Analgesic management in patients with bilateral trauma to the shoulder or the proximal third of the arm is difficult. The multimodal strategy based on the administration of local analgesics to the brachial plexus appears to be the most effective; however, there are risks associated with bilateral blocks, including phrenic nerve palsy, toxicity due to local anesthetics, and bilateral pneumothorax. These risks may be diminished using an ultrasound-guided supraclavicular approach to the brachial plexus.
This paper describes the management of a patient with bilateral injury to the shoulder and the proximal third of the humerus. The patient is taken to bilateral humeral fixation surgery and develops severe post-operative pain which does not respond to high-dose opioids and anti-inflammatory agents. He is managed initially with bilateral ultrasound-guided supraclavicular block using a low volume of a local anesthetic followed by continuous administration of bupivacaine. Pain assessment was 2/10 at 24h and 3/10 at 48h.
We concluded that bilateral supraclavicular blockade is an option in the acute management of pain after surgery to the shoulder and the proximal third of the humerus. Continuous administration of local anesthetics to the brachial plexus helps maintain the analgesic response.
El manejo analgésico de los pacientes con trauma bilateral de hombro o tercio proximal del brazo es difícil. La estrategia multimodal basada en administración de anestésicos locales en el plexo braquial parece ser la más efectiva, pero hacer bloqueos bilaterales tiene riesgos asociados, como son: la parálisis del nervio frénico, la toxicidad por anestésicos locales y el neumotórax bilateral. Estos pueden ser disminuidos con una aproximación supraclavicular al plexo braquial y el uso de ultrasonografía.
Describimos el manejo de un paciente con trauma bilateral de hombro y tercio proximal de húmero, quien es llevado a cirugía de osteosíntesis bilateral de húmero y presenta dolor postoperatorio severo que no responde a dosis altas de opiáceos y antiinflamatorios. Es manejado inicialmente con bloqueo supraclavicular bilateral guiado por ecografía con volumen bajo de anestésico local y posteriormente administración continua de bupivacaína, con una valoración del dolor de 2/10 a las 24h y 3/10 a las 48h.
