Postoperative residual curarization has been related to postoperative complications.
ObjectiveTo determine the prevalence of postoperative residual curarization in a university hospital and its association with perioperative conditions.
MethodA prospective registry of 102 patients in a period of 4 months was designed to include ASA I–II patients who intraoperatively received nondepolarizing neuromuscular blockers. Abductor pollicis response to a train-of-four stimuli based on accelleromyography and thenar eminence temperature (TOF-Watch SX®. Organon, Ireland) was measured immediately upon arrival at the postanesthetic care unit and 30s later. Uni-bivariate analysis was planned to determine possible associations with residual curarization, defined as two repeated values of T4/T1 ratio <0.90 in response to train-of-four stimuli.
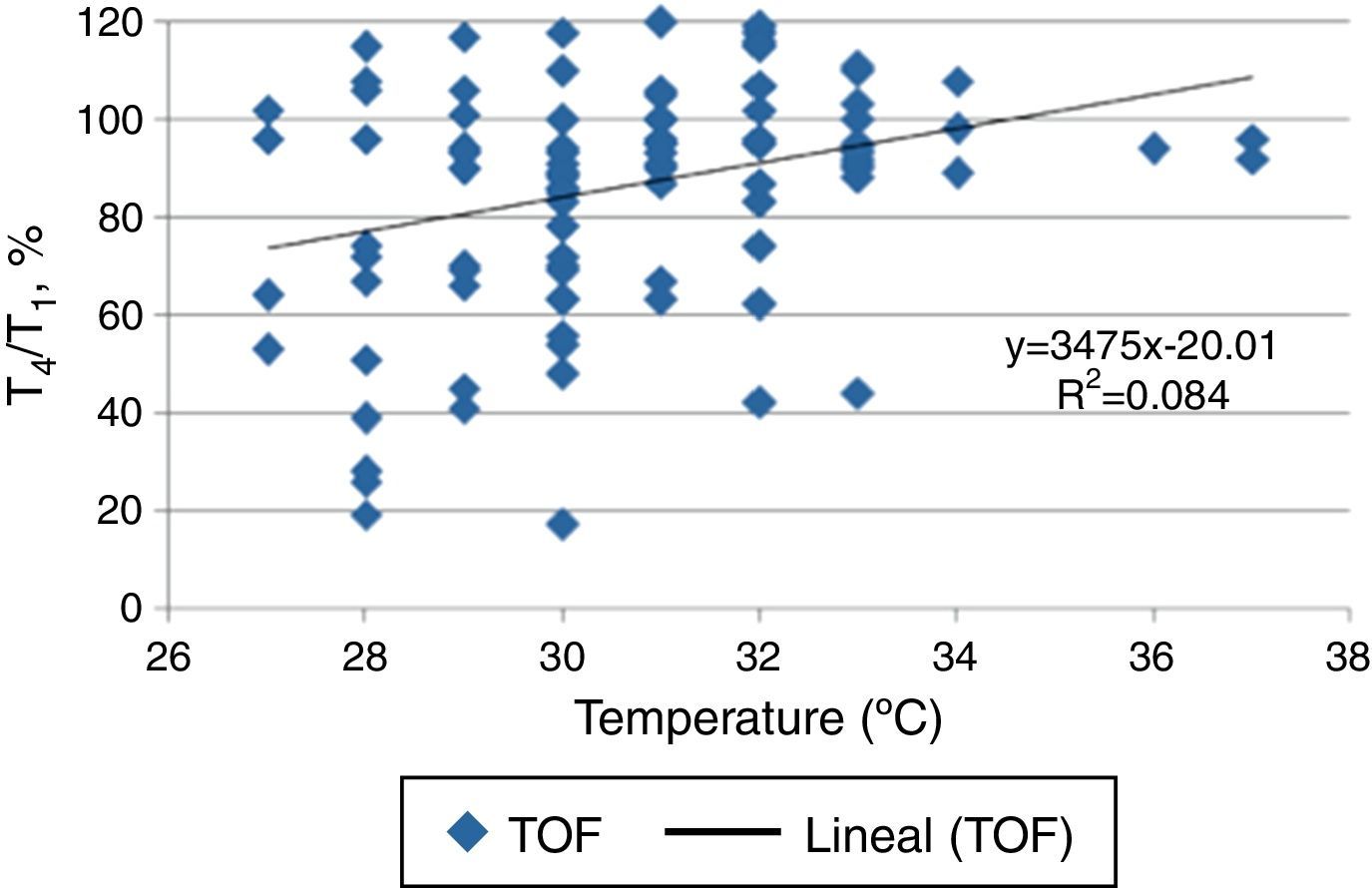
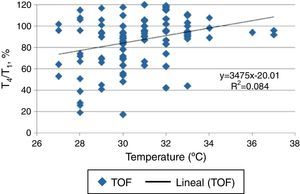
ResultsPostoperative residual curarization was detected in 42.2% of the subjects. Pancuronium was associated with a high risk for train-of-four response <0.9 at the arrive at postoperative care unit [RR:2.56 (IC95% 1.99–3.30); p=0.034]. A significant difference in thenar temperature (°C) was found in subjects with train-of-four <0.9 when compared to those who reach adequate neuromuscular function (29.9±1.6 vs. 31.1±2.2; respectively. p=0.003). However, we were unable to demonstrate a direct attribution of findings in train-of-four response to temperature (R2 determination coefficient=0.08%).
