To describe a series of activities structured for managing the difficult airway in pediatrics and to suggest an algorithm adapted to the individual child's conditions.
Materials and methodsCase review of medical literature databases (PubMed, BIREME and MD consult); the search was based on the following keywords: algorithm, difficult airway, children and pediatrics in articles published during the last 10 years, including topic reviews, systematic reviews or algorithms. The principal authors who reviewed the articles were reviewed.
The algorithm design is based on an informal consensus of pediatric anesthesiologists and on the review of all the published literature, in accordance with the availability of resources and the experience in our environment.
ResultsThe result is a proposal for a simple algorithm including sequential one-way steps for managing the difficult airway in pediatrics. Particular emphasis is placed on situations such as a suspicious airway and a suggestion is made about the equipment and devices required to follow the algorithm. These equipment and devices may be adapted to the particular circumstances of the institution.
ConclusionThis review summarizes the management of the difficult airway in pediatrics and is the first proposal ever submitted in Latin America.
Describir una serie de actividades estructuradas para el manejo de la vía aérea difícil en pediatría y sugerir un algoritmo que se adapte a las condiciones de cada niño.
Materiales y métodosRevisión de las bases de datos de la literatura médica (PubMed, Biremey MD Consult) con una búsqueda con las palabras clave: algoritmo, vía aérea difícil, niños y pediatría, de artículos publicados en los últimos 10 años y que fueran revisión de tema, revisión sistemática o algoritmos. Los artículos fueron revisados por los autores principales. El diseño del algoritmo está basado en un consenso informal de anestesiólogos pediátricos y en la revisión de la literatura publicada, adaptado a la disponibilidad de los recursos y a la experiencia en nuestro medio.
ResultadosComo resultado presentamos una propuesta de un algoritmo sencillo, con pasos secuenciales y en un solo sentido para el manejo de la vía aérea difícil en pediatría. Se hace un énfasis especial en situaciones como la vía aérea sospechosa y se presenta una sugerencia de los equipos y dispositivos necesarios para aplicar el algoritmo, los cuales pueden ser adaptados en cada institución.
ConclusiónEsta revisión sintetiza el manejo de la vía aérea difícil en pediatría y es la primera propuesta realizada en Latinoamérica.
Perioperative airway problems in children continue to cause considerable perioperative morbidity and mortality.1 Oxygen desaturation below 80% and secondary hypoxia have been recently reported as the most frequent complications in the pediatric population and are age-dependent. Neonates and children under one year are the highest risk patients.2 Additionally, children have higher oxygen consumption and this results in a very poor tolerance to apnea (just a few seconds) and they usually develop significant hypoxemia leading to severe bradycardia.3,4 Airway problems do not present only in high-risk patients, since healthy patients with no predictors of difficult airway may also develop complications if managed by unskilled practitioners in situations where children are seldom treated and the adequate resources for each age group are not available.
Pediatric airway problems require an algorithm with simple strategies adapted to the local policies of the individual institution. This review provides a general overview of the difficult airway, its classification in children, a few suggestions about the minimum equipment requirements and an overview of the various procedures that may be followed when faced with an unexpected difficult airway, in order to avoid serious complications and side effects from hypoxia.
MethodologyThe data bases consulted for literature related to the algorithms published on the management of pediatric airway were PubMed, BIREME and MD consult. The keywords used were algorithm, difficult airway, children and pediatrics. The publications reviewing the topic, systematic reviews or algorithms for airway management in the last 10 years either in English or Spanish, were selected. The two principal authors revised the articles. The design of the algorithm is based on an informal consensus of pediatric anesthesiologists from two children hospitals (Rooselvelt Institute of Pediatric Orthopedics in Colombia and Royal Aberdeen Children's hospital in the UK) for managing the difficult airway in children and adapted to the availability, experience and usefulness of the devices available in our environment.
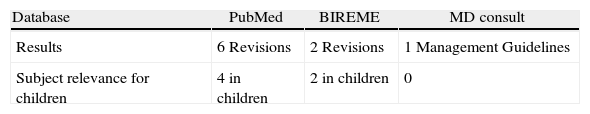
ResultsThe literature identified on the algorithm of the difficult airway in children is quite limited. One of the findings was a publication in the Spanish Journal of Anesthesiology and Resuscitation and some articles providing practical management guidelines based on local experts consensus from pediatric institutions (Table 1). We then believe that the algorithm proposed is a novel and valuable contribution to medical literature, in addition to providing simple and friendly orientation on a problem frequently seen in pediatric anesthesia.
The routine management of the difficult airway is usually easy in experienced hands. The problems with tracheal intubation are more common in children under one year of age, with an estimated incidence of 0.6%; this incidence drops to 0.1% in children of pre-school age and to 0.05% in children older than 8 years of age. Difficulties in facemask ventilation in a healthy child with normal anatomy are extremely rare.5 This is an important consideration since oxygenation and prevention of hypoxia will always be possible.
