To assess the mental health status and associated factors of Peruvian medical students during the COVID-19 pandemic.
MethodsDescriptive, multicentre, correlational study that used the “Patient Health Questionnaire-9 (PHQ-9)”, the “Generalized Anxiety Disorder-7 (GAD-7)” and the “Impact of Event Scale-Revised (IES-R)” questionnaires to evaluate mental health problems.
ResultsA total of 1,238 students from 8 Peruvian medical schools participated in the study. Of these, 68.5% were women, and the mean age was 21.4 years. Depressive symptoms were found in 74% of the participants, anxiety symptoms in 57% and distress symptoms in 65%. The variables associated with the development of symptoms of moderate-severe depression, anxiety and distress were: not having family economic stability, being in the first years of medical training, being female, and fearing that their medical training would be delayed and impaired.
ConclusionsIn a sample of medical students surveyed during the COVID-19 pandemic, mental health problems were common. The factors associated with mental health reported in this study could be useful in identifying vulnerable medical students who require timely psychosocial support and/or psychiatric care.
Evaluar el estado de salud mental y sus factores asociados en una muestra de estudiantes de Medicina peruanos durante la pandemia de COVID-19.
MétodosEstudio descriptivo, multicéntrico y correlacional que utilizó las escalas Patient Health Questionnaire-9 (PHQ-9), Generalized Anxiety Disorder-7 (GAD-7) e Impact of Event Scale-Revised (IES-R) para evaluar los problemas de salud mental.
ResultadosParticiparon en total 1.238 estudiantes de 8 facultades de Medicina de Perú. El 68,5% eran mujeres y la media de edad, 21,4 años. Se encontraron síntomas depresivos en el 74% de los participantes, síntomas de ansiedad en el 57% y síntomas de malestar en el 65%. Las variables asociadas con la aparición de síntomas depresivos moderados-graves, ansiedad y malestar fueron no tener estabilidad económica familiar, estar en los primeros años de formación médica, ser mujer y sentir el temor de que su formación médica se retrase y se deteriore.
ConclusionesEn una muestra de estudiantes de Medicina encuestados durante la pandemia de COVID-19, los problemas de salud mental fueron comunes. Los factores asociados con la salud mental reportados en este estudio podrían ser útiles para identificar a los estudiantes de Medicina vulnerables que requieran apoyo psicosocial y/o atención psiquiátrica oportuna.
The current pandemic of the novel 2019 coronavirus disease (COVID-19), caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), has brought physical risks as well as psychological challenges to the whole world.1 As of May 2 2021, more than 150 million cases and 3 173 576 deaths were reported worldwide.2 In Peru, during the same period, more than 1,7 million confirmed cases and 61 477 deaths were reported, with a lethality of 3.42%.3 To ensure a decrease in the spread of the disease, measures have been taken to limit contact and exposure such as isolation and quarantine4. On March 16 2020, Peruvian authorities decreed a state of emergency with mandatory quarantine measures.
Individuals in quarantine are particularly vulnerable to psychiatric complications for a variety of reasons: distance from each other and absence or limited interpersonal communication; in this context, depression and anxiety are more likely to occur and get worse. Furthermore, timely psychosocial interventions may not be possible.5,6 The increase in confirmed COVID-19 cases and deaths, social distancing, and quarantine bring the emergence of negative emotions. There are worldwide reports of increased anxiety,7,8 depression,9 and stress symptoms,10,11 in the general population and some vulnerable populations, such as women, older adults, unemployed individuals, patients with previous mental illness, among others.
University students are part of the population vulnerable to developing mental health problems for various reasons, one of which is uncertainty and the potential negative effect on academic progress.11–13 Medical students deserve special attention, as they are expected to have a deeper understanding of the disease, which can make them more anxious during the quarantine period.14 The current pandemic affects the clinical rotation of the medical students and other experiences important for early medical student education (in-person anatomy dissections, group learning sessions, local examinations, etc.).15 Furthermore, medical students are known to have higher levels of anxiety, depression, and stress compared to students in other university pathways.16,17. The limited information on the differential impact of the pandemic on this population not only hinders any attempt to prevent further spread of the disease but also increases existing health inequalities.18 In response to this problem, some studies have already been reported a negative impact on the mental health of medical students.14,19 However, as far as we are aware, there are no studies about the state of mental health in Peruvian medical students.
