Around the world, inguinal hernia repair is one of the most frequent surgical interventions and is associated with moderate to severe postoperative pain. TAP (Transversus Abdominis Plane) block appears to be a useful tool to reduce the morbidity associated with pain in inguinal hernia repair.
ObjectiveTo evaluate the analgesic effect of a TAP block in patients scheduled for primary inguinal hernia repair, 1h and 24-h post-surgery.
Materials and methodsRandomized controlled trial. 45 patients were randomized to receive placebo vs. TAP block. Clinical, surgical and anesthetic variables were analyzed. The primary outcome was pain in the first hour and the secondary outcome was pain during the first 24h, opiate use and side effects.
ResultsThe acute postoperative pain score during the first hour in the control group was 6 with maximum values of 9 in 22% of patients, whereas in the intervention group the pain score was 2 (SD: 1) (p: 0.03). Likewise, pain 24h postop and opiate consumption was lower in the intervention group than in the control group.
ConclusionsTAP block helps to reduce acute postoperative pain and the use of opiates in inguinal hernia repair.
La herniorrafia inguinal es una de las cirugías mas realizadas en el mundo, esta asociada con dolor postoperatorio de moderado a severo. El Bloqueo TAP (Transversus Abdominus Plane) parece ser una técnica útil para disminuir la morbilidad asociada con el dolor en herniorrafia inguinal.
ObjetivoEvaluar el efecto analgésico del bloqueo TAP a la hora y a las 24 horas postoperatorias en herniorrafia inguinal.
Materiales y métodosSe realizó un estudio doble ciego donde se aleatorizaron 45 pacientes para recibir bloqueo TAP vs placebo, se analizaron variables clínicas, quirúrgicas y anestésicas y se evaluó como resultado primario la intensidad de dolor agudo pop 1 hora después de la cirugía y como resultados secundarios el dolor a las 24 horas, el consumo de opiáceos y la presencia de reacciones adversas.
ResultadosEl dolor agudo postoperatorio a la primera hora en el grupo control fue de 6 con valores máximos de 9 en el 22% de los pacientes, mientras que el dolor en la primera hora en el grupo intervención fue de 2 (SD: 1) (p: 0,03). De igual forma el dolor a las 24 horas pop y el consumo de opiáceos fue menor en el grupo intervención que en el grupo control.
ConclusionesEl bloqueo TAP es útil en la reducción del dolor agudo pop y del consumo de opiáceos en herniorrafia inguinal.
Open inguinal hernia repair is a very frequent procedure performed in surgical services around the world1,2 and acute postoperative pain as described by patients ranges from moderate to severe3 in over 60% of the cases.4
Multiple approaches are used for managing this pain, raging from oral medication to minimal intervention including regional blocks.3 Among the regional blocks, the Transversus Abdominis Plane (TAP) block has proven to be effective in reducing acute postoperative pain and the use of opiates in patients undergoing inguinal hernia repair.5
However, this approach has not been widely disseminated as expected due to multiple reasons, including performing this technique under superficial anatomical landmarks that often leads to block failure and acute postoperative pain.6 However, with the advent of ultrasound-guided regional techniques, there has been increased interest in analyzing the effects of certain ultrasound-guided techniques.7
Siddiqui et al.,5 systematic review includes just 2 clinical control trials using ultrasound to guide the TAP block and both showed improved analgesic efficacy.
Since ultrasound-guided TAP block is a relatively new and easy to perform technique,8 we decided to undertake a randomized, controlled, double-blind clinical trial to proof its benefits in reducing acute postoperative pain following inguinal hernia repair.
