Stress has been associated with acute heart failure syndrome, with significant morbidity and mortality.
MethodologyCase report and non-systematic review of relevant literature.
Case reportA 65-year-old woman with a history of untreated generalised anxiety disorder who, after the violent death of a child, suffered oppressive pain in the precordium, neck and upper left limb that lasted more than 30min; the initial clinical suspicion was acute coronary syndrome.
Literature reviewTakotsubo cardiomyopathy is characterised by left ventricular dysfunction, reversible in most cases, and altered ventricular wall motion in the absence of coronary abnormalities, associated with high plasma concentrations of catecholamines, which in most cases coincide with an acute physical or emotional stressor.
ConclusionsTakotsubo cardiomyopathy is a differential diagnosis that physicians treating patients with suspected coronary syndrome should consider, especially in postmenopausal women with a history of psychiatric comorbidities such as generalised anxiety disorder.
El estrés se ha asociado con un síndrome de insuficiencia cardiaca aguda, con morbilidad y mortalidad importantes.
MetodologíaReporte de caso y revisión no sistemática de la literatura relevante.
Presentación del casoMujer de 65 años con antecedente de trastorno de ansiedad generalizada no tratado que, tras la muerte violenta de un hijo, sufría dolor opresivo en el precordio, el cuello y la extremidad superior izquierda que duraba más de 30min; la sospecha clínica inicial fue síndrome coronario agudo.
Revisión de la literaturaLa miocardiopatía de tako-tsubo se caracteriza por disfunción ventricular izquierda, reversible en la mayoría de los casos, y alteraciones del movimiento de la pared ventricular sin anormalidades coronarias, asociado a altas concentraciones plasmáticas de catecolaminas, que en la mayoría de los casos coinciden con un estresor agudo de tipo físico o emocional.
ConclusionesLa miocardiopatía de tako-tsubo es un diagnóstico diferencial que los médicos que atienden a pacientes con sospecha de síndrome coronario deben considerar, especialmente ante mujeres posmenopáusicas con antecedentes de comorbilidades psiquiátricas como el trastorno de ansiedad generalizada.
Takotsubo cardiomyopathy, is usually an acute, reversible disease that is easily confused with acute coronary syndrome.1 It is characterised by reduced left ventricular ejection fraction associated with abnormal ventricular wall motion patterns. It usually presents in the context of a physical or psychological stressor,2 and 90% of cases occur in women, mainly postmenopausal.3 This cardiomyopathy is found in 1–3% of all patients with suspected coronary syndrome, and 6–9% if only women are considered.1 Studies have reported that patients with takotsubo cardiomyopathy are more likely to present generalised anxiety disorder or a family history of psychiatric disorders compared to the general population.4 Although this disease is typically brought on by negative stressful events, it has recently been associated with positive emotions.5
The aim of this article is to report the case of a woman with takotsubo cardiomyopathy associated with acute stress.
MethodsCase report and non-systematic review of relevant literature. The patient was treated in the emergency department of a private clinic specialising in highly complex cardiovascular diseases in Medellín (Colombia).
Informed consent was obtained from the patient after clearly explaining that her clinical information would be used for academic purposes, and she was ensured of the confidentiality of her data.
The study was conducted according to the guidelines of the Belmont report6 and the Declaration of Helsinki.7 The literature search was performed on MEDLINE and Google Scholar. Meta-analyses, systematic reviews and case reports published in English and Spanish, with no time limits, were included. The search criterion was: “Takotsubo cardiomyopathy”.
