To evaluate the changes in the size of focal nodular hyperplasia (FNH) during long-term magnetic resonance imaging (MRI) follow-up.
Material and methodsWe reviewed 44 FNHs in 30 patients studied with MRI with at least two MRI studies at least 12 months apart. We measured the largest diameter of the lesion (in mm) in contrast-enhanced axial images and calculated the percentage of variation as the difference between the maximum diameter in the follow-up and the maximum diameter in the initial study. We defined significant variation in size as variation greater than 20%. We also analyzed predisposing hormonal factors.
ResultsThe mean interval between the two imaging studies was 35±2 months (range: 12–94). Most lesions (80%) remained stable during follow-up. Only 9 of the 44 lesions (20%) showed a significant variation in diameter: 7 (16%) decreased in size and 2 (4%) increased, with variations that reached the double of the initial size. The change in size was not related to pregnancy, menopause, or the use of birth control pills or corticoids.
ConclusionChanges in the size of FNHs during follow-up are relatively common and should not lead to a change in the diagnosis. These variations in size seem to be independent of hormonal factors that are considered to predispose.
Evaluar los cambios en el tamaño de la hiperplasia nodular focal (HNF) mediante seguimiento a largo plazo con resonancia magnética (RM).
Material y métodosSe revisaron 44 HNF de 30 pacientes, estudiadas mediante RM con al menos 2 estudios separados como mínimo 12 meses. Se midió (en mm) el diámetro mayor de la lesión en las imágenes transversales de RM con contraste, calculándose el porcentaje de variación como la diferencia entre el diámetro máximo en el seguimiento respecto al diámetro máximo inicial. Se definió como variación significativa de tamaño un porcentaje de variación superior al 20%. Se analizaron los factores hormonales predisponentes.
ResultadosLa media del intervalo de tiempo entre las 2 pruebas de imagen fue de 35±2 meses (rango: 12–94). La mayoría de las lesiones (80%) permanecieron estables durante el seguimiento, y solo 9 de las 44 lesiones (20%) mostraron una variación significativa de su diámetro. Siete de ellas (16%) disminuyeron de tamaño y 2 (4%) aumentaron, con variaciones que alcanzaron hasta el doble del tamaño inicial. El cambio de tamaño no se pudo relacionar con el embarazo, la menopausia ni el uso de anticonceptivos orales o corticoides.
ConclusiónLos cambios de tamaño de la HNF durante el seguimiento son relativamente frecuentes y no deben disuadir de este diagnóstico. Estas variaciones parecen independientes de los factores hormonales considerados como predisponentes.
Focal nodular hyperplasia (FNH) is the second most frequent benign liver lesion after hemangioma. It is present in more than 3% of the population, prevailing among young women, although it may occur in both sexes and in all age groups.1 Microscopically, FNH is made up of normal hepatocytes, Kupffer's cells and blood vessels, surrounded by fibrous septa containing a variable number of primitive biliary conduits.2 Although its etiology is not proved, it seems that a preexisting congenital vascular anomaly or a vascular malformation trigger the hyperplastic stimulus.3
FNH is usually asymptomatic and it is frequently detected incidentally in liver radiologic studies performed for other causes. In this lesion, spontaneous rupture is very rare and malignant transformation is even more so. Therefore, after accurate diagnosis with the current image methods, treatment is conservative and only clinical follow-up must be established and then by means of medium- and long-term image tests.4
Conventional MR and dynamic studies after administration of contrast offer, using strict image criteria, a greater sensitivity and specificity in the diagnosis of FNH as compared to echography or TC.5–7 In the last few years, MR specificity to characterize FNH has increased with the introduction of hepatobiliary contrasts, which have caused specificity to come close to 100%, which avoids the need to perform other invasive diagnostic techniques and procedures.8,9 Histological study of the samples obtained by means of percutaneous biopsy has, in addition, certain limitations especially at the hands of pathologists with limited experience in these lesions.10 MR has greater sensitivity (74–78%) than either echography (20%) or CT (60%)5,6 to detect the central FNH scar. Moreover, it is more sensitive than echography to detect FNH lesions, due to the fact that the lesion's echogenicity is similar to that of the adjacent parenchyma, and it has the advantage of not using ionizing radiations such as CT. That is why MR is considered the image test of choice for characterizing and following up these benign focal hepatic lesions.
