Optimal linear endobronchial ultrasound (EBUS) outcomes require sedation to ensure that the patient remains calm, immobile, and does not cough, and so that the bronchoscopist can work comfortably. The choice of anesthesia techniques, on a spectrum ranging from general anesthesia to sedation, is not standardized. The aims of this study were to determine doses, safety and satisfaction for intravenous sedation with propofol and remifentanil, and identify potential predictors of coughing during the procedure, and determine patient and bronchoscopist satisfaction with the procedure.
Patients and methodsThe prospective study included patients undergoing EBUS under sedation in a tertiary hospital.
ResultsA total of 90 patients underwent EBUS under sedation with remifentanil and propofol, at infusion rates of 0.13 (0.09–0.17)μgkg−1min−1 and 2.34 (1.5–3.6)mgkg−1h−1, respectively. Just over four fifths of the patients (81%) coughed at some point during the ultrasound procedure. In 8% of patients the procedure was promptly discontinued due to coughing and desaturation. There were no major complications directly related to sedation. Bronchoscopists and patients rated their satisfaction with the procedure as excellent or good in most cases. There was no statistically significant relationship between the number of coughing episodes during the procedure and any of the following variables: positive cough test, a habitual cough, tobacco dependence, or severity of chronic obstructive pulmonary disease.
ConclusionsRemifentanil and propofol administered by an anesthesiologist enabled spontaneously breathing patients to undergo linear EBUS, although with a high incidence of coughing and particularly desaturation. No predictors for coughing during EBUS were identified.
Para la óptima realización de la ultrasonografía endobronquial (USEB) lineal es imprescindible que el paciente esté sedado para que se mantenga tranquilo, no tosa ni se mueva y el endoscopista trabaje cómodamente con un buen rendimiento de la exploración. Actualmente la técnica anestésica no está estandarizada y varía desde una anestesia general a una sedación. El objetivo del presente trabajo es conocer la dosificación, la seguridad y la satisfacción de la sedación endovenosa con propofol y remifentanilo e identificar los posibles factores predictivos de tos durante el procedimiento.
Pacientes y métodosSe estudió prospectivamente a los pacientes a quienes se realizó la USEB bajo sedación en un hospital de tercer nivel.
ResultadosSe realizó la USEB a 90 pacientes bajo sedación con remifentanilo y propofol, a una velocidad de infusión de 0,13 (0,09-0,17) g kg−1 min−1 y 2,34 (1,5-3,6) mg kg−1 h−1, respectivamente. El 81% de los pacientes tosieron en algún momento de la exploración. En el 8% de los pacientes se interrumpió el procedimiento puntualmente por tos y desaturación. No se registraron complicaciones graves directamente relacionadas con la sedación. El nivel de satisfacción del neumólogo y del paciente con el procedimiento fue excelente o bueno en la mayoría de casos. No se observó relación estadísticamente significativa entre el número de episodios de tos durante la ecobroncoscopia y las variables test de la tos, ser tosedor habitual, hábito tabáquico o grado de severidad de la EPOC.
ConclusionesLa sedación con remifentanilo y propofol realizada por un anestesiólogo permite realizar la USEB lineal en ventilación espontánea aunque con una elevada incidencia de tos y desaturación, siendo esta última la complicación más frecuente. No se encontraron factores predictivos de la tos durante el procedimiento.
Transbronchial needle aspiration (TBNA) guided by ultrasound bronchoscopy or linear endobronchial ultrasound (EBUS) is a minimally invasive procedure of great help in the diagnosis of mediastinal lymphadenopathy and tumors.1 Morbidity and cost are lower than with mediastinoscopy2,3 and the main indication for the procedure is staging of patients with lung cancer.1–8
Linear EBUS is performed using a flexible echo-bronchoscope that comprises a distal ultrasound probe to allow concurrent ultrasound and endoscopic views. It also allows to perform cytology and histology biopsies under real-time ultrasound control.4,8,9
The anesthetic technique used in EBUS has not been standardized and varies substantially by institution and individual anesthetist. Initially, exploration was done under general anesthesia and orotracheal intubation or laryngeal mask.10,11 Recently, improvements in the learning curve and in patient preparation have shortened exploration time, which has resulted in a growing trend towards replacing general anesthesia with sedation.12 Sedation during EBUS is complex because it requires achieving two opposite goals, i.e., tolerance of the exploration without coughing or moving, and avoiding respiratory depression since the airway is not open for ventilation.
There are few publications on drugs and ideal sedation doses. Consequently, the objectives of this study were to determine the efficacy and safety of intravenous sedation with propofol and remifentanil for EBUS, as well as to identify potential predictors for cough during the procedure.