ConclusionsA high prevalence of postoperative residual curarization persists in university hospitals, despite a reduced use of “long-lasting” neuromuscular blockers. Strategies to assure neuromuscular monitoring practice and access to therapeutic alternatives in this setting must be considered. Intraoperative neuromuscular blockers using algorithms and continued education in this field must be priorities within anesthesia services.
La relajación residual postoperatoria ha sido asociada con mayores complicaciones postoperatorias.
Objetivodeterminar la prevalencia de relajación residual postoperatoria en un hospital universitario y su relación con condiciones perioperatorias.
MétodosSe diseñó un registro prospectivo de 4 meses de duración, que incluyó pacientes ASA I-II que intraoperatoriamente recibieran bloqueadores neuromusculares. Se registró la respuesta del abductor pollicis a un estímulo de tren de cuatro mediante aceleromiografía y se midió la temperatura de la eminencia tenar (TOF-Watch SX®.Organon, Ireland) inmediatamente al ingreso a recuperación y a los 30 segundos. Se realizó análisis uni y bivariado para determinar posibles asociaciones con relajación residual postoperatoria, definida como dos respuestas sucesivas al estímulo tren-de-cuatro con una relación T4/T1 <0.90.
ResultadosSe reclutaron 102 pacientes, encontrando una prevalencia de relajación residual del 42.2%. Pancuronio fue asociado con un riesgo elevado de TOF<0.9 al ingreso a recuperación [RR:2,56 (IC95% 1.99-3.30); p=0.034]. Se evidenció una diferencia significativa en la temperatura tenar de los pacientes que presentaban relajación residual, al compararla con pacientes que recuperaron su función neuromuscular [Grupo evento=29.9±1.6 (n=43); Grupo control=31.1±2.2 (n=59)]. Sin embargo no se logró determinar una atribución directa de relajación residual a esta medición (coeficiente de determinación=0.08%)
ConclusiónPersiste una alta prevalencia de relajación residual postoperatoria en los hospitales universitarios, a pesar del uso reducido de bloqueadores neuromusculares de larga duración. Se hace indispensable encaminar estrategias para incentivar la monitoria neuromuscular y establecer algoritmos que permitan un manejo eficiente de los bloqueadores neuromusculares.
Nondepolarizing neuromuscular blocking agents (ND-NMBA) have commonly used in surgical units to facilitate endotracheal intubation and during procedures under general anesthesia to provide adequate surgical conditions or optimize ventilatory support. Postoperative residual curarization (PORC), defined as the presence of T4/T1 ratio <0.9 ratio in response to the “train-of-four” (TOF) stimulation,1–3 has been subject of multiple publications over the past three decades with a incidence reported up to 40%, even when the cut-off of TOF ratio to define PORC was as low as <0.7.4–9
The value of TOF ratio<0.9, to define PORC, was recommended after papers wich reported that, below this cutoff, functional recovery of the laryngeal muscles and upper esophagus were not complete, even if the patient were holding ventilation in normal limits and overcoming clinical tests.3,10 Subsequent reports showed that rates of TOF<0.9 were associated with longer lenght of stay in the Post Anesthesia Care Unit (PACU).11,12 This adverse event is still being present today, even with the use of intermediate acting ND-NMBA or use of drugs such as neostigmine for reversing neuromuscular block.7,13–15 In Latin America there is a poor clinical applicability of neuromuscular relaxation monitoring (NMRM) as well as in the rest of the world.16
This study aimed to assess the prevalence of PORC on admission to the PACU of patients treated at a university hospital as our primary objective, and to determine possible associations with demographic aspects and perioperative variables.