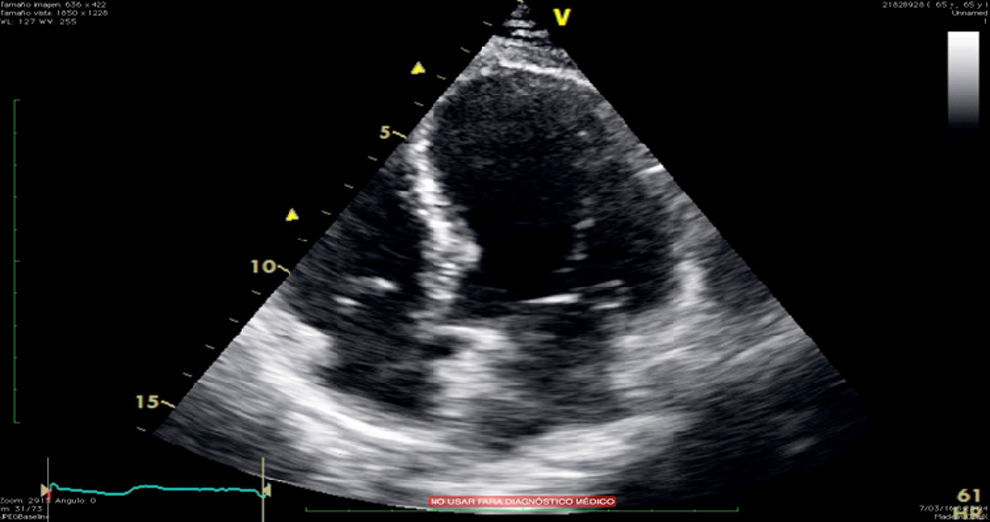
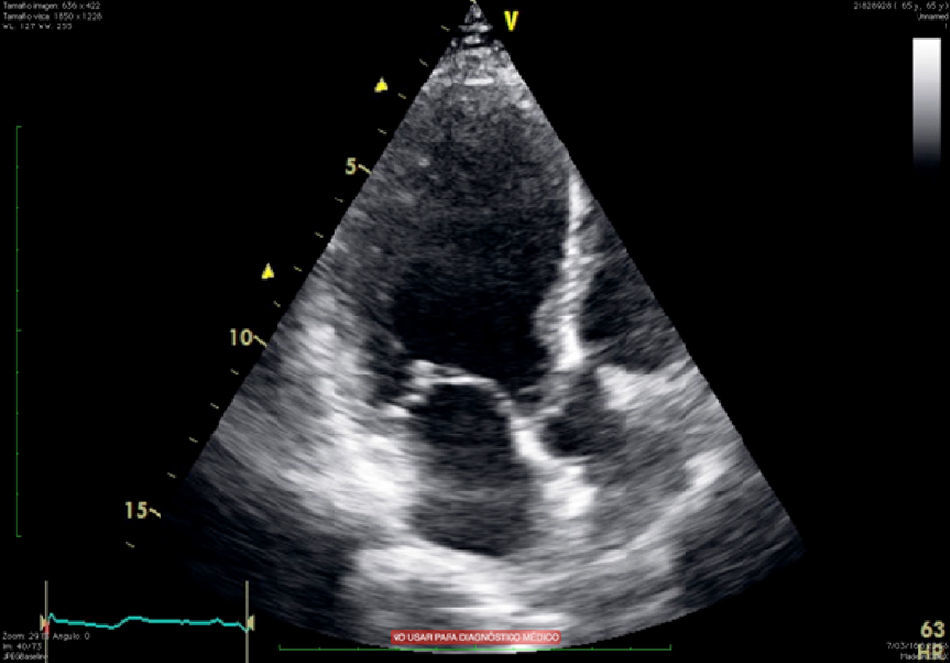
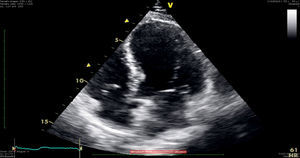
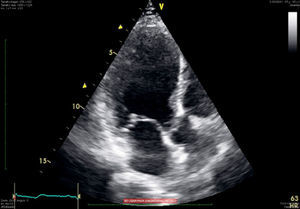
Presentation of the caseA 65-year-old woman with a history of high blood pressure and dyslipidaemia. She presented at the emergency department with precordial pain radiating to the neck and ipsilateral upper extremity, which began after the violent death of her son and lasted more than 30min. The emergency department diagnosed the symptoms as an acute coronary syndrome. At admission to the emergency department, the patient's vital signs were: blood pressure, 116/68mmHg; heart rate, 68bpm; respiratory rate, 18rpm and oxygen saturation, 96%. The physical examination was within normal limits. An electrocardiogram showed T-wave inversion on the inferior wall, with no other changes, and troponin levels of 2.19ng/ml (Table 1). Treatment was started for a diagnosis of acute myocardial infarction without ST segment elevation. After performing risk stratification, we decided on a prompt invasive strategy. Transthoracic echocardiography showed abnormal diastolic function due to type I relaxation impairment, with an ejection fraction of 35%, together with left ventricular apical akinesis causing the “ballooning” shown in the echocardiographic image of the left ventricle during systole (Figs. 1 and 2). The coronary angiography was normal.
