefit from endovascular treatment up to 24h after the onset of symptoms.12–14 The anterior circulation ASPECTS (Alberta Stroke Program Early CT Score) scale helps to predict which patients will have good clinical outcomes after mechanical thrombectomy among patients with occlusions of the large vessels of the anterior circulation.
The posterior circulation ASPECTS (pc-ASPECTS) scale is a semi-quantitative scale that has been shown to be capable of predicting favourable outcomes, mortality rate and eventual infarction grade in patients with BAO.15–17 In patients with a posterior circulation stroke, the pc-ASPECTS scale used in conjunction with non-contrast computed tomography (NCCT) did not demonstrate sufficient sensitivity to be used as a screening tool for endovascular treatment. However, the pc-ASPECTS scale used in conjunction with CT angiography source images (CTASI) has shown promising preliminary results in the prediction of eventual ischaemic lesions.16 Three different studies,15–17 conducted by the same group of investigators, suggest that the pc-ASPECTS with CTASI may be useful as a screening tool for endovascular treatment in patients with acute BAO, although this has not been fully demonstrated. The pons-midbrain index (PMI) is another semi-quantitative scale capable of predicting clinical outcome in patients with acute vertebrobasilar artery occlusion, using CTASI to do so, although this scale's utility has only been demonstrated in a single study18 (Fig. 1).
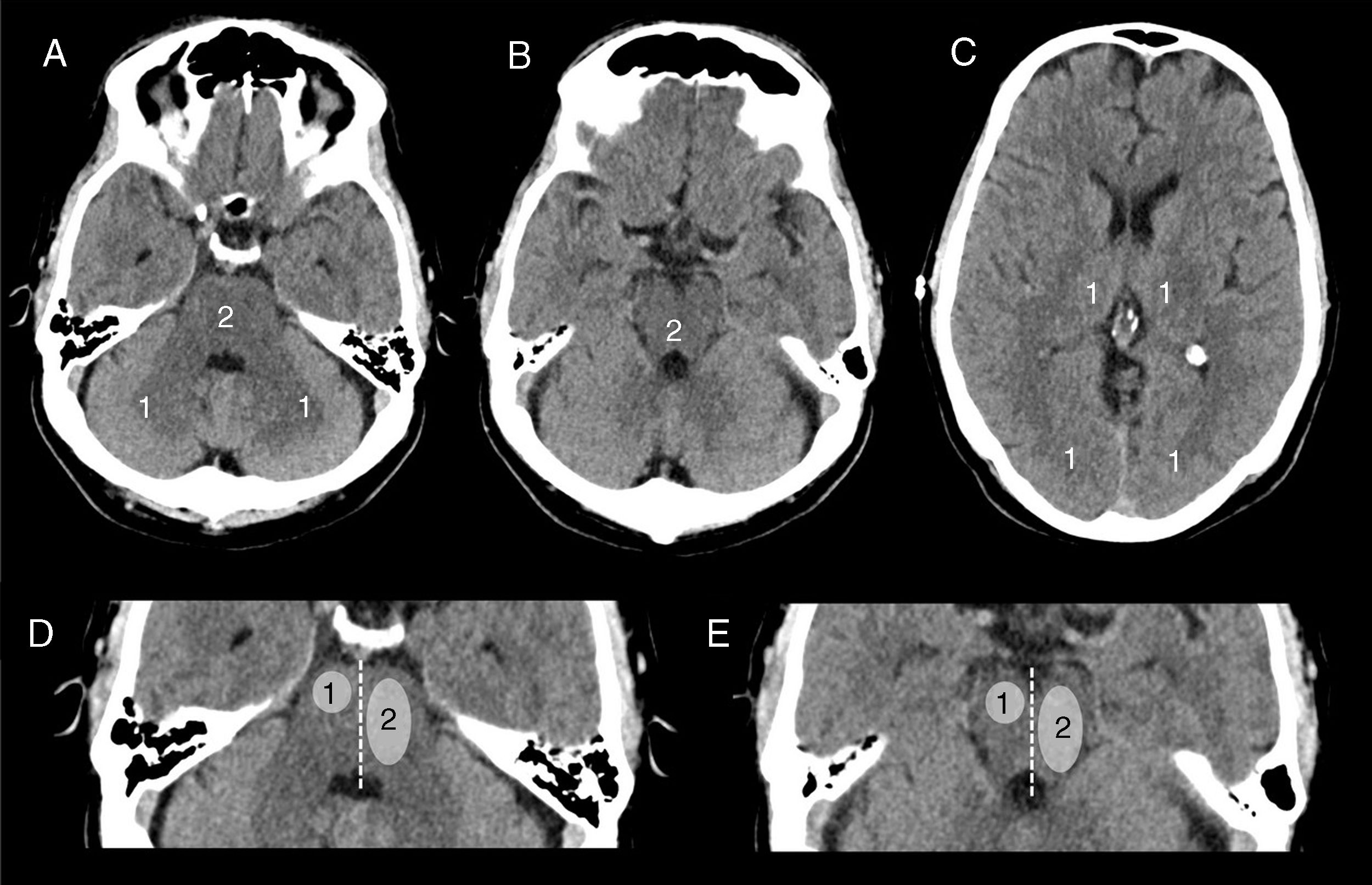
ASPECTS (Alberta Stroke Program Early CT Score) scale (A, B and C) and pons-midbrain index (PMI) (D and E). On the pc-ASPECTS scale, we deducted one or two points depending on the territory affected: right or left thalamus, cerebellum or the territory of the posterior cerebral artery (one point); any part of the midbrain or pons (two points). A score of ten indicates a normal scan. On the PMI, we divided the pons and midbrain into two territories each (left and right). We assigned one point when 50% or less of the territory was affected and two points if more than 50% of the territory was affected. A score of zero indicated a normal scan.