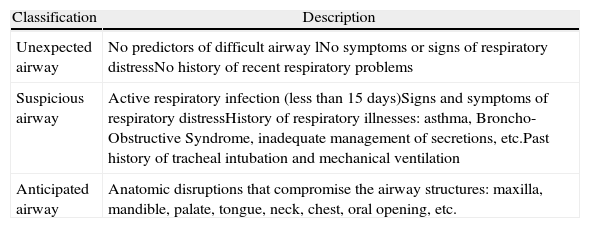
Children's airway may be classified into three types (Table 2): the normal or unexpected airway, the suspicious airway and the anticipated difficult airway.
Airway classification in children.
| Classification | Description |
| Unexpected airway | No predictors of difficult airway lNo symptoms or signs of respiratory distressNo history of recent respiratory problems |
| Suspicious airway | Active respiratory infection (less than 15 days)Signs and symptoms of respiratory distressHistory of respiratory illnesses: asthma, Broncho-Obstructive Syndrome, inadequate management of secretions, etc.Past history of tracheal intubation and mechanical ventilation |
| Anticipated airway | Anatomic disruptions that compromise the airway structures: maxilla, mandible, palate, tongue, neck, chest, oral opening, etc. |
The most frequent cases occur in the unexpected or unforeseen airway, where there is an acute airway obstruction as a result of lack of experience or due to the wrong maneuvers in the airway. Such obstruction may be anatomic (due to soft tissue or the tongue) or functional (due to dynamic closure of the glottis). These patients usually have a normal airway with no predictors of difficult airway. The problems arise in a critical and acute manner, hence requiring an immediate solution with a simple algorithm that may be followed in every scenario, is practical and includes consecutive and effective strategies (read further).
The suspicious airway is more difficult to approach since it requires experience in pediatric anesthesia. It is the result of inflammation of the respiratory tract, trauma, foreign bodies or allergies. These children exhibit clinical signs or symptoms suggesting some kind of airway patency disruption. Usually they show up during emergency surgery, when children suffer from active respiratory infection, chronic respiratory disorders such as asthma, bronchial obstructive syndromes or poor management of respiratory secretions and require an emergency surgical procedure. These patients are at high risk of acute airway obstruction due to laryngospasm and perioperative ventilation failure. Although they do not have any airway anatomic defects (difficult intubation), they should be considered as a difficult airway.
Finally there is the anticipated difficult airway that should be managed by experienced pediatric anesthesiologists in institutions with appropriate human and technological resources available. These patients have evident anatomical malformations compromising the airway and may be congenital (genetic syndromes) or acquired (trauma, surgery or burns). The pathologies compromising the trachea and the subglottis, as well as anterior mediastinal masses, are a challenge, even for the most experienced pediatric anesthesiologist.
The unexpected difficult airwayPredicting the level of airway difficulty in children is not easy because the predictors used in adult patients may not be applicable to children. The predictors that have shown good sensitivity and specificity such as mandibular protrusion, Mallampati's classification and movement of the atlanto-occipital joint are very difficult to assess in children, particularly in children less than 3 years of age.6
The intermaxillary distance or the gap between the upper and lower incisors, the thyromental distance, the temporomandibular joint movement measured as mouth opening (the mouth opening is appropriate when the patient is able to place two of his/her fingers in the vertical direction inside the mouth), and mandibular disorders, such as retrognatia, micrognatia or prognatism, are all easier to assess in children.7 These predictors may be useful when complemented with the clinical record and good questioning aimed at identifying specific symptoms of airway functional problems such as stridor, snoring, dysphonia, suction or swallowing disorders, obstructive sleep apnea syndrome, or abnormal sleeping positions. The physical examination is intended to identify any craniofacial anomalies, genetic syndromes, or dysmorphic features that may compromise the anatomy or the physiology of the respiratory tract.8 A simple inspection contributes with very useful information, particularly when the child cries or is being fed, since it is then possible to simultaneously evaluate the mouth opening, the tongue, the teeth, the velopalatal coordination and the patency throughout the airway.
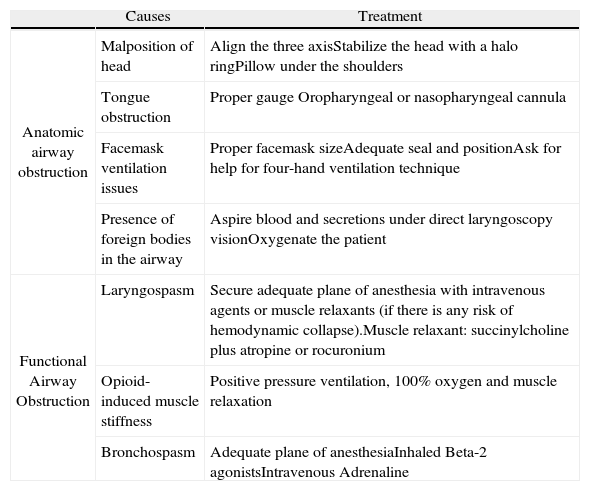
The main causes of anatomic or functional obstruction of the airway in children are described in Table 3.
