The use of total intravenous anaesthesia (TIVA) has been growing worldwide over the past 20 years due to the creation of new drugs and the development of new target-controlled infusion pumps, many of which have already been approved in the United States by the FDA (Food and Drugs Administration), in Europe and in Colombia. However, the use of TIVA has not been expanded yet as part of routine practice.
ObjectiveTo determine the frequency of TIVA use in our country and to identify existing barriers for its implementation.
Materials and methodsSurvey designed to determine the use of TIVA in general anaesthesia practice in Colombia. A representative random sample of the universe of anaesthetists registered in the database of the Colombian Society of Anaesthesiology and Resuscitation (S.C.A.R.E.) was calculated. Reminders were sent by e-mail and some of the selected respondents were contacted by phone.
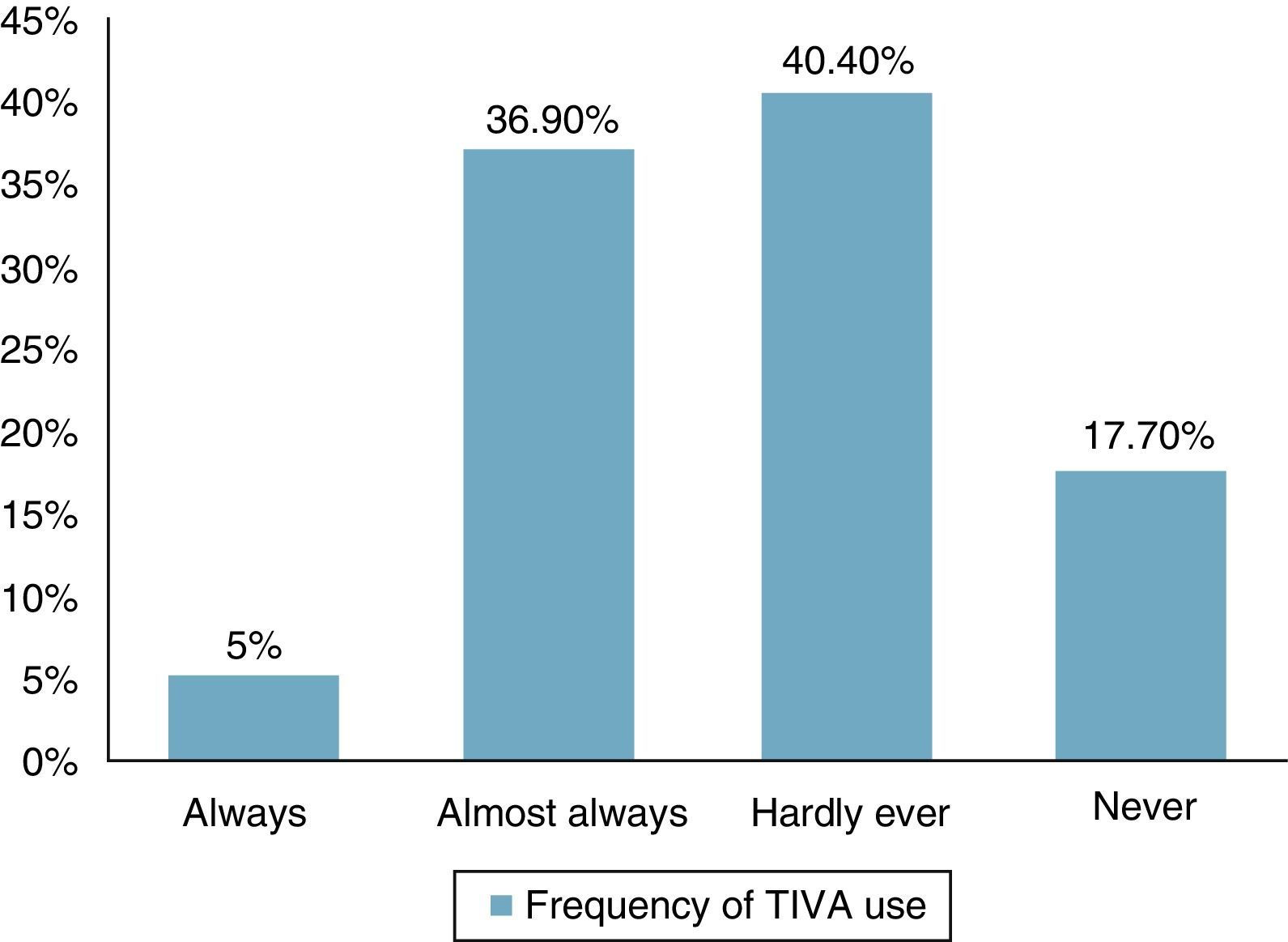
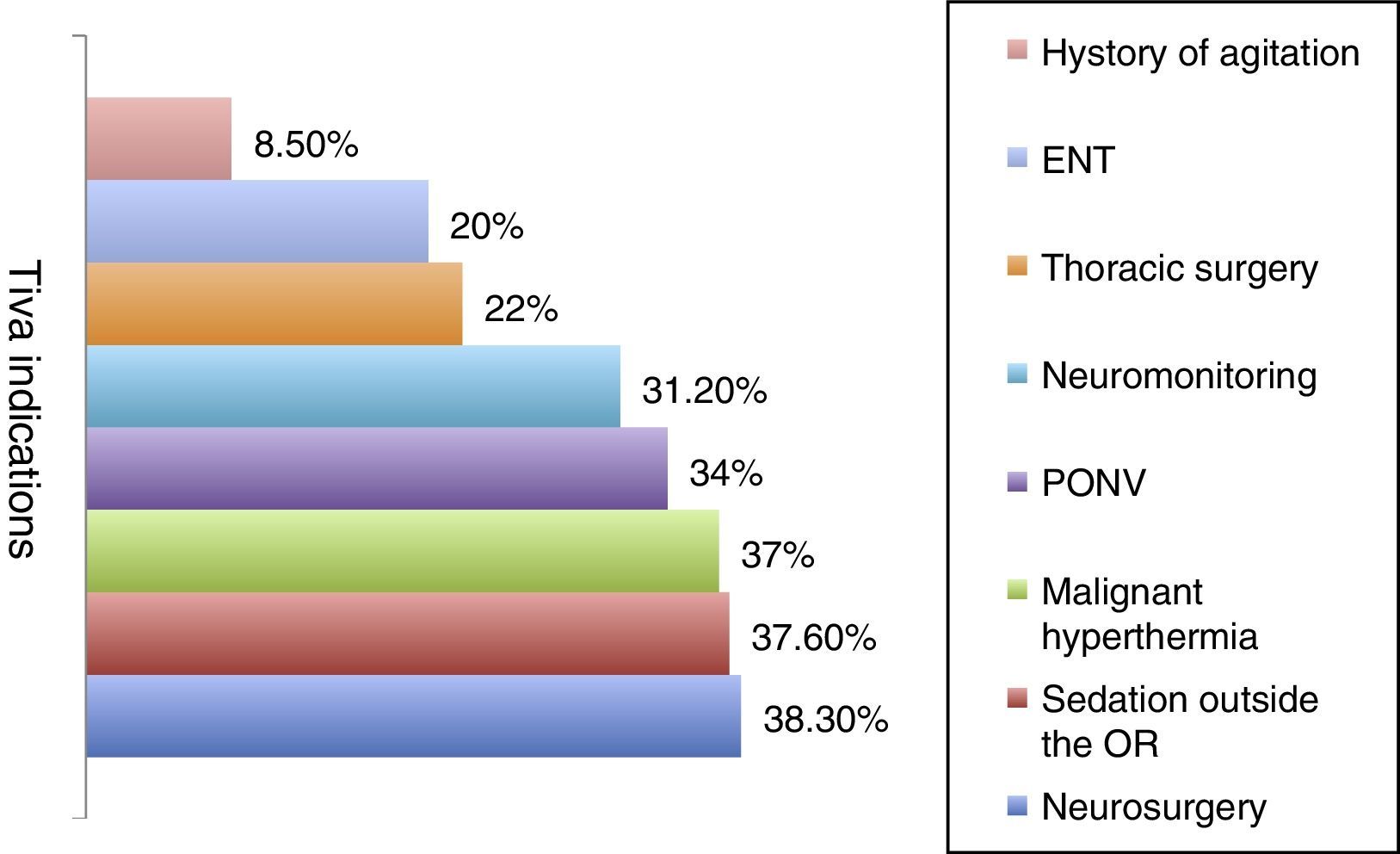
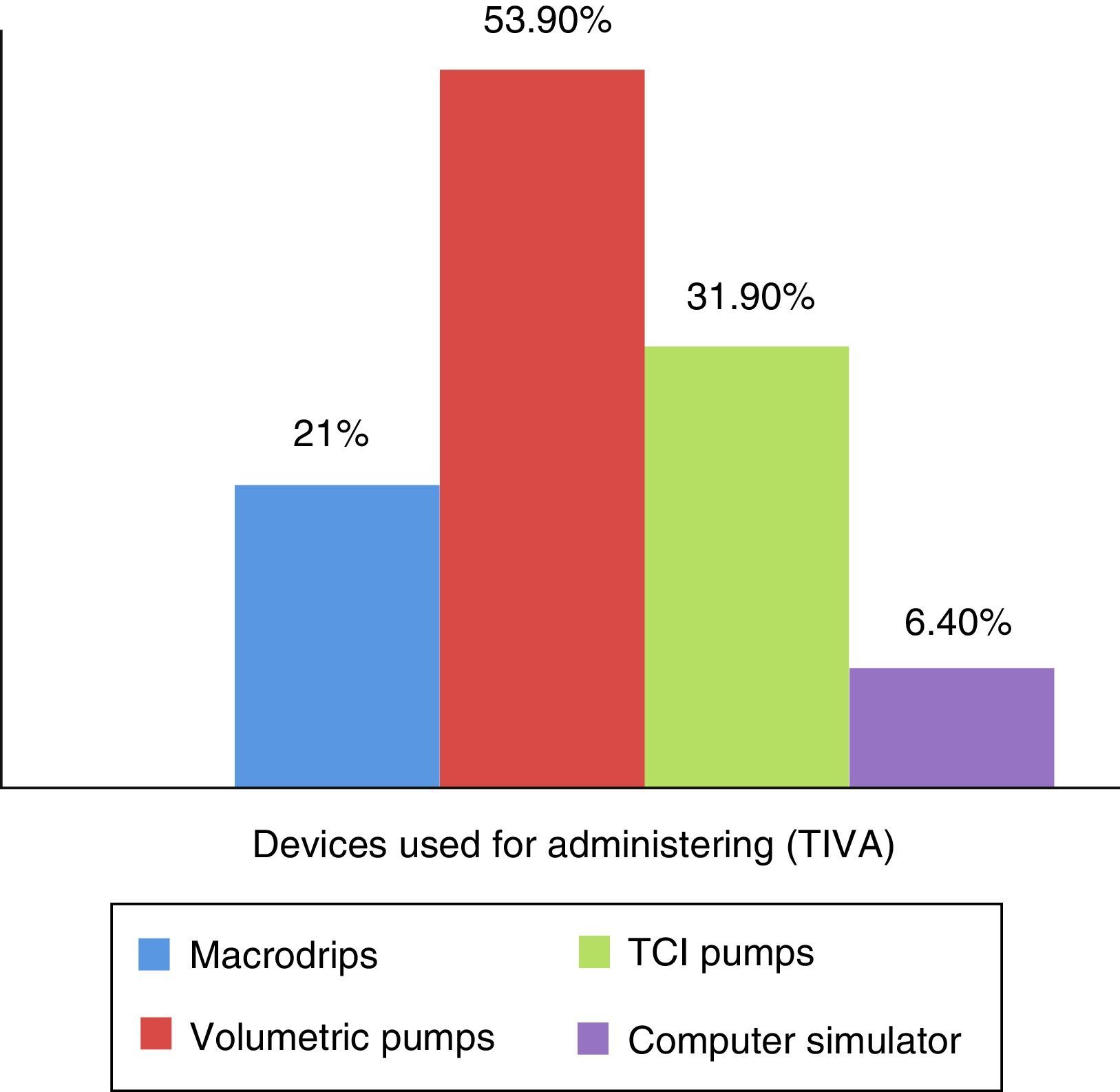
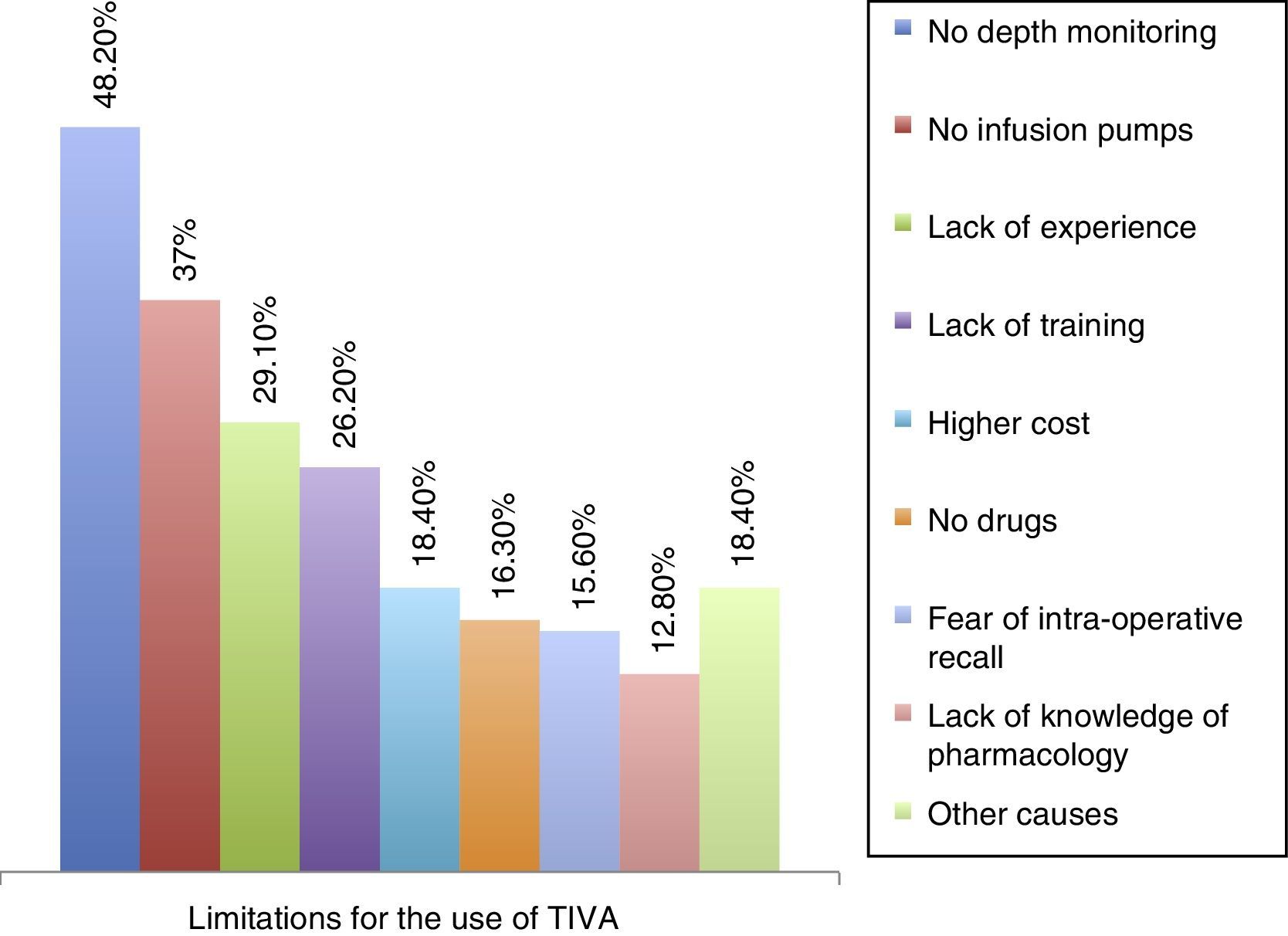
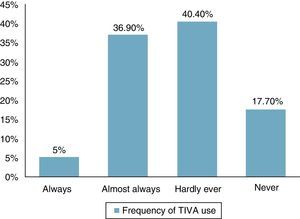
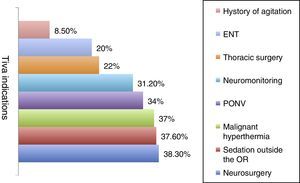
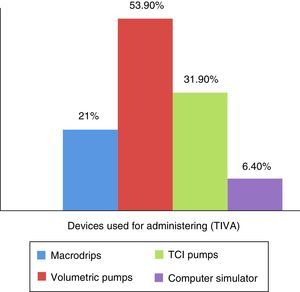
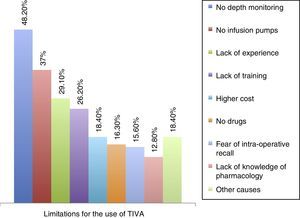
ResultsOverall, 141 (32.4%) responses were obtained. The frequency of TIVA use was reported as Always, 7 (5.0%), Almost Always, 52 (36.9%), Hardly Ever, 57 (40.4%) and Never, 25 (17.7%). The techology used for TIVA administration included macro drip devices (n=30, 21.3%), volumetric pumps (n=76, 53.9%), TCI pumps (n=45, 31.9%), and computer programmes (n=9, 6.4%). The limitations identified for the use of TIVA included low availability of