MethodsThe trial was developed at the Special Healthcare Services Hospital (Hospital de caldas) in Manizales city between 2014 and 2015. The trial was designed and submitted to the group of graduate professors of anesthesiology, Universidad de Caldas, to the surgery department, the council of the school of health sciences, and to the ethics committee of Universidad de Caldas and all of them upon successive evaluation gave their approval to proceed with the trial. Later the trial was submitted before the research ethics committee of the Special Healthcare Services Hospital and upon completing a bioethical analysis, the committee approved the trial. The trial was included in the registry of clinical control trials www.clinicaltrials.gov and was monitored by the Anesthesiology graduate research committees of the Universidad de Caldas and the Hospital Servicios Especiales de Salud (SES).
ParticipantsAdults between 18 and 80 years old, ASA I and II, scheduled for ambulatory pre-peritoneal approach mesh inguinal hernia repair. The exclusion criteria were as follows: multiple hernia repairs, allergies to the standard medications included in the protocol, inability to communicate with the patient (because of the patient's own pathologies or as a result of technical or logistic difficulties), need to administer spinal anesthesia instead of general anesthesia, intraoperative need to do other types of surgery (colectomy, vascular repair, medium laparotomies), surgical complications, preoperative use of analgesics, or patient's refusal to participate in the trial.
All patients were instructed about the technique and on the research model and then all of them completed the informed consent to participate in the clinical trial.
Care protocolAll patients received the same model of anesthetic care as follows: a venous line was inserted 1h before surgery and prophylactic antibiotics were administered. Patients underwent non-invasive intermittent blood pressure monitoring, oximetry, cardioscopy and exhaled CO2. Intravenous anesthetic induction was administered with Propofol 2mg/kg plus lidocaine 40mg and remifentanyl 0.35mcg/kg/min for 6min. The airway was managed using a laryngeal mask 3. For 50–70kg, a #4 laryngeal mask was used, and #5 for over 70kg. The mechanical ventilation was adjusted in a controlled per volume manner. The maintenance of anesthesia was done using sevofluorane to maintain an expired value of 1.4% and intravenous remifentanil infusion between 0.1 and 0.2mcg/kg/min.
Immediately after securing the airway, all patients were assessed with a 13mHz (GE Logic-e-) lineal transducer to search the planes of the abdominal wall muscles bilaterally. Then, using a short axis and plane technique, the transversus abdominus plane was accessed on the mi-axillary line between the rib margin and the ipsilateral iliac crest at the surgical site, using a needle for administering the study substance (placebo vs. anesthetic mix according to the randomization). The time between the removal of the needle and the actual skin incision was measured to be 10min.
The surgical technique used was inguinal hernia repair using a pre-peritoneal approach, and mesh placement.
At the start of surgery 8mg of IV dexamethasone were administered and 20min prior to the end of surgery (as informed by the surgeon), 30mg/kg of dipirone and 4mg of IV morphine were administered.
The awakening from anesthesia was achieved with the suspension of the IV and inhaled medication and the patient was transferred to the post-anesthesia care unit with an Aldrette score above 8. The patients were advised on the possibility to require pain mediation as needed. A trained nurse to administer rescue medication for pain was assigned to the post-anesthesia care unit if needed. The rescue medication consisted of 2mg of IV morphine at the patient's request and if the patient repeatedly demanded analgesia, the doses administered 10min apart.
1h after stopping the administration of the general anesthesia, all patients were interviewed by a research assistant who was not aware of the intra and pre-operative conditions in each case, with a view to determine the level of pain, the use of analgesics, and the presence of any adverse reactions such as vomiting, pruritus, dry mouth, somnolence and respiratory depression.
All patients were discharged from the post-anesthesia care unit with an Aldrette score of 10, and the following analgesia regime: oral acetaminophen 1g every 6h, Naproxen 250mg every 8h and in case of severe pain, 25mg of oral tramadol in drops (10 drops).
24h post-surgery, a call was made to all patients to ask them about pain, use of rescue medication and the occurrence of any adverse reactions.
Blinding and randomizationThe trial was randomized, double blind, placebo controlled. Patients were randomly allocated to one of two groups: the intervention group (AL), received 20mL of bupivacaine 0.25% with epinephrine 1:400,000 in the Transversus Abdominis Plane ipsilateral to the hernia repair. The control group received 20mL of SSN 0.9%.