Concluimos que el bloqueo supraclavicular bilateral es una opción para el manejo del dolor agudo en cirugía de hombro y tercio proximal de húmero. La administración continua de anestésicos locales al plexo braquial contribuye a mantener la respuesta analgésica.
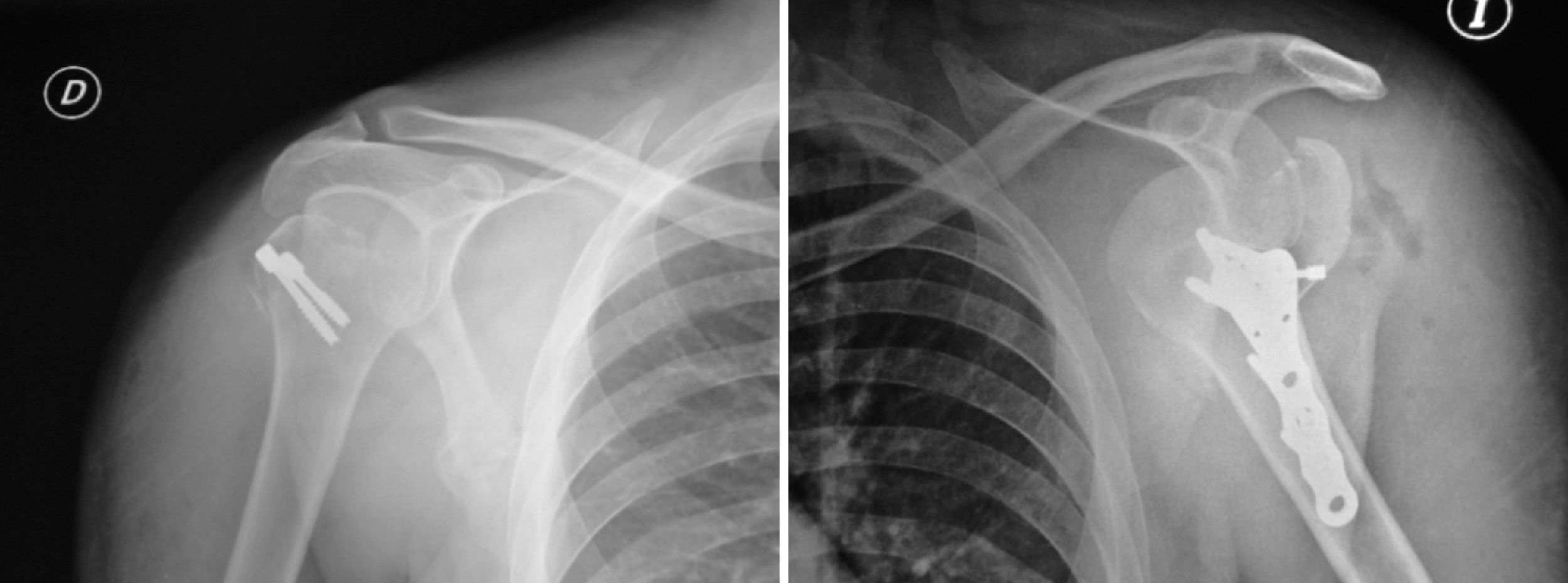
Thirty-five year-old male patient complaining of pain in both shoulders and functional impairment of one day of duration. X-rays show a fracture dislocation of the left shoulder and dislocation of the right shoulder. The patient is taken to surgery for closed reduction of both shoulders. A left inter-scalene block is performed for post-operative analgesia, using 15ml of 0.375% levobupivacaine.
Two days later the patient is taken to surgery for bilateral humeral fixation and repair of the left rotator cuff (see Fig. 1).
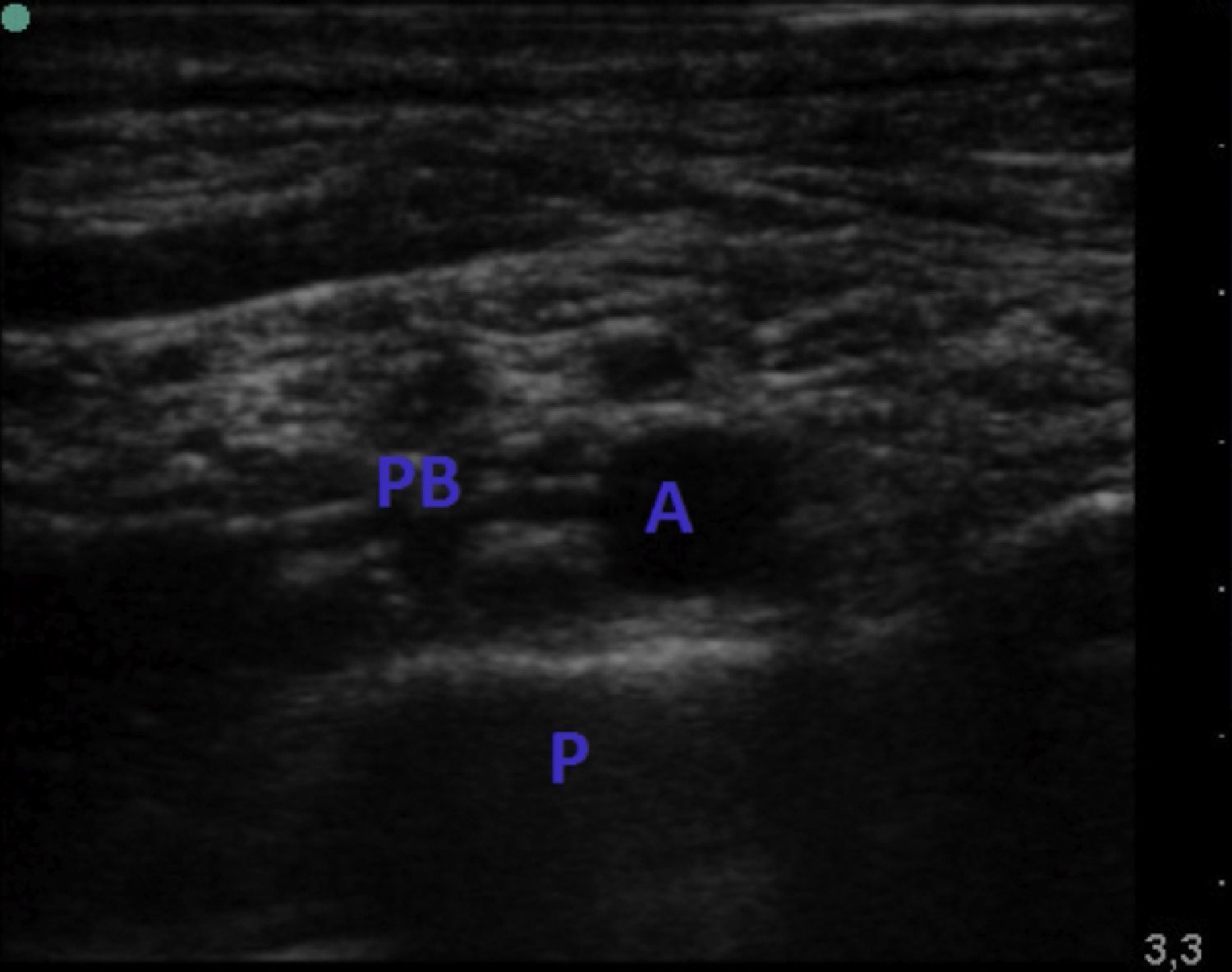
During the post-operative period, the patient developed severe pain, which did not improve despite high-dose opioids and NSAIDs. It is decided to perform a bilateral supraclavicular block (see Fig. 2) using 10cc of 0.375% levobupivacaine in each side, achieving pain control during a 12-h period.
Following the two blocks, the patient does not show evidence of respiratory distress or desaturation at any time. No abnormality is found in the chest X-ray.
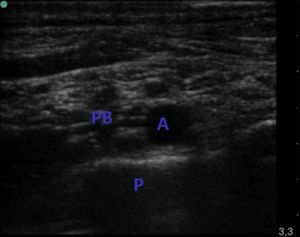
After 12h, the pain came back and was assessed as 10/10 on the verbal numerical scale, particularly in the left shoulder. Consequently, it was decided to place a left supraclavicular catheter for continuous infusion of 0.1% bupivacaine at a rate of 5cc per hour (see Fig. 3), achieving good pain control assessed as 2/10 at 24h and 3/10 at 48h (see Fig. 4).
DiscussionShoulder surgery is associated with significant post-operative pain requiring the use of high-dose opioids that favor the occurrence of adverse effects such as vomiting, nausea, pruritus, respiratory depression and urinary retention.1
The best strategy for the control of post-operative pain in shoulder surgery is a multimodal approach consisting of the concomitant use of NSAIDs, opioids and local anesthetics, either through a nerve block or infiltration into the wound.2
Peripheral blocks with local anesthetics used in this type of surgery include: interscalene, subacromial, intra-articular, suprascapular and axillary nerve blocks.1,3 The subacromial infiltration is performed by the surgeon before closing the surgical wound, by filling the subacromial space with 20–50cc of local anesthetic. This simple technique is a good alternative to interscalene blockade because it does not produce the adverse effects of this block; however, if done repeatedly, it may lead to chondrolysis associated with local anesthetics.4,5