anaesthesia depth monitoring (n=68, 48.2%) and infusion pumps (n=52, 36.9%), lack of experience (n=41, 29.1%), little availability of workshops (n=26, 18.4%), low availability of medications (n=23, 16.3%), fear of intra-operative recall (n=22, 15.6%), limited knowledge of pharmacology (n=18, 12.8%), increased anaesthesia time (n=13, 9.2%), and perceived difficulty for performing the technique (n=13, 9.2%).
ConclusionsThe use of TIVA has been limited by the low availability of technology, lack of experience or knowledge among anaesthetists, and a preference for the balanced anaesthesia technique. Many anaesthesiologists prefer balanced techniques for general anaesthesia. Some devices used for TIVA administration raise concerns about patient safety.
En los últimos 20 años el uso de la anestesia total endovenosa (TIVA) se ha expandido en todo el mundo debido a la creación de nuevos medicamentos y al desarrollo de nuevas bombas de infusión controladas por objetivo, muchas de las cuales ya han sido aprobadas por la Food and Drug Administration en USA, Europa y Colombia; sin embargo, el uso de TIVA aún no se ha expandiendo en la práctica rutinaria de la anestesia.
ObjetivoInvestigar la frecuencia del uso de TIVA en nuestro país y las limitaciones que actualmente existen.
Materiales y métodosSe diseño una encuesta para determinar el uso de la TIVA en Colombia. Se calculó una muestra aleatoria representativa de los anestesiólogos registrados en la Sociedad Colombiana de Anestesiología. Se enviaron recordatorios por correo electrónico y algunos anestesiólogos seleccionados se contactaron por vía telefónica.
ResultadosSe obtuvieron 141 (32,4%) respuestas. La frecuencia del uso de TIVA fue reportada así: Siempre 7 (5,0%), casi siempre 52 (36,9%), casi siempre 57 (40,4%) y nunca 25(17,7%). La tecnología implementada para la administración de TIVA incluyó equipos de macro goteo (n=30: 21,3%), bombas volumétricas (n=76; 53,9%), bombas de TCI (n=45; 31,9%) y programas de computador (n=9; 6,4%). Las principales limitaciones para el uso de TIVA fueron la poca monitorización de la profundidad anestésica (n=68; 48,2%) y de bombas de infusión (n=52; 36,9%), falta de experiencia (n=41; 29,1%), poca disponibilidad de talleres (n=26; 18,4%), poca disponibilidad de medicamentos (n=23; 16.3%), temor al recordar intraoperatorio (n=22; 15,6%), conocimiento limitado sobre farmacología (n=18; 12.8%), incremento en el tiempo de anestesia (n=13; 9,2%), y la dificultad percibida de desarrollar la técnica (n=13; 9,2%).
