Faced with the dilemma of extending the anesthesiology residency from 3 to 4 years, there have been several arguments for and against. However, the starting point of the discussion must be redesigning the national program curricula to move away from a fixed-time training and variable competencies, to a competency-based model; i.e., fixed competencies and variable time frames.
Ante la disyuntiva de prolongar la duración de la residencia en anestesiología de 3 a 4 años se han esgrimido varias razones de lado y lado. Sin embargo, la discusión debe partir de un rediseño curricular de los programas nacionales para dar el paso de un entrenamiento de tiempo fijo y competencias variables a el paradigma de educación basada en competencias, es decir, competencias fijas y tiempo variable.
The need to extend the time of the anesthesiology program in Colombia from 3 to 4 years has been discussed for over one decade. Those in favor argue that increasing the training to 4 years would ensure broad exposure of the resident to all areas of anesthesiology, including those that have been confined to the traditional curricula (i.e., trauma anesthesia or anesthesia for neonates). Those who are against change argue that based on case series, after 3 years of training residents are able to exceed by far the number of cases required to safely perform the primary procedures in our discipline and that extending the program also means prolonging the time during which the resident receives no income but has to pay for one more year of tuition. However, the approach and potential solution to this question is a curriculum that was labeled obsolete 100 years ago and was dismissed one decade ago in the United States and Europe.1,2
The current curriculum is based on the time residents are exposed to the various areas of anesthesiology, emphasizing the development of a curricular structure based on 2-month rotations. This type of curriculum is designed based on the knowledge the resident is expected to learn during his/her training. The learning processes depend on what the professors teach the residents; the objective is to acquire the knowledge pertaining to the discipline and the completion of the program is fixed, rather than variable.3 The problem with this approach is that professors are able to certify versus the regulatory agencies and the general public, that residents completed a minimum number of credits, including exposure to specific anesthesiology areas and that after 3 (or 4) years, we can attest to their knowledge, but to a lesser extent to their necessary skills and attitude required in clinical practice. However, is this really the case? The lack of uniformity in the quality of health care professionals in Colombia is no secret. The complexities of the health system and the growing pressure by the control agencies and by our patients, should lead us to optimize our residents’ skills and be able to effectively and reliably proof that residents have all the necessary competencies to treat patients safely and consistently. The term “competencies” refers to the evident ability of a healthcare professional to integrate multiple components such as knowledge, skills and attitudes.4
What shall we do then?Any medical undergraduate and postgraduate program shall be based on the attainment of competencies, rather than on structures and time periods. Competency-based education (CBE) is just the opposite of our current paradigm. CBE emphasizes the final result of the training process; in other words, the characteristics and skills of the future graduate professional, and this is different from emphasizing the contents we want to teach. Learning is not hierarchical and is equally dependent on the professor and the student. The objective is not to acquire knowledge, but knowing how to use that knowledge; furthermore, and the time to complete the program is not fixed but variable.3,4 Based on this model, we – the medical schools – shall then be able to certify exactly which are the capabilities of our residents, vouch to their competencies in all areas required in medical practice.5–7
How does this curricular model works?The underlying principle of CBE is that healthcare professionals must be competent in each and every field of the practice of medicine. CBE purports that they shall not be just expert physicians, but also need to perform roles that have been neglected in the traditional models but are nonetheless essential for our professional performance. In the Canadian model, for instance, the competency domains that must be mastered by their professionals are 7: expert physician, communicator, leader, health sponsor, academician and professional.8 In the United States and in Europe, these domains change discretely, but also focus on comprehensiveness.9,10 Additionally, a number of specific competencies were described within each domain, more clearly describing the domain characteristics. The message is that each program must be designed to ensure and assess that residents become competent in each of these domains. Under the current status of education in Colombia, do you as a professor have the necessary evidence to know whether your resident is able to communicate bad news? To properly lead a team during cerebral-cardio-pulmonary resuscitation? Is aware of the challenges of the current healthcare system and takes the appropriate steps?