Blockade of the axillary nerve (through any approach), and of the suprascapular nerve, ensures complete shoulder analgesia.6 The technique most frequently used to achieve this blockade is the interscalene approach to the brachial plexus. The single access provides good analgesia, although short-lasting; for this reason the use of continuous block in very painful surgeries is needed.1
The continuous interscalene block is a technique commonly used in the management of post-operative shoulder surgery, but one of most frequent adverse effects associated with its use is phrenic nerve paralysis, a contraindication for bilateral blocks. It has been found that this block may reduce vital capacity by 50%, and this is why patients with associated lung diseases cannot tolerate it.1
The supraclavicular block is often used as an analgesic or anesthetic technique in surgeries below the middle third of the arm,7 and it is less frequently associated, when compared to the interscalene block, with adverse reactions such as Horner's syndrome, recurrent laryngeal nerve palsy, and symptomatic diaphragmatic paralysis.1 It may also be used for shoulder surgery together with the suprascapular nerve block.8
Are there any recommendations for bilateral upper-limb blocks?It has always been believed that performing bilateral surgery in injured limbs simultaneously is not a good option, either from the surgical or anesthetic point of view.8 However, surgeons have recently chosen to take patients with bilateral trauma to a single-stage surgical solution. This poses a significant challenge for the anesthetist, in particular when the injury is to the upper limb, because the option of neuroaxial anesthesia, available for lower limb surgery, is not available for the upper limbs.8
At the present time, ultrasonography has become widely used as a tool for direct visualization of the anatomical structures and of the needle, leading to a lower rate of adverse effects caused by blind identification of the nerves and the administration of large volumes of local anesthetic with their potential toxicity.9 This means that ultrasonography is a good alternative for performing simultaneous peripheral blocks.