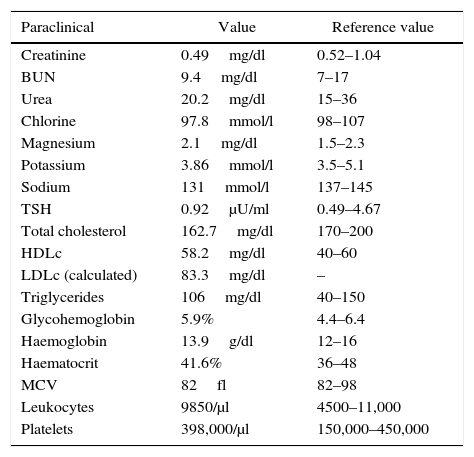
Laboratory tests.
| Paraclinical | Value | Reference value |
|---|---|---|
| Creatinine | 0.49mg/dl | 0.52–1.04 |
| BUN | 9.4mg/dl | 7–17 |
| Urea | 20.2mg/dl | 15–36 |
| Chlorine | 97.8mmol/l | 98–107 |
| Magnesium | 2.1mg/dl | 1.5–2.3 |
| Potassium | 3.86mmol/l | 3.5–5.1 |
| Sodium | 131mmol/l | 137–145 |
| TSH | 0.92μU/ml | 0.49–4.67 |
| Total cholesterol | 162.7mg/dl | 170–200 |
| HDLc | 58.2mg/dl | 40–60 |
| LDLc (calculated) | 83.3mg/dl | – |
| Triglycerides | 106mg/dl | 40–150 |
| Glycohemoglobin | 5.9% | 4.4–6.4 |
| Haemoglobin | 13.9g/dl | 12–16 |
| Haematocrit | 41.6% | 36–48 |
| MCV | 82fl | 82–98 |
| Leukocytes | 9850/μl | 4500–11,000 |
| Platelets | 398,000/μl | 150,000–450,000 |
Liaison psychiatry evaluated the patient by means of an unstructured psychiatric interview, that found a sad patient who cried throughout the interview. She described in detail the violent death of her son two days previously. He had been in a bar with his girlfriend when he was attacked and stabbed in the chest by a stranger, and died almost immediately. The patient, upon hearing the news, was overcome by deep sadness, crying and anxiety, and could not stop thinking about her dead son. Because of the autopsy, the mother was only allowed to view her son's body one day after the murder, during the wake, when she asked for the coffin to be opened so that she could “say goodbye”. In the patient's own words: “[at that moment] I felt a great pain... in my soul and immediately began to feel a pain in my chest and arm, and I was rushed to A&E”.
The patient described herself as a “nervous” person who worries a lot, often imagining the worst outcomes, such as when her son would go out on Saturdays and she worried that he would get into a fight and “get into trouble”. This caused heart palpitations, a feeling of suffocation and great anxiety. According to her family, these symptoms were troublesome, but the patient had never sought medical or psychological advice.
Another negative life event involved the murder of the patient's husband 20 years earlier at the hands of her brother. At that time, she also experienced precordial pain as soon as she heard the news. She was ill for several days, but did not seek medical advice.
The mental status examination showed an alert patient, orientated to time and place, attentive, who made eye contact, and showed a depressed and anxious emotional state. Language was normal. Thoughts were coherent and logical. She expressed depressive and anxious ideas related to the violent death of her son. She showed no sensory/perceptual or memory alterations, good judgement and limited future focus.
The patient is considered to meet the DSM-5 criteria for baseline generalised anxiety disorder (excessive worry about future events throughout her life, which is beyond her control and is associated with restlessness, feeling constantly on edge, cannot stop thinking, muscle tension and difficulty sleeping) and acute stress disorder (exposure to violent death of her son, intrusive thoughts of her son's face in the coffin, nightmares, great psychological distress, inability to remember what happened, general insomnia, hyporexia, inability to concentrate and constant edginess). These symptoms began immediately after receiving the news of the death of her son, and were exacerbated when she saw his body; the symptoms lasted for five days. The psychiatrist started treatment with clonazepam 0.5mg/day.