Due to the impact of the current situation on mental health, it is crucial to examine the factors associated with the mental health problems of the medical student population, so appropriate psychosocial intervention programs can be developed. The present study aims to evaluate the mental health status of Peruvian medical students, as well as the factors associated with it.
MethodsStudy design and target populationThe design of the study is a non-experimental correlational cross-sectional approach, based on an online survey aimed at Peruvian medical students and conducted between April 24 and May 10, 2020. A total of 8 of the 49 Peruvian medical schools were invited to participate: Universidad Católica Santa María (UCSM), Universidad Científica del Sur (UCSUR), Universidad San Martín de Porres (USMP), Universidad Nacional Mayor de San Marcos (UNMSM), Universidad Privada Antenor Orrego (UPAO), Universidad Peruana Cayetano Heredia (UPCH), Universidad Privada San Juan Bautista (USJB), and Universidad Ricardo Palma (URP). Six of these 8 schools are located in the capital city of Lima.
Following the recommendations of social distancing, participants were surveyed virtually. All authors belong to the scientific societies of these universities; they were in charge of collecting the sample following a strategy of convenience through social networks (Facebook, Instagram, and email). Data collection occurred between April 24 and May 10, 2020, 6 weeks after the beginning of the state of emergency and mandatory quarantine by the Peruvian Government. The inclusion criteria were: acceptance to participate in the study, no previous psychiatric diagnosis or treatment, and having correctly completed the survey.
Measurement InstrumentsDepressive symptomsFor the evaluation of depressive symptoms, the Patient Health Questionnaire-9 (PHQ-9) was used. As it is known, PHQ-9 is also a self-administered scale consisting of 9 items, rated on a Likert scale ranging from 0 (not at all) to 3 (almost every day). The PHQ-9 score reflects five categories of severity of depressive disorders: none (0-4), mild (5-9), moderate (10-14), moderately severe (15-19), and severe (20-27). In studies carried out in Latin America, PHQ-9 has been proven to be a valid and reliable tool for detecting depressive symptoms in various types of population.20,21 The PHQ-9 was validated in Peru. Indicia of validity included internal structure, invariance of measurement, and adequate values of internal consistency.22
Anxious symptomsGeneralized Anxiety Disorder-7 (GAD-7) is a universally valid and efficient self-administered scale to assess the severity of anxiety disorders in clinical practice.23 The scale has been translated and validated into Spanish.24 It consists of 7 items directly aimed at the measurement of anxiety symptomatology during the 2 weeks before self-application. Each item was rated on a Likert scale ranging from 0 (not at all) to 3 (almost every day). GAD-7 ratings reflect 4 levels of severity of anxiety disorder: none (0-4), mild (5-9), moderate (10-14), and severe (15-21).
Distress symptomsTo assess the level of distress, the Impact of Event Scale-Revised (IES-R), a self-reporting instrument, was used.25 Each item is rated on a Likert scale ranging from 0 (not at all) to 4 (extremely). IES-R scores reflect 4 levels of distress severity: none (0-8), mild (9-25), moderate (26-43), and severe (44-88). The scale has been translated and validated into Spanish.26
Other variablesInformation was collected on the following variables: age (years), gender, academic period (pre-clinical, clinical, internship), work, religion, with whom they live, steady family income, lives with a person with COVID-19, lives with a person exposed to COVID-19, if the student received online classes, fear of being late in finishing their career and fear of compromising their medical training.
Data analysesData analysis was performed using the statistical program SPSS 22.0 (IBM Corp). It began with a descriptive analysis to characterize the population according to the variables evaluated. The scores of the three assessment tools had a nonnormal distribution and were presented with the median [interquartile range]. The nonparametric Mann-Whitney's U and Kruskal-Wallis tests followed by post-hoc Dunn-Bonferroni test were used to evaluate each characteristic of the population. Then, the outcome variables of mental health: depression, anxiety, and distress were dichotomized into clinically irrelevant (none-mild) and clinically relevant (moderate-severe).