Our hypothesis is that CTASI may help to predict the clinical outcome of patients with acute BAO prior to endovascular treatment. Given the difficulty of conducting randomised clinical trials in patients with acute BAO, both for ethical reasons and due to the low incidence of the disease, it is important to have as much information as possible for the management of these patients.
Consequently, the validation of a tool for the identification of patients who might benefit from endovascular treatment must play a fundamental role in the management of these patients. The principal objective of our study was to assess the prognostic value of the pc-ASPECTS scale and the PMI in patients with BAO who successfully underwent angiographic recanalization after mechanical thrombectomy.
Material and methodsPatient selectionWe conducted a single-centre retrospective study of 22 patients with acute BAO treated at our centre between November 2008 and July 2013. The patients enrolled had BAO confirmed by digital subtraction angiography, received endovascular treatment within the 24h following the onset of symptoms and successfully underwent angiographic recanalization (mTICI 2b–3).19 In all the stroke victims, the clinical and imaging assessments were conducted according to our unit's stroke management clinical protocol. The clinical assessment was performed by a neurologist specialising in stroke management on arrival at the hospital, with the presence of BAO being associated with severe neurological deficit defined by a score of more than 6 on the National Institutes of Health Stroke Scale (NIHSS) and a score of 2 or less on the modified Rankin scale (mRS). The exclusion criteria for endovascular reperfusion treatment were evidence of haemorrhages or prolonged infarctions of the encephalic trunk in the NCCTs performed at baseline (clear hypodensity in the midbrain and pons with obliteration of the basal cisterns), onset of symptoms more than 24h prior or the presence of terminal disease.
Our study was approved by the hospital's independent ethics committee and the written consent of all the patients (or their relatives) was obtained prior to treatment.
Clinical dataThe clinical data collected on admission to the hospital were: age and sex of the patients; cardiovascular risk factors such as hypertension, diabetes, atrial fibrillation, smoking or dyslipidaemia; and baseline NIHSS score. The clinical outcome was assessed using the mRS score at 90 days. The predefined outcome variables for this study were favourable outcome (defined as a score of 2 or less on the mRS) at 90 days and mortality rates.
Imaging protocolAll patients followed our stroke unit's standardised protocol for the management of ischaemic stroke. Sequential NCCTs were taken in a multislice CT scanner (Siemens Somatom Definition Flash or Siemens Sensation 64, Erlangen, Germany) at 140kV, 230 mAs, with a slice thickness of 5mm from the base to the vertex of the skull with continuous axial slices parallel to the orbitomeatal line. The NCCT was followed by a cerebral perfusion computed tomography (CPCT) study, administering a 40–60ml injection of intravenous contrast (Ultravist 300–370mg/ml, Bayer Hispania, Barcelona, Spain) at 5–6ml/s over 60s, accompanied by CTA (computed tomography angiography) using the helical scanning technique. The images were obtained after injecting a 50-ml bolus of intravenous contrast (Ultravist 300–370mg/ml, Bayer Hispania, Barcelona, Spain) at 5ml/s. The images were acquired automatically using CareDose4D to locate the region of interest (ROI) in the ascending aorta. The CTASI were reconstructed with slices of 5mm in thickness in axial planes at intervals of half the thickness. The standard imaging protocol includes sequential NCCT follow-up in the first 24h after the intervention in order to detect any haemorrhagic complications.
Information on the procedureThe routine procedure includes recording information about intravenous fibrinolysis, stent location, time elapsed between the onset of symptoms and performing the inguinal puncture, duration of the procedure (time elapsed from puncture to recanalization), time to recanalization (time elapsed from the onset of symptoms to recanalization), endovascular approach (intra-arterial thrombolysis and/or mechanical thrombectomy), type of device (Solitaire [Covidien, Dublin, Ireland], Trevo [Stryker, Mountain View, California] or MERCI [Stryker, Mountain View, California]) and all complications secondary to the endovascular treatment (vessel perforations or artery dissections).
