The Gerbode Defect is a rare form of intracardiac shunt from the left ventricle to the right atrium resulting from a defect in the membranous portion of the inter-ventricular septum. This defect can be congenital or acquired, with acquired causes including complications of aortic valve replacements and endocarditis. Intraoperative real time transesophageal echocardiography and 3D echocardiography are vital for diagnosis and anatomic characterization of the shunt. A thorough understanding of echocardiography is necessary to visualize the shunt across various anatomic planes which aids in surgical correction.
El Defecto de Gerbode es una rara manifestación de la comunicación interventricular del ventrículo derecho a la aurícula derecha, resultante de un defecto en la porción membranosa del tabique inter-ventricular. El defecto en cuestión puede ser congénito o adquirido y entre las causas adquiridas se encuentran complicaciones de los reemplazos de la válvula aórtica y la endocarditis. La ecocardiografía intraoperatoria en tiempo real y la ecocardiografía en 3D son vitales para el diagnóstico y la caracterización anatómica de la intercomunicación. Se hace necesario comprender a fondo la ecocardiografía para visualizar la intercomunicación a través de distintos planos anatómicos, lo cual ayuda a la corrección quirúrgica.
This is a 79-year-old man with history of hyperlipidemia, hypertension and smoking with diffuse 3 vessel coronary artery disease and moderate to severe aortic stenosis who underwent aortic valve replacement (AVR) with a #21 bovine bioprosthetic valve and three vessel coronary artery bypass grafts at an outside hospital (OSH). A year after this procedure the patient presented to an OSH with fluid retention and a new heart murmur. He was found to have prosthetic valve enterococci endocarditis which was subsequently treated with intravenous antibiotics. The patient