The use of checklists in healthcare, has proven to be a useful means for improving safety in care and reducing errors and adverse events; however, acceptance and use by healthcare practitioners is still an important problem.
ObjectiveTo describe the degree of knowledge and acceptance of the use of checklists, and to determine the percentage of safe practices performed by healthcare workers during obstetric care in obstetrics and gynaecology units in Colombia.
MethodCross-sectional observational study. The sample consisted of healthcare teams of the obstetric areas in three institutions. The acceptance survey was given based on convenience sampling to 38 healthcare workers in institution A, 74 in institution B and 50 in institution C, and 29 maternal care observations were made in each institution.
ResultsIt was found that healthcare workers are aware of the checklists, have used them or are using them, and show and intermediate level of favourable attitudes, institution A being the one with the most favourable attitude towards their use. The three institutions had similar percentages of compliance with safe behaviours (72–79%), but some had lower values in areas such as confirming or administering antibiotics, compliance with the hand washing protocol, and processes related to patient or family education.
ConclusionsHealthcare professionals working in the obstetric units assessed had, at the time, knowledge and experience with the use of checklists and relatively good attitudes towards them; moreover, the level of compliance with safe behaviours was medium to high.
El uso de listas de verificación en el área de la salud, ha mostrado ser una herramienta útil para mejorar la seguridad en la atención, disminuir errores y eventos adversos; sin embargo, uno de los principales problemas se presenta en la aceptación y uso que los trabajadores de la salud hacen de las mismas.
ObjetivoDescribir el grado de conocimiento y aceptación en el uso de listas de verificación y determinar el porcentaje de prácticas seguras que realizan los trabajadores de la salud durante la atención del parto en tres unidades de ginecobstetricia en Colombia.
MetodologíaEstudio observacional de corte transversal. La muestra estuvo conformada por equipos de la salud de las tres instituciones que hicieron parte del estudio en las áreas de atención a gestantes. Se aplicó, bajo un muestreo por conveniencia, la encuesta de aceptación a 38 trabajadores de la salud de la institución A, 74 de la B y 50 de la C y se realizaron 29 observaciones de atención a gestantes en cada centro.
ResultadosSe encontró que los trabajadores de la salud conocen, han usado o usan listas de verificación y muestran actitudes favorables en un nivel intermedio, siendo la institución A la que mostró actitudes más favorables al uso de las mismas. Las tres instituciones tuvieron un porcentaje similar en el cumplimiento de los comportamientos seguros (72% - 79%), pero algunos de éstas mostraron valores menores en aspectos como: confirmar o suministrar antibióticos, cumplir el protocolo del lavado de manos y los procesos relacionados con la educación a los pacientes o acompañantes.
ConclusionesLos trabajadores de las unidades de obstetricia evaluadas tenían, en ese momento, conocimientos y experiencia en el uso de listas de chequeo y actitudes algo favorables frente a las mismas; además, el nivel de cumplimiento de comportamientos seguros estuvo en un porcentaje medio-alto.
The use of checklists in healthcare has been shown to be a useful means for improving safety in healthcare, reducing errors and adverse events, enhancing the exchange of information, and improving work team cohesiveness.1–4 Workers are responsible for completing this type of tool and, consequently, it is important to design strategies to assess the degree of knowledge among the staff of the tools that they will use, as well as to determine their willingness to implement them in their units; this in order to create programmes that can have an impact on compliance with practices designed to improve patient safety.
However, evidence shows that despite the positive results of the use of checklists in healthcare, implementation and compliance by healthcare staff has not been an easy task. Some of the hurdles that have a direct impact on acceptance of these tools are related to the lack of staff and the fact that they perceive the tool as a burden and that completing it takes away time from their work and disrupts the workflow. Likewise, it has been reported that the staff feels that checklists do not favour communication, imposes a delay, and increases the amount of paper work and the overall workload.5,6
This means that before implementing checklists, it is important to know the perception of healthcare professionals regarding their use and usefulness. It is also paramount to have a clear knowledge of safe practices performed routinely and to identify which of them are forgotten or omitted during the care process in order to determine compliance with checklists and the usefulness of their implementation.7–10
In 2015, the World Health Organisation (WHO) launched the Safe Childbirth Checklist, aimed at improving essential practices in maternal and perinatal care. This list includes 29 behaviours that need to be checked at four specific times during delivery care: admission, before childbirth, after childbirth and before discharge. Efforts are currently being made to implement it in different parts of the world.11
This research is part of a project designed to implement the safe childbirth checklist in Colombia. This requires answers to the following questions: which safe practices are performed or omitted by healthcare workers during delivery and childbirth in the obstetric sand gynaecology (OB/GYN) units in Colombia; and what is the level of knowledge and acceptance of the use of checklists among healthcare staff in the OB/GYN units in Colombia.