Radiological dataTwo diagnostic neuroradiologists (with over 10 and 5 years’ experience, respectively), who were given no clinical information whatsoever, assessed the location of the thrombus by common accord using digital subtraction angiography, dividing the basilar artery (BA) into three segments: Proximal BA (from the confluence of the two vertebral arteries to the start of the anterior inferior cerebellar artery [AICA]), middle BA (from the AICA to the start of the superior cerebellar artery [SCA]) and distal BA (above the start of the SCA). The length (in millimetres) and density (measured in Hounsfield units with the ROI tool) of the thrombus were also recorded. Both the pc-ASPECTS scale and the PMI were used to assess parenchymal ischaemia of the posterior circulation confirmed in the CT images. The pc-ASPECTS scale was assessed using NCCT and CTASI: ten points were assigned to the posterior circulation, one point is deducted for the appearance of early ischaemic alterations (hypodensity or hypoattenuation) in each of the following locations: the territory of the left or right posterior cerebral artery, the thalamus or cerebellum, and two points for any of the areas of the midbrain or pons. The PMI was assessed with CTASI; zero to eight points were assigned to bilateral hypodensity in the pons and midbrain. A PMI of zero indicates no hypodensity in either the midbrain or the pons. Each side of both the midbrain and pons was classified as: 0=no hypodensity; 1=50% or less hypodensity; 2=more than 50% hypodensity. A PMI of eight indicated bilateral hypodensity of more than 50% in both the midbrain and the pons (Fig. 1). We did not analyse the CPCT study due to artefacts in the posterior fossa or because it was performed above the encephalic trunk, meaning that we did not have good enough data for the analysis.
Haemorrhagic events were classified according to the clinical and post-procedural NCCT criteria. Both haemorrhagic infarctions and parenchymal haemorrhages were classified based on the ECASS-2 criteria.20 Symptomatic intracranial haemorrhages were defined as the presence of blood on the NCCT secondary to clinical deterioration or a drop of four points on the NIHSS scale. Complications secondary to the procedure, such as artery perforations, defined as the extravasation of angiographic contrast occurring during the procedure, or artery dissections, described as the presence of an intimal flap on the control angiogram obtained after the thrombectomy, were also documented.
Statistical analysisThe descriptive analysis included frequencies and percentages for the categorical variables and means (standard deviation, SD) or medians (interquartile range, IQR) for the continuous variables. Initially, the patients were classified into two groups based on clinical outcome (favourable/unfavourable), then later into two groups based on mortality rate at 90 days. For the analysis, in accordance with Puetz et al.,15–17 we also divided the patients into groups based on the pc-ASPECTS scale (≥8 vs. <8) and PMI (≥3 vs. <3). The univariate analysis was carried out using the Mann–Whitney U test for the continuous variables and the χ2 test or Fisher's exact test for the categorical variables. The statistical analyses were carried out using the Statistical Package for the Social Sciences (SPSS) version 20.0 (IBM, Chicago, Illinois). P-values <0.05 were considered statistically significant.
ResultsPatientsBetween November 2008 and July 2013, 22 consecutive patients with BAO were hospitalised to receive endovascular treatment at our centre. Four patients were excluded from the analysis because they did not undergo CTA (two patients) or because their recanalization was unsuccessful (the other two patients). Therefore, 18 patients with BAO, baseline CTA and successful recanalizations after endovascular treatment were ultimately included in the study.
The patients’ characteristics and information on the procedure can be seen in Table 1.
Baseline patient characteristics and information on the procedure by group, classified using the CTASI pc-ASPECTS scale.
| All | Classification on the CTASI pc-ASPECTS scale | p-value | ||
|---|---|---|---|---|
| 8–10 | 0–7 | |||
| Age (years), median (IQR) | 58 (49–81) | 62 (45–81) | 54 (49–60) | 0.29 |
| Male, n (%) | 12 (66.7) | 8 (61.5) | 4 (80) | 0.47 |
| Baseline NIHSS, median (IQR) | 14 (8–30) | 13 (8–31) | 26 (7-) | 1 |
| Time elapsed from onset to treatment (min.), median (IQR) | 227 (130–398) | 311 (188–441) | 131 (95–309) | 0.14 |
| Time elapsed from onset to recanalization (min.), median (IQR) | 370 (213–503) | 414 (225–522) | 270 (163–410) | 0.21 |
| IV tPA, n (%) | 5 (27.8) | 5 (38.5) | 0 (0) | 0.11 |
| Stent, n (%) | 7 (38.9) | 4 (30.8) | 3 (60) | 0.27 |
| Symptomatic intracranial haemorrhages, n (%) | 0 (0) | 0 (0) | 0 (0) | – |
| Vascular risk factors, n (%) | ||||
| Diabetes mellitus | 4 (22.2) | 3 (23.1) | 1 (20) | 0.89 |
| Hypertension | 11 (61.1) | 9 (69.2) | 2 (40) | 0.27 |
| Atrial fibrillation | 3 (16.7) | 3 (23.1) | 0 (0) | 0.25 |
| Current smoker | 5 (27.8) | 4 (30.8) | 1 (20) | 0.66 |
| Dyslipidaemia | 8 (44.4) | 5 (38.5) | 3 (60) | 0.42 |
IQR, interquartile range; IV, intravenous; NIHSS, National Institutes of Health Stroke Scale.