continued to have complaints of fluid retention and worsening murmur and presented to our hospital for second opinion 8 months later. Physical exam revealed grade 3/6 end systolic murmur and 2/4 long diastolic murmur heard at the left sternal border. Transthoracic echocardiogram showed paravalvular leaks around the bioprosthetic aortic valve with moderate to severe aortic insufficiency (AI), a dilated left ventricle (LV) and additional blood flow originating at the level of the aortic valve communicating with the right atrium (RA). Preoperative CT angiography showed a dilated aortic root with patent bypass grafts.
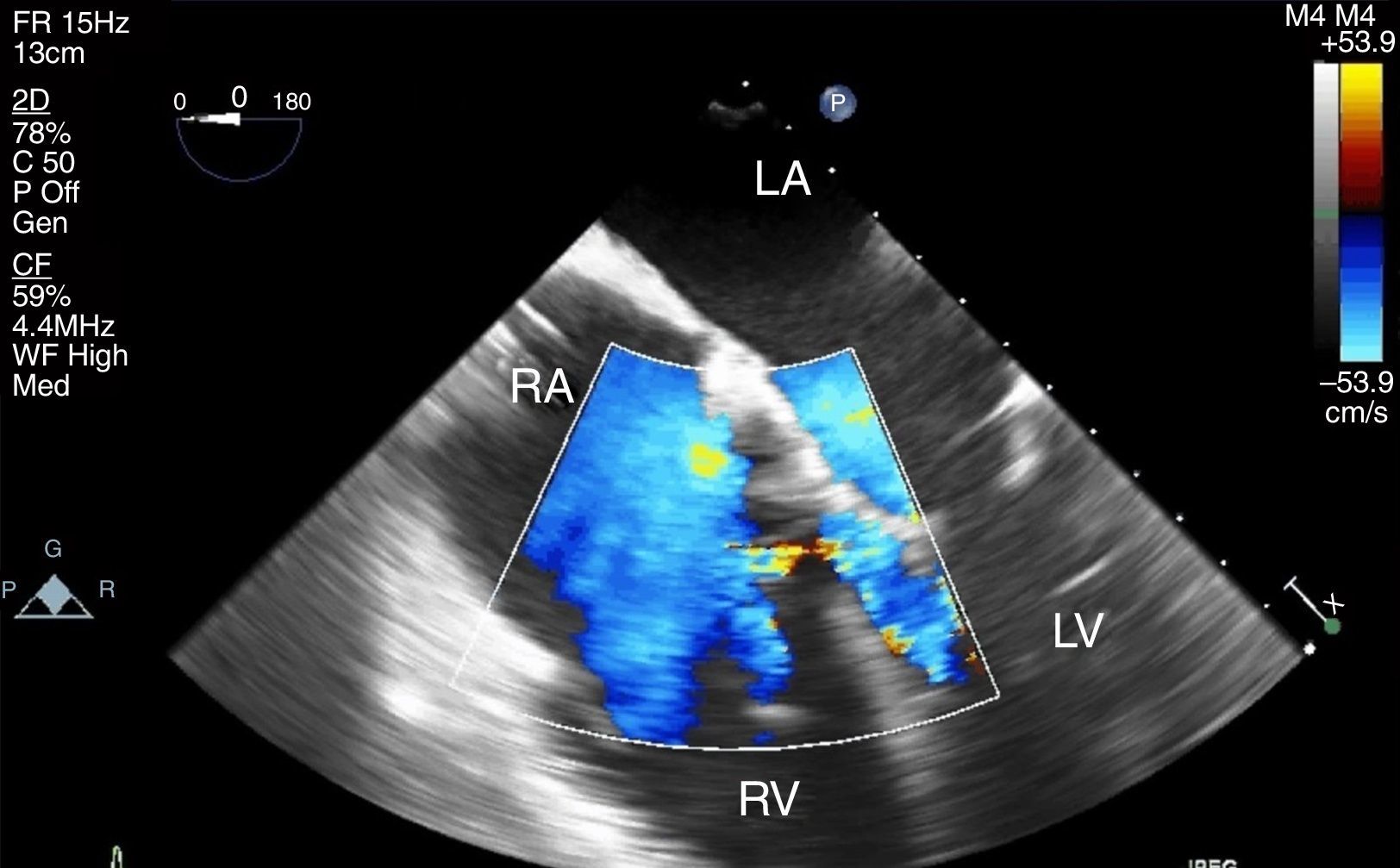
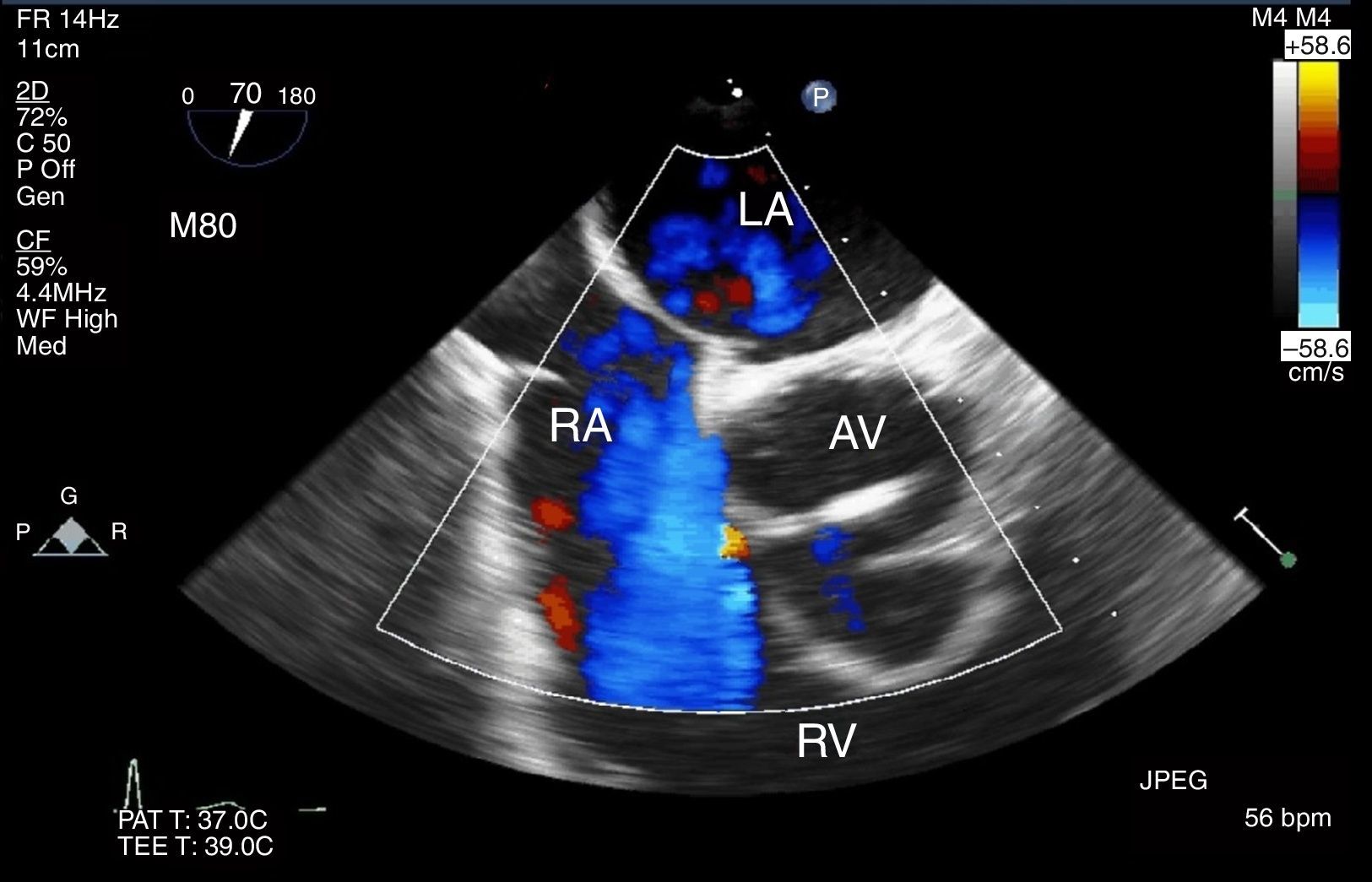
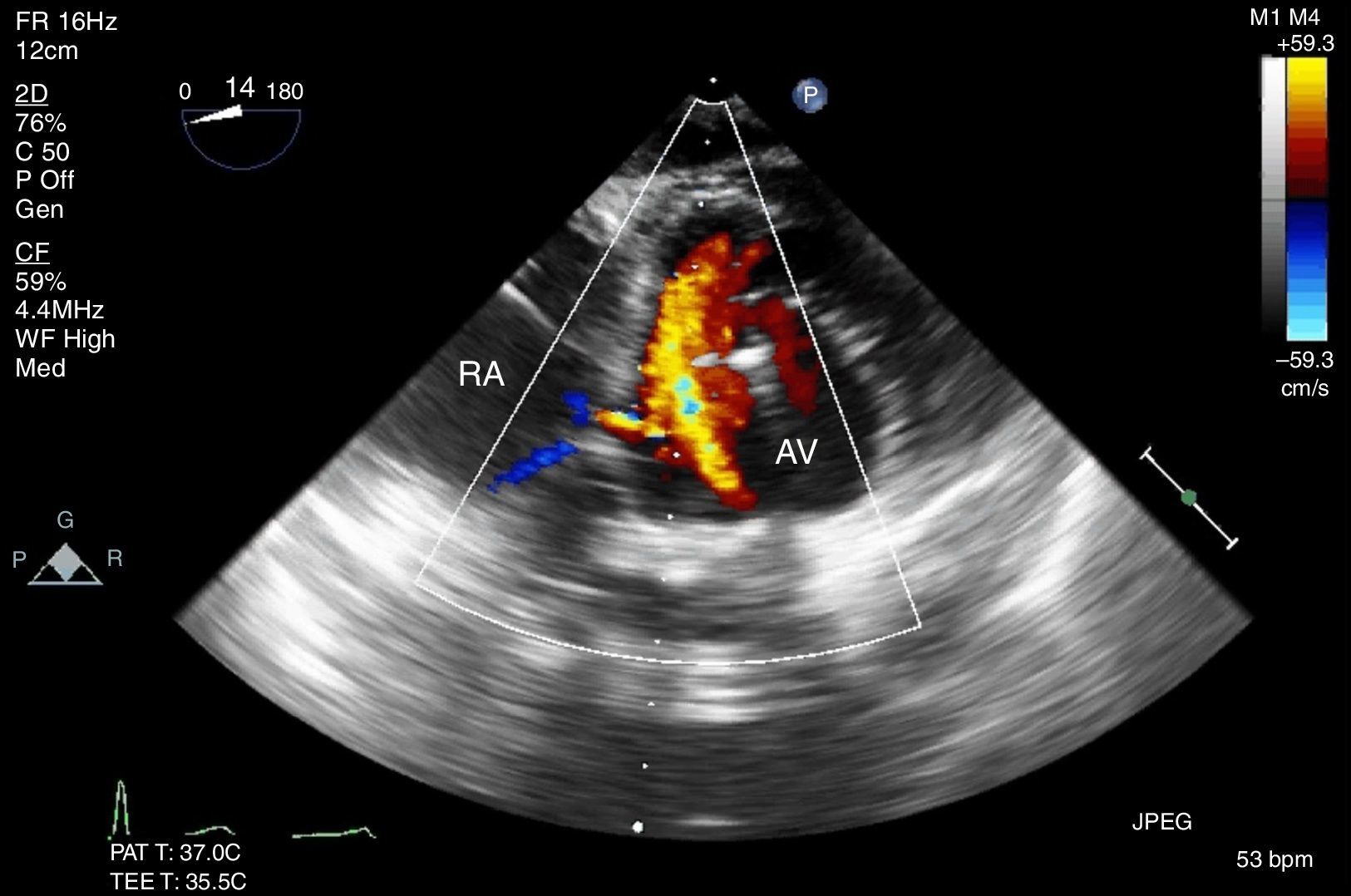
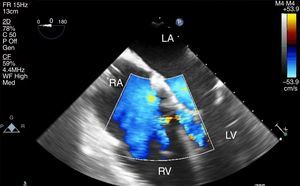
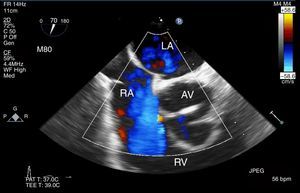
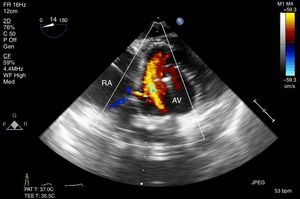
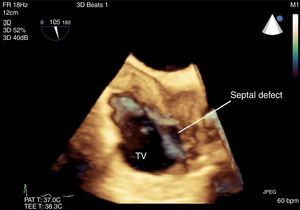