MethodCross-sectional observational studyPopulationThe sample consisted of healthcare teams working in the obstetric areas in the three institutions which agreed to participate in the study. There were no exclusion criteria.
A sample size of 29 observations was estimated to be needed in order to detect an initial mean of 10 safe practices, a standard deviation of 3.0, an accuracy of 1.0, alpha 0.05, and an a 10% proportion of expected losses.
For assessing acceptance of the checklist, a sample size was estimated for the population of each institution, taking an expected percentage of 75%, with an accuracy of 10, a 95% confidence interval and the design effect of 1. The results were the following: in institution A, with a population of 46 subjects, a minimum sample of 29; in institution B, with a population of 180 subjects, a minimum sample of 52; and in institution C, with a population of 94 subjects, a minimum sample of 41.
ProcedureThe observers attended the obstetric reception area and measured the number of safe practices performed during the course of the care process. The observers did not interact in any way with the patients or the healthcare professionals during their observations. The acceptance surveys were given to each of the health workers until the minimum sample size was reached by institution, using sequential convenience sampling.
Ethical considerationsThis work was performed in accordance with the international and national recommendations for biomedical research.12,13 Healthcare workers were not subjected to any disturbing interventions.
The research protocol was approved by the ethics committees of the participating institutions, after having received approval from the Ethics Committee of Universidad Nacional de Colombia.
ToolsA list based on the Safe Childbirth Checklist was designed to measure the percentage of safe behaviours performed and it was used to record whether the healthcare team complied with the expected behaviours in each of the stages of obstetric care. Overall, 47 safe behaviours were observed (12 on admission, 14 before childbirth, 11 after childbirth, and 10 at discharge).
The acceptance survey comprised 22 items. The knowledge sub-scale consisted of 4 dichotomous items (yes/no) and was scored from zero (0) to four (4), where zero was no knowledge or use of checklists, and 4 was knowledge, past use, and current use in daily practice. The acceptance sub-scale consisted of 18 Likert-type items (from totally disagree to totally agree), with scores ranging between 18 and 90, where 18 reflected unfavourable attitudes regarding the use of checklists because they were considered not very useful, difficult to apply, not contributing to safety or creating additional workload, and 90 reflected favourable attitudes.
Bias controlIn order to control for the Hawthorne effect, the observers attended the obstetric units one week before starting formal measurements, considering resource availability and the fact that there is still no clear knowledge about how to control it effectively.14 The workers were given just a general overview beforehand of what was being measured, in order to reduce the possibility of behaviour shaping. In order to control for measurement and observation bias, the observers received training in advance so that they could fulfil their job and measure variables under high quality standards.
ResultsAcceptance surveyThe survey was given to a total of 162 workers from the three participating institutions. The results are shown in Tables 1 and 2.
Frequency and percentage by jobs of the staff given the Checklist Acceptance Survey.
| Institution | Total no. of respondents | Job | Frequency | (%) |
|---|---|---|---|---|
| A | 38 | Licensed practical nurse | 17 | 44 |
| Nursing | 6 | 16 | ||
| General practitioner | 6 | 16 | ||
| OB/GYN | 6 | 16 | ||
| Paediatrics | 3 | 8 | ||
| B | 74 | Licensed practical nurse | 34 | 46 |
| Nursing | 14 | 19 | ||
| General practitioner | 5 | 7 | ||
| OB/GYN | 18 | 24 | ||
| Paediatrics | 2 | 3 | ||
| Anesthesiology | 1 | 1 | ||
| C | 50 | Licensed practical nurse | 22 | 44 |
| Nursing | 7 | 14 | ||
| General practitioner | 4 | 8 | ||
| OB/GYN | 10 | 20 | ||
| Medical student | 7 | 14 |
Results of the checklist acceptance survey.