ConclusionesEl uso de TIVA se ha limitado por la poca disponibilidad de tecnología, falta de experiencia, y por que se prefiere la técnica balanceada para la anestesia. Algunos dispositivos usados para la administración de TIVA pueden comprometer la seguridad del paciente.
According to the records of the United States National Medical Library, the first publications on the use of total intravenous anaesthesia (TIVA) came out in the 1970s. Since then, the number of publications has grown year after year, from 20 to 200 in the last decade,1 bringing to light the benefits of the use of TIVA as compared to other general anaesthesia techniques.
Compared with balanced anaesthesia that uses inhaled anaesthetics through specialised gas delivery systems, TIVA offers clear advantages, including the absence of contamination, negligible cardiovascular depression, low neurohumoral response, reduced oxygen consumption, lower incidence of postoperative nausea and vomiting, early and predictable recovery leading to earlier discharge in outpatient surgery, and less postoperative agitation in high risk patients.2,3 Moreover, TIVA does not require a sophisticated device for delivering anaesthetic gases or waste gas extraction systems.4,5 Compared with regional anaesthesia, the only prerequisite for TIVA is the availability of a safe venous line; it takes less time than regional or neuroaxial techniques, and it entails no risk of failed blocks or unpredictable duration of the anaesthesia.6
Despite all these benefits, current anaesthesia practice is still dominated by balanced anaesthesia, which combines the use of inhaled agents with intravenous opioids. The choice of one technique over another depends on the anaesthetist's personal experience, patient variables and the availability of supplies and equipment in the work setting.7 Some of the limitations reported in the literature regarding the use of TIVA include the lack of devices such as infusion pumps in the work place, costs, the unavailability of adequate and safe intravenous drugs, the difficulty in determining the anaesthetic plane, and the lack of education and training for performing the technique.8,9
The main objective of this study was to determine the use of total intravenous anaesthesia in the clinical practice in Colombia during the year 2015–2016.
Materials and methodsCross-sectional cohort study using an on-line questionnaire sent out to a group of active anaesthetists practicing in Colombia taken from the database of the Colombian society of Anaesthesiology and Resuscitation (S.C.A.R.E) from September 1, 2015 to February 1, 2016. In order to optimise the response rate, the survey was developed on the basis of 6 specific questions on the use of TIVA in anaesthesia, requiring less than 5min to complete. Follow-up phone calls were used to contact the anaesthetists who did not respond to the initial on-line survey, in order to increase the number of responses.
A representative sample of active anaesthetists in Colombia was calculated from the number registered in the SCARE database, and a random selection was made. Anaesthetists who were not actively practicing their profession at the time of the survey were excluded. All the participants agreed to respond to the survey voluntarily and freely and accepted the informed consent used to introduce the survey. The forms were sent by e-mail over the “encuestafacil.com” platform. The questionnaire was sent twice by e-mail and the authors contacted non-responders by telephone in order to increase the number of fully completed responses. The respondents did not receive any form of financial or material incentive to participate. The project was submitted to and approved by the Research Ethics Committee of SCARE, as recorded in Minutes N CE201508 of July 28, 2015. The final manuscript was drafted following the recommendations contained in CHERRIES and in the good practice guidelines for publishing surveys.10,11
Statistical analysisA representative sample was calculated for estimating proportions using a simple random non-replacement method in finite populations in Excel, and random selection was performed using the negative coordinated method in Excel.
A sample of 434 participants was calculated, with a 95% reliability and approximate error of 0.05, out of a universe of 2573 anaesthetists registered in the S.C.A.R.E. database. Response numbers and their proportions were used for the description of categorical items. Only fully completed questionnaires were analysed.