Due to the severity of the paravalvular leaks and AI, the patient was scheduled for redo AVR. Intraoperative pre-cardiopulmonary bypass transesophageal echocardiography (TEE) confirmed severe AI and dilated LV. Further interrogation confirmed blood flow between the LV and the RA, consistent with an acquired Gerbode-type ventricular septal defect (VSD), with flow present in both systole and diastole. No 2-D or color flow doppler (CFD) evidence of a communication between the aortic root and the RA was seen (Figs. 1–6).
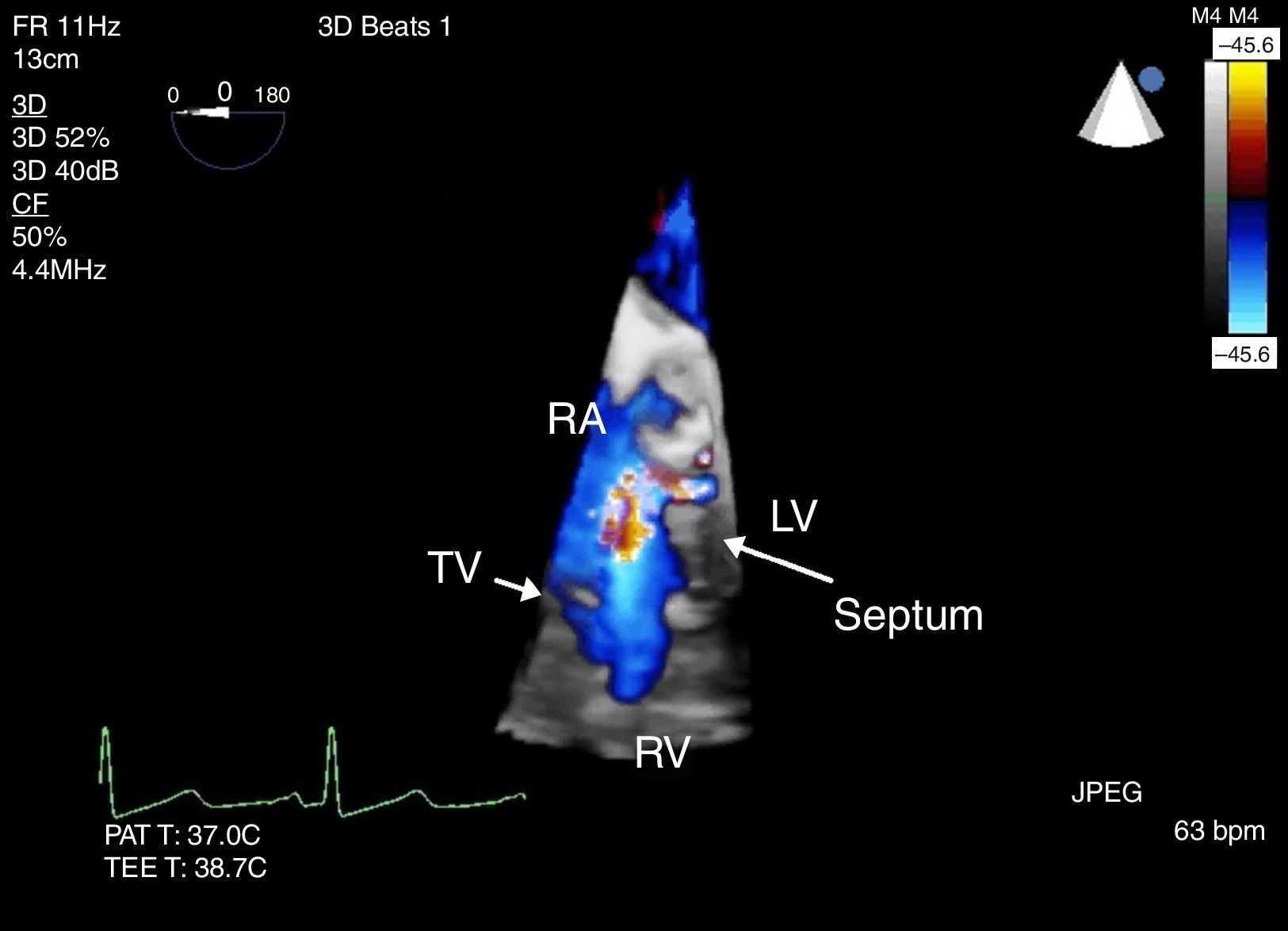
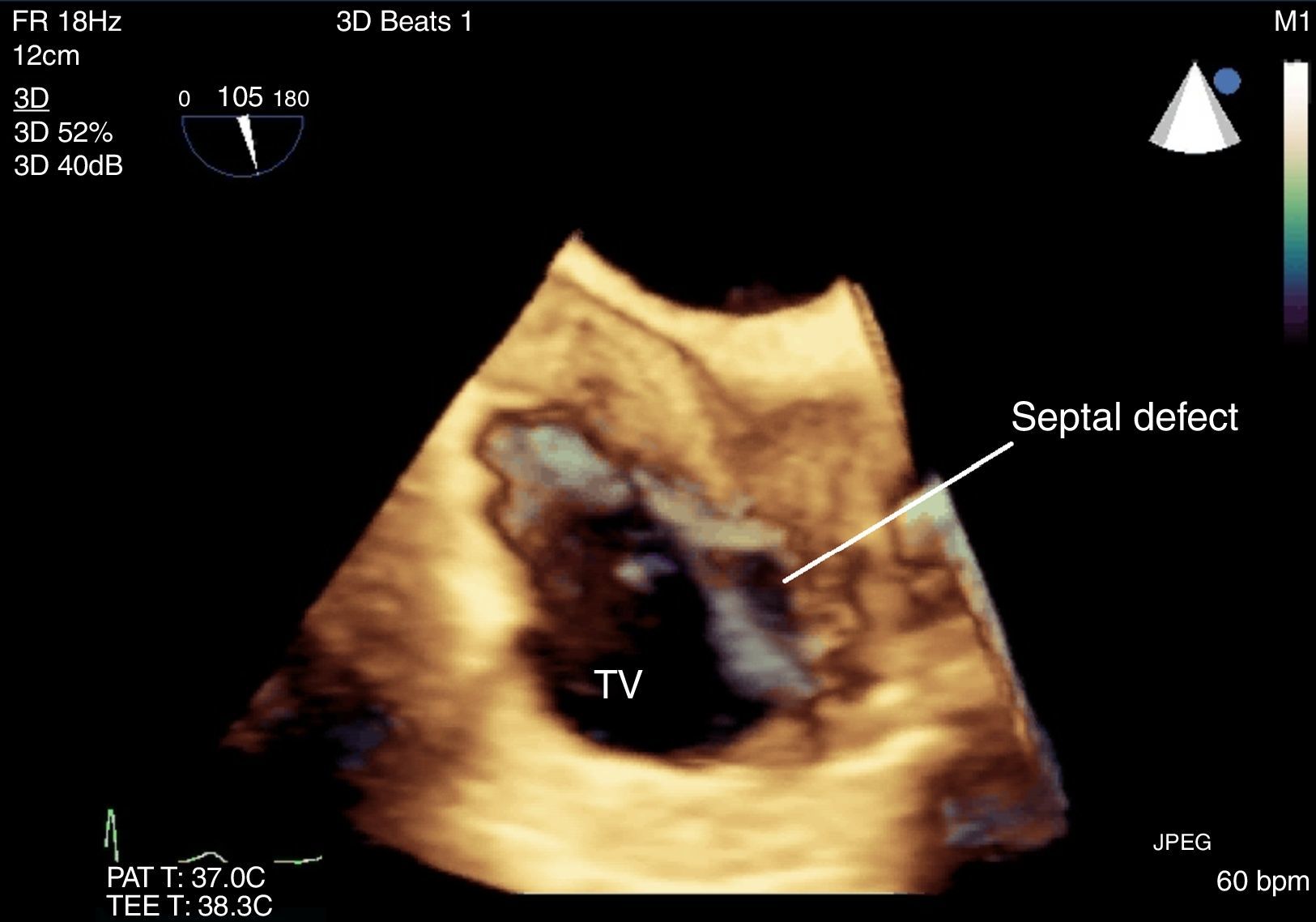
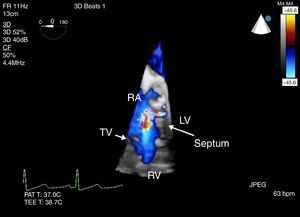
3-D CFD across the defect seen from Fig. 1, ME four chamber view. Flow is seen above the level of the tricuspid valve (TV) with a defect in the septum.
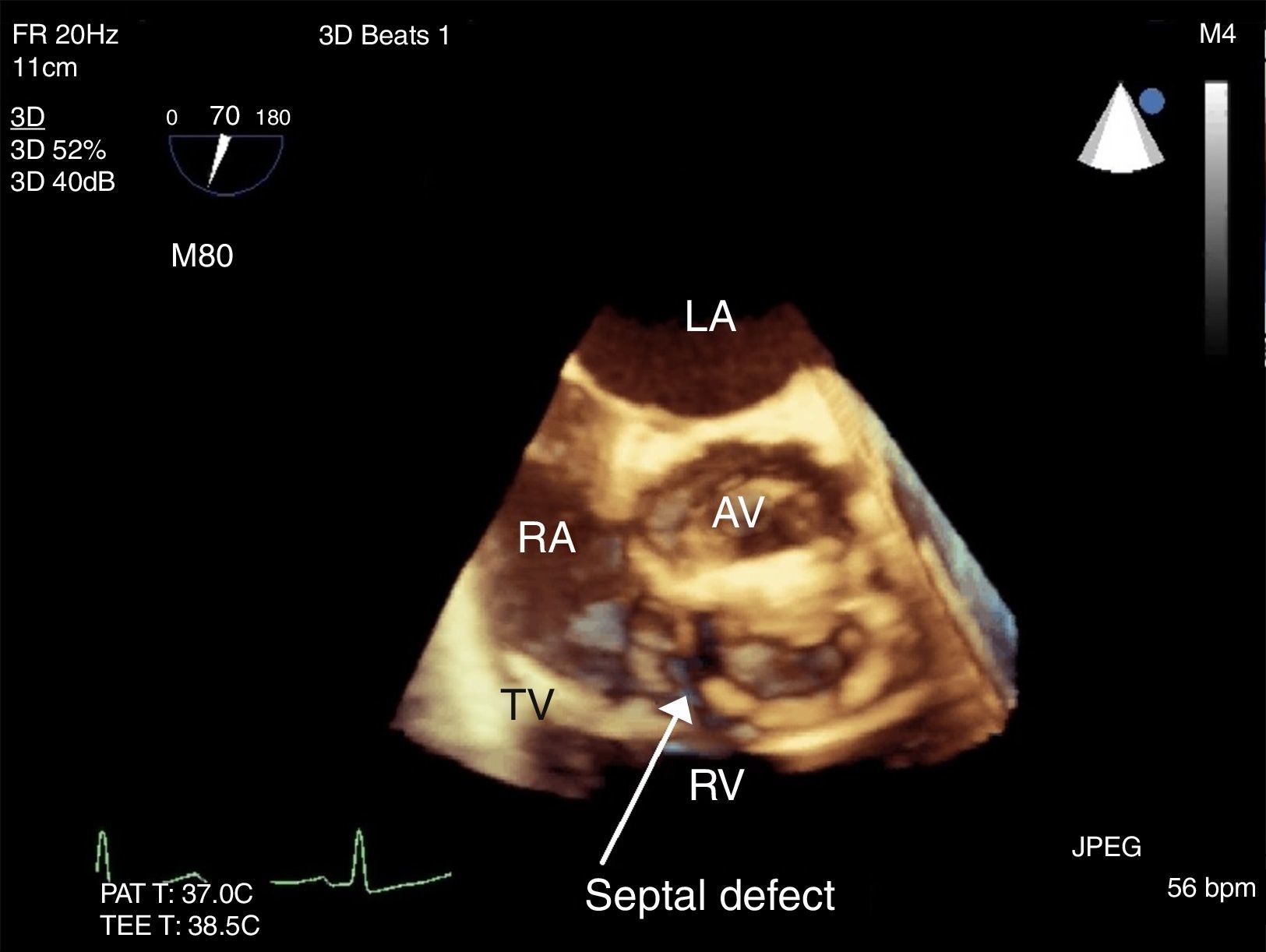
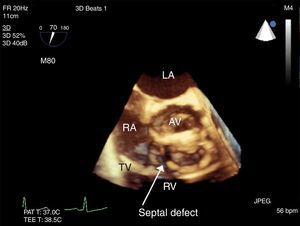
3-D image showing the septal defect above the tricuspid valve seen from Fig. 2, ME RV inflow-outflow tract view.