| Institution | Subscale | Median (IQR) | Minimum–maximum |
|---|---|---|---|
| A | Knowledge | 4 (3–4) | 1–4 |
| Acceptance | 68 (62–77) | 45–90 | |
| B | Knowledge | 4 (4–4) | 0–4 |
| Acceptance | 67.5 (63–76) | 41–90 | |
| C | Knowledge | 4 (3–4) | 0–4 |
| Acceptance | 77 (73–83) | 45–88 |
IQR: inter-quartile range.
Source: Authors.
As shown, the survey was given to individuals performing different jobs, with a greater participation of licensed practical nurses and registered nurses, who are the majority of the workers in these units.
Based on the results of the survey, it was found that all the respondents, in general, are aware, have used or use checklists, and showed an intermediate level of favourable attitudes, institution A being the one with the most favourable attitudes regarding their use.
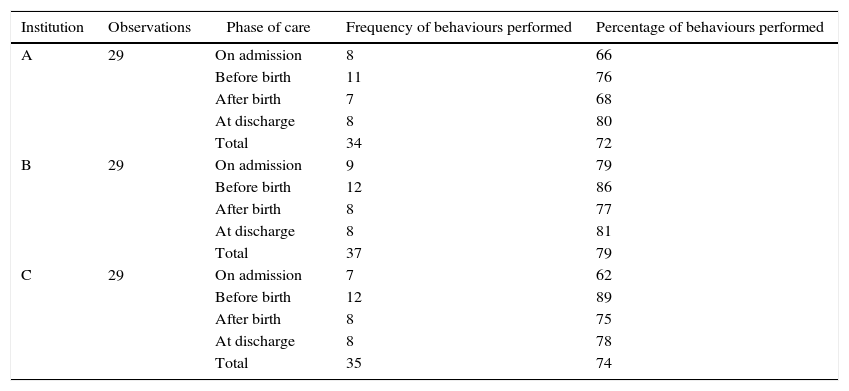
Safe behavioursThe observers followed compliance with the 47 safe behaviours (see Annex 1), and the compliance percentages at each of the institutions are shown in Table 3.
Percentage compliance with safe behaviours proposed in the checklist, before initiating the intervention (baseline).
| Institution | Observations | Phase of care | Frequency of behaviours performed | Percentage of behaviours performed |
|---|---|---|---|---|
| A | 29 | On admission | 8 | 66 |
| Before birth | 11 | 76 | ||
| After birth | 7 | 68 | ||
| At discharge | 8 | 80 | ||
| Total | 34 | 72 | ||
| B | 29 | On admission | 9 | 79 |
| Before birth | 12 | 86 | ||
| After birth | 8 | 77 | ||
| At discharge | 8 | 81 | ||
| Total | 37 | 79 | ||
| C | 29 | On admission | 7 | 62 |
| Before birth | 12 | 89 | ||
| After birth | 8 | 75 | ||
| At discharge | 8 | 78 | ||
| Total | 35 | 74 |
The percentage of compliance with safe behaviours was roughly the same in the three institutions, ranging between 72% and 79%, with the lowest percentage occurring at the time of admission in institution C (62%), and the highest during the time before childbirth in the same institution (89%).
Source: Authors.
In the three institutions, the behaviours that were least observed were number 4 (“determining whether the mother needed antibiotics”), number 9 (“following the hand washing protocol”) and number 12 (“educating the mother and companion on signs of alarm”). Likewise, institutions A and C had low compliance for behaviour number 2 (“initiating the Partograph”) and 11 (“the presence of a companion is allowed”).
Before childbirth, percentage of compliance for behaviour number 2 was very low in the three institutions (“determining whether the mother needed antibiotics”), and behaviours 12 and 13 were rarely observed in institution A (determining the” availability of suction and resuscitation supplies”), and behaviour 14 (“determining the availability of an assistant in case he/she is needed”) in institution B.