Those who were skeptical of the CBE model argued that while the final result was clear in terms of the characteristics that healthcare professionals should have, it was difficult to translate these abstract domains into gradual, simpler, and above all, observable processes.11 This is why milestones were developed for each specific competency. Milestones are observable processes in daily practice corresponding to the progression of each competence domain of residents throughout their training. For instance, a first year resident must be capable of developing a complete medical record, identifying any relevant clinical problems, and understanding the process to obtain the informed consent as part of the pre-anesthesia evaluation under direct supervision. However, a last year resident shall be able to do it independently, to act as advisor to colleagues from other specialties, and making sure that the informed consent is comprehensive and understood by the patient. Through this approach, the actions that the residents shall be able to implement are specified, in accordance with their year of residency and for each particular competency. The model was criticized because competencies and milestones continue to be compartmentalized, and in the end these tools failed to consider the comprehensive nature of medical care, where the medical student shall be able to combine his/her different roles in a relevant manner.7,12
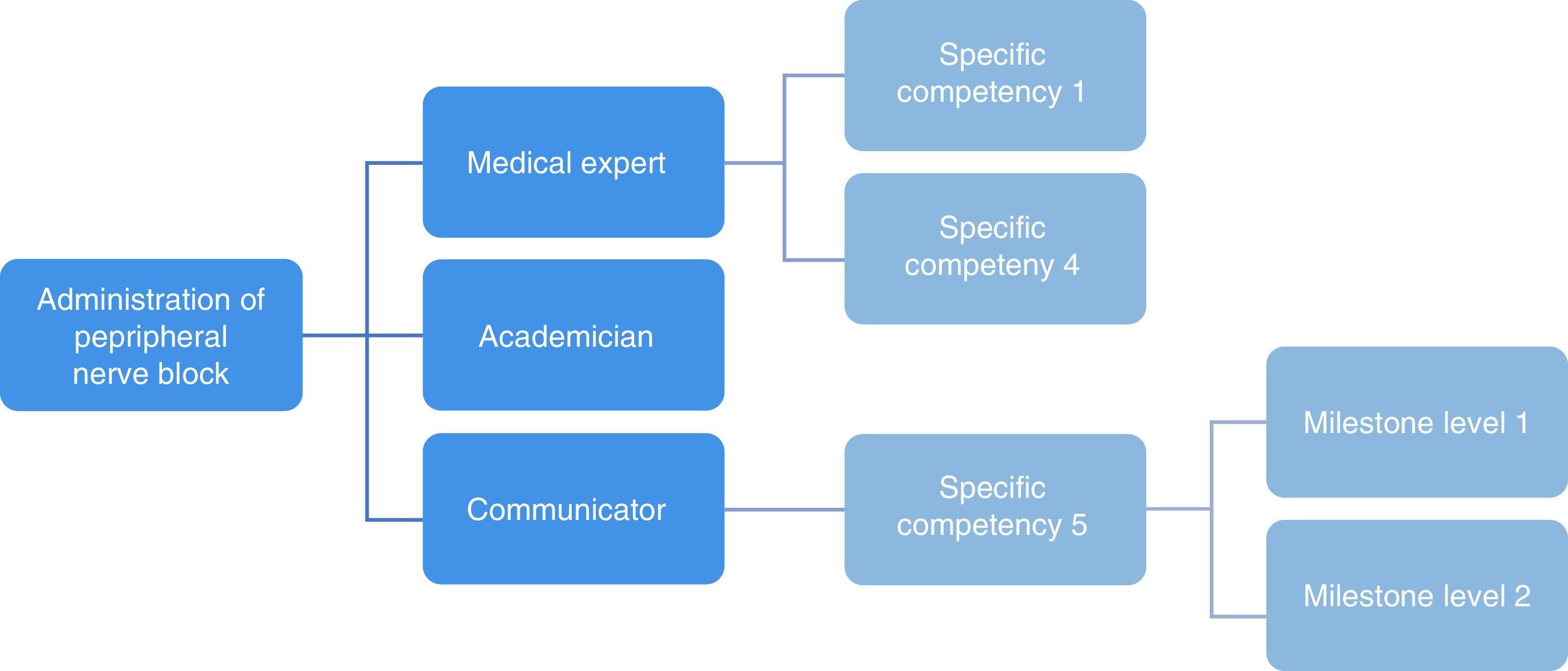
In response to these last concern, the Entrust able professional activities (EPA's) were developed. The EPAs are professional performance activities describing and demarcating the tasks of a particular discipline. These are professional activities that may be entrusted to the resident upon proof of his/her ability to perform properly.13 In order to carry out an EPA, the resident shall be able to integrate various competencies and their corresponding milestones domains to provide safe care to the patient.14 Some examples of EPAs in anesthesiology include management of acute postoperative pain or perioperative anesthesia care of the ASA I/II patient for intermediate risk surgery.15,16 Each EPA gives a basic description of the activity and specifies the competencies required for its implementation17 (see Fig. 1).