The mix used in the trial was prepared by the central sterile services of the Special Healthcare Services (SES) in a closed room and packed in 20mL syringes, with the same appearance and texture, code-labeled to retain the blind status of the trial.
All of the healthcare staff was blind to the type of substance administered.
The randomization was done by having an outsider not familiar with the design, implementation and evaluation of the trial flip a coin, and a link number was assigned between the patient and the study substance. This information was forwarded to the SES sterilization central and was saved on a sealed envelope until the time of analyzing the data.
TechniqueThe study substance was injected between the space of the anterior fascia of the transversus abdominis muscle and the posterior fascia of the internal oblique muscle under ultrasound guidance at 13mHz with a linear transducer (Logiq e GE) and a neuro-protected needle (50mm Braun Stimuplex) in plane. Three trained anesthesiologists visually confirmed the TAP, and the appropriate distribution of the study substance between the two muscles described.
Registry auditAll the information collected with the measurement instruments was matched against the medical records and confirmed with the patient when making the 24-h call.
Outcome variablesThe primary endpoint used to calculate the sample and design the trial was acute postoperative pain during the first 24h after surgery, evaluated using the verbal numerical scale.
The secondary endpoints were use of opiates and adverse reactions associated with the intervention (according to the opinion of the treating anesthesiologist).
InterviewsIn the course of the trial, the patients were interviewed on 4 occasions; first, when selected as potential participants when they were educated about the nature of the trial and those who accepted to participate filled the informed consent. This informed consent was sent to the registry to do the randomization and both the patient and the physician were blinded. The second time was on the day of surgery, when the socio-demographic and the clinical variables of each patient were recorded and once again the exclusion and inclusion criteria were reviewed. The third time was 1h after surgery, when the pain scores, opiate use and adverse reactions were recorded and once again to verify that no exclusion criteria were present. Finally, after 24h of surgery a new interview was made to confirm all the previously collected information and the patient was interviewed about pain, use of rescue doses and the presence of any adverse reactions.
Sample sizeThe sample size was estimated with a view to show the reduction in acute postoperative pain during the first hour – moderate, severe, mild – using an expected pain score of 6–7 in the numerical analog scale and a 2–3 points reduction with a variance of 1. The type 1 error was 0.05 and the type 2 error was 0.2. This resulted in a sample size of 40 and a 10% expected loss leading to a randomized sample size of 44.
Statistical methodsThe normal distribution pattern of the variables was analyzed using Kolmogorov–Smirnov test and the significance tests were done according to the characteristics of the variables, using both Chi square and Fisher's tests. The statistical package used was SPSS version 21.0. The baseline variables were analyzed with respect to the 2 randomized groups, looking for associations and the primary and secondary endpoints. Statistical significance was established at values below 0.05.