Finally, to determine the risk factors associated with participants’ mental health, a logistic regression analysis (stepwise method) was performed. The strength of association of the variables examined was reported as adjusted odds ratio (aOR) with a 95% confidence interval (95%CI), after adjustment for confounders, including gender, age, academic period, economic stability, lives with a person exposed to COVID-19, fear of damaging medical training, and fear of being late in the career. It was considered statistically significant when P<.05 in a 2-tailed analysis.
Ethical considerationsThe guidelines of the Helsinki Declaration were followed. Each participant provided signed virtual informed consent. The research was carried out with the authorization of the Ethics Committee of the Universidad San Martín de Porres School of Medicine, as noted in document N. 238-2020-CIEI-FMH-USMP.
ResultsInitially, 1549 participants were recruited. Students who did not meet the inclusion criteria included the following categories: not agreeing to participate in the study (n=8), and previous psychiatric diagnosis and treatment (n=297). Besides, 6 subjects were excluded because they filled out their forms incorrectly. A total of 1238 participants were included in the study. The distribution of students by university was: UCSM, 119 (9.6%); UCSur, 124 (10%); USMP, 203 (16.4%); UNMSM, 122 (9.9%); UPAO, 120 (9.7%); UPCH, 93 (7.5%); UPSJB, 220 (17.8%), and URP, 237 (19.1%).
The mean age of the students was 21.4± 3.7 (range, 16-48) years. The majority of participants were women (68.5%), unemployed (88.7%), living with a partner or family member (93.5%), and with family economic stability (77%). Other characteristics are noted in table 1.
A total of 327 (26%) of the students reported no depressive symptoms, 490 (40%) had mild symptoms, 242 (20%) moderate, 137 (11%) moderately severe, and 42 (3%) severe. According to the GAD-7, 528 (43%) of the students reported no anxiety symptoms, 475 (38%) had mild symptoms, 177 (14%) moderate symptoms, and 58 (5%) severe symptoms. Finally, according to the IES-R, 435 (35%) students reported no symptoms of distress, 454 (37%) had mild symptoms, 216 (17%) moderate symptoms, and 133 (11%) severe symptoms.