Medium-long term FNH follow-up by means of image tests do not generally show changes in the size of the nodules,11,12 although on occasion both lesion regression and progression have been documented.13–15 However, serial MR studies comparing the size of lesions are few.11–13
The objective of this study is to evaluate the degree of variation of FNH size by means of contrasted MR dynamic images given this test's maximum sensitivity to delimit lesions, so as to know FNH natural history.
Material and methodsMR images of 30 patients presenting a definite FNH diagnosis were reviewed as well as at least 2 MR examinations. The definite diagnosis was by histology or by typical criteria in MR. All the subjects belonged to 2 hospitals and the sample was obtained from a 10-year retrospective search (2000–2010). None of the patients had a history of chronic hepatopathies or primary neoplasia.
The patients signed an informed consent in writing to use a contrast medium in MR and the use of their data in scientific evaluations. Since the study was retrospective and the patients authorized the use of the data for scientific purposes, it was deemed unnecessary to request approval from the ethics committee.
The series was made up of 23 women and 7 men, with ages ranging from 18 to los 83 years (median: 39±9 years). Before the diagnosis, 7 women (23%) were taking oral contraceptives and one man (3%) steroids. Two women (6%) became pregnant during follow-up after diagnosis. Six patients (20%) had been postmenopausal for over a year before diagnosis, but none of them was taking substitutive hormonal therapy.
FNH lesions were single in 21 patients (70%) and multiple in 9 (30%). In order to avoid measurement errors with digital calibrators and partial volume biases, only the FNH lesions presenting a diameter greater than 10mm upon diagnosis were included. Finally, 4 patients with 2 lesions and 5 patients with 3 lesions were counted; therefore the total number of FNH lesions studied was 44. The images were acquired with an MR machine of 1.5T (Philips Medical Systems, Best, the Netherlands) with body coils. The study protocol differed minimally between the two hospitals, but it remained stable during all the 10-year follow-up period. In all the examinations gradient echo (GE) sequences were performed adjusted on T1 in opposite phase/phase (RT=150–170ms; ET=2.3–4.6ms; inclination angle: 70–80°; matrix: 235–512, and rectangular field of vision) and adjusted images on T2 by means of spin echo (SE) or turbo spin echo (TSE) (RT=2.000–3.000ms; ET=90–130ms; matrix: 235–512, and rectangular field of vision). In all the cases a GE 2D dynamic study adjusted on T1 was performed with fat suppression (RT=120–130ms; ET=1.3–1.5ms; angle: 70°, matrix: 258–512 and rectangular field of vision). 4 phases in apnea were obtained (early arterial, portal, balance and tardive phases), after intravenous administration in rapid injection of a gadolinium chelate of extracellular distribution (at a dose of 0.2ml/kg). Prior to that the retardation time was calculated for the early arterial phase by means of a 1ml contrast test, with which the time of arrival in the abdominal aorta was established in a high temporal resolution and a low spatial resolution transversal sequence. The portal phase was considered to be some 35–45s after the arterial one, that of balance at 90s and the tardive one at 3min after administration of contrast. Cut thickness was 6–7mm, adjusted to the cranial-caudal dimension of the liver, the space between cuts was always 10% of the cut's thickness and pixel size equal to or less than 1.5mm in its maximum dimension.
FNH was diagnosed by biopsy in 16 cases and by typical behavior in MR in 28. The following MR criteria were considered as typical behavior of FNH lesions: an isointense or discretely hypointense homogeneous signal in the images adjusted on T1, and isointense or discretely hyperintense in the sequences adjusted on T2. The typical central scar was defined with low signals in adjusted sequences on T1 and high signals in sequences adjusted on T2. During the dynamic study after administration of intravenous contrast typical lesions showed an intense, homogeneous contrast uptake during the arterial phase, which then became practically isointense (excepting the scar) during the portal and the balance phases. The central scar was considered typical when it was hypointense in the arterial and portal phases and slightly hyperintense in the balance phase. The presence of the central scar in lesions greater than 30mm was not deemed necessary for FNH diagnosis.
The analysis of lesion size was performed by consensus between 2 radiologists with ample experience in abdominal image. The maximum transversal diameter of the lesions was measured in the images obtained in the arterial phase of the MR dynamic study, using electronic calibrators. In those patients who had more than 2 MR tests, the most separated examinations were reviewed. Lesion size was always measured in similar images to avoid measuring errors for lack of co-register.