Materials and methodsPrior institutional ethics approval, a prospective observational registry of patients ASA I and II >18 years undergoing elective or emergency surgery under general anesthesia (in whom the use of ND-NMBA be envisaged) was designed. The size of the representative sample of the surgical population was defined and data were collected continuously during business hours during the time in which the expected number of patients was completed. All patients were invited to participate and gave their consent at admission to the surgical unit. Subjects with previous diagnosis of neurological or neuromuscular disease, those who were transferred to other places different to PACU or who requiring postoperative mechanical ventilation, were excluded.
At the end of surgery, an independent observer registered information on demographics, type of procedure and perioperative time, ND-NMBA used (type, total dose and method of administration), use of neostigmine (dose), use or not of NMRM and the result of TOF tests performed on admission to PACU.
A second-year resident of Anesthesiology or technical assistant previously trained and blinded to perioperative management were responsible to perform NMRM immediately for admission to PACU and 30s later. TOF-Watch SX® (Organon, Ireland) acceleromyographic monitor was used, in order to evaluate the response of the adductor pollicis muscle. After cleaning the site, an electrode (distal) was positioned at the point where the proximal flexor line of the wrist crosses the radial side of the flexor carpi ulnaris; the proximal electrode was placed 3–4cm away from the first one, on the ulnar nerve area. Simultaneously, surface temperature was determined by a sensor placed on the thenar eminence. The TOF test was applied by four stimuli of 0.2milliseconds (ms) duration at 2Hz and at 30mA.17,18 After 30s the test was repeated and registered; if incongruities were detected, a third test, was performed after 60s.
PORC was defined as the presence of a T4/T1 ratio<0.90 ratio in response to the TOF test.3,10 Procedure was validated based on the evaluation of the interrate reliability (20% of the sample). In regards to the test and results, the anesthesiologist remained blinded to control the treatment bias.
Statistic analysisSample size was calculated based on a reported incidence of PORC around 35% to detect a confidence level of 95% and a power of 80%. An estimate of 95 subjects were decided to include after adjusting for possible losses by 15%. The prevalence of the outcome of interest was calculated as follows: number of patients with PORC on the number of patients ASA I and II, who undergoing emergency or elective surgery, requiring NMBA in the established period (4 months). Processing and data analysis was performed using SPSS 20.0 (SPSS Statistics for Windows, version 20.0. Armonk, NY). Categorical variables are described as proportions and percentage distributions while numerical variables as means and standard deviations (SD). Differences among groups were evaluated based on analysis of variance of one way. Significance level α<0.05 was set a priori. Concordance analysis was performed with the MedCalc® (Mariakerke, Belgium, http://www.medcalc.be) software.
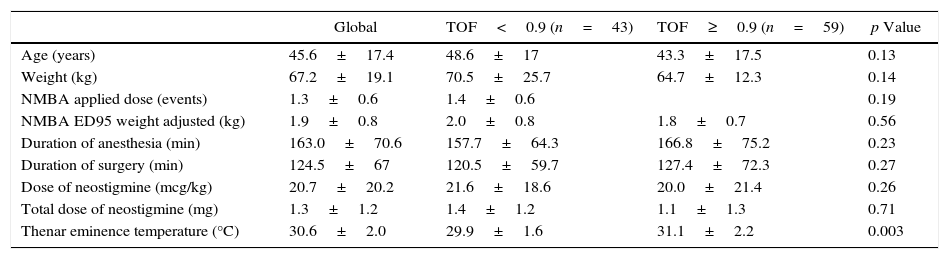
ResultsA total of 102 subjects accepted to participate in this study. Procedures included: general surgery (33.3%), head and neck (16.7%), gynecology (14.7%), orthopedics (12.7%) and other (13.7%). Only the temperature (°C), recorded in the thenar eminence on arrival in PACU, was significantly lower in patients with TOF<0.90 (29.9±1.6 vs. 31.1±2.2; p=0.003). Other demographic characteristics related to surgery showed no differences between groups (Table 1).