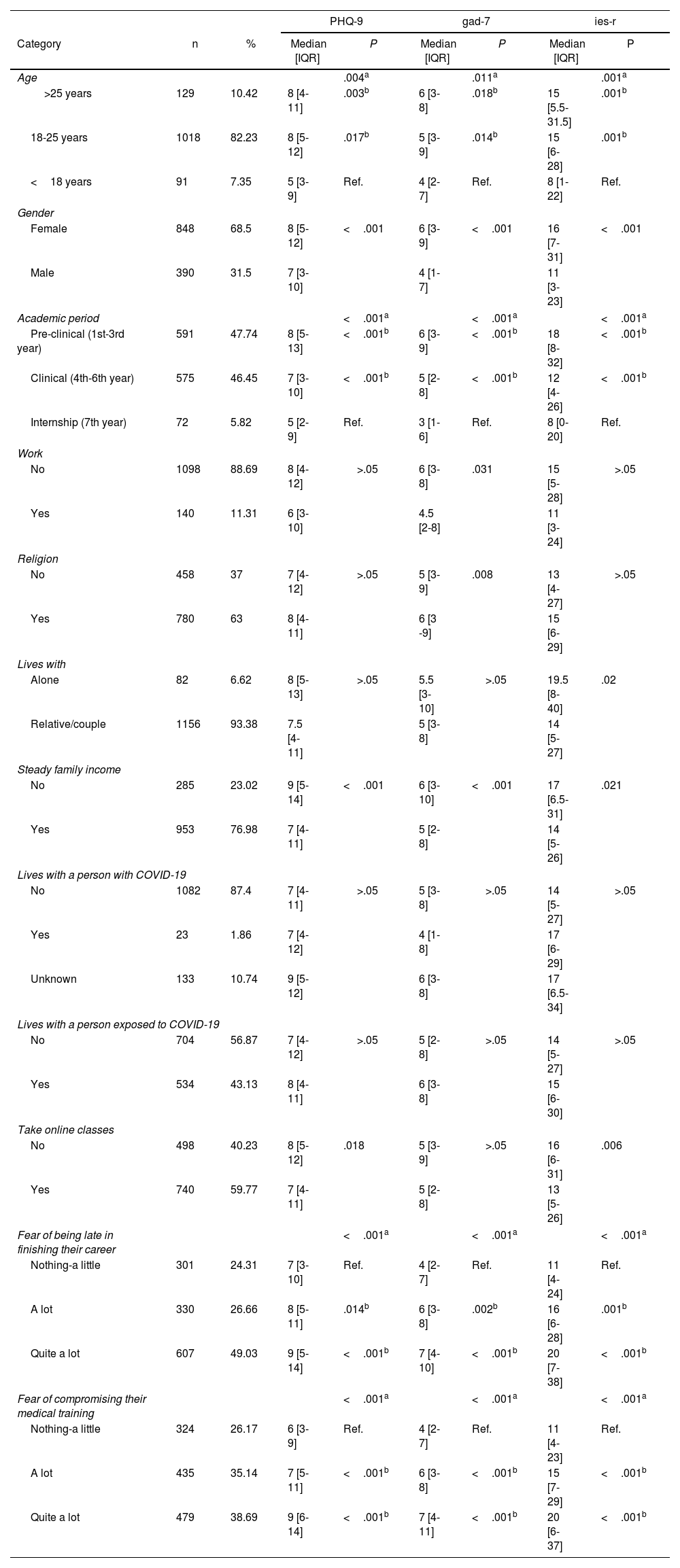
In Table 1 we depict the relationship between the students’ socio-demographic variables and the occurrence of depression, anxiety, and distress (median scores). Student older than 25 years and with age between 18-25 years had significative higher scores when compared with students younger than 18 years in the evaluated mental health (respectively: depression, P=.003 and P=.017; anxiety, P=.018 and P=.015; distress, P=.001 and P=.002). Women also had significative score in all mental health (all P<.001). In academic period, compared with those in the internship (7th year), students in pre-clinical (1st-3rd year) and clinical (4th-6th year) period had significative higher scores for all psychiatric symptoms (P<.001 for both period vs internship). Students who did not work or that did practice religion had significantly higher scores in anxiety (P=.031), but not for depression or distress (all P>.05). Those who lived alone presented significantly higher scores only on distress levels (P=.02). Students that lacked family financial stability had significantly higher scores on depression, anxiety, and distress (all P<.001). There was no difference in students living with a COVID-19 exposed or affected person for scores of depression, anxiety, or distress (all P>.05). Students who reported not taking online classes scored higher on depression (P=.018) and distress (P=.006), but not in anxiety (P>.05). Students who mentioned to feel a lot or quite a lot of fear of being delayed in completing their careers had higher scores when compared with students with nothing/a little fear for this situation (respectively: depression, P=.014 and P<.001; anxiety, P=.002 and P<.001; distress, P=.001 and P<.001). Finally, students who mentioned to feel a lot or quite a lot of fear of compromising training as doctors had higher scores of depression, anxiety, and distress when compared with students with nothing/a little fear for this problem (P<.001 for all comparisons).
Evaluation of the depression, anxiety and distress score among medical students.
