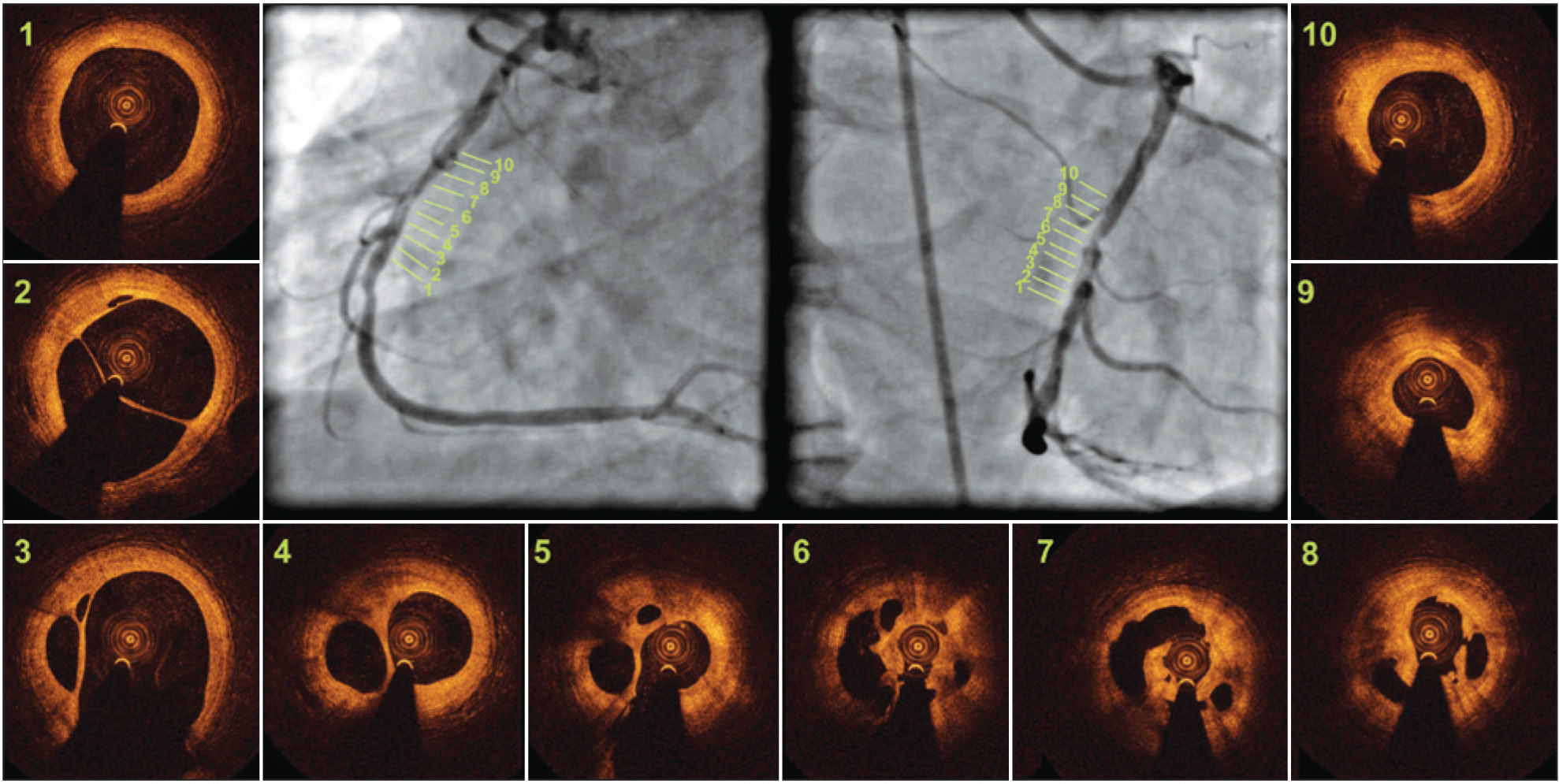
A 57-year-old male patient with a history of myocardial infarction two months before was treated conservatively. Coronary angiography evidenced a single lesion in the middle segment of the right coronary artery, with intraluminal haziness and preserved distal flow (Thrombolyis in Myocardial Infarction [TIMI] 3) (Figure 1).
– Angiography and optical coherence tomography. Angiography of the right coronary artery in two orthogonal projections, showing intraluminal haziness and preserved distal flow (TIMI 3). The optical coherence tomography images 1 and 10 indicate the references of the stenotic segment, while images 2 to 9 represent sections of the vessel along the stenotic segment, which measured 18.2mm in length. The presence of multiple intraluminal cavities can be observed, separated by tissue septa with high intensity and low attenuation of the light signal, and smooth inner surface, consistent with the presence of an organized, white, recanalized thrombus.
An evaluation with optical coherence tomography was performed in order to assess the morphology and composition of stenosis, in addition to guiding the intervention procedure.