Causes and treatment of airway obstruction in children.
| Causes | Treatment | |
| Anatomic airway obstruction | Malposition of head | Align the three axisStabilize the head with a halo ringPillow under the shoulders |
| Tongue obstruction | Proper gauge Oropharyngeal or nasopharyngeal cannula | |
| Facemask ventilation issues | Proper facemask sizeAdequate seal and positionAsk for help for four-hand ventilation technique | |
| Presence of foreign bodies in the airway | Aspire blood and secretions under direct laryngoscopy visionOxygenate the patient | |
| Functional Airway Obstruction | Laryngospasm | Secure adequate plane of anesthesia with intravenous agents or muscle relaxants (if there is any risk of hemodynamic collapse).Muscle relaxant: succinylcholine plus atropine or rocuronium |
| Opioid-induced muscle stiffness | Positive pressure ventilation, 100% oxygen and muscle relaxation | |
| Bronchospasm | Adequate plane of anesthesiaInhaled Beta-2 agonistsIntravenous Adrenaline |
The initial management of ventilation in children begins with a sound facemask technique and the initial maneuvers to achieve patency of the airway. Daily practice and education are the pillars for achieving good results in time. The causes of functional or mechanical obstruction must be ruled out. In the latter case, it is critical to rule out the presence of foreign bodies, regurgitation, blood or secretions inside the airway that must be immediately suctioned under direct vision with laryngoscopy.
Tracheal intubation should be attempted once the airway has been cleared and a proper anesthetic plane is secured. The initial approach to intubation should always be direct laryngoscopy, except for those cases with a medical or surgical history of anticipated difficult airway that requires an initial approach with a different device. Forced intubation with the glottis closed or in an improper anesthetic plane should be avoided, since it causes airway trauma and worsens the obstruction, leading to desaturation, hypoxia and secondary bradycardia.
There are other causes of obstruction and airway dysfunction that are not easy to recognize at the physical examination of children; for instance, the subglottic stenosis that should be suspected in every patient with a history of intubation and mechanical ventilation. These cases require using balloon-free and smaller tracheal tubes for a successful tracheal intubation and, under extreme circumstances, requires the participation of a surgeon to dilate the trachea.
When facemask ventilation is not possible because of anatomic supraglottic obstruction or whenever the maneuvers for securing a patent airway are difficult to perform, a laryngeal mask (LMA) or other supraglottic device (SGD) may be used to correct the obstruction, ventilate and oxygenate, while alternate plans to accomplish the tracheal intubation are established.9
Functional airway problems may arise from several causes but the most frequent one is an inadequate plane of anesthesia that results in laryngospasm or bronchospasm. Similarly, the rapid administration of a bolus of intravenous opioids in children may result in woody thorax and even glottis closure making ventilation difficult.10,11
Laryngospasm as a consequence of inadequate plane of anesthesia requires early treatment. The administration of additional doses of hypnotics such as propofol is a common practice, but may have an important hemodynamic impact and result in severe hypotension.12,13 Muscle relaxation is more appropriate, particularly in the presence of severe hypoxia, bradycardia or impending cardiovascular collapse.14 Muscle stiffness from opioids, with or without glottis closure, also requires muscle relaxation with short-acting drugs such as succinylcholine (0.5–1mg/kg), always accompanied by a dose of intravenous atropine or rocuronium (0.5mg/kg).15 When a venous access is not available in children, the relaxant may be administered intramuscularly or intraosseously. The latter is more recommended because it ensures a faster and more predictable onset of action of the drug.
Airway rescue options show up in the algorithm in case of emergency situations: “Can’t intubate, Can’t ventilate”. This is the worse case scenario, and fortunately, it is very rare in pediatric anesthesia. Such a situation calls for a surgical approach such as tracheostomy, surgical or needle cricothyroidotomy. In children less than 8 years, a needle cricothyroidotomy is favored, while the equipment is prepared for an open tracheostomy performed by a surgeon. Percutaneous cricothyroidotomy is indicated in patients older than 8 years of age, because the airway structures are similar to those in adults and the probability of an airway injury or the development of a false route is less likely. An experienced pediatric or ENT surgeon should be present whenever a difficult airway is anticipated. Rigid bronchoscopy is also a good option usually used by pediatric surgeons to approach the airway, removing foreign bodies or dilating the tracheal stenosis.
However, although there is little evidence to make absolute recommendations of some of these options in children, these are options available in our environment and in some cases they may save the life of a patient. The initial trial in animal models suggest that surgical cricothyroidotomy may be superior to the needle technique in pre-school patients16,17; even in adults, needle cricothyroidotomy has not been quite successful18,19; although it continues to be an option as part of the airway algorithm to supply oxygen for a few minutes. These techniques are desperate measures to help us remember that ventilation and oxygenation are critical, before proceeding to tracheal intubation.