| PHQ-9 | gad-7 | ies-r | ||||||
|---|---|---|---|---|---|---|---|---|
| Category | n | % | Median [IQR] | P | Median [IQR] | P | Median [IQR] | P |
| Age | .004a | .011a | .001a | |||||
| >25 years | 129 | 10.42 | 8 [4-11] | .003b | 6 [3-8] | .018b | 15 [5.5-31.5] | .001b |
| 18-25 years | 1018 | 82.23 | 8 [5-12] | .017b | 5 [3-9] | .014b | 15 [6-28] | .001b |
| <18 years | 91 | 7.35 | 5 [3-9] | Ref. | 4 [2-7] | Ref. | 8 [1-22] | Ref. |
| Gender | ||||||||
| Female | 848 | 68.5 | 8 [5-12] | <.001 | 6 [3-9] | <.001 | 16 [7-31] | <.001 |
| Male | 390 | 31.5 | 7 [3-10] | 4 [1-7] | 11 [3-23] | |||
| Academic period | <.001a | <.001a | <.001a | |||||
| Pre-clinical (1st-3rd year) | 591 | 47.74 | 8 [5-13] | <.001b | 6 [3-9] | <.001b | 18 [8-32] | <.001b |
| Clinical (4th-6th year) | 575 | 46.45 | 7 [3-10] | <.001b | 5 [2-8] | <.001b | 12 [4-26] | <.001b |
| Internship (7th year) | 72 | 5.82 | 5 [2-9] | Ref. | 3 [1-6] | Ref. | 8 [0-20] | Ref. |
| Work | ||||||||
| No | 1098 | 88.69 | 8 [4-12] | >.05 | 6 [3-8] | .031 | 15 [5-28] | >.05 |
| Yes | 140 | 11.31 | 6 [3-10] | 4.5 [2-8] | 11 [3-24] | |||
| Religion | ||||||||
| No | 458 | 37 | 7 [4-12] | >.05 | 5 [3-9] | .008 | 13 [4-27] | >.05 |
| Yes | 780 | 63 | 8 [4-11] | 6 [3 -9] | 15 [6-29] | |||
| Lives with | ||||||||
| Alone | 82 | 6.62 | 8 [5-13] | >.05 | 5.5 [3-10] | >.05 | 19.5 [8-40] | .02 |
| Relative/couple | 1156 | 93.38 | 7.5 [4-11] | 5 [3-8] | 14 [5-27] | |||
| Steady family income | ||||||||
| No | 285 | 23.02 | 9 [5-14] | <.001 | 6 [3-10] | <.001 | 17 [6.5-31] | .021 |
| Yes | 953 | 76.98 | 7 [4-11] | 5 [2-8] | 14 [5-26] | |||
| Lives with a person with COVID-19 | ||||||||
| No | 1082 | 87.4 | 7 [4-11] | >.05 | 5 [3-8] | >.05 | 14 [5-27] | >.05 |
| Yes | 23 | 1.86 | 7 [4-12] | 4 [1-8] | 17 [6-29] | |||
| Unknown | 133 | 10.74 | 9 [5-12] | 6 [3-8] | 17 [6.5-34] | |||
| Lives with a person exposed to COVID-19 | ||||||||
| No | 704 | 56.87 | 7 [4-12] | >.05 | 5 [2-8] | >.05 | 14 [5-27] | >.05 |
| Yes | 534 | 43.13 | 8 [4-11] | 6 [3-8] | 15 [6-30] | |||
| Take online classes | ||||||||
| No | 498 | 40.23 | 8 [5-12] | .018 | 5 [3-9] | >.05 | 16 [6-31] | .006 |
| Yes | 740 | 59.77 | 7 [4-11] | 5 [2-8] | 13 [5-26] | |||
| Fear of being late in finishing their career | <.001a | <.001a | <.001a | |||||
| Nothing-a little | 301 | 24.31 | 7 [3-10] | Ref. | 4 [2-7] | Ref. | 11 [4-24] | Ref. |
| A lot | 330 | 26.66 | 8 [5-11] | .014b | 6 [3-8] | .002b | 16 [6-28] | .001b |
| Quite a lot | 607 | 49.03 | 9 [5-14] | <.001b | 7 [4-10] | <.001b | 20 [7-38] | <.001b |
| Fear of compromising their medical training | <.001a | <.001a | <.001a | |||||
| Nothing-a little | 324 | 26.17 | 6 [3-9] | Ref. | 4 [2-7] | Ref. | 11 [4-23] | Ref. |
| A lot | 435 | 35.14 | 7 [5-11] | <.001b | 6 [3-8] | <.001b | 15 [7-29] | <.001b |
| Quite a lot | 479 | 38.69 | 9 [6-14] | <.001b | 7 [4-11] | <.001b | 20 [6-37] | <.001b |
GAD-7: 7-item Generalized Anxiety Disorder; IES-R: 22-item Impact of Event Scale-revised; IQR: interquartile range; PHQ-9: 9-item Patient Health Questionnaire; Ref.: reference for post hoc comparisons in Dunn-Bonferroni test.