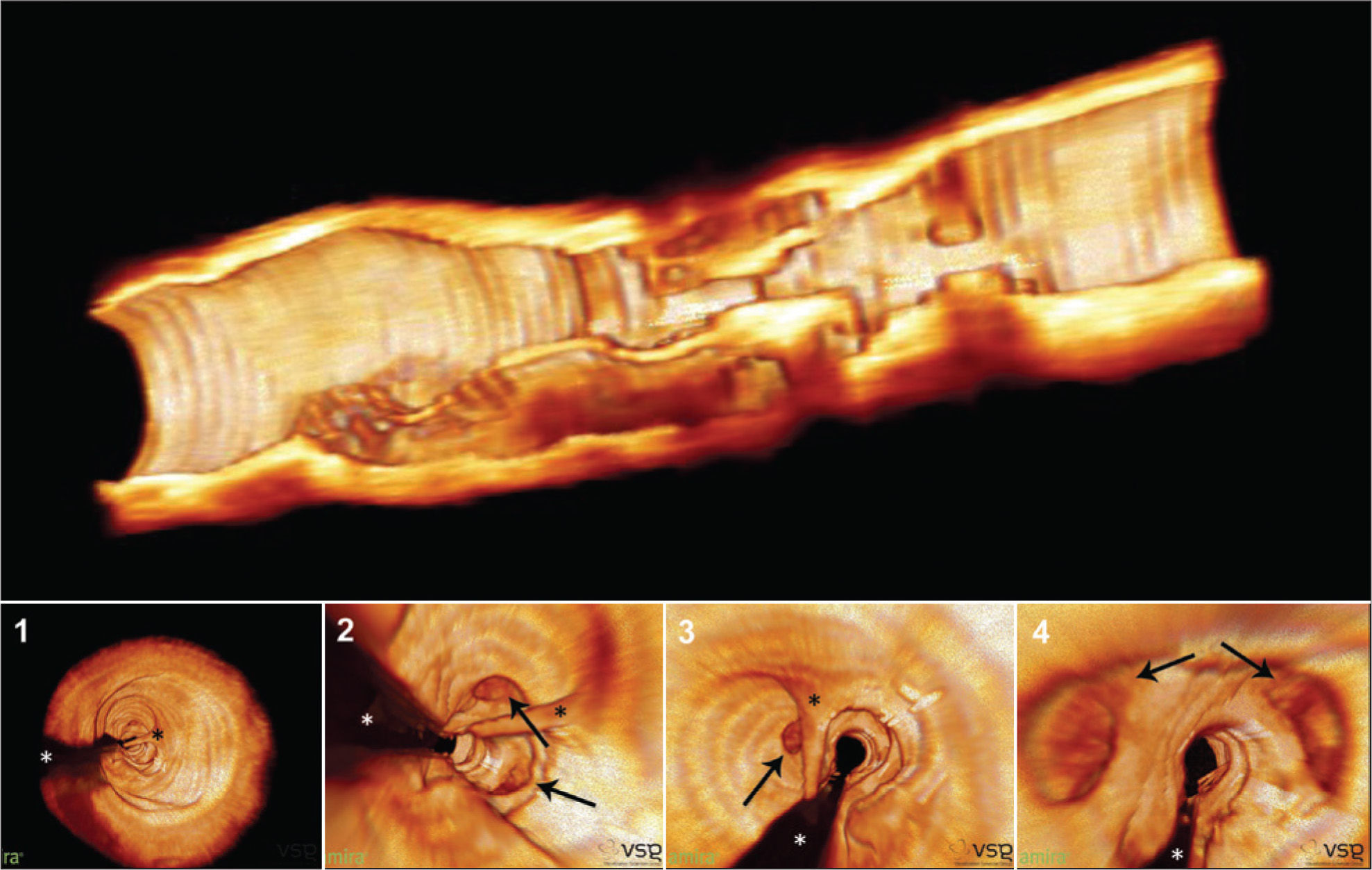
Figures 1 and 2 show a complex structure, with the vascular lumen divided into multiple cavities separated by high-intensity tissue and low attenuation of the optical signal, suggesting the presence of an organized, white, recanalized thrombus, which was crossed using a 0.014-inch hydrophilic guide with mouldable tip.
– Three-dimensional reconstruction of optical coherence tomography images. In the top panel, three-dimensional image of the open vessel in the longitudinal direction, showing multiple orifices and trajectories along the stenosis. In the lower panel, fly-through images of the coronary in the proximal-distal direction with large septum (black asterisks), separating the vascular lumen into two major cavities, and presence of multiple channels (arrows) throughout the trajectory. The shadow produced by the metal guide is indicated by the white asterisks.
Recanalisation or neovascularisation has been described by pathological studies in approximately one-third of old thrombotic coronary occlusions. Its size can vary, and it is characterized by multiple vascular channels created within the thrombus, with its surface covered by endothelium and separated by thin strands of connective tissue. This phenomenon is often underdiagnosed in angiographic studies. Although frequently found at the angiography, intraluminal filling defects are non-specific findings, and may correspond to several other pathological conditions, such as dissections, plaque rupture, calcification, aneurysms, and fresh thrombi. In this case, the use of optical coherence tomography allowed for the diagnosis and detailed morphological evaluation of the lesion with intraluminal haziness at the angiography.
CONFLICTS OF INTERESTThe authors declare no conflicts of interest.