Demographics of subjects recruited according to the response to two TOF stimuli upon arrival in recovery.
| Global | TOF<0.9 (n=43) | TOF≥0.9 (n=59) | p Value | |
|---|---|---|---|---|
| Age (years) | 45.6±17.4 | 48.6±17 | 43.3±17.5 | 0.13 |
| Weight (kg) | 67.2±19.1 | 70.5±25.7 | 64.7±12.3 | 0.14 |
| NMBA applied dose (events) | 1.3±0.6 | 1.4±0.6 | 0.19 | |
| NMBA ED95 weight adjusted (kg) | 1.9±0.8 | 2.0±0.8 | 1.8±0.7 | 0.56 |
| Duration of anesthesia (min) | 163.0±70.6 | 157.7±64.3 | 166.8±75.2 | 0.23 |
| Duration of surgery (min) | 124.5±67 | 120.5±59.7 | 127.4±72.3 | 0.27 |
| Dose of neostigmine (mcg/kg) | 20.7±20.2 | 21.6±18.6 | 20.0±21.4 | 0.26 |
| Total dose of neostigmine (mg) | 1.3±1.2 | 1.4±1.2 | 1.1±1.3 | 0.71 |
| Thenar eminence temperature (°C) | 30.6±2.0 | 29.9±1.6 | 31.1±2.2 | 0.003 |
Data expressed as mean±ED.
Source: Authors.
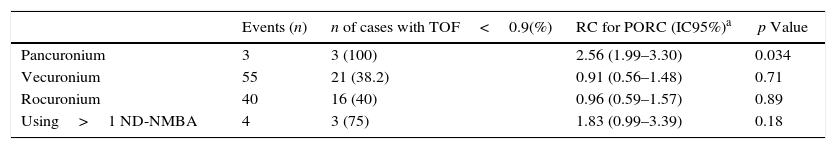
Vecuronium (53.9%), rocuronium (39.2%) and pancuronium (3%) were the ND-NMBA used in this sample. At the end of procedure none of the subjects received cyclodextrins or ND-NMBA (benzylisoquinolinics) while the use of more than one ND-NMBA was observed in 4 of the cases. When exploring for a possible causality between PORC and type of ND-NMB used, it was found that the use of pancuronium was significantly associated with this outcome: [RR 2.56 (95% CI 1.99–3.30); p=0.034]. Additionally, a non-significant trend to increased cases of PORC was found when combinations of these drugs (Table 2) were presented.
Neuromuscular blockers used and their relation to PORC in the sample studied.
| Events (n) | n of cases with TOF<0.9(%) | RC for PORC (IC95%)a | p Value | |
|---|---|---|---|---|
| Pancuronium | 3 | 3 (100) | 2.56 (1.99–3.30) | 0.034 |
| Vecuronium | 55 | 21 (38.2) | 0.91 (0.56–1.48) | 0.71 |
| Rocuronium | 40 | 16 (40) | 0.96 (0.59–1.57) | 0.89 |
| Using>1 ND-NMBA | 4 | 3 (75) | 1.83 (0.99–3.39) | 0.18 |
ND-NMBA, nondepolarizing-neuromuscular blocking agent.
The reversal of neuromuscular blockade was performed in 57% of patients and in all cases neostigmine was used at doses between 20 and 25mcg/kg. No significant differences were found when analyzed whether its application was associated with decreased incidence of TOF<0.90 on arrival in PACU. Similarly no relationship between the use of NMRM and a significant decrease of PORC was found.
To clarify the influence of the temperature measured in the thenar eminence on the TOF test results, we performed a concordance analysis. Coefficient of determination (R2) showed a value of 0.08%, indicating that the results obtained in the TOF test could not attributed at least completely by this factor (Fig. 1).