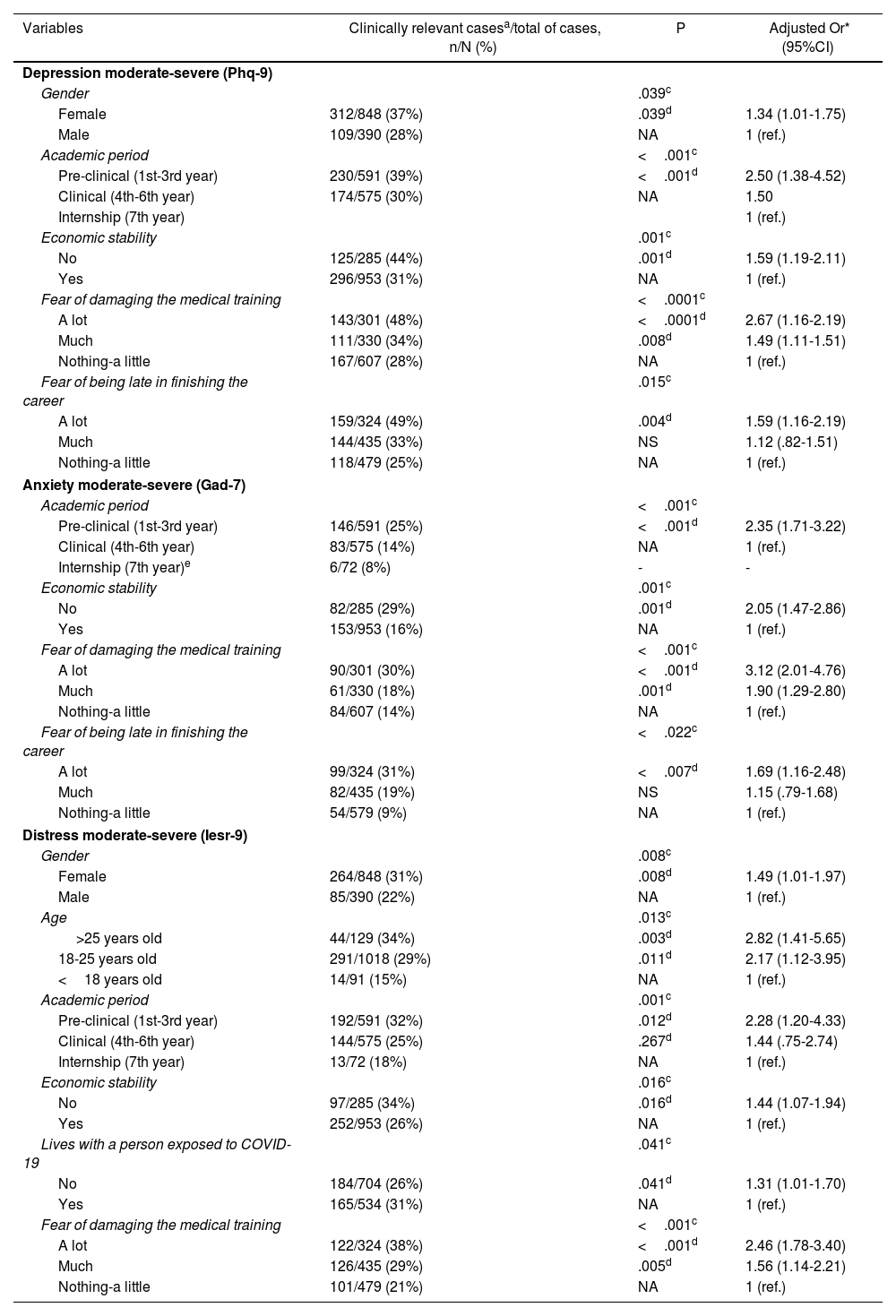
In the logistic regression analysis, it was found that women were a factor associated with clinically relevant symptoms of depression (aOR=1.34; 95%CI, 1.01-1.75) and distress (aOR=1.49; 95%CI, 1.01-1.97). Being in pre-clinical years (1st-3rd year) were a factor associated with clinically relevant symptoms of depression (aOR=2.50; 95%CI, 1.38-4.52), anxiety (aOR=2.35; 95%CI, 1.71-3.22), and distress (aOR=2.28; 95%CI, 1.20-4.33). Not having family economic stability was another variable associated with clinically relevant symptoms of depression (aOR=1.59; 95%CI, 1.19-2.11), anxiety (aOR=2.05; 95%CI, 1.47-2.86), and distress (aOR=1.44; 95%CI, 1.07-1.94). The fear of damaging the medical training since the pandemic was another factor associated with clinically relevant symptoms of depression (aOR=2.67; 95%CI, 1.16-2.19), anxiety (aOR=3.12; 95%CI, 2.01-4.76), and distress (aOR=2.46; 95%CI, 1.78-3.40). Further associations can be found in table 2.