The locations of the occlusions were: BA proximal segment in two patients (11.1%), medial segment in six patients (33.3%) and distal segment in ten patients (55.6%). With regard to recanalization, the eventual score obtained on the mTICI was 2b in eight patients (44.4%), with ten patients (55.6%) achieving a score of 3 on the same scale.
Eight patients (44.4%) had a favourable clinical outcome (mRS 0–2) at three months, and the mortality rate was 38.8% (seven patients). The remaining three patients (16.8%) had mRS scores of three in one case, four in another case and five in the remaining case. With regard to endovascular complications, no artery dissections or perforations whatsoever were detected during the procedure. Two patients (11.1%) presented haemorrhagic infarctions (HI2) in follow-up neurological imaging, but no parenchymal haematomas or symptomatic cerebral haemorrhages were observed.
Imaging dataNCCT and CTASI were available for all patients included in the study. Based on the NCCT, ten patients (55.6%) had no hypodensities (pc-ASPECTS score of ten); four patients (22.2%) obtained a score of nine on the pc-ASPECTS scale; one patient (5.6%) obtained a score of eight; two patients (11.1%) a score of seven; and one patient (5.6%) a score of six. The group of patients with scores between zero and seven on the NCCT pc-ASPECTS scale was comprised of only three patients (16.7%). None of the patients observed on the NCCT pc-ASPECTS scale had a score of less than six. Based on the NCCT, the mean thrombus density was 52.29±15.70HU and the mean length based on CTA was 148±146.94mm.