Considering that there is not just one approach for bilateral anesthesia in the upper limb, the only option open to the anesthetist for providing regional anesthesia or analgesia in a patient with bilateral upper limb injury is a bilateral brachial plexus block.10
If bilateral brachial plexus block is considered, it is of vital importance to bear in mind the main risks of this technique, including toxicity due to local anesthetics, phrenic nerve palsy, and pneumothorax.8
The development of toxicity due to local anesthetics is a multifactorial reaction influenced not only by individual characteristics beyond the control of the practitioner, but also by other factors that may be controlled, including the rate of administration and the mass (concentration) of the local anesthetic.11 When a nerve block is used as the single anesthetic strategy in bilateral procedures, the amount of local anesthetic required usually exceeds the toxicity limits, although this is something that happens often with no significant clinical effect.12 The option of supplementing regional anesthesia with profound intra-operative sedation in order not to surpass those limits ensures adequate post-operative analgesia, which is usually difficult to achieve in these surgical procedures.8 However, there are groups of anesthetists who prefer regional anesthesia and have managed, through the use of ultrasound, to reduce the effective amount of the drugs in order to achieve surgical blockade with a minimum amount of local anesthetic.8
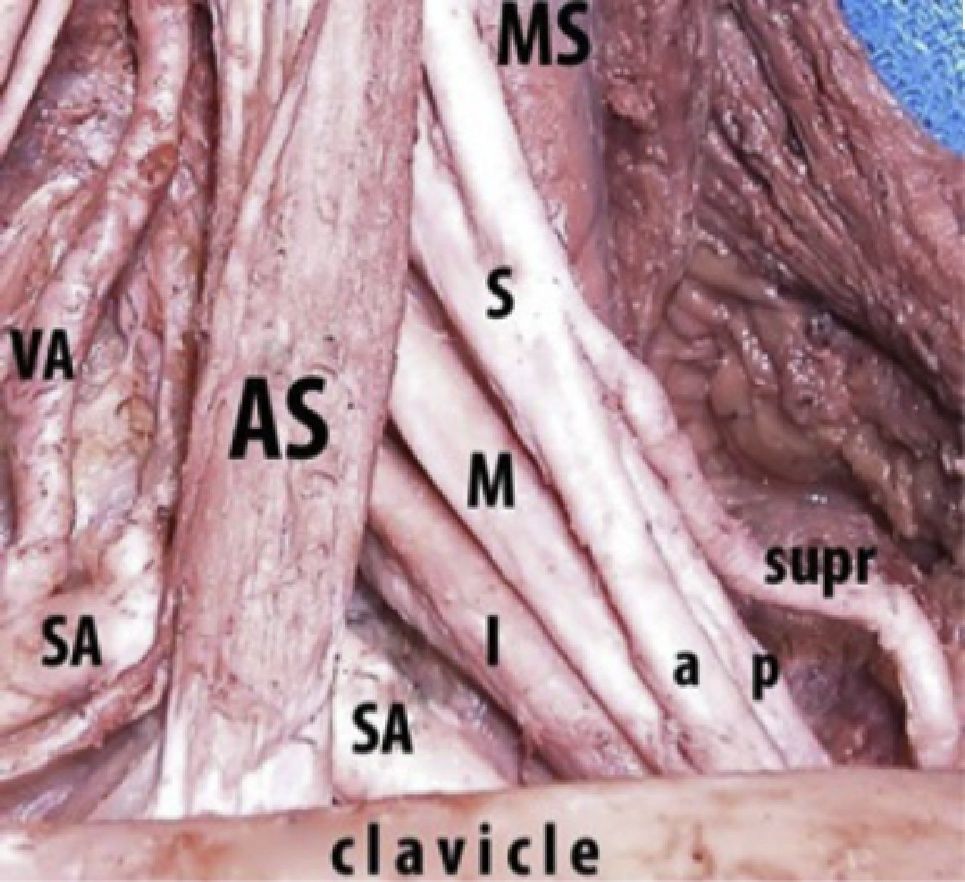
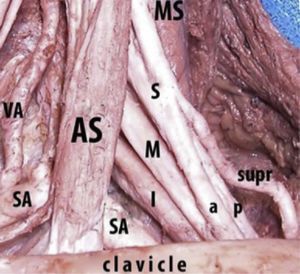
Phrenic nerve palsy is a very important consideration when administering bilateral brachial plexus blockade. When it happens, it may create a serious condition requiring mechanical ventilation because of bilateral diaphragmatic paralysis.13 In this regard, it is critical to consider the level of plexus block, because for the axillary and infraclavicular approaches, the presence of this adverse reaction is hardly inexistent, whereas with the interscalene block is it very high.14 However, axillary and infraclavicular blocks for shoulder and proximal humerus surgery are practically useless; and even though they are possible if low concentrations of the local anesthetic are used, they entail a huge risk. Bearing these considerations in mind, the only option left is to perform a supraclavicular block which, although not free of the risk of phrenic nerve palsy, may provide adequate post-operative analgesia in patients undergoing shoulder or proximal humerus surgery, as long as the local anesthetic is administered under ultrasound guidance to help identify the suprascapular nerve, which traverses at this level, lateral to the brachial plexus (see Fig. 5).15
In 1979, Knoblanche published a paper showing that the incidence of phrenic nerve palsy with the use of the supraclavicular block was 67%.16 However, it has been determined recently that this incidence is closer to 17%17 and that, with the use of ultrasound guidance, it may be reduced almost completely,18 which could be very useful should a bilateral supraclavicular block be needed.