Relationship among EPAs, competency domains, specific competency and milestones in competency-based education. Source: Taken and reproduced with authorization of the Association of American Medical College. Core Entrust Able Professional Activities for Entering Residency: Curriculum Developers’ Guide, 2014.
If we establish the competency domains with their specific competencies, the milestones and the EPAs required for training of anesthesiology residents, we shall be able to identify the necessary educational activities throughout the residency period, the rotations needed and the evaluation methods to certify their achievements. The key is understanding that students achieve variable levels of competencies. There are some residents that make progress very quickly, while others take longer and have to work harder. What is important is to document each progress individually, in accordance with the capabilities exhibited by the resident. This means that there may be some residents that need less rotation time than others, or vice versa, some require longer rotations. Consequently, progress shall be subject to proof of competency. Likewise, it is possible that the same resident acquires a particular competency very quickly, while other domains may be more difficult to master. We all have had residents who excel in acquiring knowledge but experience difficulties with the necessary practical skills, or some that may even be both knowledgeable and skilled, but have poor interpersonal skills to relate with the patients or his/her peers. This does not mean that in order to train professionals that provide efficient and safe care, residents are hard pressed to develop these competencies prematurely; all residents shall be given a prudent period of time to develop their competencies, and shall be ensured that they will have the means to identify any difficulties and receive the necessary assistance to overcome those hurdles.3,18,19
This is why the discussion about the length of the anesthesiology program shall be reformulated and take a step back. We as members of a professional association are called to establish the minimum training requirements in terms of the components described in the CBE, to design a program that meets those needs and to create preliminary two-month rotations that lead the development of EPAs. The question we must answer is whether the average student requires 3 or 4 years of training to accomplish the final result. Probably it may take longer, but by no means less than 3 years. For instance, in the EU, the minimum length of time for a residency is 3 years, and in the UK, it may even extend to 7 years.20
If we insist in building solutions based on the traditional model, we may run the risk of simply continuing to emphasize the acquisition of knowledge, disregarding other equally relevant competencies and, in the long run, extending the training period during which the resident does not receive any compensation, but on the contrary, must pay high tuition fees. The latter point is particularly relevant for the training of physicians in Colombia, considering that in other countries such as Spain, extending the training period may even be beneficial to residents since they will have a secure job and remuneration for a longer period of time.
Why should we force the resident to comply with 4 years of the program when he/she has proven to be competent in all domains of competency and may independently perform all the EPAs in our discipline in 3 years? Or just the opposite, why shall we graduate anesthesiologists after 3 years of training, is they have proven to be competent in all the EPAs? Both scenarios are irresponsible, both for the resident as for his/her future patients.
However, the model exhibits certain limitations to be kept in mind. First there is a need to train the current professors since they have never received a competency-based education. The professor's commitment is a corner stone in the success of the implementation of the CBE. Secondly, tailor-made training necessarily entails longer times and professor dedication that goes hand in hand with tracking the individual, rather than collective, achievements of residents. Thirdly, any curricular change entails restructuring of the evaluation system that necessarily involves changing the mind-set and an additional burden for professors. We believe that despite the difficulties, it is worthwhile advancing towards the modernization of the residency programs in Colombia, since the impact in terms of health service quality improvement sufficiently compensates for any change-associated efforts.
FinancingThe authors did not receive sponsorship to carry out this article.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Olmos-Vega FM, Bonilla-Ramirez AJ. ¿3 o 4 años de residencia en anestesiología?: cómo plantear la discusión en términos de educación basada en competencias. Rev Colomb Anestesiol. 2017;45:128–131.