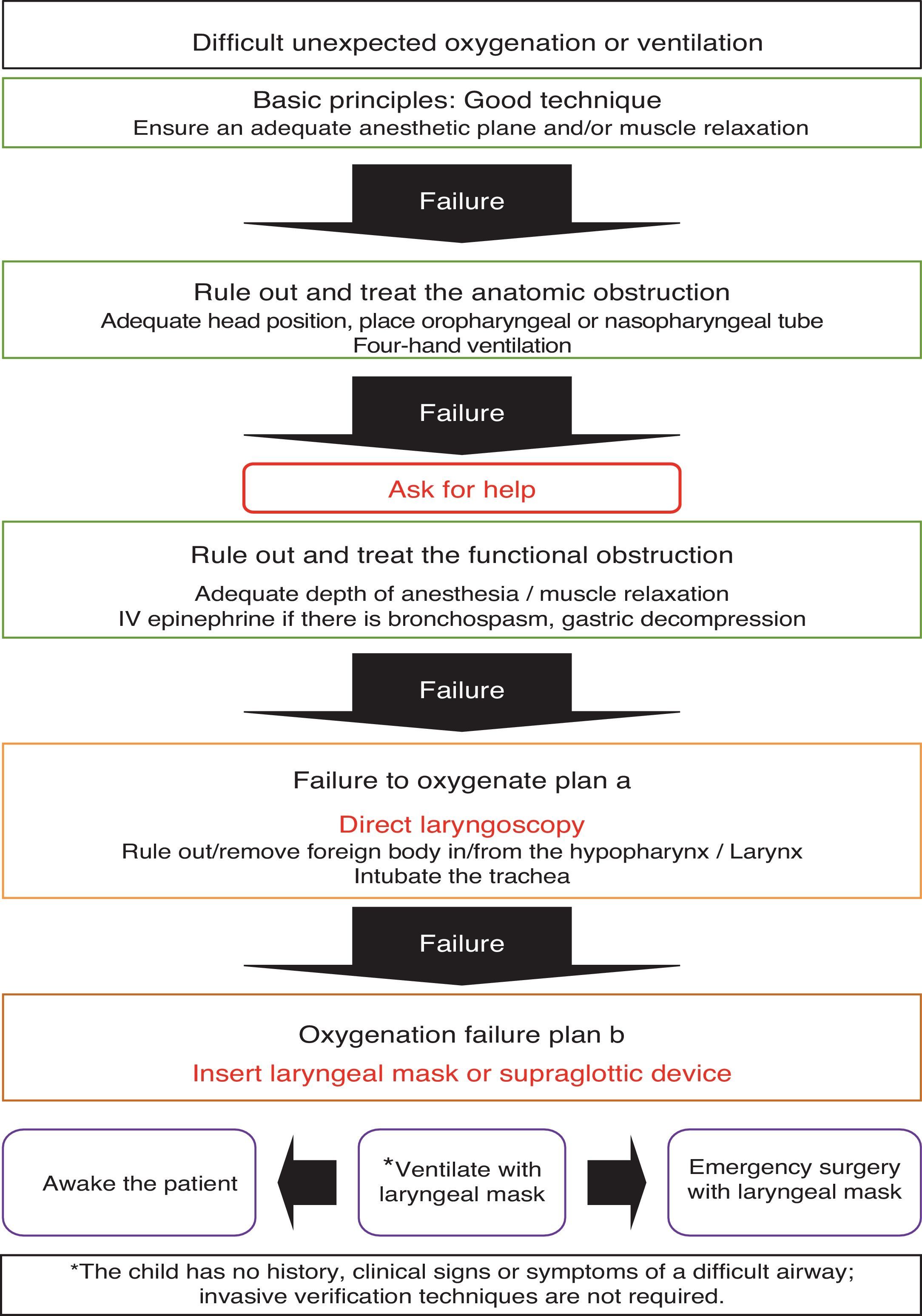
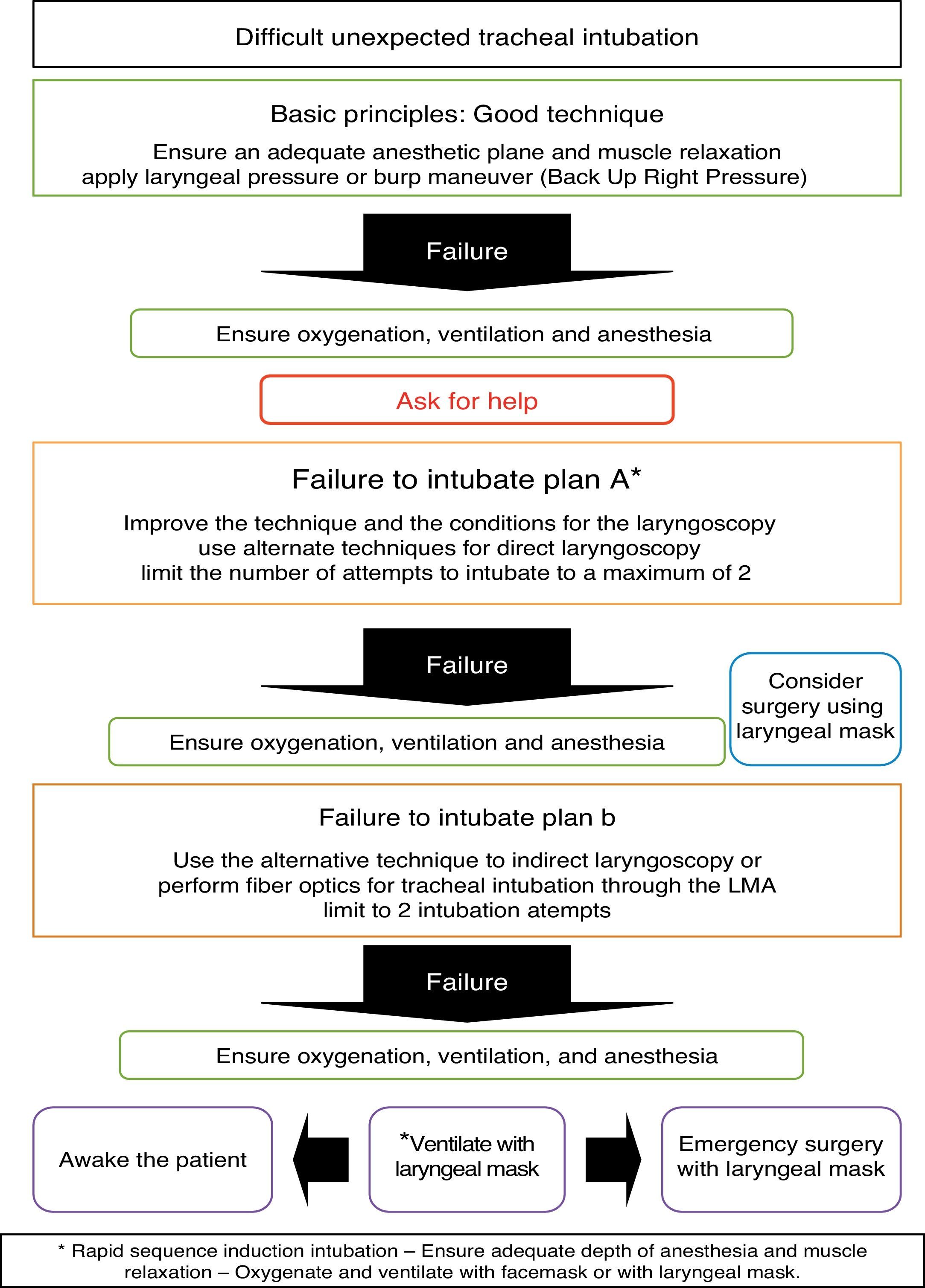
Based on this analysis a simple algorithm is described to achieve ventilation and tracheal intubation in children with unexpected difficult airway (Figs. 1 and 2). This algorithm is intended simply as a guide to be adapted to the local conditions, the equipment available and the institutional experience.
The initial treatment is based on improving the basic maneuvers such as correcting the patient's position to ensure a patent airway, using an oropharyngeal or a nasopharyngeal cannula and the four-hand ventilation technique with two people in charge. Pre-oxygenation with 100% oxygen is useful since it provides a few additional minutes for manipulating the airway; however, it is not easy to do when children are awake and therefore the child should be sedated or must be performed under anesthetic induction. When these maneuvers fail, help must be sought and simultaneously identify and start treatment to solve the anatomical or functional airway problems and apply the management algorithm.
Direct laryngoscopy is Plan A or the initial plan to confirm the difficulty for intubation, in addition to helping to rule out or remove any foreign bodies that may obstruct the glottis. If the vocal folds can be visualized and these are open, the trachea shall then be intubated. Intubation should not be forced because it may lead to severe tissue trauma and turn a difficult airway into an unmanageable airway. If intubation is not possible, a supraglottic device such as the laryngeal mask may be used as an alternative to facemask ventilation in order to secure the child's ventilation and avoid operator fatigue, while other options are prepared for tracheal intubation. Oxygenation and ventilation are the key components.
In order to facilitate the intubation, whether with direct laryngoscopy or with video laryngoscopy, it is recommended to place the patient in the right position to align the airway axis and to do the BURP maneuver (Back Up Right Pressure) that improves the visualization of the vocal folds.20 If the initial plan fails, help must be sought and have an alternate plan prior to the administration of the muscle relaxant. Plan B following a failed laryngoscopy – whether as a result of poor technique or inadequate conditions of the patient – is a new instrument-assisted laryngoscopy performed by a different operator to facilitate the tube passage into the trachea; i.e., guides, bougies, various types of blades, stylets or video laryngoscopes, for a maximum of two attempts. Ideally plan B should include a fiber optic nasal intubation technique, or an oral approach using a laryngeal mask. It should be emphasized that direct laryngoscopy intubation attempts should be limited (no more than three) to prevent airway tissue trauma. In some cases you may even consider an initial surgical approach of the airway, with facemask or supraglottic devices.