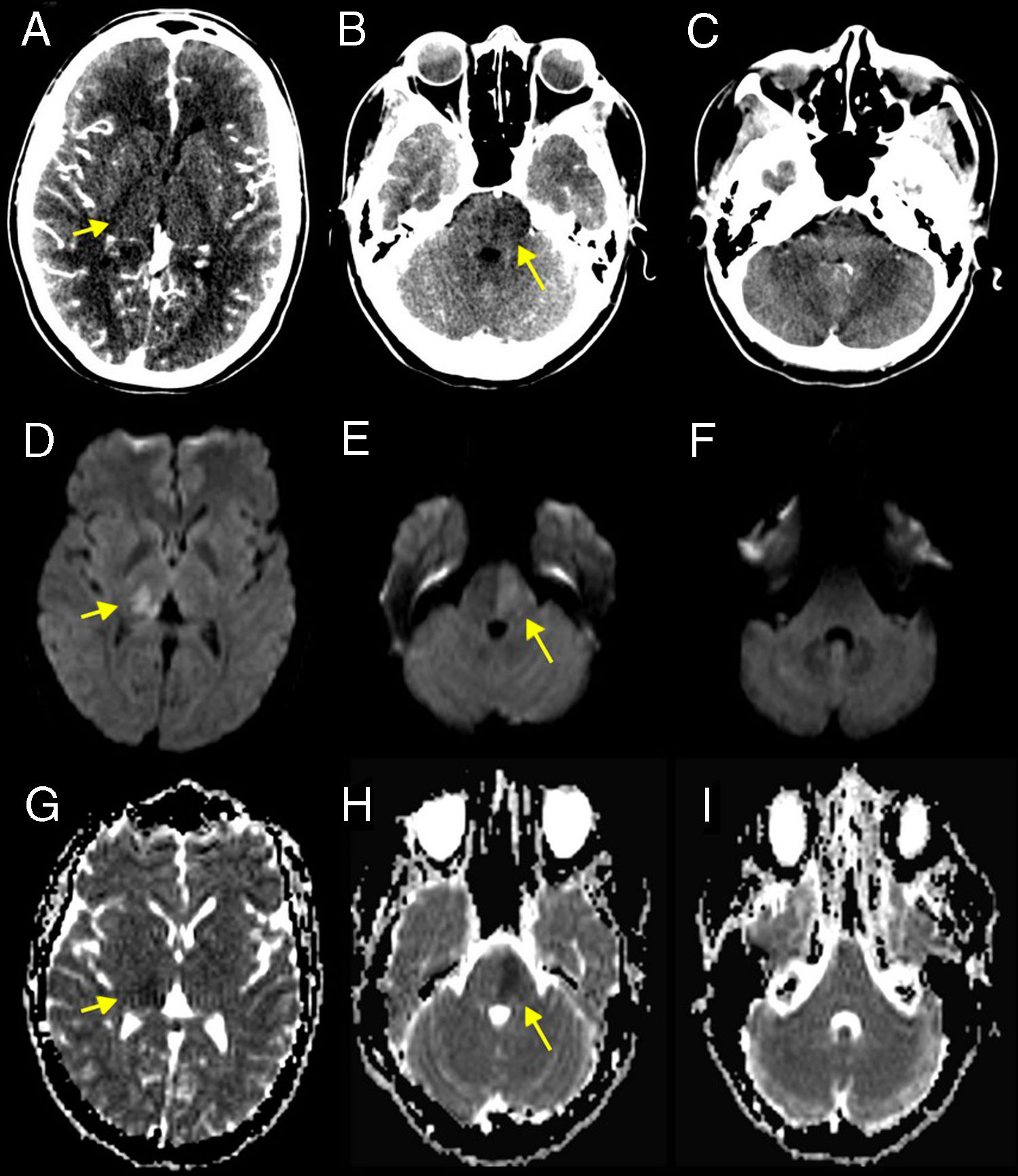
In the CTASI, seven patients (38.9%) obtained scores of ten on the pc-ASPECTS scale; five patients (27.8%) obtained a score of eight; two patients (11.1%) a score of six; and one patient (5.6%) each scores of nine, seven, five and four on the pc-ASPECTS scale (Fig. 2). The group of patients with scores between zero and seven on the CTASI pc-ASPECTS scale consisted of five patients (27.8%). With regard to the PMI, also calculated from the CTASI, nine patients (50%) obtained a score of zero, three patients (16.7%) each scores of three and four; and one patient (5.6%) scores of two, five and eight in the PMI. The group with scores between three and eight in the PMI using CTASI included eight patients (44.4%).
Example of a patient with basilar artery occlusion. The CT angiography source images confirm that the hypoattenuation of the right thalamus (one point) (A) and the left pons (two points) (B) without other hypoattenuated areas (C) gave a score of seven on the pc-ASPECTS scale. The magnetic resonance imaging performed 36h after carrying out successful recanalization without endovascular treatment confirmed this finding (D-I).
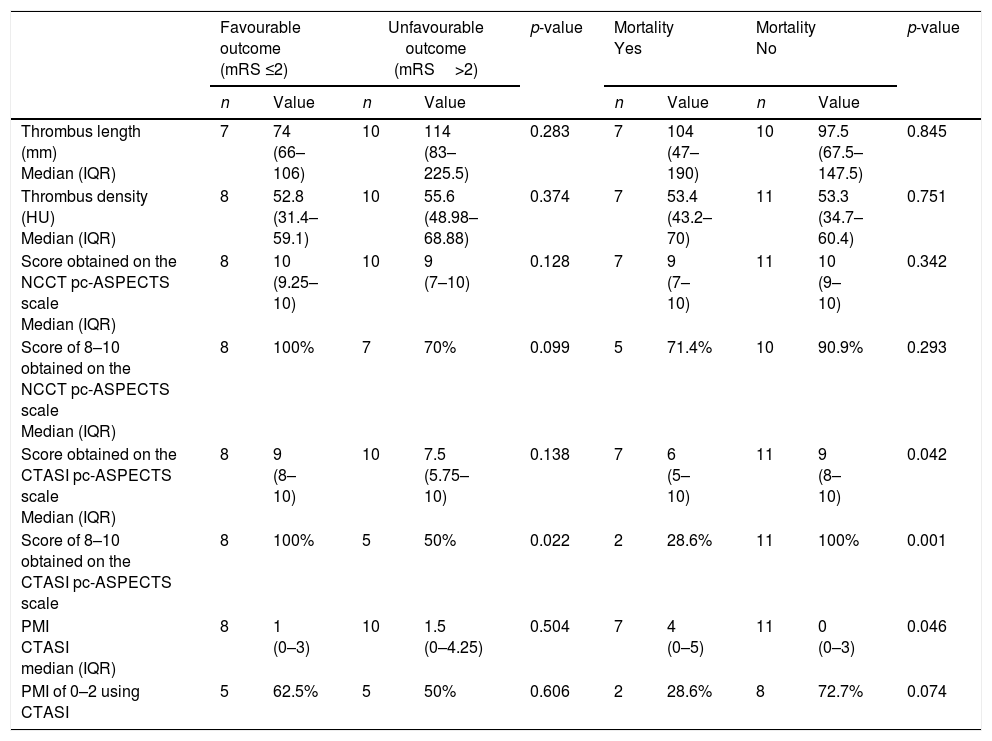
The relationship between the imaging findings and the functional outcomes can be seen in Table 2. In terms of thrombus length and density, no significant differences were recorded in either clinical outcome or mortality. There was also no association between the NCCT pc-ASPECTS scale and a favourable outcome or lower mortality risk in the univariate analysis dichotomised to <8 vs. ≥8.