After childbirth, the behaviours with the lowest compliance level were number 11 (“educating the mother and companion on signs of alarm”) in the three institutions; number 1 (“checking for abnormal bleeding”) in institutions A and B; and 2 and 10 (“determining whether the mother needed antibiotics and whether breastfeeding and skin-to-skin contact with the newborn were initiated”) in institution A; and number 6 (“determining whether the newborn needed antibiotics”) in institution C.
Before discharge, the lowest levels of compliance were found for behaviours 8 and 10 (“education on family planning” and “signs of alarm at home”) in the three institutions; number 4 (“determining whether the newborn is feeding well”) in institution A, and behaviour 2 (“determining whether the mother needed antibiotics”) in institution C.
DiscussionAfter the impact of the use of checklists in safe surgery, the WHO launched the Safe Childbirth Checklist in order to help reduce maternal and neonatal morbidity and mortality.15 Colombia was among the countries that adhered to the participation in this pilot test, and in its study it assessed compliance with the safe behaviours comprising the WHO checklist adapted for Colombia. Likewise, it measured acceptance of the use of checklists by healthcare workers in three obstetric units in the country as a preliminary research before its adoption.11
Overall, the percentage of compliance with safe behaviours was similar for the three institutions (72–79%). However, there was lower compliance with some behaviours like determining the need for antibiotics or providing them, complying with the hand washing protocol, and complying with processes related to patient and companion education. In the case of antibiotics, non-compliance may have been associated with the difference in criteria used in the checklist for their administration, and the criteria of the Colombian clinical practice guidelines for care during childbirth, which recommends meeting two or more criteria before giving antibiotics, in an attempt at preventing microbial resistance.16
In a systematic review, Ronsmans et al. (2006) found that infections are one of the main causes of maternal mortality. Consequently, it is important to review the criteria used for providing or withholding antibiotics in the country's protocols and guidelines in order to adjust them to the WHO recommendations.17 Regarding the other behaviours, the results may be associated with low compliance with institutional protocols and the fact that Colombia lacks programmes designed to promote a literacy culture in health.18
The other cases of non-compliance that were identified and which are of great relevance for childbirth care included failure to start the Partograph on time, failure to confirm availability of suction and resuscitation supplies, failure to check for abnormal bleeding, failure to start breastfeeding protocol, and failure to allow the presence of a companion during labour. These result in a deterioration of the quality of care and in an increased risk for the mother and the newborn. For this reason, there is a need to think about implementing interventions like those of the Karnataka Centre (India) which helped improve individual practices and mitigate some of the problems during delivery care, through interventions that consisted of involving the administrative leaders in the process, providing a one-day training (8h) of theory and practice on safety principles in obstetric units, identification of current practices and the way to use the checklist, one week of simulation and supervised practice, and constant monitoring and evaluation.19
Regarding the acceptance survey, healthcare workers reported that they are aware, use or have used checklists, and they were found to be at an intermediate level of acceptance. These positive results may be associated with the fact that the safe surgery checklist a well as other checklists in healthcare were implemented in Colombia more than three years ago and they are mandatory in many instances because they are used as care quality indicators.20,21
Noteworthy among the strengths of this study is bias control by the observers, achieved by means of a prior training of the teams of workers in an attempt at standardising and ensuring the quality of the data collection process. The three implementers had the same knowledge and ability to identify the behaviours, leading to a homogenous observation across the three institutions. Also noteworthy was the performance of the measurements with minimum contact between the observers and the healthcare workers of each institution in order to reduce the Hawthorne effect, mitigating the possibility of the workers changing their behaviours because they felt observed and appraised.19,22 Additionally, the survey on checklist acceptance was designed and reviewed by a group of expert jurors and had adequate validity and reliability indicators.23
Notwithstanding, one of the limitations was failure to include a heterogenous sample of healthcare institutions, given that the three participating institutions were located in urban areas and provided intermediate and high complexity services. This means that the results do not represent the diversity of maternal care context in the country, in particular in rural settings with limited access to physical, technological and human resources.
Another issue was convenience selection of the respondents to the checklist acceptance survey. The survey was given to the workers who agreed to complete the tool voluntarily; this voluntary acceptance, in the use of checklists, may have impacted the results in the sense that they could have been overestimated considering that the group of volunteers may have been more prone to exhibiting a favourable attitude towards checklists. To avoid this type of bias, the recommendation when considering the implementation of a checklist in obstetrics is to first determine the degree of acceptance by all the healthcare staff working in that area.