ResultsOf the 434 randomly selected anaesthetists, 141 (32.48%) responded the questionnaire, 110 over the web, and 31 by telephone. The frequency of TIVA use was defined as follows: Always, 100% of patients; Almost Always, 50–99% of patients; Hardly Ever, less than 50%; and Never, 0% of cases. The frequency use of the TIVA technique is described in Fig. 1, and it was found that it is used always and almost always by 41.9% of the respondents. The main indications considered by the participants for the use of TIVA were neurosurgery (38.3%), sedation outside the operating room (37.6%), and risk of malignant hyperthermia (36.9%). All other indications were less frequent and are described in Fig. 2. For the question on the use of devices for the administration of intravenous drugs, it was found that TIVA is given mainly with volumetric pumps (53.9%) and TCI (31.9%) pumps. The use of other devices is shown in Fig. 3.
Of the respondents, 60% consider that TCI pumps are absolutely necessary for TIVA administration, while 73% also consider the availability of anaesthetic depth monitoring like BIS or entropy as a pre-requisite for using this anaesthesia technique. Of the respondents, 120 (85.1%) reported having received training in the use of TIVA and 57 (40.4%) reported having TCI pumps available at their work places. The surveyed anaesthetists found that little availability of anaesthesia depth monitoring (48.2%), the lack of infusion pumps (36.9%) and the lack of experience with the technique (29.1%) were the main limitations for the use of TIVA; other limitations are described in Fig. 4.
The scant availability of technology to support TIVA administration and/or monitoring of the depth of anaesthesia are important limitations to the use of this anaesthetic technique because devices like TCI pumps, BIS monitors or entropy increase the safety of the technique. Additionally, the respondents reported that balanced techniques are easier to perform and they are more familiar with this technique when compared with total intravenous anaesthesia.
DiscussionDespite the worldwide expansion of intravenous anaesthesia over the past 20 years, supported by the creation of new drugs with an improved pharmacokinetic profile, the pace of TIVA development varies among the different regions of the world, particularly where financial resources are limited. The aim of this study was to examine the use of total intravenous anaesthesia in our country, the main indications and the limitations identified by the respondents for the adoption of this type of anaesthesia technique. It is the first study of its kind conducted in our country.
Of the total representative sample, the response rate was 32%. The survey showed that total intravenous anaesthesia is used always 5% of the time and almost always 37% of the time. It is interesting to note that anaesthetists in Colombia are familiar with total intravenous anaesthesia techniques due to the availability of hypnotic agents that are predictable, easy to titrate and have a clear pharmacokinetic profile. This has popularised this type of anaesthetic technique among almost half of the anaesthetists surveyed.12,13
Many advantages of the intravenous anaesthesia technique have been described and, at present, there are clear recommendations and indications for the use of TIVA both in paediatric as well as adult patients.14 However, this survey found that the main indications for which the respondents consider the administration of TIVA are neurosurgery (66%), sedation outside the operating room (37.6%), risk of malignant hyperthermia (36.9%) and, less frequently, a history of postoperative nausea and vomiting, intra-operative neurophysiological monitoring, thoracic surgery, otolaryngological surgery, and patients with a history of postoperative delirium or agitation, all of which are described in the literature as indications for administering TIVA.14
There are various methods for the administration of total intravenous anaesthesia, including sophisticated infusion pumps based on effector site concentration control known as target controlled infusion (TCI), or plasmatic controlled infusion (PCI) pumps; volumetric pumps based on simulators that use pharmacokinetic models to calculate individualised doses for each patient15; and manual infusion techniques for a simpler form of TIVA administration that do not required additional devices or technologies. These manual techniques use fixed weight-based concentrations and allow to vary the dose over time in accordance with the needs of the patient or the surgery. These manual infusions may be combined with different pharmacokinetic models in order to estimate effector site concentration. Many of these systems are available for use in our country by means of electronic devices like smart phones, and there are reports of excellent clinical performance for remifentanil and propofol infusions using mathematical algorithms designed to calculate effector site concentration.16 This study revealed that anaesthetists use mainly volumetric pumps for TIVA administration (53.9%), followed less frequently by TCI pumps (31.9%), macrodrip devices (21.3%), and pharmacokinetic software (6.4%). However, 60% of the respondents believe that TCI pumps are a prerequisite for administering total intravenous anaesthesia as is also the case for the ability to monitor depth of anaesthesia with the help of devices like BIS (bi-spectral analysis) or entropy in order to perform the technique safely and have the ability to predict the state of hypnosis in each patient.13
Regarding training and education in intravenous anaesthesia, 120 respondents (85.1%) reported having received some form of education on the technique. This is striking considering that the technique is not generally taught during anaesthesia training. A significant proportion of TIVA education is obtained outside the residence programme, especially through courses taught during congresses, self-learning and the support of peers at work. This appears to be related to the importance that anaesthetists attach to the need to develop knowledge and skills in the use of the technique, prompting them to find other non formal sources of education.