Relationship between imaging findings and functional outcomes.
| Favourable outcome (mRS ≤2) | Unfavourable outcome (mRS>2) | p-value | Mortality Yes | Mortality No | p-value | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| n | Value | n | Value | n | Value | n | Value | |||
| Thrombus length (mm) Median (IQR) | 7 | 74 (66–106) | 10 | 114 (83–225.5) | 0.283 | 7 | 104 (47–190) | 10 | 97.5 (67.5–147.5) | 0.845 |
| Thrombus density (HU) Median (IQR) | 8 | 52.8 (31.4–59.1) | 10 | 55.6 (48.98–68.88) | 0.374 | 7 | 53.4 (43.2–70) | 11 | 53.3 (34.7–60.4) | 0.751 |
| Score obtained on the NCCT pc-ASPECTS scale Median (IQR) | 8 | 10 (9.25–10) | 10 | 9 (7–10) | 0.128 | 7 | 9 (7–10) | 11 | 10 (9–10) | 0.342 |
| Score of 8–10 obtained on the NCCT pc-ASPECTS scale Median (IQR) | 8 | 100% | 7 | 70% | 0.099 | 5 | 71.4% | 10 | 90.9% | 0.293 |
| Score obtained on the CTASI pc-ASPECTS scale Median (IQR) | 8 | 9 (8–10) | 10 | 7.5 (5.75–10) | 0.138 | 7 | 6 (5–10) | 11 | 9 (8–10) | 0.042 |
| Score of 8–10 obtained on the CTASI pc-ASPECTS scale | 8 | 100% | 5 | 50% | 0.022 | 2 | 28.6% | 11 | 100% | 0.001 |
| PMI CTASI median (IQR) | 8 | 1 (0–3) | 10 | 1.5 (0–4.25) | 0.504 | 7 | 4 (0–5) | 11 | 0 (0–3) | 0.046 |
| PMI of 0–2 using CTASI | 5 | 62.5% | 5 | 50% | 0.606 | 2 | 28.6% | 8 | 72.7% | 0.074 |
CTASI, CT angiography source images; HU, Hounsfield units; IQR, interquartile range; mRS, modified Rankin scale; NCCT, non-contrast computed tomography; PMI, pons-midbrain index.
Values in bold represent statistically significant differences (p < 0.05).
According to the analysis, the patients who survived had much higher mean scores on the CTASI pc-ASPECTS scale [9 (8–10)] vs. 6 (5–10); p=0.042] and much lower values on the PMI scale [0 (0–3) vs. 4 (0–5); p=0.046].
The CTASI pc-ASPECTS scale, dichotomised to <8 vs. ≥8, was associated with a favourable outcome (RR: 2.6; 95% CI: 1.3–5.2) and a lower mortality risk (RR: 6.5; 95% CI: 7.8–23.3). All patients who survived and who were functionally independent had scores of eight or more on the pc-ASPECTS scale. None of the five patients with scores below eight on the pc-ASPECTS scale using CTASI survived. In contrast, the PMI obtained using CTASI, dichotomised to <3 vs. ≥3, was not associated with either a favourable outcome or lower mortality risk.
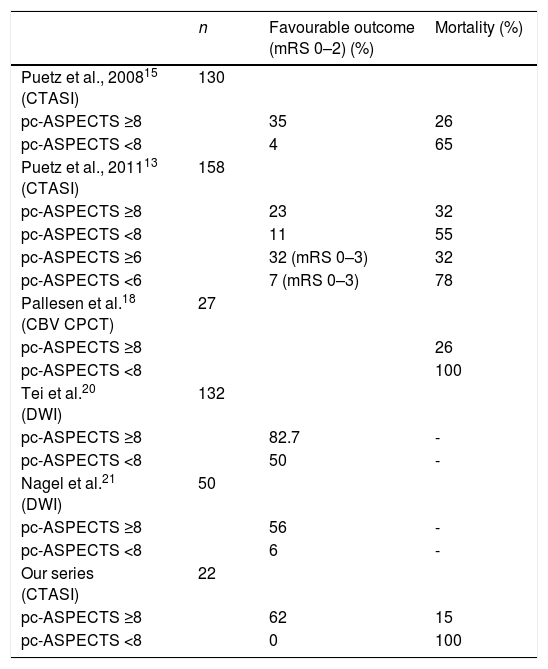
DiscussionThis study reveals that in patients with acute BAO successfully recanalized via mechanical thrombectomy, the CTASI pc-ASPECTS scale was predictive of both functional outcome and mortality rate, while the PMI obtained using CTASI was only predictive of mortality. Several studies have already been published using the pc-ASPECTS scale with various imaging techniques (Table 3).