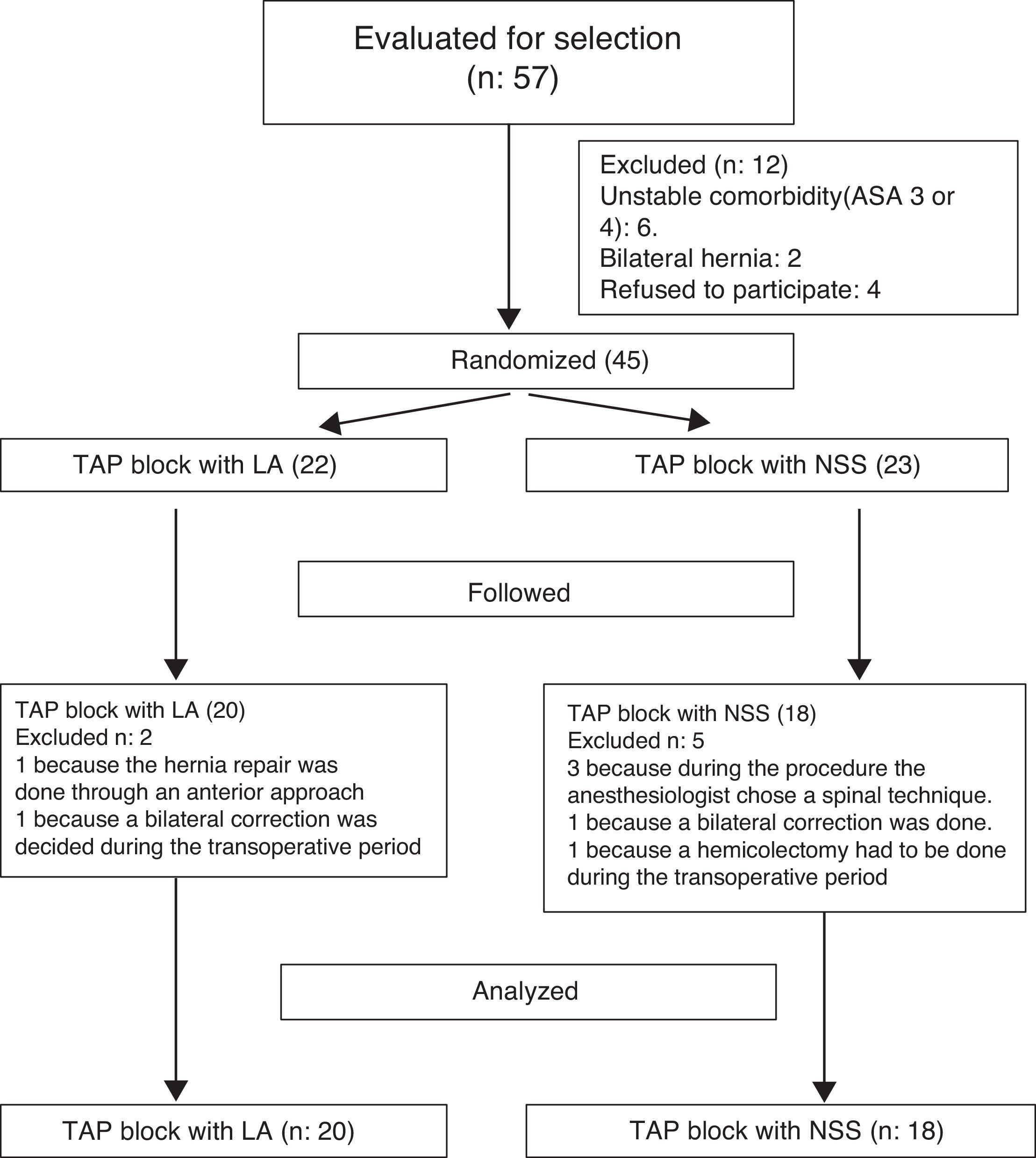
Results57 patients were chosen to participate in the trial, of which 12 had to be excluded for meeting any of the exclusion criteria. 45 patients were randomized and the final analysis was finally done on 38 patients due to follow-up failures and some intervention-related variations (1 patient had to undergo hemicolectomy and 2 patients received subarachnoid anesthesia) (Fig. 1).
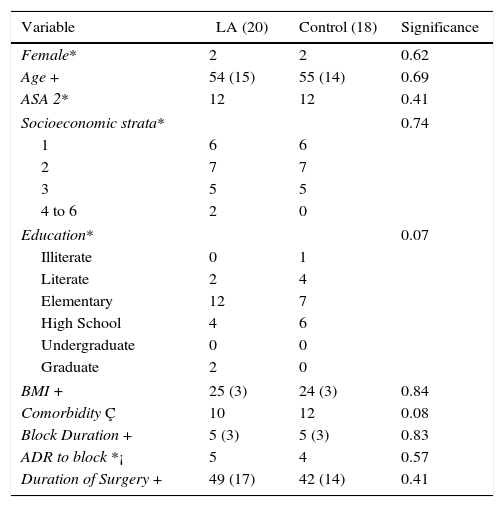
The baseline variables of the two groups analyzed were very similar, as shown in Table 1.