Patients and methodsPopulationAll patients undergoing linear EBUS-guided TBNA for the study of mediastinal lymphadenopathy or masses between January 2009 and June 2010 using sedation with remifentanil and propofol were analyzed prospectively and consecutively. Patients under 18 years of age, or patients who had been intubated previously or had a tracheostomy, non-collaborating patients, or patients who were allergic to any of the drugs administered were excluded. The study was approved by the Clinical Research Ethics Committee (2011/4544/I) of our institution.
ProcedureAll the explorations were performed by the same bronchoscopist, whereas sedation was given by three anesthetists, following a standardized protocol. All patients were assessed during the preoperative visit and came to the procedure after a minimum fasting period of 6h. The majority of the explorations were done on an outpatient basis. One hour before the procedure, the patients were given diazepam 5mg sublingual as anxiolytic premedication and 1mg intramuscular atropine. On arrival at the Respiratory Endoscopy Unit, patients received topical anesthesia with 5ml of nebulized 2% lidocaine at 6–8l/min for 10min, followed by 5ml of liquid 2% lidocaine solution for gargles. Monitoring consisted of continuous electrocardiography, blood pressure and peripheral hemoglobin saturation (SpO2) using pulse oximetry (Dash 2500, General Electric). Oxygen therapy was administered through a nasal cannula with the aim of achieving a SpO2 greater than 97%. The oropharyngeal cannula (Williams) was placed 20min after the topical oral anesthesia, boosting local anesthesia with a 10% lidocaine spray in the event of intolerance. The administration of 1mg of midazolam was at the discretion of the anesthetist on the basis of the anxiety reported by the patient. The continuous infusion of propofol and remifentanil was then started with no initial bolus, in order to keep the patient calm, breathing spontaneously and responding to verbal or tactile stimuli. Remifentanil and propofol perfusion was started at a rate of 0.1μgkg−1min−1 and 2mgkg−1h−1, respectively. The exploration was started 5min after the initiation of sedation, provided the level of sedation was appropriate, with the instillation of 5ml of 2% lidocaine through the endoscope (model BF-UC180F Olympus, Tokyo) on the vocal cords, 2.5ml on the trachea, and 2.5ml on each main bronchus.
If the patient moved or coughed repeatedly, remifentanil perfusion was increased 0.5μgkg−1min−1 and, if after 5min the desired clinical response was not obtained, propofol perfusion was increased 1mgkg−1h−1. If the patient continued to move or cough in spite of those measures, the rate was modified at the anesthetist's discretion up to a maximum of 0.25μgkg−1min−1 of remifentanil and 5mgkg−1h−1 of propofol. On the other hand, in the event of an episode of apnea, desaturation or excess sedation, perfusions were stopped and once the episode was addressed, the prior rate of infusion was reduced 0.5μgkg−1min−1 for remifentanil and 1mgkg−1h−1 for propofol.
After completing the exploration, the satisfaction of both the pulmonologist and the patient with the anesthetic procedure was recorded, together with the number of coughing episodes and their interference with the endoscopic technique, and the intensity of pain during the test.
VariablesThe following variables were recorded- (1)
Dosing of the drugs administered.
- (2)
Number of coughing episodes and desaturation during the exploration. The frequency of coughing episodes during the procedure was calculated by grouping the episodes under 4 categories on the basis of the number of occurrences: 0–5, 6–10, 11–20 and more than 20 coughing spells. Desaturation was defined as a drop in SpO2 <90% for more than 1min, while FIO2 and oxygen supply were maintained at all times.
- (3)
Factors that could predict the presence of cough: cough test, history of habitual coughing, smoking, presence and severity of COPD. The cough test was performed by asking the patient to cough after a deep breath, and it was considered positive if the patient coughed more than once.13 The test was performed before giving nebulized lidocaine. Cough was considered to be habitual, chronic or recurrent if present for more than eight weeks. Smoking was recorded according to 3 categories: (a) non-smokers: subjects who had never smoked; (b) smokers: subjects who reported smoking daily or occasionally at the time of the interview; and (c) former smokers: subjects who had quit smoking more than 6 months before the bronchoscopy. Airflow obstruction in COPD patients was defined by spirometry when the post-bronchodilation FEV1/FVC ratio was lower than 0.7 (or below the lower normal limit in subjects over 60 years of age).