ConclusionsThe conclusion from these results was that, in the three healthcare institutions observed, the healthcare staff working in the obstetric area were aware of the checklists and exhibited favourable attitudes towards them; moreover, they complied with the majority of the safe behaviours suggested by the WHO for safe childbirth, without having received prior training on the Safe Childbirth Checklist. However, in terms of safe behaviours, it was found that low-compliance items were the ones associated with the main causes of maternal and neonatal morbidity and mortality in our country, namely, severe bleeding and infections, confirming the importance of implementing strategies to reduce mortality from these causes in healthcare institutions providing obstetric care.16,24
The checklist acceptance survey is a useful tool for assessing the willingness of healthcare workers to modify their clinical practices and for helping institutions, based on the results obtained, to structure their change management processes. As highlighted by Gómez in 2003, staff engagement is critical for the implementation of any technology, including checklists.21
In order to ensure 100% compliance, it is important for healthcare workers to receive training based on guidelines, protocols, manuals and tools, and for managers to set up follow-up, control and non-punitive appraisals in order to facilitate changes in behaviour, thus increasing adherence to these types of clinical practices; the evidence shows that these institutional changes are a challenge to all.25–28 In other words, it is important to implement strategies that promote a culture of patient safety and impact all the participants in the care process.
Finally, it is suggested to make a more heterogenous sample selection for future research, and to consider potential factors that may impact compliance and acceptance, including such things as complexity level, work overload, lack of competent staff, and shortage of supplies. Likewise, it is important to undertake a study to collect information on the reasons why healthcare workers do not adhere to the essential practices contained in the Safe Childbirth Checklist when the evidence shows that doing so contributes to lower maternal and neonatal morbidity and mortality.
Ethical disclosuresProtection of human and animal subjectsThe authors state that for this investigation, the international and national ethical standards for researches with human been were followed.
Confidentiality of dataThe authors state that they have followed the protocols of its work center on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the informed consent of the patients and/or subjects referred to in the article. This document works in the power of the correspondence author.
FundingThis work was funded by COLCIENCIAS (Colombian Science, Technology and Research Department), CT: 657-2014, Code: 500865741087; Sociedad Colombiana de Anestesiología y Reanimación (S.C.A.R.E. – Technology Development Centre) and the Clinical Research Institute of Universidad Nacional de Colombia.
Conflicts of interestDr. Javier Hernando Eslava is currently the Director at the Technology Development Centre of the Sociedad Colombiana de Anestesiología y Reanimación (S.C.A.R.E.).
Ana Carolina Amaya, María Lucero Cortés, Diana Franco, Juan David Mojica and Sully Hernández worked as contractors for the Technology Development Centre of the Sociedad Colombiana de Anestesiología y Reanimación (S.C.A.R.E.) during the implementation of this project.
SAFE BEHAVIOUR OBSERVATION FORM
| No. | Behaviour | Yes | No |
|---|---|---|---|
| On admission | |||
| 1 | Was it determined in the mother needed to be referred and, if yes, was she referred? | ||
| 2 | Was the Partograph started when cervical dilatation was greater than, or equal to, 4cm? | ||
| 3 | Was it determined if the mother was allergic to any medication(s) and, if yes, were those medications documented? | ||
| Mother needs | |||
| 4 | Was it determined if the mother needed antibiotics and, if yes, was she given them? | ||
| 5 | Was it determined if the mother needed magnesium sulphate and, if yes, was she given it? | ||
| 6 | Was it determined if the mother needed antihypertensive drugs and, if yes, was she given them? | ||
| 7 | Was it determined in the mother was tested for syphilis and, if no, was a rapid test performed? In case it was positive, was she given treatment? | ||
| 8 | Was it determined if the mother was tested for HIV and, if no, was a rapid test performed. In case it was positive, was she given treatment? | ||
| Supplies confirmation | |||
| 9 | Was the availability of essential supplies confirmed and was the hand washing protocol followed? | ||