The risk of pneumothorax when brachial plexus blockade is used varies depending on the site of approach, and is estimated to range between 0.3 and 6% for paresthesias in the case of the landmark-guided supraclavicular approach.19 The incidence of this complication in ultrasound-guided supraclavicular approaches is unknown and, to date, there are only case reports that are insufficient to arrive at a clear determination of this risk, although it is considered to be extremely low.8
Bilateral proximal brachial plexus blockade at the supraclavicular level may be an option for the analgesic management of patients with bilateral injuries of the shoulder and the proximal third of the humerus, considering that there are associated risks that could be diminished with the use of ultrasonography and the administration of lower amounts of local anesthetics.
And what about continuous blocks for bilateral upper limb surgery?Continuous administration of low-dose local anesthetics is very useful for controlling post-operative pain in upper limb surgery, but recommendations for bilateral administration are scarce. Although bilateral use of continuous 0.2% ropivacaine has been reported using the interscalene approach,14 the risk of phrenic nerve palsy and the catheter migration are important considerations, and the need for monitoring potential complications using special devices such as a spirometer or an ultrasound machine may limit its use during the perioperative period. The supraclavicular approach to the brachial plexus for the continuous administration of local anesthetics is an analgesic option for patients with shoulder and proximal arm injuries, but there are no references in the literature regarding its bilateral use.
ConclusionsUltrasound-guided bilateral supraclavicular brachial plexus blockade is an analgesic option in cases of surgery of the shoulder and proximal third of the arm, because it allows the use of low-dose local anesthetics, and entails a lower risk of phrenic nerve palsy compared to the interscalene approach. However, clinical monitoring has to be optimized to ensure early detection of signs of respiratory distress or breathing complications. A useful tool to diminish the risk of toxicity due to local anesthetics is to administer the anesthetic at different times on each side, thus reducing the plasma peak usually associated with adverse effects. Continuous brachial plexus block with local anesthetics at low concentrations may be used for post-operative analgesia in the most painful limb or the limb undergoing the bloodiest procedure, always supplemented with a multimodal strategy.
Funding sourceAuthors’ own resources.
Conflict of interestNone declared.
Please cite this article as: Vásquez MI, et al. Bloqueo supraclavicular bilateral con ecografía. Rev Colomb Anestesiol. 2012;40:304–8.