Lesion size variation was calculated by means of the following equation: [(initial diameter−follow-up diameter)/initial diameter]×100, which was expressed as relative percentage. When the change in this parameter was greater than 20%, it was defined as significant size variation, in order to minimize errors by inter- and intra-observer measurement. When the percentage was negative, it was considered lesion regression and when the percentage was positive, lesion progression. The lesions which neither regressed nor progressed were considered stable.
The statistic analysis was performed by means of the Chi-square with contingency tables. A p value of less than 0.05 was considered significant.
ResultsIn the MR images to diagnosis, all the hepatic lesions presented typical behavior, except for one scar that did not take up in the tardive phase and one lesion that presented a signal intensity slightly below the surrounding hepatic parenchyma in the balance and tardive phases. None of the lesions had fat in the echo gradient sequences in the opposite phase or capsule in the tardive phase. A central scar was detected in the pre-contrast study in 16 (36%) of the 44 lesions, of which 13 (81%) were detected in 22 lesions that measured 30mm or more, and 3 (19%) were observed in 22 lesions smaller than 30mm. No central scar was detected in lesions smaller than 20mm. Conclusive MR diagnosis was reached in all the cases except 2, which were biopsied.
The median time interval between the two image tests was 35±2 months (range: 12–94 months). The median FNH size at the moment of diagnosis was 37.2mm (range: 10–120mm) and the median size variation during the follow-up was 2.1mm (range: −32 to 52mm).
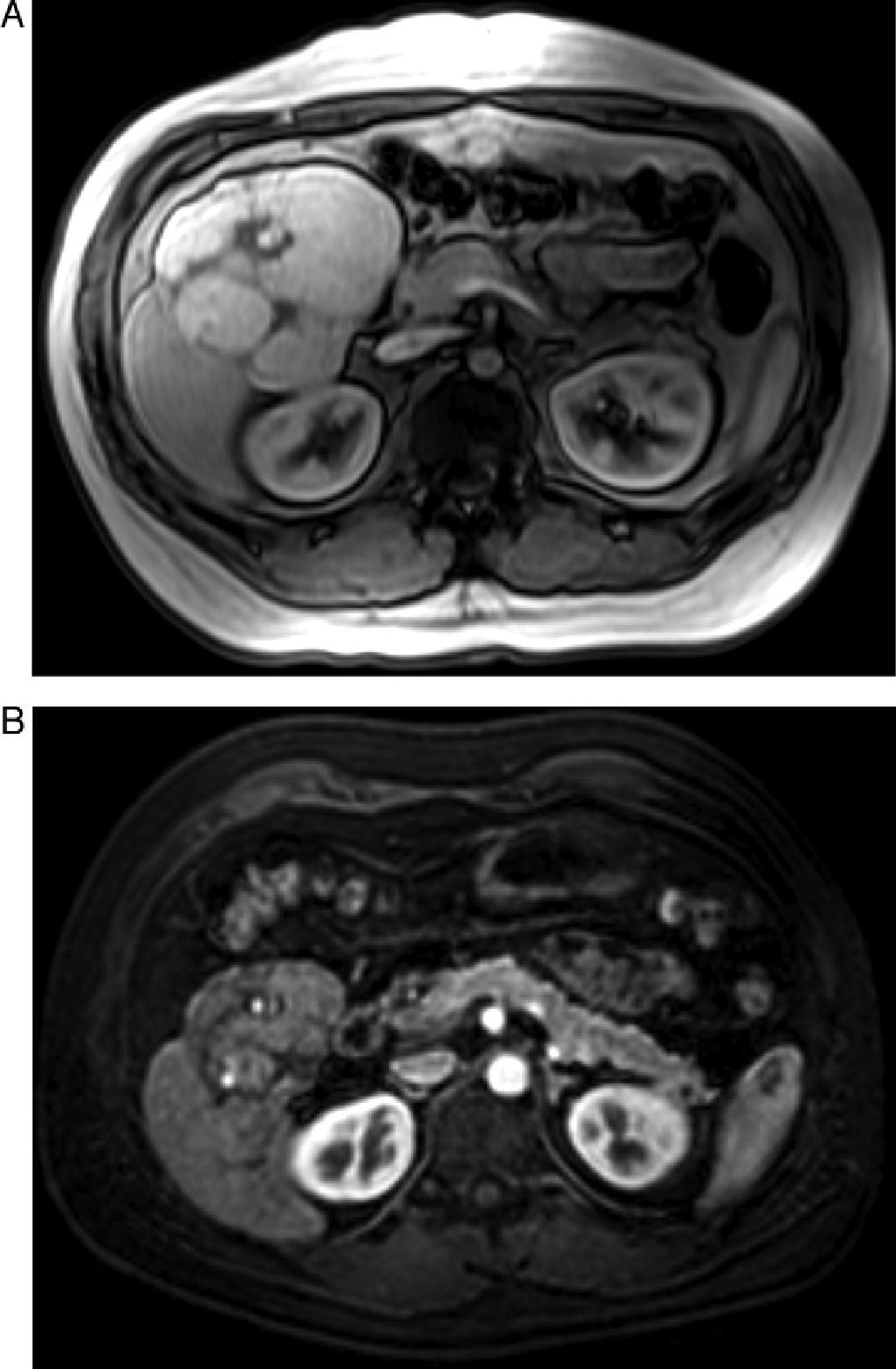
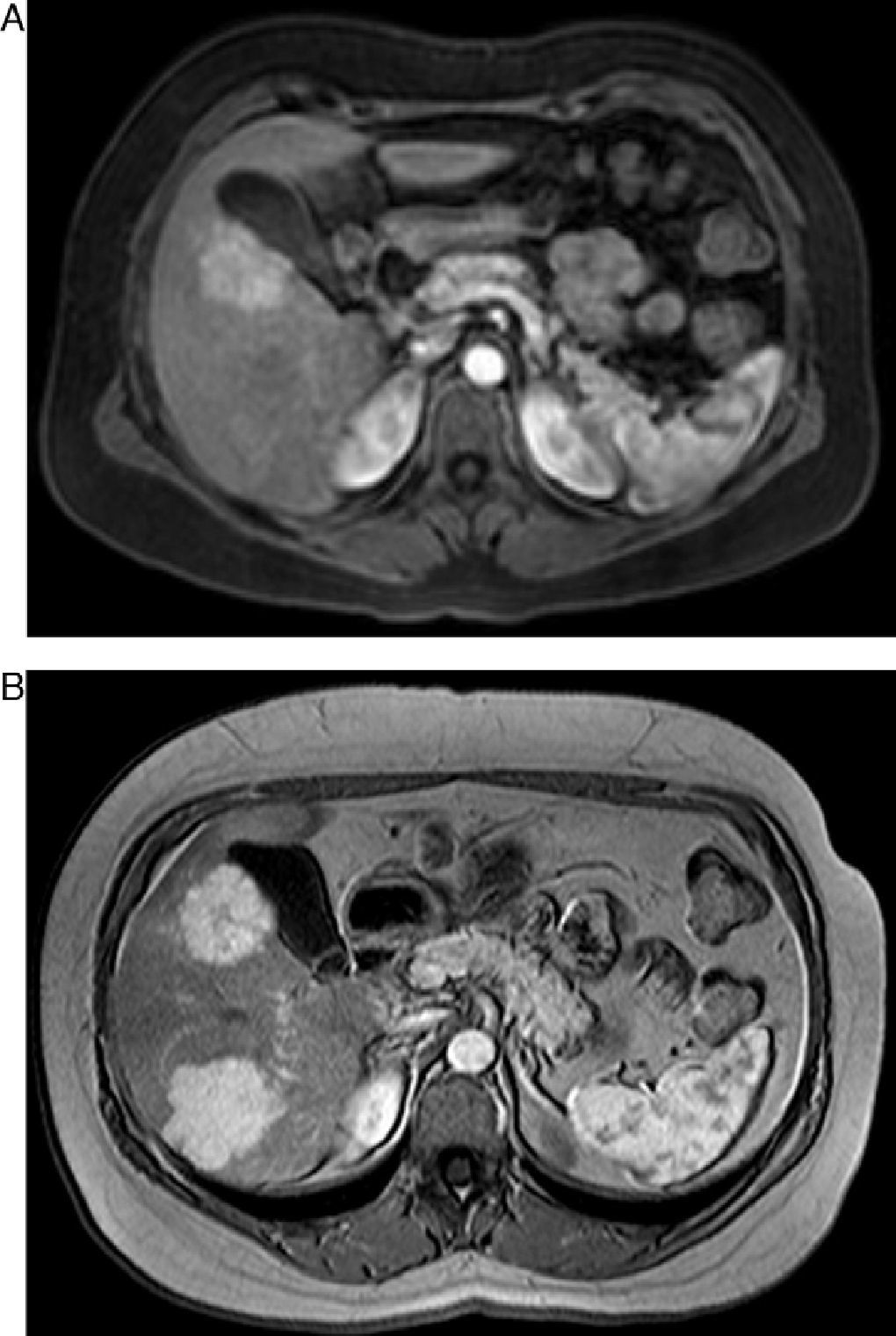
Of the 44 lesions, 35 (80%) remained stable during the follow-up period, while 9 (20%) showed significant variation in their maximum diameter. Of the 9 lesions with variation, 7 (16%) diminished their size (Fig. 1) and 2 (5%) increased it. In 3 lesions, measuring 50, 35 and 34mm, size reduction was very significant (34, 49 and 74%, respectively). A lesion presented spontaneous regression, with 22mm of diameter at the moment of diagnosis and disappearance after 53 months of follow-up. In a patient with 3 lesions in the second control performed after 72 months, a lesion remained stable; another grew in size and a third one of 52mm appeared as new in the second control (Fig. 2).