Variables associated with mental health in medical students evaluated by the logistic regression analysis.
| Variables | Clinically relevant casesa/total of cases, n/N (%) | P | Adjusted Or* (95%CI) |
|---|---|---|---|
| Depression moderate-severe (Phq-9) | |||
| Gender | .039c | ||
| Female | 312/848 (37%) | .039d | 1.34 (1.01-1.75) |
| Male | 109/390 (28%) | NA | 1 (ref.) |
| Academic period | <.001c | ||
| Pre-clinical (1st-3rd year) | 230/591 (39%) | <.001d | 2.50 (1.38-4.52) |
| Clinical (4th-6th year) | 174/575 (30%) | NA | 1.50 |
| Internship (7th year) | 1 (ref.) | ||
| Economic stability | .001c | ||
| No | 125/285 (44%) | .001d | 1.59 (1.19-2.11) |
| Yes | 296/953 (31%) | NA | 1 (ref.) |
| Fear of damaging the medical training | <.0001c | ||
| A lot | 143/301 (48%) | <.0001d | 2.67 (1.16-2.19) |
| Much | 111/330 (34%) | .008d | 1.49 (1.11-1.51) |
| Nothing-a little | 167/607 (28%) | NA | 1 (ref.) |
| Fear of being late in finishing the career | .015c | ||
| A lot | 159/324 (49%) | .004d | 1.59 (1.16-2.19) |
| Much | 144/435 (33%) | NS | 1.12 (.82-1.51) |
| Nothing-a little | 118/479 (25%) | NA | 1 (ref.) |
| Anxiety moderate-severe (Gad-7) | |||
| Academic period | <.001c | ||
| Pre-clinical (1st-3rd year) | 146/591 (25%) | <.001d | 2.35 (1.71-3.22) |
| Clinical (4th-6th year) | 83/575 (14%) | NA | 1 (ref.) |
| Internship (7th year)e | 6/72 (8%) | - | - |
| Economic stability | .001c | ||
| No | 82/285 (29%) | .001d | 2.05 (1.47-2.86) |
| Yes | 153/953 (16%) | NA | 1 (ref.) |
| Fear of damaging the medical training | <.001c | ||
| A lot | 90/301 (30%) | <.001d | 3.12 (2.01-4.76) |
| Much | 61/330 (18%) | .001d | 1.90 (1.29-2.80) |
| Nothing-a little | 84/607 (14%) | NA | 1 (ref.) |
| Fear of being late in finishing the career | <.022c | ||
| A lot | 99/324 (31%) | <.007d | 1.69 (1.16-2.48) |
| Much | 82/435 (19%) | NS | 1.15 (.79-1.68) |
| Nothing-a little | 54/579 (9%) | NA | 1 (ref.) |
| Distress moderate-severe (Iesr-9) | |||
| Gender | .008c | ||
| Female | 264/848 (31%) | .008d | 1.49 (1.01-1.97) |
| Male | 85/390 (22%) | NA | 1 (ref.) |
| Age | .013c | ||
| >25 years old | 44/129 (34%) | .003d | 2.82 (1.41-5.65) |
| 18-25 years old | 291/1018 (29%) | .011d | 2.17 (1.12-3.95) |
| <18 years old | 14/91 (15%) | NA | 1 (ref.) |
| Academic period | .001c | ||
| Pre-clinical (1st-3rd year) | 192/591 (32%) | .012d | 2.28 (1.20-4.33) |
| Clinical (4th-6th year) | 144/575 (25%) | .267d | 1.44 (.75-2.74) |
| Internship (7th year) | 13/72 (18%) | NA | 1 (ref.) |
| Economic stability | .016c | ||
| No | 97/285 (34%) | .016d | 1.44 (1.07-1.94) |
| Yes | 252/953 (26%) | NA | 1 (ref.) |
| Lives with a person exposed to COVID-19 | .041c | ||
| No | 184/704 (26%) | .041d | 1.31 (1.01-1.70) |
| Yes | 165/534 (31%) | NA | 1 (ref.) |
| Fear of damaging the medical training | <.001c | ||
| A lot | 122/324 (38%) | <.001d | 2.46 (1.78-3.40) |
| Much | 126/435 (29%) | .005d | 1.56 (1.14-2.21) |
| Nothing-a little | 101/479 (21%) | NA | 1 (ref.) |
95%CI: 95% confidence interval; GAD-7: 7-item Generalized Anxiety Disorder; IES-R, 22-item Impact of Event Scale-Revised; NA: not applicable; NS: not significant (P>.05); OR: odds ratio; PHQ-9: 9-item Patient Health Questionnaire.