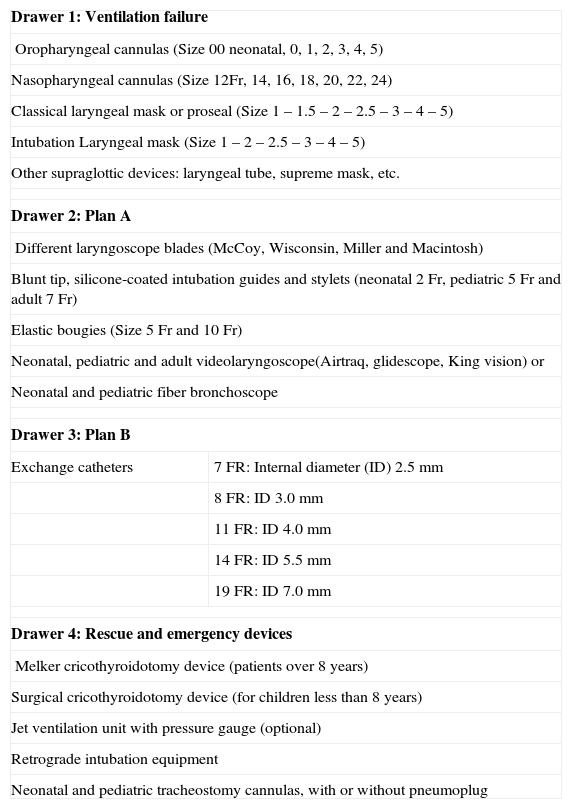
It is highly recommended to have available a difficult airway cart containing various devices for various pediatric ages, in addition to the equipment needed in case of an emergency and to be able to follow the algorithm. Table 4 illustrates a list of the minimum equipment and devices necessary that should be available in the cart.
Suggested Equipment and devices for the difficult airway cart in pediatrics.
| Drawer 1: Ventilation failure | |
| Oropharyngeal cannulas (Size 00 neonatal, 0, 1, 2, 3, 4, 5) | |
| Nasopharyngeal cannulas (Size 12Fr, 14, 16, 18, 20, 22, 24) | |
| Classical laryngeal mask or proseal (Size 1 – 1.5 – 2 – 2.5 – 3 – 4 – 5) | |
| Intubation Laryngeal mask (Size 1 – 2 – 2.5 – 3 – 4 – 5) | |
| Other supraglottic devices: laryngeal tube, supreme mask, etc. | |
| Drawer 2: Plan A | |
| Different laryngoscope blades (McCoy, Wisconsin, Miller and Macintosh) | |
| Blunt tip, silicone-coated intubation guides and stylets (neonatal 2 Fr, pediatric 5 Fr and adult 7 Fr) | |
| Elastic bougies (Size 5 Fr and 10 Fr) | |
| Neonatal, pediatric and adult videolaryngoscope(Airtraq, glidescope, King vision) or | |
| Neonatal and pediatric fiber bronchoscope | |
| Drawer 3: Plan B | |
| Exchange catheters | 7 FR: Internal diameter (ID) 2.5mm |
| 8 FR: ID 3.0mm | |
| 11 FR: ID 4.0mm | |
| 14 FR: ID 5.5mm | |
| 19 FR: ID 7.0mm | |
| Drawer 4: Rescue and emergency devices | |
| Melker cricothyroidotomy device (patients over 8 years) | |
| Surgical cricothyroidotomy device (for children less than 8 years) | |
| Jet ventilation unit with pressure gauge (optional) | |
| Retrograde intubation equipment | |
| Neonatal and pediatric tracheostomy cannulas, with or without pneumoplug | |
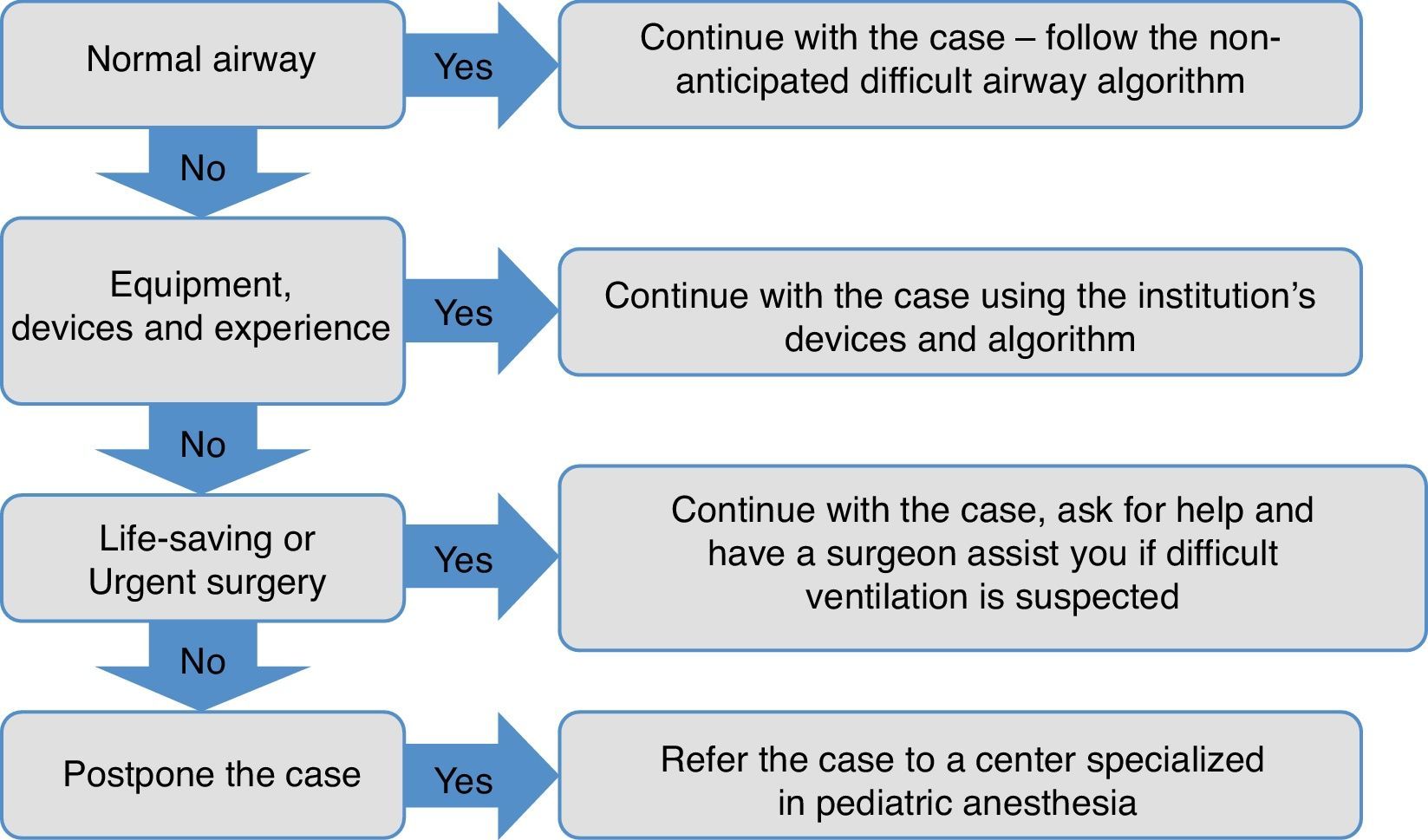
Children with anticipated difficult airway require trained practitioners in pediatric anesthesia and a careful planning of the particular case. Fortunately, these situations are rare in pediatric anesthesia and they are usually elective procedures for which there is enough time for proper evaluation and planning of the case, including equipment, staff and all the necessary resources. Fig. 3 shows the proposed algorithm for managing these type of patients.
The following section is a discussion of the principles and the most frequent scenarios with these patients.