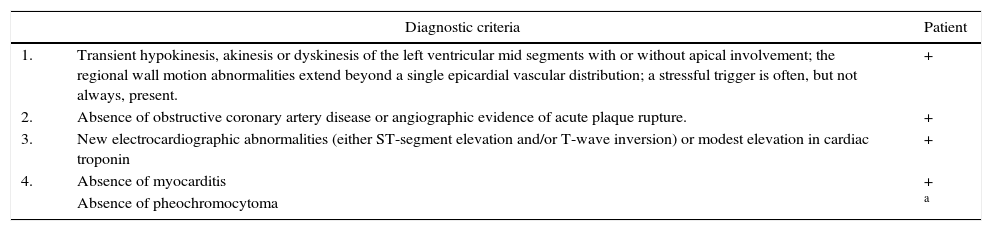
Due to altered ventricular wall contraction, slightly elevated troponin levels, electrocardiographic abnormalities, normal coronary angiography, presence of emotional stress, absence of clinical findings of myocarditis, cerebrovascular events, and cocaine use, a diagnosis of takotsubo cardiomyopathy was made. Although no specific tests were performed to rule out pheochromocytoma or myocarditis, as required by Mayo Clinic criteria (Table 2), there were no other clinical findings in the patient that raised a suspicion of this diagnosis. The patient made good progress. She tolerated initiation of cardiac rehabilitation with no precordial pain or haemodynamic alterations, and was discharged on the third day of hospitalisation, with a medical prescription for enalapril 20mg/12h, metoprolol 25mg/12h, atorvastatin 40mg/day, omeprazole 20mg/day, clonazepam 2 drops/8h, trazodone 50mg/night and sertraline 50mg/day; she was given an appointment for follow-up transthoracic echocardiography in the cardiology department at 1 month, and an appointment for follow-up psychiatry.
Diagnostic criteria for takotsubo cardiomyopathy. Mayo Clinic, 2008.
| Diagnostic criteria | Patient | |
|---|---|---|
| 1. | Transient hypokinesis, akinesis or dyskinesis of the left ventricular mid segments with or without apical involvement; the regional wall motion abnormalities extend beyond a single epicardial vascular distribution; a stressful trigger is often, but not always, present. | + |
| 2. | Absence of obstructive coronary artery disease or angiographic evidence of acute plaque rupture. | + |
| 3. | New electrocardiographic abnormalities (either ST-segment elevation and/or T-wave inversion) or modest elevation in cardiac troponin | + |
| 4. | Absence of myocarditis | + |
| Absence of pheochromocytoma | a | |
Taken and modified from Prasad et al.17
In 1990, Sato et al.8 described five clinical cases with manifestations of acute coronary syndrome, with no findings of coronary disease, and with transient left ventricular apical akinesis. Takotsubo is the name of a Japanese octopus trap, and was first used by Sato et al. to describe this condition due to its resemblance to the left ventricular image during systole of these patients (Fig. 3).
Takotsubo cardiomyopathy is a disease triggered by physical or emotional stress,2 and is characterised by reversible left ventricular dysfunction, and wall motion abnormalities, typically hypokinesia in the apical segment and hyperkinesia in the basal segments that causes the characteristic apical ballooning1,9 (Figs. 1 and 2), that extend beyond the territory of a coronary artery.10
PathophysiologyElevated catecholamines have been shown to play a key role in the pathophysiology of this entity, but the mechanism is unclear.1–3,9 Several theories have been proposed, such as the epinephrine-mediated activation of the β2-adrenoreceptor which in turn couples to inhibitory G-proteins and shuts down the contractile activity of the heart.9 Coronary microvascular dysfunction, coronary artery spasm and left ventricular outflow tract obstruction cause an imbalance between oxygen supply and demand, thus causing the affected cells to shut down.3,9
Oestrogens are a protective factor against cardiovascular disease because they inhibit myofibroblast differentiation, regulate the effect of epinephrine on the cardiac presynaptic nerves, and attenuate catecholamine- and glucocorticoid-mediated stress response.3,12–14 Takotsubo cardiomyopathy is more prevalent in postmenopausal women, probably due to oestrogen depletion occurring at this stage.3
EpidemiologyTakotsubo cardiomyopathy is an entity with a strong preference for the female sex (86% of cases compared to only 14% in men).11 Age is also an important factor in this disease, since 79.1% of those affected are over 50 years of age.2
A recent meta-analysis identified the presence of an emotional stressor in 39% of cases, a physical stressor in 35% and no detectable stressors in 17% of patients.11
An association has been found between takotsubo cardiomyopathy and neurological (7%) and psychiatric (24%) disorders, among which anxiety disorders (13%), mood alterations (9%) and delirium or dementia (2%) predominate.11 According to one of the mechanisms put forward to explain this association, anxious patients are subjected to constant chronic psychological stress that, in a situation of acute stress, triggers the syndrome. Stress-related mechanisms that may promote myocardial dysfunction include activation of the hypothalamic-pituitary-adrenal axis and the sympathetic nervous system, serotonergic dysfunction, secretion of proinflammatory cytokines and platelet activation. Some studies have also suggested that the presence of psychosocial factors, such as a family history of depression and anxiety or social isolation, play an important role in the onset of this disease.4
