Pain management is part of the comprehensive approach to all patients and results in clear benefits. As such, obstetric analgesia seeks to reduce pain and provide better care during labour. However, its use is sometimes limited due to lack of access to, or availability of, anaesthesia services. Alternative techniques to the epidural analgesic approach are found in the literature, for use by general practitioners or healthcare staff in lower complexity settings. This article discusses general aspects of epidural obstetric analgesia, and other pharmacological and non-pharmacological management options.
El manejo del dolor hace parte del abordaje integral de todos los pacientes y muestra claros beneficios. En este sentido, la analgesia obstétrica busca disminuir el dolor y brindar una mejor atención durante el trabajo de parto. A pesar de ello, su uso se ve limitado en ocasiones por falta de acceso o disponibilidad del servicio de anestesiología. En base a esto, en la literatura se encuentran técnicas alternativas al abordaje peridural para manejo analgesico, las cuales pueden ser empleadas por medicos generales o personal de salud de menor nivel de complejidad. Este artículo abordará aspectos generales sobre la analgesia obstétrica epidural, y otras opciones de manejo farmacológicas y no farmacológicas.
At the present time, obstetric analgesia in the context of the Colombian health system is covered by the Mandatory Health Plan.1 However, this intervention is not always used routinely, and its use is estimated to be higher in developed countries as compared to developing countries. In our setting, most of these procedures are performed in patients enrolled in pre-paid or private medicine plans, partly due to the inequity of the system and the ability to gain access to the procedure.2 Notwithstanding, all obstetric patients must be the subject of comprehensive care, and pain management must be an important component of the approach to these patients, given that studies have found that the absence of analgesia during labour is associated with a higher risk of postpartum depression and post-traumatic stress. Moreover, pain is considered as an unnecessary source of distress.3 This article presents the results of a review of this topic, as well as useful management alternatives.
MethodThe literature was reviewed, including several primary and secondary data sources covering the past 6 years (2009–2005) found in databases such as PubMed, Cochrane, and in anaesthesia and health publications listed in the References. The articles for analysis were selected from those bibliographic sources and they are presented from the authors’ point of view.
Topic developmentObstetric analgesia is used with the aim of alleviating pain during labour. At the present time, one of the most widely used techniques is peridural analgesia, based on the use of drug infusion into this virtual space to create sensory blockade. This pain is now known to originate as a result of uterine contraction and cervical dilatation stimuli that travel up the spinal cord (T10-L1). This process triggers an adaptive hormonal response and rising cortisol and catecholamine levels.4
Epidural obstetric analgesia has not shown to have an impact on the rate of caesarean sections or neonatal Apgar scores. However, it has been associated with an increase in instrumented delivery when given during the expulsive phase; hence the need to perform it early on (during the latency and active phases).5 For the technique, the patient is placed in lateral decubitus, the intervertebral space (L3-L4) is palpated, the peridural space is localised (loss of resistance or use of saline solution), and, finally, a No. 18–16 infusion catheter is introduced. It was shown in one study that there is no significant difference in terms of the type of method used for localising the peridural space when the anaesthetist is trained in both techniques.6
This type of analgesia is considered as the best management tool. However, despite good effectiveness and safety, it does entail complications, including neurological abnormalities during the peripartum period: lateralised analgesia (16.4%), vessel puncture (8.7%), paresthesias (8.2%), difficult technique (5.2%), ineffective analgesia (2.7%), and arterial hypotension (2.5%). In the postpartum period, complications include lumbar pain (18.5%), urinary retention (3.4%), post dural puncture headache (1.4%), and peripheral neuropathy (0.9%).7
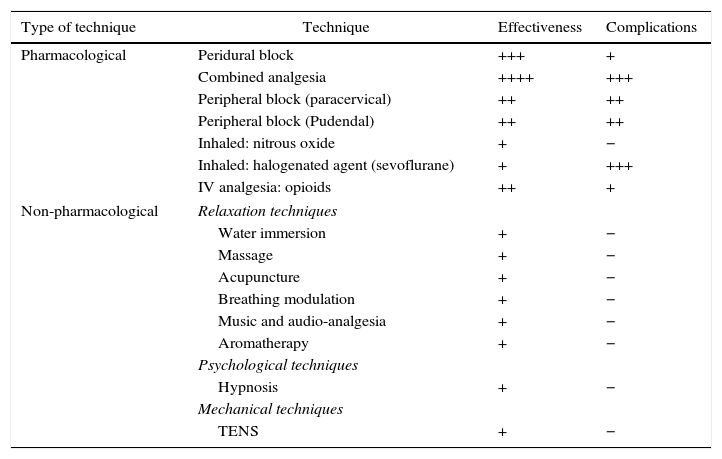
Additionally, mention is made in the literature of both pharmacological and non-pharmacological alternatives to peridural analgesia (see Table 1). These vary in effectiveness and are used in case of failure or unavailability of the procedure.8
Management of obstetric analgesia: alternative techniques.