The patient underwent aortic root replacement with a 22mm homograft and patch repair of the Gerbode defect with PeriGuard® (Synovis, St. Paul, MN, USA). TEE post CPB showed no aortic insufficiency with a peak gradient of 10mmHg across the Homograft AV. No evidence of Gerbode defect was present. The patient was transferred from the ICU to the regular floor on post-operative day 4 and discharged home on post-op day 8.
DiscussionOur patient presented with stenosis and insufficiency of his bioprosthetic aortic valve with an acquired Gerbode-type VSD. Intraoperative TEE examination was thus tailored to focus on these pathologies before and after surgical repair.
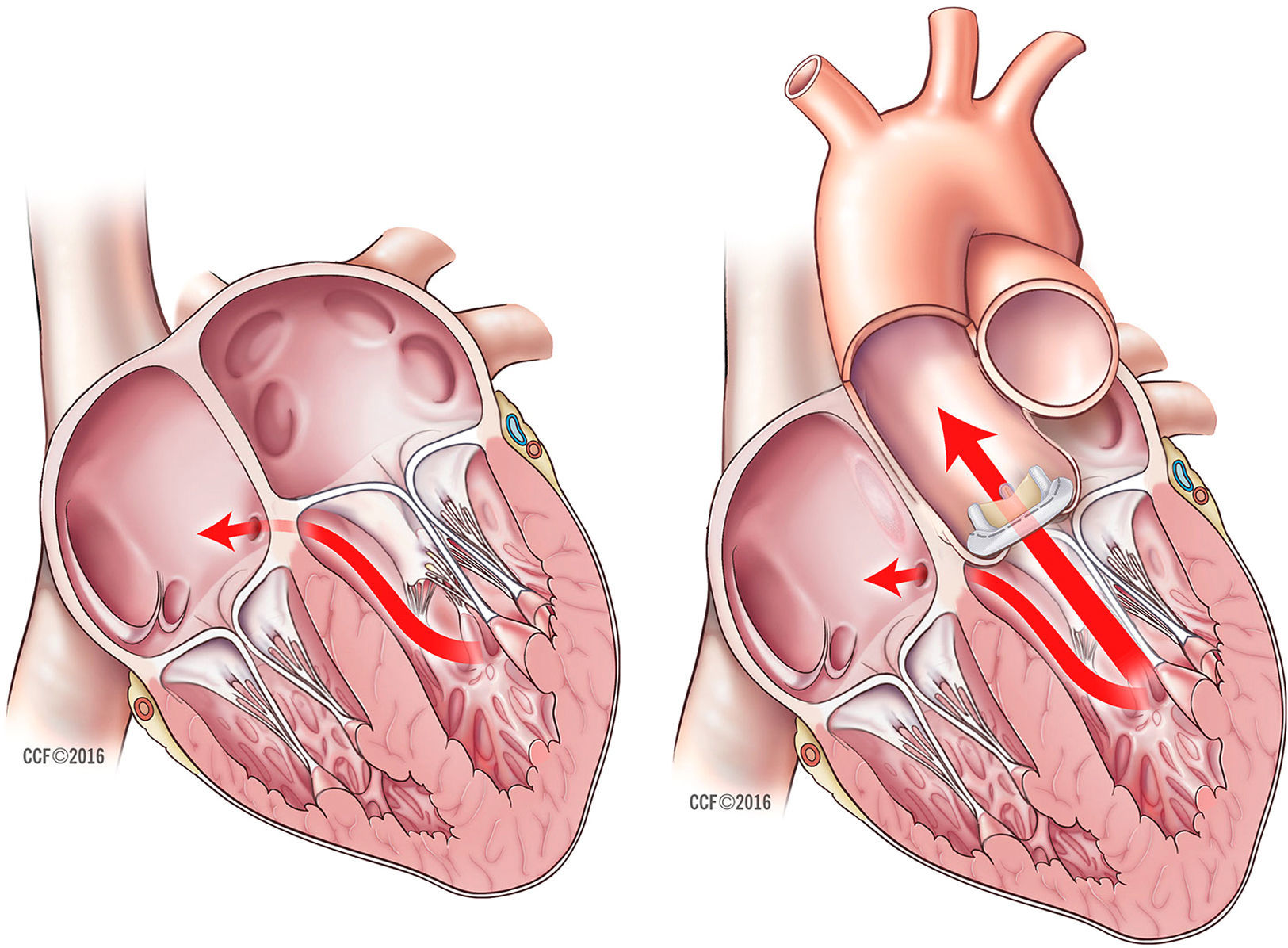
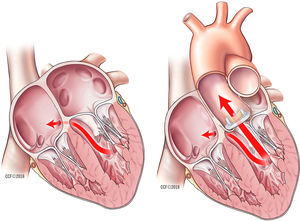
The Gerbode defect is a rare form of shunt from the LV to RA due to either congenital or acquired causes. The defect occurs in the membranous portion of the inter-ventricular septum above the level of the tricuspid