Suspicious difficult airwayRespiratory infections, foreign bodies inside the airway, bleeding and trauma of airway tissues may suddenly turn the suspicious airway into a difficult airway. The severity of the symptoms and the rate at which they develop determine the urgency and the need to proceed to an intervention. The patient's underlying disease demands a timely recognition and treatment should focus on two key areas: (1) the cause of the obstruction; is it anatomical or functional? and (2) How much time do I have before requiring an intervention? Experience in pediatric anesthesia is key to the successful management of these patients.
Many of these children require emergency surgery that constitutes a dual challenge: choosing the best anesthetic technique and the strategies for manipulating the airway. Supraglottic devices such as the laryngeal mask or oropharyngeal cannulas should be used with care because in some cases they may worsen the airway problems by increasing the risk of laryngospasm or displacing foreign bodies inside the airway. However, an intubation laryngeal mask may be a lifesaver in a failed tracheal intubation of a patient with active airway bleeding when facemask ventilation is not feasible and video laryngoscopes fail to provide adequate visibility; this device allows for oxygenation of the patient and for tracheal intubation. The participation of a surgeon or ENT doctor should be considered when the anesthesiologist lacks the expertise, in the presence of severe obstruction under the glottis, or in case of difficulty to establish adequate patient oxygenation/ventilation; under such circumstances, consideration should be given to the possibility of a surgical access of the airway.
Expected or anticipated difficult airwayThese patients have anatomical alterations of the airway, the neck or the chest that makes intubation and/or ventilation difficult. They require a multidisciplinary approach in institutions where these patients are assessed by pediatric anesthesiologists, pediatricians, ENT physicians and pediatric surgeons to lower the risk of complications and avoid hypoxia and its fatal consequences.19,21 These patients should be ideally scheduled for elective surgery after careful planning and selecting various options to manage the airway; these options should be readily available when taking care of the patient. Only the urgent surgical cases should be managed outside this scenario and require the participation of at least two anesthesiologists and one surgeon.