The severity of the COPD was based on the spirometric classification and included four stages: Stage I: mild (FEV1% ≥80); Stage II: moderate (FEV1% ≥50 and <80); Stage III: severe (FEV1% ≥30 and <50) and Stage IV: very severe (FEV1% <30).14,15
- (4)
Pulmonologist and patient satisfaction with the procedure. Sedation was assessed by the endoscopist as follows: excellent (best); good (procedure conducted with very few occurrences); fair (procedure that could be performed but took longer because of occurrences); poor (multiple occurrences forcing to stop the procedure); and bad (the procedure could not be started because of poor tolerance). Patient satisfaction was assessed at the end of the ultrasound bronchoscopy by asking the patient if he/she would undergo the same type of sedation in the future if necessary.
- (5)
Pain intensity during the exploration. Pain intensity was measured at the end of the procedure using a visual analog scale (VAS), where 0 was no pain and 10 the worst pain possible.
- (6)
Length of the procedure. The length of the EBUS was considered from the moment the echo-bronchoscope was introduced in the mouth until it was removed, whereas sedation was considered from the moment anesthetic administration with infusion pumps was started until it was interrupted at the end of the exploration. The length of the procedure does not specify the number of biopsies made and includes the time spent waiting for the in situ pathology test results.
- (7)
Complications of sedation or of the procedure.
Categorical variables have been described in terms of absolute frequencies and percentages, and the quantitative variables have been expressed as means and standard deviation, or as median and 25th and 75th percentiles, according to whether they presented a normal distribution or not. In order to determine if there was a relationship between two categorical variables, the Chi square test or the exact Fisher test was used depending on the application conditions. In order to quantify the relationship between quantitative variables, the Spearman's Rho correlation or the Mann–Whitney U test was used. For all the analyses, p<0.05 was considered significant. The analyses were performed using the SPSS 15.0 (SPSS Inc., Chicago) statistical package.
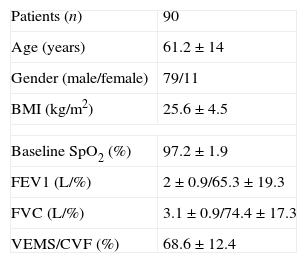
ResultsThe study included 90 patients whose demographic and clinical characteristics are shown in Table 1.
Demographic data and respiratory function.
| Patients (n) | 90 |
| Age (years) | 61.2±14 |
| Gender (male/female) | 79/11 |
| BMI (kg/m2) | 25.6±4.5 |
| Baseline SpO2 (%) | 97.2±1.9 |
| FEV1 (L/%) | 2±0.9/65.3±19.3 |
| FVC (L/%) | 3.1±0.9/74.4±17.3 |
| VEMS/CVF (%) | 68.6±12.4 |
Values expressed as mean±SD of n. BMI: body mass index; FEV1: maximum expired volume in 1s; FVC: forced vital capacity.
Premedication with 1mg intravenous midazolam was used in 48% of patients. The starting dose for sedation was 0.1μgkg−1min−1 of remifentanil and 2mgkg−1h−1 of propofol. The time elapsed between the start of sedation and the beginning of the test was 7 (5–10)min. The median rate of remifentanil and propofol infusion was 0.13 (0.09–0.17)μgkg−1min−1 and 2.34 (1.5–3.6)mgkg−1h−1, respectively. The length of sedation was 52 (38–65)min and the length of the EBUS was 40 (25–51)min.
During the ultrasound bronchoscopy, 74 patients (81%) coughed at some point during the exploration. Of those who coughed, 5 patients (6.7%) did so when the oropharyngeal cannula was introduced, and 56 (75.6%) when the echo-bronchoscope was passed between the vocal cords. In 58 cases (78.3%), the exploration was performed with no interruptions despite the cough. In the remaining 16 patients (21.6%), cough led to the prompt interruption in the procedure, and in 4 cases (5.4%) the echo-bronchoscope had to be removed temporarily because of the inability to continue with the procedure. In all of these cases, the procedure was resumed after the patients were stabilized.
The cough test was performed in 78 patients (86.6%), and it was positive in 24 cases (31%) and negative in 54 (69%).
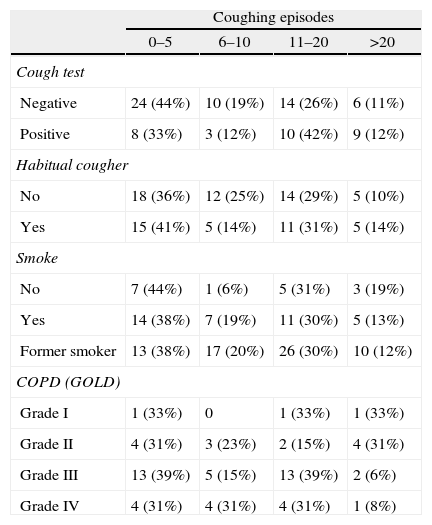
There were 36 patients (40%) with habitual cough. No statistically significant relationship was observed between the number of coughing episodes during the endoscopy and the following variables: positive cough test, habitual cough, smoking habit, or degree of COPD severity (Table 2). No association was observed between the dose of remifentanil and propofol and cough (Spearman's Rho correlation ρ=0.012, p=0.907 and ρ=0.1 p=0.3 for remifentanil and propofol, respectively). In contrast, there was a direct statistically significant relationship between a positive cough test and having habitual cough (χ2 test, p<0.001).