valve (Fig. 7). The acquired causes include complications of invasive cardiac procedures like aortic valve replacements, endocarditis, trauma or myocardial infarction. The pathogenesis of an intra-cardiac fistula with endocarditis is due to translocation of the infection from the valve to adjacent myocardium.1–3 Real-time TEE is the mainstay for diagnosis and 3-D echocardiography can provide anatomic characterization of the shunt. The TEE views that show the Gerbode defect best are those that can examine the interventricular septum, particularly the membranous septum. These include the mid-esophageal four-chamber view, right ventricular inflow-outflow tract view, trans-gastric short axis and deep trans-gastric views. 3-D echocardiography can help distinguish a Gerbode defect from sinus of Valsalva rupture, ventricular septal defects and tricuspid regurgitation.4
Our patient likely developed the Gerbode defect secondary to the surgical intervention he had to replace his aortic valve and/or the enterococci endocarditis. The Gerbode defect was best seen in the mid-esophageal four chamber view, the right ventricular inflow-outflow tract view and deep trans-gastric view (Figs. 1–6). Flow was seen through the defect during both systole and diastole excluding the possibility of tricuspid regurgitation artifact. CFD and 3-D echocardiography were used for anatomic characterization of the defect.
Surgical repair of Gerbode defects had previously been the sole treatment option for patients with symptomatic shunts but over the last two decades percutaneous closure has been increasingly performed.4 With percutaneous intervention, 3-D TEE has developed into a tool to not only diagnose Gerbode defects but also plays a vital role in percutaneous device sizing and monitoring device deployment. Percutaneous repair was not indicated in our patient as open heart surgery was required to replace the aortic valve. Surgical approach is still the preferred treatment in the repair of a lesion caused by infective endocarditis.4 Intraoperative TEE was essential to identify and characterize the defect which helped localize the defect and confirm the repair.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that the procedures followed were in accordance with the regulations of the relevant clinical research ethics committee and with those of the Code of Ethics of the World Medical Association (Declaration of Helsinki).
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document
FundingInstitutional Funding provided by the Department of Cardiothoracic Anesthesiology, Anesthesiology Institute, Cleveland Clinic.
Conflicts of interestNo conflicts of interest to disclose.
Please cite this article as: Bustamante S, Cheruku S. Ecocardiografía transesofágica intraoperatoria para evaluar el defecto tipo Gerbode. Rev Colomb Anestesiol. 2017;45:147–150.