Finally, the main limitations identified in the group of respondents which discourage the use of total intravenous anaesthesia in routine practice include the lack of monitoring of the depth of anaesthesia, the lack of infusion pumps, the lack of expertise in the use of TIVA, the absence of training workshops or practice settings, the prevailing perception that TIVA increases the cost of anaesthesia, the little availability of drugs, the fear of intra-operative recall, little knowledge of drug pharmacology as recognised by some anaesthetists, and finally, the perception of difficulty and lack of confidence to perform this type of technique. Besides these reasons, some anaesthetists reported their preference for balanced techniques combining an inhaled anaesthetic with the intravenous infusion of an opioid. This is so because many practitioners are more familiar with this type of anaesthesia and prefer not to innovate.
It is interesting to note that many anaesthetists believe that the use of total intravenous anaesthesia requires costly technology hardly available in our setting. They reported on the absolute need to have TCI pumps and monitoring of the depth of anaesthesia as prerequisites for administering intravenous anaesthesia. However, it has been shown that manual infusion techniques are as effective and reliable as techniques that use TCI pumps, and provide similar anaesthesia quality and no events of intra-operative recall.15 A survey conducted in the United Kingdom revealed that only 38% of the anaesthetists used TCI pumps, despite their being readily available.17
A similar study was conducted in Brazil in 2006 to assess the use of TIVA by means of a survey sent to 150 anaesthetists and 102 residents. The aim of the study was to assess “attitudes” of the respondents towards the technique. The positive factors that supported the use of TIVA were the quality of awakening and the prospect of future development of more drugs suitable for this technique.8,18 Likewise, the respondents reported a desire to learn and perform total intravenous anaesthesia techniques in their routine practice. They also reported that the availability of BIS monitoring for the depth of anaesthesia would increase the use of TIVA.
Notwithstanding the availability of all these devices, it is important to gain adequate knowledge of pharmacology and pharmacokinetics as the scientific basis for performing the technique safely and predictably,16 and also as the basis for new research in the area and for the future development of new technologies and pharmacokinetic models.19
LimitationsThe limitations of the study have to do with the implementation of the survey, the low percentage of responses and the way each participant interprets the questions. Consequently, results cannot be generalised to the practice of anaesthesia in Colombia. The use of a phone call by the authors in order to increase the number of responses may represent a bias in data collection because some of the interviewees may have felt intimidated or obliged to mark a particular answer. Survey-type studies in general have limitations because of the low percentage of responses and the interpretation and interest attached by each participant to the questions.
ConclusionsThis study leads the authors to conclude that TIVA is a technique available to most anaesthetists in Colombia, although there is still some confusion regarding indications for its administration. Despite the fact that the majority of the respondents reported having received education on the use of TIVA, results point to the fact that there are misconceptions about the theory and the practical applications, added to the limited availability of the technology. This has had a negative impact on the regular use of TIVA in our setting. Some of the devices used for TIVA administration are a source of concern, as is the case of macrodrip system that may be unpredictable and have a negative effect on patient safety.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
FundingAuthors’ own resources.
Conflict of interestNone to disclose. Doctors Echeverry-Marín, Vanegas-Saavedra and Leguizamón are afiliated to S.C.A.R.E.
Opinons showed in this paper own to the authors and do not reflect the S.C.A.R.E.’s ones.
Please cite this article as: Echeverry-Marín PC, Arévalo J, Pinzón P, Vanegas-Saavedra A, Leguízamon M. Uso de la Anestesia Total Intravenosa en Colombia: encuesta nacional dirigida a anestesiólogos activos en Colombia. Rev Colomb Anestesiol. 2017;45:122–127.