Relationship between the cough test, being a habitual cougher, smoking habit and COPD severity and coughing spells during EBUS.
| Coughing episodes | ||||
| 0–5 | 6–10 | 11–20 | >20 | |
| Cough test | ||||
| Negative | 24 (44%) | 10 (19%) | 14 (26%) | 6 (11%) |
| Positive | 8 (33%) | 3 (12%) | 10 (42%) | 9 (12%) |
| Habitual cougher | ||||
| No | 18 (36%) | 12 (25%) | 14 (29%) | 5 (10%) |
| Yes | 15 (41%) | 5 (14%) | 11 (31%) | 5 (14%) |
| Smoke | ||||
| No | 7 (44%) | 1 (6%) | 5 (31%) | 3 (19%) |
| Yes | 14 (38%) | 7 (19%) | 11 (30%) | 5 (13%) |
| Former smoker | 13 (38%) | 17 (20%) | 26 (30%) | 10 (12%) |
| COPD (GOLD) | ||||
| Grade I | 1 (33%) | 0 | 1 (33%) | 1 (33%) |
| Grade II | 4 (31%) | 3 (23%) | 2 (15%) | 4 (31%) |
| Grade III | 13 (39%) | 5 (15%) | 13 (39%) | 2 (6%) |
| Grade IV | 4 (31%) | 4 (31%) | 4 (31%) | 1 (8%) |
Cough test: p=0.621 (Fisher test); habitual cougher: p=0.691 (Fisher test); smoking habit: p=0.645 (Fisher test); COPD severity according to GOLD criteria: Spearman's Rho correlation ρ=−0.109, p=0.406. n=number of patients.
Of all patients, 52% had COPD criteria (Tiffeneau index <70), and of them, 3 were type I in the GOLD scale, 13 were type II, 33 were type III and 13 were type IV.
Forty-three patients (47.8%) had desaturation episodes (SpO2 <90%): 29 had up to 3 episodes, 9 had between 4 and 8, and 5 patients had >8 desaturation episodes. Of these patients, 12 recovered spontaneously with an increase in oxygen supply, and oxygenation improved in 31 cases with additional mandibular subluxation maneuvers, except for 3 patients who required manual ventilation and interruption of the ultrasound bronchoscopy. In no case was orotracheal intubation required for airway control.
A tendency towards a greater number of desaturation episodes was observed in patients with lower baseline oxygen saturation (SpO2 <97) (p=0.04).
No objective association was found among the dose of remifentanil, propofol and premedication with the desaturation episodes (Mann–Whitney test p=0.69 for remifentanil, p=0.82 for propofol and χ2 test p=0.51 for premedication). Neither did we observe a relationship between premedication and remifentanil and propofol dosing (Mann–Whitney test p=0.4 and p=0.2, respectively).
The level of satisfaction of the pulmonologist with the procedure was rated as excellent in 37 cases, good in 42, fair in 10 and poor in 1 case.
All patients except one reported that they would agree to the exploration in the future if it were necessary. Pain from the ultrasound bronchoscopy was rated as 0 in the VAS by 93% of patients, and between 0 and 4 by the remaining 7%.
Major complications included 2 arrhythmias at the end of the exploration, one fast atrial fibrillation and one supraventricular paroxysmal tachycardia that resolved with electric cardioversion and carotid massage, respectively. One patient developed minimal self-limiting bleeding with the biopsy sampling. There were no unexpected hospital admissions as a result of these complications.
DiscussionThis study describes the sedation procedure for linear EBUS at our institution. The technique has had excellent acceptance by both bronchoscopists as well as patients. The majority of patients had coughing spells during the procedure with no predictors having been found for this response.