These patients may present any of the following situations: difficult facemask ventilation defined as the difficulty to establish adequate ventilation because of improper seal, excessive ventilation leaks or because of a huge resistance to the inflow or outflow or air, which leads to hypoventilation, desaturation, cyanosis, gastric insufflation or non-availability of capnography; difficult laryngoscopy is defined as the difficulty or impossibility to visualize part of the vocal folds after two or more attempts of laryngoscopy by a trained anesthesiologist; finally, difficulty for tracheal intubation is defined as the difficulty to introduce a tube inside the trachea after multiple attempts and when two or more devices have been used for intubation.22
Maintaining spontaneous ventilation with inhaled induction, intravenous induction or a mixed technique is a useful strategy to check facemask ventilation if possible and to ensure the patient's ventilation while the airway management maneuvers are performed. The benefit of this approach is that it gives us more time to do various intubation maneuvers without having to interrupt the procedure to ventilate the patient, making it more reassuring and comfortable for the operator. Muscle relaxation is not an absolute contraindication in difficult airway patients provided they can be ventilated with a facemask to avoid the “Can’t intubate/Can’t ventilate” situation. However, the apnea produced by relaxation reduces the time required for the tracheal intubation maneuvers, requires permanent ventilation assistance and a highly skilled and experienced practitioner to manipulate the airway.
Facemask ventilation may be optimized using devices such as the oropharyngeal or nasopharyngeal cannula, four-hands ventilation technique, or the use of a supraglottic device such as the laryngeal mask.17 A surgeon has to be present when the patient presents major airway edema or clear and known history of difficult facemask ventilation and when the oxygenation rapidly deteriorates.
There is a wide range of alternatives and options for managing the airway in our environment, including: intubation with supraglottic devices, optical instruments or video laryngoscopes23 and more invasive techniques such as retrograde intubation, cricothyroidotomy and tracheostomy. Fiber optic tracheal intubation continues to be the preferred device for managing the anticipated and elective airway in children24; however it entails considerable drawbacks because it has a long learning curve, so it cannot be used in critical or emergency scenarios because it is time consuming and its success drops in the presence of bleeding or abundant secretions inside the airway.
Tracheostomy is a final option to be considered in cases of difficult airway in children and should be planned from the beginning, before edema, bleeding or repeated airway trauma hinder ventilation of the patient. In severe cases with a considerable airway distortion, a prophylactic tracheostomy should be considered to ensure the patient's safety not just intraoperative, but also during the immediate postop and throughout the hospitalization.25
There are a special group of patients, like newborn babies with congenital airway malformations (giant hygromas, lymphangiomas or head and neck tumors) that require urgent airway approach and very usually the tracheal intubation is done with the patient awake immediately after birth.26 The laryngeal mask may also be used in the newborn baby that is awake, using topical anesthesia; once the ventilation is secured, you may try to intubate using fiber optics through the laryngeal mask.27–29
Patients with a difficult airway should be extubated fully awake and when total recovery of the neuromuscular function has been verified. Some authors recommend doing a reversible extubation with a tube exchange catheter in difficult airway patients and with additional risk factors for emergency reintubation.30
Rapid sequence intubationRapid sequence induction (RSI) is done to deliver tracheal intubation is the shortest possible time. The classical technique is not recommended in children because of the inability to oxygenate or ventilate them prior to laryngoscopy. This situation usually results in hypoxia and hypotension.31 A gradual inhalation induction with spontaneous ventilation (in the absence of vascular access) or a titrated intravenous induction that ensures adequate depth of anesthesia without causing a cardiovascular prolapse are the most frequently used options in children. Upon confirming the patency of the airway, a short-acting muscle relaxant may be administered and intermittent mild facemask ventilation may be administered to avoid gastric bloating and secondary regurgitation, while the necessary maneuvers are applied for placement of a tracheal tube with a pneumoplug.32–35
ConclusionsAnticipating difficult airway problems in children and having a structured approach mark the difference between good and poor outcomes. A preliminary evaluation, experience and adaptation of the algorithm to the local conditions and availabilities should altogether accomplish the goal and prevent the serious consequences of perioperative hypoxia. The algorithm herein discussed is simply a practical guide that may be adapted to the conditions of the particular institution, in accordance with the available resources, the complexity of the patients and a staff with considerable experience in pediatric patients.
Continuous education, training and clinical simulation in emergency situations are necessary strategies for developing the skills and competencies in pediatric anesthesia, with a view to prepare the human team responsible for taking care of children and as part of the pediatric health care quality improvement process.
FundingAuthors’ resources.
Conflict of interestNone.
Dr. Bruno Bisonnette. Children of the world Anesthesia Foundation. www.cotwaf.com.
Please cite this article as: Marín PCE, Engelhardt T. Algoritmo para el manejo de la vía aérea difícil en pediatría. Rev Colomb Anestesiol. 2014;42:325–334.