| Type of technique | Technique | Effectiveness | Complications |
|---|---|---|---|
| Pharmacological | Peridural block | +++ | + |
| Combined analgesia | ++++ | +++ | |
| Peripheral block (paracervical) | ++ | ++ | |
| Peripheral block (Pudendal) | ++ | ++ | |
| Inhaled: nitrous oxide | + | − | |
| Inhaled: halogenated agent (sevoflurane) | + | +++ | |
| IV analgesia: opioids | ++ | + | |
| Non-pharmacological | Relaxation techniques | ||
| Water immersion | + | − | |
| Massage | + | − | |
| Acupuncture | + | − | |
| Breathing modulation | + | − | |
| Music and audio-analgesia | + | − | |
| Aromatherapy | + | − | |
| Psychological techniques | |||
| Hypnosis | + | − | |
| Mechanical techniques | |||
| TENS | + | − | |
Source: Authors.
Pharmacological therapies include combined analgesia consisting of the administration of a dose of anaesthetic to the subarachnoid space using a single puncture in addition to peridural analgesia. This technique is useful in cases of severe pain but it is associated with a higher rate of adverse reactions.9 Other therapies include bilateral paracervical block and pudendal block, which provide rapid onset analgesia (2–5min); although useful, they require training and are risky in cases of placental insufficiency or prematurity.10
Inhaled agents are another option, among them nitrous oxide. This agent is of short latency, rapid excretion and does not give rise to neonatal depression, but its analgesic effectiveness is controversial. On the other hand, halogenated agents like sevoflurane can also be used. However, they are used infrequently because they require monitoring and training, and may induce uterine relaxation, and neurological/respiratory depression.11 For intravenous analgesia, the agents of choice are opioids. They act centrally and their main advantage is that they do not require the constant presence of the anaesthetist. They are moderately effective and high doses have been associated with vomiting, nausea, itching, maternal sedation and foetal respiratory depression.12
On the other hand, there are non-pharmacological therapies, which may be combined in order to increase their analgesic effect. These types of therapies are associated with a low incidence of complications and they can be used by the healthcare staff in cases where neuroaxial analgesia is not available.13 They are classified into three groups: relaxation, psychological and mechanical techniques.
Relaxation techniques include warm water immersion, acupressure (Shiatsu), massage, breathing modulation, music (audio-analgesia) and aromatherapy. They help tolerate pain rather than eliminate it, and they require ante-natal training.14,15 Hypnosis, a psychological technique, has been shown to significantly reduce the use of analgesics and the risk of postpartum depression. It is of limited usefulness in patients with a history of psychosis or psychiatric disorders.16
Mechanical techniques include transcutaneous electrical nerve stimulation (TENS), in which a pair of electrodes are placed in the paravertebral region, one at T10-L1, and the other at S2-S4. It has been shown to improve pain severity and its use is recommended from the initial stages of labour given that it stimulates endorphin release.17 These techniques may be useful in clinical practice, and research into their use in multimodal management of obstetric patients should be encouraged.
ConclusionThe review showed that the most effective therapies are the ones that involve some form of neural blockade. However, they require the constant presence of an anaesthetist, something which is not critically important in the case of pharmacological therapies based on the use of opioids, or for non-pharmacological approaches that may be performed by other healthcare staff and general practitioners. Although some of these techniques require antepartum training, they may be a very useful option as part of management in low-complexity hospitals.
Along these lines, every hospital and clinic in our setting should use the best therapeutic option available to them for managing pain. The benefits are clear as was discussed previously, considering that pain is not justifiable from the ethical point of view and, consequently, it requires a timely comprehensive approach to the maternal population whenever possible. We recommend that heads of obstetric services should implement obstetric analgesia protocols as part of the care provided to patients in labour.
FundingNone.
Conflict of interestThe authors declare having no conflict of interest.
Please cite this article as: Gomezese OF, Ribero BE. Analgesia obstetrica: Situación actual y alternativas. Rev Colomb Anestesiol. 2017;45:132–135.