Group characteristics according to the baseline variables.
| Variable | LA (20) | Control (18) | Significance |
|---|---|---|---|
| Female* | 2 | 2 | 0.62 |
| Age + | 54 (15) | 55 (14) | 0.69 |
| ASA 2* | 12 | 12 | 0.41 |
| Socioeconomic strata* | 0.74 | ||
| 1 | 6 | 6 | |
| 2 | 7 | 7 | |
| 3 | 5 | 5 | |
| 4 to 6 | 2 | 0 | |
| Education* | 0.07 | ||
| Illiterate | 0 | 1 | |
| Literate | 2 | 4 | |
| Elementary | 12 | 7 | |
| High School | 4 | 6 | |
| Undergraduate | 0 | 0 | |
| Graduate | 2 | 0 | |
| BMI + | 25 (3) | 24 (3) | 0.84 |
| Comorbidity Ç | 10 | 12 | 0.08 |
| Block Duration + | 5 (3) | 5 (3) | 0.83 |
| ADR to block *¡ | 5 | 4 | 0.57 |
| Duration of Surgery + | 49 (17) | 42 (14) | 0.41 |
*Values Measured. + mean and standard deviation. Ç number of patients exhibiting any type of comorbidity. ¡ Patients that presented Adverse Drug Reactions to the block were classified by the attending anesthesiologist. LA: Local anesthetic.
Source: authors.
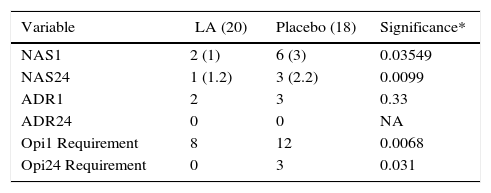
The acute postoperative pain during the first hour after surgery was lower in the intervention group (ANS of 2 with a standard deviation of 1 in the LA group and a ANS of 6m with a standard deviation of 2 in the NSS group) versus the control group, with statistical significance of 0.03. Furthermore, 24h after surgery although pain in both groups was mild, there was a significant statistical difference in pain intensity (see Table 2).
Primary and secondary results.
| Variable | LA (20) | Placebo (18) | Significance* |
|---|---|---|---|
| NAS1 | 2 (1) | 6 (3) | 0.03549 |
| NAS24 | 1 (1.2) | 3 (2.2) | 0.0099 |
| ADR1 | 2 | 3 | 0.33 |
| ADR24 | 0 | 0 | NA |
| Opi1 Requirement | 8 | 12 | 0.0068 |
| Opi24 Requirement | 0 | 3 | 0.031 |
NAS1: Numerical Analogue Scale one hour after surgery. NAS24: Numerical Analogue Scale 24 after surgery. ADR1: Adverse Drug Reaction one hour after surgery. ADR24: Adverse Drug Reaction 24 hours after surgery. Opi1: Opiate medications used during the first hour after surgery. Opi24: Opiate medications used in 24 hours after surgery. LA: Group of patients in whom local anesthetics were used. * Significance measured according to Chi2 or Fisher's Test.
Source: authors.
The number of patients requiring opiates during the first postoperative hour was more that half of the patients studied (52%), but was statistically significant higher in the control group with a P value of 0.0068.
Similarly, 24h after surgery, a larger number of patients required opiate-like rescue medication in the control group: 17 vs. 0%.
Overall, there were no significant differences in the occurrence of adverse reactions associated with the interventions between the two groups.