pc-ASPECTS and clinical outcomes in various studies with different imaging techniques.
| n | Favourable outcome (mRS 0–2) (%) | Mortality (%) | |
|---|---|---|---|
| Puetz et al., 200815 (CTASI) | 130 | ||
| pc-ASPECTS ≥8 | 35 | 26 | |
| pc-ASPECTS <8 | 4 | 65 | |
| Puetz et al., 201113 (CTASI) | 158 | ||
| pc-ASPECTS ≥8 | 23 | 32 | |
| pc-ASPECTS <8 | 11 | 55 | |
| pc-ASPECTS ≥6 | 32 (mRS 0–3) | 32 | |
| pc-ASPECTS <6 | 7 (mRS 0–3) | 78 | |
| Pallesen et al.18 (CBV CPCT) | 27 | ||
| pc-ASPECTS ≥8 | 26 | ||
| pc-ASPECTS <8 | 100 | ||
| Tei et al.20 (DWI) | 132 | ||
| pc-ASPECTS ≥8 | 82.7 | - | |
| pc-ASPECTS <8 | 50 | - | |
| Nagel et al.21 (DWI) | 50 | ||
| pc-ASPECTS ≥8 | 56 | - | |
| pc-ASPECTS <8 | 6 | - | |
| Our series (CTASI) | 22 | ||
| pc-ASPECTS ≥8 | 62 | 15 | |
| pc-ASPECTS <8 | 0 | 100 |
CBV CPCT, cerebral blood volume mapping in a cerebral perfusion computed tomography study; CTASI, CT angiography source images; DWI, diffusion-weighted imaging; mRS, modified Rankin scale.
According to the only three articles published by the same author, patients with BAO and scores of eight or higher on the CTASI pc-ASPECTS scale are more likely to have good functional outcomes.15–17 This study included patients who underwent different treatment techniques; nevertheless, this difference remained consistent in a sub-analysis of 21 patients who underwent angiographic recanalization. Our study focussed on patients with acute BAO and successful recanalizations after endovascular treatment, avoiding the potential bias of the prognostic effect of recanalization.
In 2011, Puetz et al. assessed patients in the Basilar Artery International Cooperation Study (BASICS) registry with CTASI pc-ASPECTS scores15; some 23% of patients with scores of eight or more on the CTASI pc-ASPECTS scale had good functional outcomes (scores of 0–2 on the mRS) versus just 11% of patients with scores under eight. After making the corresponding adjustments in a multivariate model, patients with scores of eight or more on the CTASI pc-ASPECTS scale were twice as likely to have good functional outcomes (RR: 2; 95% CI: 1.1–3.8). In the post hoc analysis, dichotomised with a cut-off point of six, some 32% of patients with scores of six or more on the CTASI pc-ASPECTS scale had favourable outcomes (scores of 0–3 on the mRS) versus just 7% of patients with scores under six. After making the corresponding adjustments in a multivariate model, patients with scores of six or more on the CTASI pc-ASPECTS scale were three times as likely to have good functional outcomes (RR: 3.1; 95% CI: 1.2–7.5). These results suggest that the scores obtained on the CTASI pc-ASPECTS scale dichotomised with a cut-off of six were capable of discerning favourable outcomes in their patients. The different results obtained can be explained in part by the technical differences in the treatments used, by the unknown initial recanalization rates, and by the lack of exclusion criteria relating to the window of time.
According to our results, more than 60% of patients will be functionally independent (scores of 0–2 on the mRS) if they have BAO and scores of eight or more on the CTASI pc-ASPECTS scale, provided that the recanalization is successful. The fact that, in our series, none of the patients with scores below eight on the CTASI pc-ASPECTS scale had favourable outcomes, in spite of successful recanalization, leads us to think that patients in this situation are unlikely to benefit from recanalization treatments.
On the other hand, the scores obtained on the NCCT pc-ASPECTS scale in this study showed no association with clinical outcomes, in keeping with the data published in the specialist literature. Puetz et al.16,17 demonstrated that clinical outcomes cannot be predicted using the score obtained on the NCCT pc-ASPECTS scale. In this study,16 CTASI was found to be more sensitive than NCCT in detecting ischaemic alterations in patients with suspected vertebrobasilar ischaemia.
Pallesen et al.21 analysed the prognostic impact on the pc-ASPECTS scale in computed tomography perfusion (CTP) studies in the BASICS registry population. They detected that CTP studies were performed in only 4.6% of the BASICS registry population and that the pc-ASPECTS scale dichotomised with a cut-off score of eight was not associated with favourable outcomes (scores of 0–3 on the mRS) with any imaging technique. Cerebral blood volume (CBV) mapping was the most commonly used technique in this work, and those patients with scores below eight on the pc-ASPECTS scale using CBV mapping had a high mortality rate (all three died within one month versus six of the 23 patients with scores of eight or more on the pc-ASPECTS scale using CBV mapping).