Asymptomatic 35-year-old male, without predisposing hormonal factors. MR images of gradient echo adjusted on T1 during the precocious phase after administration of intravenous contrast. (A) 114-mm FNH in segment VI. (B) Ninety-four months later, it is possible to observe size decrease (relative variation percentage 28%).
Asymptomatic 49-year-old woman. MR images of gradient echo adjusted on T1 during the precocious phase after administration of intravenous gadolinium. (A) Hypervascular lesion of 41mm of maximum diameter in segment V. (B) In follow-up performed 72 months later, a new 52mm lesion has appeared in segment VI with stability of lesion in segment V.
The 7 lesions that shrank in size were observed in 5 women and 2 men, with ages ranging from 25 to 45 years (median: 37 years). The 2 lesions that increased were detected in 2 women aged 37 and 47 years (median: 40 years). The ages of the remaining 23 patients in whom FNH remained stable were an average of 40 years (range: 18–83 years). There were no statistically significant differences in age.
The median follow-up time for the lesions that showed size variation was 53 months (range: 14–94) and for the stable ones 29 months (range: 12–60). This difference in follow-up observation time was statistically significant (p<0.05).
Most patients (22 cases, 73%) were asymptomatic, and FNH was an incidental finding in image studies performed for other reasons. Only 8 patients (27%) presented unspecific discomfort or abdominal pain in the right hypochondrium. Five patients (17%) showed alterations of hepatic function (serum elevation of gamma-glutamyl transpeptidase and/or transaminase). The levels of alpha-fetoprotein were normal in all the patients. In one patient hepatic steatosis became evident in the MR images, but in none of the cases there were clinical or image findings of chronic hepatopathy or cirrhosis. During follow-up symptomatology was resolved in the 8 patients with clinical signs. In these cases, there was no relation between symptom resolution and size change in the lesions, since in all of them the lesions were stable.
Before diagnosis, 8 patients (27%) were taking hormonal treatment (7 women and one man). Of the 7 women taking oral contraceptives regularly, FNH was single in 4 of them and multiple in 3, with a total of 12 FNH. Six women stopped taking oral contraceptives after diagnosis and in this group; only 2 of the 11 lesions shrank in size, while the rest remained stable. The man taking steroids stopped taking them after diagnosis and his single FNH did not change its size.
Two women with 3 FNH lesions became pregnant during follow-up. One of the lesions shrank 34%, while the other 2 remained stable.
Six women had entered menopause more than a year before diagnosis. Of the 9 FNH lesions in this group, one lesion was a first appearance in one patient, another grew and the rest of the lesions remained stable.
There were 14 patients (47%) with 19 lesions (43%) that did not present any predisposing hormonal factor. Of them, 15 remained stable while 3 shrank and one disappeared.
The contingency tables did not show any relation between hormonal state and size variation of the lesions (p=0.9).
DiscussionThe summary of the findings in our work is that most (80%) of the FNH showed stable size, 16% shrank and 4% grew during MR follow-up.
The advance in quality and the increasing frequency of the use of modern image techniques to study the abdomen have made it possible to detect and diagnose FNH without the need for histological confirmation. Several articles published recently show that MR is the most accurate diagnostic technique for this objective.5–9 Using strict, widely-accepted criteria, MR makes it possible to characterize FNH lesions in most patients without the need for obtaining a percutaneous biopsy of the lesion.