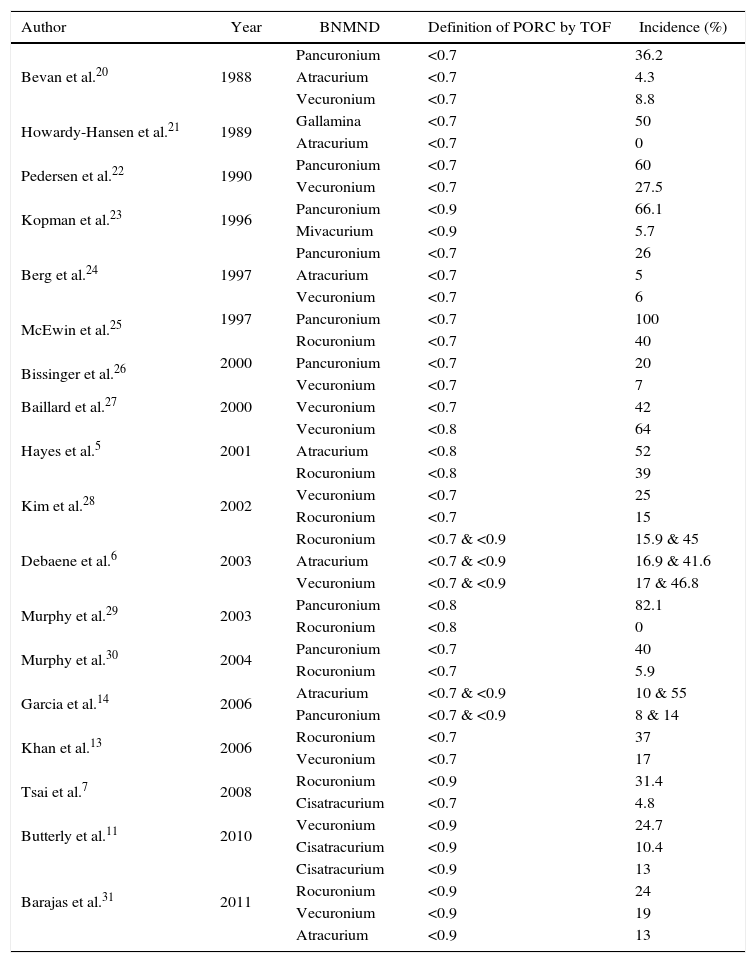
DiscussionPORC incidence reported in our study was 42.2%, similar to that reported in previous publications (Table 3), despite the widespread use of intermediate-acting ND-NMBA figure. We would like to highlight the use of doses close to DE95x2 in the sample analyzed and a total preference for the use of ND-NMBA of steroid type, whereas a global trend is toward the use of lower doses of these drugs and a reduction of their use only for selected cases. Our data show that pancuronium is associated with a greater probability of PORC as reported by previous studies.19 Although the sample size of our study does not allow us to make greater assertions, we believe there is a greater likelihood of adverse events related to the combined use of more than one ND-NMBA.
Incidence of postoperative residual curarization found in previous studies and evolution of diagnostic criteria (TOF).
| Author | Year | BNMND | Definition of PORC by TOF | Incidence (%) |
|---|---|---|---|---|
| Bevan et al.20 | 1988 | Pancuronium | <0.7 | 36.2 |
| Atracurium | <0.7 | 4.3 | ||
| Vecuronium | <0.7 | 8.8 | ||
| Howardy-Hansen et al.21 | 1989 | Gallamina | <0.7 | 50 |
| Atracurium | <0.7 | 0 | ||
| Pedersen et al.22 | 1990 | Pancuronium | <0.7 | 60 |
| Vecuronium | <0.7 | 27.5 | ||
| Kopman et al.23 | 1996 | Pancuronium | <0.9 | 66.1 |
| Mivacurium | <0.9 | 5.7 | ||
| Berg et al.24 | 1997 | Pancuronium | <0.7 | 26 |
| Atracurium | <0.7 | 5 | ||
| Vecuronium | <0.7 | 6 | ||
| McEwin et al.25 | 1997 | Pancuronium | <0.7 | 100 |
| Rocuronium | <0.7 | 40 | ||
| Bissinger et al.26 | 2000 | Pancuronium | <0.7 | 20 |
| Vecuronium | <0.7 | 7 | ||
| Baillard et al.27 | 2000 | Vecuronium | <0.7 | 42 |
| Hayes et al.5 | 2001 | Vecuronium | <0.8 | 64 |
| Atracurium | <0.8 | 52 | ||
| Rocuronium | <0.8 | 39 | ||
| Kim et al.28 | 2002 | Vecuronium | <0.7 | 25 |
| Rocuronium | <0.7 | 15 | ||
| Debaene et al.6 | 2003 | Rocuronium | <0.7 & <0.9 | 15.9 & 45 |
| Atracurium | <0.7 & <0.9 | 16.9 & 41.6 | ||
| Vecuronium | <0.7 & <0.9 | 17 & 46.8 | ||
| Murphy et al.29 | 2003 | Pancuronium | <0.8 | 82.1 |
| Rocuronium | <0.8 | 0 | ||
| Murphy et al.30 | 2004 | Pancuronium | <0.7 | 40 |
| Rocuronium | <0.7 | 5.9 | ||
| Garcia et al.14 | 2006 | Atracurium | <0.7 & <0.9 | 10 & 55 |
| Pancuronium | <0.7 & <0.9 | 8 & 14 | ||
| Khan et al.13 | 2006 | Rocuronium | <0.7 | 37 |
| Vecuronium | <0.7 | 17 | ||
| Tsai et al.7 | 2008 | Rocuronium | <0.9 | 31.4 |
| Cisatracurium | <0.7 | 4.8 | ||
| Butterly et al.11 | 2010 | Vecuronium | <0.9 | 24.7 |
| Cisatracurium | <0.9 | 10.4 | ||
| Barajas et al.31 | 2011 | Cisatracurium | <0.9 | 13 |
| Rocuronium | <0.9 | 24 | ||
| Vecuronium | <0.9 | 19 | ||
| Atracurium | <0.9 | 13 |
TOF, train of four; ND-NMBA, non-depolarizing neuromuscular blocker agents; PORC, postoperative residual curarization.