The diagnostic reference standard to detect ischaemic alterations in patients with posterior circulation stroke is magnetic resonance imaging (MRI) using diffusion-weighted imaging (DWI).22 Various studies have demonstrated that DWI is a useful tool to predict functional outcomes in patients with posterior circulation stroke. Tei et al.23 demonstrated that more than 80% of patients with scores of eight or more on the pc-ASPECTS scale using DWI had favourable outcomes. Nagel et al.24 revealed that only 6% of patients with scores of seven or less on the pc-ASPECTS scale using DWI had favourable outcomes, compared to patients with scores of eight or more on the same scale, 56% of whom had favourable outcomes.
Both CTP and MRI studies have limitations relating above all to their availability and artefacts that can hinder their use when selecting these patients. In contrast, CTASI is a simple tool for post-processing images obtained from CTA, which is generally performed as part of routine imaging for patients with large vessel occlusions. In any event, in posterior circulation stroke, there is no mismatch that would allow its comparison with anterior circulation stroke. Studies conducted in the future must focus on this issue so that attempts can be made to standardise screening of patients with BAO.
In terms of scales to assess collateral status in BAO, a recent study published by Yang et al. confirmed that the BATMAN scale using cerebral angiography is capable of predicting the functional outcome of patients with acute BAO who undergo mechanical thrombectomy.25 The main limitation of collateral status scales such as the BATMAN scale is that collateral status is a dynamic process that can change during an arterial occlusion in terms of blood pressure, intracranial pressure, etc. On the other hand, the pc-ASPECTS and PMI scales identify the nucleus of the infarction, which allows the patient's disability to be calculated based on the areas affected.
The main limitation of our study is the small sample of patients due to the low prevalence of this disease and restrictive inclusion criteria. This restriction to only include patients with acute BAO successfully recanalized after endovascular treatment was used to avoid the possible bias of the prognostic effect of recanalization and different methods of treatment. Moreover, all patients were treated 7h from the onset of symptoms, which is the reason why we cannot determine the usefulness of this scale beyond this period of time.
This study may be useful to predict functional outcomes after recanalization of a BAO with endovascular treatment using the CTASI pc-ASPECTS scale. Patients with low scores on said scale are unlikely to benefit from recanalization treatment. In any event, our results recommend against excluding these patients from the possibility of receiving this treatment. There is still some debate over which patients would benefit from recanalization treatment. The results of our study would need to be validated in a randomised controlled trial in order to decide whether or not to treat a patient with BAO, which would seem difficult from an ethical perspective, as well as because of the low incidence of the disease. We also propose a multicentre registry that would enable these results to be confirmed, with CT and MRI performed prior to treatment for comparison. All images must also be analysed by various specialists with different experiences in this field, in order to be able to determine inter- and intra-observer analysis concordance.
To conclude, the CTASI pc-ASPECTS scale appears to be useful in predicting functional outcomes after recanalization of a BAO via endovascular treatment. Scores of eight on this scale have a prognostic value. All patients who survived and who were functionally independent had scores of eight or more on the pc-ASPECTS scale. However, these results need to be validated in a randomised controlled trial before deciding whether or not to treat a patient with BAO.
Authorship- 1.
Responsible for the integrity of the study: MFW, ALR.
- 2.
Study conception: MFW, ALR, FXZ, JB, LSR, SA, EC, RV, LO, JMM, NB.
- 3.
Study design: MFW, ALR, FXZ, JB, LSR, SA, EC, RV, LO, JMM, NB.
- 4.
Data collection: MFW, ALR, FXZ, SA, EC, NB.
- 5.
Data analysis and interpretation: MFW, ALR, FXZ, JB, LSR, SA, EC, RV, LO, JMM, NB.
- 6.
Statistical processing: MFW, ALR.
- 7.
Literature search: MFW, ALR.
- 8.
Drafting of the article: MFW, ALR.
- 9.
Critical review of the manuscript with intellectually relevant contributions: MFW, ALR, FXZ, JB, LSR, SA, EC, RV, LO, JMM, NB.
- 10.
Approval of the final version: MFW, ALR, FXZ, JB, LSR, SA, EC, RV, LO, JMM, NB.
The authors declare that they have no conflicts of interest.
Please cite this article as: Werner MF, López-Rueda A, Zarco FX, Blasco J, San Román L, Amaro S, et al. Valor de la escala ASPECTS de circulación posterior y del índice puente-mesencéfalo en imágenes de TC sin contraste y angiografía por TC en pacientes con oclusiones de la arteria basilar recanalizados tras trombectomía mecánica. Radiología. 2019;61:143–152.