Clinical presentationBetween 1% and 9% of patients with signs or symptoms of acute myocardial infarction actually present takotsubo cardiomyopathy.1 In the acute phase of the disease, the clinical presentation, electrocardiographic findings and biomarker profiles are often similar to those of an acute coronary syndrome.8
There is chest pain in up to 55% of cases; troponins are elevated by 15–100%; 53% of patients present ST segment changes, and 49% present changes in the Q- and T-waves.11
In a study of 1750 patients, the predominant symptoms at admission were chest pain (75.9%), dyspnoea (46.9%) and syncope (7.7%).2 Manifestations such as hypotension, palpitations, pulmonary oedema, ventricular arrhythmias, cardiogenic shock and cardiac arrest were less common.8
DiagnosisTo date, there is no universally accepted diagnostic strategy for this disease, so different authors have proposed their own diagnostic criteria.15 The first to do so were a group of researchers from the Mayo Clinic in 2004. The same group later updated their recommendations in 2008, and these latest criteria are the most widely used today.8,16,17 For diagnosis, the 4 proposed criteria must be fulfilled (Table 2).
The main challenge in diagnosing takotsubo cardiomyopathy is differentiating it from acute coronary syndrome. This can be achieved by using electrocardiography, cardiac enzymes test, echocardiography or cardiac magnetic resonance imaging, with coronary angiography and left ventriculography being the gold standard.10 Other diseases that should be ruled out are: pheochromocytoma, cocaine intoxication, myocarditis and cerebrovascular disease.8,18
TreatmentNo randomised studies or expert consensus statements on the management of this disease have yet been published, so recommendations are based on the pathophysiology and the natural course of the disease.19 While awaiting test results to rule out takotsubo cardiomyopathy, patients should receive the treatment recommended for acute coronary syndrome.8 If the patient does not present cardiogenic shock, beta blockers and angiotensin converting enzyme inhibitors are used, since they block and modulate (respectively) the response to excess catecholamines; anxiolytics should be administered to treat the underlying cause. However, if the patient presents with cardiogenic shock, intra-aortic balloon pumps, intravenous fluids, inotropes or beta-blockers may be used.19 In patients with intraventricular thrombi in whom half of the thrombi are not evident during initial diagnostic imaging, the risk of cardioembolic complications is estimated at 33%. Therefore, it is advisable to administer anticoagulants in all patients while the ventricular akinesis resolves, provided there is little risk of bleeding.19,20
Prognosis and complicationsA meta-analysis reported an in-hospital mortality rate of 4.5% in these patients.21 Long-term mortality ranges from 0% to 17%, and recurrence from 0% to 11.4%.1 The possible complications of this disease are: acute heart failure, cardiogenic shock, third-degree atrioventricular block, ventricular tachycardia, ventricular tachycardia in torsade de pointes, ventricular fibrillation, dynamic left ventricular outflow tract obstruction, acute mitral regurgitation, apical thrombus formation, cardioembolic stroke, rupture of the left ventricle, and right ventricular dysfunction associated with pleural effusion and pericarditis.1
ConclusionsThis case illustrates the close relationship between stress and cardiovascular disease. Takotsubo cardiomyopathy is a differential diagnosis that physicians treating patients with suspected coronary syndrome should consider, especially in postmenopausal women with a history of psychiatric comorbidities such as generalised anxiety disorder.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that the procedures followed were in accordance with the regulations of the relevant clinical research ethics committee and with those of the Code of Ethics of the World Medical Association (Declaration of Helsinki).
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Vergel J, Tamayo-Orozco S, Vallejo-Gómez AF, Posada MT, Restrepo D. Síndrome del corazón roto y estrés agudo. A propósito de un caso. Rev Colomb Psiquiat. 2017;46:257–262.