| 10 | Was the availability of gloves confirmed and were they used for every vaginal examination? In the event of ruptured membranes, were sterile gloves used? | ||
| 11 | Was the presence of a companion encouraged and allowed during labour? | ||
| 12 | Was the mother or the companion educated to recognise signs of alarm and ask for help? | ||
| Before birth | |||
| 1 | Was the Partograph completed when cervical dilation was greater than, or equal to, 4cm? | ||
| Mother needs | |||
| 2 | ¿Was it determined whether the mother needed antibiotics and, if yes, were they administered? | ||
| 3 | ¿Was it determined whether the mother needed magnesium sulphate and, if yes, was it administered? | ||
| 4 | ¿Was it determined if the mother needed antihypertensive drugs and, if yes, were they administered? | ||
| Confirm supplies for the mother: | |||
| 5 | Was the availability of sterile gloves for delivery care confirmed? | ||
| 6 | Was the availability of antiseptics for patient washing and preparation in accordance with the institutional protocol confirmed? | ||
| 7 | Was the availability of uterotonic agents confirmed (preferably oxytocin) for care during delivery? | ||
| Confirm supplies for the newborn: | |||
| 8 | Was the availability of a clean towel confirmed? | ||
| 9 | Was the availability of sterile scalpel or scissors to cut the cord confirmed? | ||
| 10 | Was the availability of rubber ligature, plastic forceps or umbilical tapes confirmed? | ||
| 11 | Was the availability of a heat source confirmed? | ||
| 12 | Was the availability of a suction device confirmed? | ||
| 13 | Was the availability of bag/valve/mask confirmed? | ||
| 14 | If needed, is there an assistant available (healthcare staff/companion) to accompany during delivery? | ||
| After birth | |||
| 1 | Was it determined whether maternal bleeding was normal and, if not, was the institutional protocol for managing bleeding activated? | ||
| The mother needs | |||
| 2 | Was it determined whether the mother needed antibiotics and, if yes, were they administered? | ||
| 3 | Was it determined whether the mother needed magnesium sulphate and, if yes, was it administered? | ||
| 4 | Was it determined whether the mother needed antihypertensive drugs and, if yes, were they administered? | ||
| The newborn needs | |||
| 5 | Was it determined whether the newborn needed referral and, if yes, was it referred? | ||
| 6 | Was it determined whether the newborn needed antibiotics and, if yes, were they administered? | ||
| 7 | Was it determined whether the newborn needed special care or monitoring and, if yes, was it provided? | ||
| 8 | Was it determined whether the newborn needed antivirals and, if yes, were they administered? | ||
| 9 | Was the newborn screened for congenital hypothyroidism and blood classification? | ||
| 10 | Were breastfeeding and skin-to-skin contact initiated in healthy conditions? | ||
| 11 | Was the mother or the companion educated to recognise signs of alarm in the mother or the newborn and to ask for help in case they occur? | ||
| Before discharge | |||
| 1 | Was maternal bleeding checked and, if found abnormal, was it controlled and was discharge postponed? | ||
| 2 | Was it determined whether the mother needed antibiotics and, if yes, were they administered and was discharge postponed? | ||
| 3 | Was it determined whether the newborn needed antibiotics and, if yes, were they administered, was discharge postponed and were special care and monitoring provided? | ||
| 4 | Was it determined whether the newborn was feeding well and, if not, was discharge postponed and were good breastfeeding practices established? | ||
| 5 | Was it determined whether an HIV positive mother has been given anti-retroviral coverage for 6 weeks for herself and the baby and, if not, was breastfeeding interrupted and was the institutional protocol applied? | ||
| 6 | Was it determined whether the mother and the newborn received treatment based on the serology results? | ||
| 7 | Were catheters and lines removed if they were used? | ||
| 8 | Was counselling on family planning given and was the mother referred for the administration of the selected method? | ||
| 9 | Was a follow-up appointment assigned? | ||
| 10 | Does the mother or the companion recognise the signs of alarm and is ready to ask for help in the event any of those signs are manifested in the mother or the newborn? | ||
Source: authors.
Please cite this article as: Amaya-Arias AC, Cortés ML, Franco D, Mojica JD, Hernández S, Eslava-Schmalbach J. Comportamientos seguros y aceptación de listas de verificación en tres unidades de ginecobstetricia de tres instituciones de áreas urbanas de Colombia. Rev Colomb Anestesiol. 2017;45:22–30.