With a definite image diagnosis, management of these patients consists in an image follow-up that checks the stability of the lesion,4 which gives us the opportunity to study the lesions along time and define its natural history. In our series we did not detect bleeding complications or malignant transformations during follow-up, just like other previous studies with a follow-up period approximating our 35 months.12–18
Different previous works have assessed size variation of FNH lesions, with results matching ours, and they have documented lesions that grow and shrink, although with variability in the percentages. Mathieu et al.12 followed 136 FNH women up by means of MR for a period of 9 years and they detected size changes in only 4 patients (3%), with reduction in 3 patients and progression in one. On the other hand, Leconte et al.13 determined the size changes in a series of 18 lesions by CT and/or MR and they observed, after a 37-month follow-up, stability in 33% of the FNH, shrinking in 56% and growth in 11%. Di Stasi et al.18 using echography, found size reduction in 7 of the 16 FNH (44%), with spontaneous regression in one (6%) after a 33-month follow-up. D’Halluin et al.14 evaluated 44 cases of FNH by means of echography for a median period of 45 months and they found size reduction in 30% of the cases, increase in 27% and stability in 43%. In the series published by Kuo et al.,15 24 FNH lesions (71%) remained stable, 3% progressed and 26% regressed for a median period of 42 month of ultrasonographic follow-up. Of the lesions that regressed, complete disappearance occurred in 6 (18%) cases. In our work we have selected MR for FNH lesion size assessment because it is more sensitive than ultrasound to detect them and follow them up.
Other works13 have used a 3D volumetric measurement technique by means of the method of area addition, which is more accurate to assess the tumor's total size. In our study, we have used one-dimensional measurement of the long axis similarly to other authors,11,12 since it results into a more objective, reproducible and easy to perform measurement in the images acquired in the dynamic study with contrast, thickness ranging from 6 to 7mm.
We have not found any relationship between FNH size variation and y the known predisposing hormonal factors. The role of oral contraceptives and pregnancy in FNH development and complications continues to be controversial. Some authors have suggested that high doses of exogenous estrogens and pregnancy may be associated with size increase of FNH lesions.19 Cases of FNH spontaneous regression after oral contraceptives were discontinued have also been published.20 According to our results, other authors11,12,17 have shown that contraceptives have no influence on FNH natural history.
Our study's limitations lie on its retrospective character, which prevents us from analyzing lesion size variations in a time-regulated manner, the fact that it was conducted in two different hospitals, with different equipment although with similar sequences, and that there were different follow-up period among patients. In our series, the patients with stable lesions have a shorter follow-up time and therefore, these lesions might have shown size changes if the follow-up had been longer. Another aspect to bear in mind is the absence of histological confirmation in many cases with very specific FNH MR findings. We believe that this bias does not limit the work's results. Perhaps, in light of our results, more comprehensive knowledge about FNH natural history with a prospective study does not contribute clinically relevant information to manage this condition.
In conclusion, although most FNH lesions remain stable in time (80%), size variations are not rare and neither are even spontaneous appearance and regression. We have not been able to establish a relation between lesion size variation and the presence of possible predisposing hormonal factors. Although accurate FNH diagnosis may be made with MR avoiding biopsy in many patients, changes in size during follow-up should not dissuade use of this diagnosis.
Authors- 1
Person responsible for the study's integrity: CRF, LMB.
- 2
Conception of the study: CRF and LMB.
- 3
Design of the study: CRF and LMB.
- 4
Data acquisition: CRF, AT, ADV and CM.
- 5
Data analysis and interpretation: CRF and LMB.
- 6
Statistical treatment: CRF and LMB.
- 7
Bibliographic search: CRF.
- 8
Writing of the paper: CRF and LMB.
- 9
Critical revision of the manuscript with intellectually relevant contributions: LMB, AT, ADV, CM.
- 10
Approval of final version: CRF, LMB, AT, ADV, CM.
The authors declare that they do not have any conflict of interests.
Please cite this article as: Ramírez-Fuentes C, Martí-Bonmatí L, Torregrosa A, del Val A, Martínez C. Variación de tamaño de la hiperplasia nodular focal mediante resonancia magnética. Radiología. 2013;55:499–504.