During the past decade, scientific societies have recommended sedation and topical anesthesia of the oropharynx during fiberoptic bronchoscopy.16–19 This sedation is imperative with the new endobronchial ultrasound procedures because of their longer duration and greater invasiveness requiring minimization of movements and cough responses in order to take the cytology and histology samples by TBNA. For the patient, cough is the main issue during the bronchoscopy.20 For the endoscopist, cough is also a problem because ultrasound landmarks are lost, slowing down the procedure; and if coughing spells occur while the needle biopsy is being performed, if may lead to injury of the mediastinal structures and a lower yield of the test. Different drugs with anti-cough effects have been used to palliate coughing, including hydrocodone, dextromethorphan, opioids, codeine, etc., with varying results.16,21–28
Since the advent of ultrasound bronchoscopy, the anesthetic technique has been changing. Slonim11 considered that general anesthesia with endotracheal tube or laryngeal mask offered excellent working conditions for the endoscopist. Sarkiss10 also considered that general anesthesia was mandatory given the larger size of the EBUS instrument when compared with the conventional fiberoptic bronchoscope.10,29 General anesthesia avoids coughing, and reduces bronchospasm and laryngospasm which are the minor complications described most frequently but, on the other hand, limits the dynamic study of the vocal cords that can only be done when the patient is conscious.
With the introduction of EBUS in our institution, assistance by an anesthetist was requested. Based on our previous experience with radial EBUS30 and digestive endoscopy, we decided that sedation with propofol and remifentanil was the technique of choice.
The initial reference doses used for sedation were the ones used at our institution for endoscopic retrograde cholangiography, adjusted afterward to the clinical needs in each case. No propofol bolus was used because, in our experience, it favors respiratory depression, and we believe that this was the main reason why only 3% of patients required manual ventilation.
No relationship was observed between the dose of propofol and remifentanil given to the patients in the study and the desaturation episodes. This lack of association came as a surprise to the authors because the dose should have been the most important determining factor for desaturation. It is worth highlighting that in our group of patients, 48% had at least one episode of desaturation and, in 14 cases, the episodes occurred repeatedly throughout the procedure. The incidence of desaturation is too high in our opinion as to allow us to state that sedation is safe, especially when a SatO2<90% was considered as desaturation. Despite these results, desaturation was resolved in most cases by the increase in oxygen supply, and no more additional aggressive measures such as orotracheal intubation were required.
No relationship was found either between the sedation dose and the number of coughing spells. This result was unexpected because it would seem that a shallower sedation would favor coughing, while deeper sedation would diminish it but create greater desaturation. An attempt was made at identifying factors that could predict which patients would have a greater number of coughing spells during the procedure. The first one consisted of the cough test which, when positive, indicates the presence of bronchial secretions and the potential for greater bronchial reactivity. However, we were unable to confirm the hypothesis, and the cough test was not shown to be a predictor for cough during the procedure. Also, smoking and the presence of habitual coughing were not predictive factors for cough, as was also the case for COPD, regardless of severity. It would be interesting to find predictive factors, which is why more studies for identifying new variables are required. We believe that other aspects such as the presence of a bronchial infection at the time of the exploration might influence cough intensity. There may also be factors associated with the technique that may influence greater bronchial irritability. The number of bronchial needle biopsies or other types of airway manipulations, like other diagnostic tests, may also play a determining role. However, those aspects were not analyzed in this study and we cannot arrive at conclusions.
Acceptance of the sedation technique by the pulmonologists was excellent or good in 87.8% of cases. They were able to work comfortably in most cases, with cough and desaturation being the occurrences that forced them to interrupt the test and remove the ultrasound bronchoscope, slowing the procedure in 7 patients (7.7%). Among the patients, 98% were satisfied and considered that the procedure was not painful and that they would repeat it if it were necessary.
This study has some limitations. First, no measurement scale was used for sedation. The bispectral index was used in the first few cases, but it was found to be not useful because of high interference with the electromyogram. Second, the initial sedation doses were predetermined, but the same was not true for the number of times the perfusion rate was changed. Third, considering that it was total intravenous anesthesia, the dose should have been adjusted according to plasma concentrations using the TCI (Target Controlled Infusion) pumps, but these pumps are not available in the area where fiberoptic bronchoscopy is performed in our hospital, and only volumetric pumps can be used.
It would be interesting to conduct another prospective study to validate the effectiveness of the dose observed in this series and continue the search for a cough predictor so that patients may be classified as potential coughers or non-coughers, and act accordingly. It would also be interesting to conduct a clinical trial with a different drug in order to assess desaturation and improve safety.
The conclusion from our study is that sedation with remifentanil and propofol given by an anesthetist allows linear EBUS to be performed under spontaneous ventilation in a way that is satisfactory to patients and bronchoscopists alike, albeit with a high incidence of coughing and desaturation. No predictive factors for cough during the procedure were found.
FundingAuthor's own resources
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Vila E, et al. Sedación con propofol y remifentanilo para la ultrasonografía endobronquial con punción-aspiración en tiempo real. Rev Colomb Anestesiol. 2013;41:120–6.