Source: Authors.
We believe our results may be due to multiple factors. In the first instance, there are barriers on awareness to prevent and detect this adverse event within anesthesia teams this adverse event. Additionally, the absence of other therapeutic alternatives such as benzylisoquinolinics, which have been associated with a lower incidence of PORC and interindividual variability,32,33 limits the staff practicing in public hospitals, unable to decide between different current therapeutic options in diverse clinical scenarios. Nevertheless and as shown by our results, a proportionally smaller pancuronium use has been observed. We estimate a further reduction in the use of this drug for the coming years, as usual option in operating rooms.
It has been suggested that routine use NMRM intraoperatively, could reduce the incidence of PORC,34 and thus decrease complications associated with this morbid condition. It is well known that clinical tests as elevation of the head or feet, evaluation of minute volume among others, have a poor positive predictive value for detecting PORC.5,17 Even in the case of acceleromyography (considered the current standard of care for NMRM), there is a significant variability that does not fully rule out PORC even under optimal conditions for its measurement.18,30 This fact, together with the high degree of interindividual variation in the response and time effect against equipotent doses of ND-NMBA reinforce our recommendation of not only encourage the use of NMRM, but a need to implement institutional protocols for the management of ND-NMBA in ICU35 and operating rooms as places where a large number of factors negatively influence the predictability of the clinical response to these drugs.
Our finding about the correlation between lower thenar temperatures and a higher proportion of PORC deserves further analysis. A failed statistical causality between these temperatures (coefficient of determination) and the main event can be explained by the high variability between central temperatures and peripheral areas.36 However, we believe that lower temperatures found in the group with a TOF ratio<0.9 may represent a higher proportion of intraoperative hypothermia in this group, which has been directly related to prolonged effect of NMB.9,14
This study represents one of the first publications in Latin America in order to delimit this problem at public university hospitals14,32,37; scenarios where limitations in alternative therapies and devices for monitoring and preservation of homeostasis during surgery are frequent. Similarly, the approaches and routines in NMB dosage, NMRM use and reversal of NMB are heterogeneous as shown our results. However, we must recognize important limitations in this report since aspects such as missed data of core temperatures for the subjects after surgery, the exact timing of NMB reversal (when this was performed) or ensuring a temperature above 32°C in the member assessed, could not be dealt with. In regards to standardization of TOF test arrival upon PACU, we follow the guidelines for NMRM, considering that the voltages used in our study are valid for the evaluation of neuromuscular function for awake patiens.38
ConclusionsCurrent prevalence of PORC in a Latin American university hospital representative of other institutions in the area, is as high as reported by similar studies around the world. Despite an apparent reduction in the use of long lasting ND-NMBA an unacceptably high incidence of this adverse event persists. Although this study failed to show a clear association between hypothermia and PORC, we considered that the absence of thermal protection strategies could be a precipitant factor related to ND-NMBA problems in PACU. Given the high prevalence of this problem, we strongly suggest to enhance strategies to stimulate the routine practice of NMRM in public hospitals and efforts to assure availability of different therapeutic options for this purpose, as well as to encourage surgical teams to build ND-NMBA using algorithms in order to offer the best possible perioperative care to our patients.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that the procedures followed were in accordance with the regulations of the relevant clinical research ethics committee and with those of the Code of Ethics of the World Medical Association (Declaration of Helsinki).
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
FinancingThe authors did not receive sponsorship to carry out this article.
Conflicts of interestThe authors report that they have no conflict of interest.
Please cite this article as: Ariza F, Dorado F, Enríquez LE, González V, Gómez JM, Chaparro-Mendoza K, et al. Relajación residual posoperatoria en la unidad de cuidados postanestésicos de un hospital universitario: Estudio de corte transversal. Rev Colomb Anestesiol. 2017;45:15–21.