DiscussionThis trial may show the advantages of TAP Block to reduce acute postoperative pain 1h after mesh-based unilateral hernia repair with a pre-peritoneal approach, in contrast with the conventional, non-interventionist systemic analgesia technique, when administering 20mL of anesthetic solution directly between the anterior fascia of the transversus abdominus muscle and the posterior fascia of the internal oblique muscle using ultrasound guidance in the mid-axillary line between the iliac crest and the ipsilateral costal margin. This is compatible with the results of the papers by Sidiqui et al., who showed the benefits of this block for abdominal wall surgery.5 Ot is however very important to define the extent of this statement, since the intervention is subject to a large number of variables that may account for the contradictory findings of other authors that despite using ultrasound guidance failed to identify any difference between TAP block and placebo.9 Among the variables that could account for such differences is the fact that ultrasound is an operator-dependent technique,10 resulting in partial administration of the therapeutic substances on sites other than the expected areas, particularly in the case of TAP block.
Other variables include the site where the technique is used (subcostal, mid-axillary line, Petit's triangle),11 local anesthetic infusion rate, time of administration (before the incision or upon completion of the surgical procedure), type of local anesthetic used (ropivacaine, bupivacaine, other), time elapsed before evaluating pain (1, 2, 4, 6, 8, 24h post-surgery) and total volume of local anesthetic injected ç, all of which may account for the type of differences identified.12
Due to the difficulties in collecting the sample, some patients that could have contributed to enhance the power of this conclusion had to be excluded. Some of the particular difficulties included; the strict experimental design from the selection of patients according to the surgical approach used for the hernia repair (anterior vs. pre-peritoneal), the use of a mesh, the ASA classification (ASA III patients were excluded), and the anesthetic technique (exclusion of neuro-axial anesthesia). There were also some difficulties in terms of availability of patients to perform the surgery in the healthcare center planned (specifically due to the lack of continuity of healthcare services to the insurers: disruption in the relationship among the healthcare providers – IPS – and the Health Promoting Institutions – EPS –).
The reduction of acute postoperative pain at 24h is important because inguinal hernia repair is one of the procedures most frequently associated with persistent postoperative pain13 and management of acute pain is one of the factors involved in controlling such entity,14 but the mean reduction levels identified in our trial are within the mild range and hence may not be clinically relevant.
The lower use of opiates is quite evident both during the first hour and at 24h after surgery, affecting the quality of care of patients,15 the adverse drug-related reactions16 and time to discharge from the post-anesthesia care unit. Although associated adverse reactions failed to show significant differences, the use of a TAP block could shorten the hospital length of stay associated with the administration of analgesia during inguinal hernia repair surgery.17
ConclusionsOur trial shows the benefits of ultrasound-guided TAP block to reduce acute postoperative pain following unilateral hernia repair during the first hour and at 24h postop, with a decreased use of opiates by patients – though the need for opiates use is not totally abolished. This further emphasizes the idea already expressed by some authors that acute postoperative pain management in inguinal hernia repair must follow systemic and regional strategies.
Furthermore, the TAP block may reduce the discomfort in patients the first day after surgery and the need to use additional medication such as tramadol, for ambulatory pain management.
In this particular case, the TAP block seems to be a useful and simple strategy to administer regional techniques leading to optimized patient recovery when undergoing these procedures, keeping in mind that the effect may not be that clear, depending on the characteristics of the injection.18
Ethical disclosuresProtection of human and animal subjectsThe authors declare that the procedures followed were in accordance with the regulations of the responsible Clinical Research Ethics Committee and in accordance with those of the World Medical Association and the Helsinki Declaration.
Confidentiality of dataThe authors declare that no patient data appears in this article.
Right to privacy and informed consentThe authors must have obtained the informed consent of the patients and/or subjects mentioned in the article. The author for correspondence must be in possession of this document.
FundingOwn resources.
Conflict of interestNone.
Please cite this article as: Aguirre-Ospina OD, Gómez-Salgado JC, Chaverra D, Alzate M, Ríos-Medina ÁM. Bloqueo del plano transverso del abdomen en herniorrafia inguinal. Ensayo clínico controlado. Rev Colomb Anestesiol. 2017;45:159–165.
Registration number at Clinicaltrials.gov VIP 1691514.