This study sought to describe the characteristics of mental health in Peruvian medical students during the COVID-19 pandemic. The reported prevalence of clinically relevant symptoms of depression (34%), anxiety (19%), and distress (28%) is similar to the previous literature. In other studies, depression (35.5%),14 anxiety (21.3-22.1%),14,19 and distress (11.10-26.63%)27 symptoms have been reported. In a study realized among United States medical students during the COVID-19 pandemic, 30.6% and 24.3% of respondents screened positive for anxiety and depression, respectively, using GAD-7 and PHQ-9.28 Our study was conducted 6 weeks after the beginning of the mandatory quarantine in Peru. Longer quarantine duration is associated with poorer mental health, specifically distress symptoms.29
The prevalence of clinically relevant depressive symptoms reported in this study is higher than what was documented in the Peruvian population before the pandemic, in which a prevalence of 6.4% was reported using the PHQ-9.30 This would suggest that the COVID-19 infection has some impact on mental health in the Peruvian medical students by increasing the prevalence of clinically relevant depressive symptoms.
Logistic regression analyses indicate that being female is a factor associated with the development of depression, anxiety, and distressing symptoms. This result supports what has been reported in other studies, which indicate that the presence of depressive, anxiety, and distress symptoms tend to be more frequent in women, thus constituting a vulnerable population.27,31 In addition, women tend to have more symptoms of hyperactivity, recurrent distressing memories, and negative cognitive and mood disorders.10 However, in other studies, these findings have not been reported.14,19
Being in the early years of medical training is a factor associated with the development of moderate-severe depressive, anxiety, and distressing symptoms. Few studies have examined this variable. Liu et al.14 reported that there is no significant difference in the levels of anxiety and depression of medical students concerning the academic year. Halperin et al.28 found that the stage of education influenced the survey outcomes, and pre-clinical students had a higher prevalence of depression and anxiety, possibly due to relocation, uncertainty associated with exam dates, at-home distractions, and less medical school experience.28 Studies carried out before the start of the pandemic have documented that mental health problems in medical students are more frequent during the early years of their training, which decrease as their university education progresses.16 On the other hand, belonging to older age groups was a factor associated with poor mental health. This is different from what Tang et al.32 reported, who found no relationship between age and depressive or distressing symptoms.
Fear of delaying completion of medical school and having their medical training compromised was a factor associated with the development of moderate-severe depressive, anxiety, and distressing symptoms. Concerns around future career disruption, attenuated relationships with medical teachers, and disruption of ongoing extracurricular activities were prevalent among medical students, which underlines the considerable uncertainty amid the COVID-19 pandemic.33 In the United States, the COVID-19 pandemic disrupted the education of medical students. The majority of students wanted to return to clinical rotation and were willing to accept the risk of COVID-19 infection.34
The lack of family economic stability is a factor associated with the development of moderate-severe depressive and anxiety symptoms. These results are similar to those reported by Cao et al.,19 who found that anxiety levels in a sample of Chinese medical students were higher in those who expressed greater concern about delaying their academic training (r=.315; P<.001) and in those who did not have family financial stability. The pandemic not only affects public health but also has an impact on household economies. Due to the pandemic, many people in Peru have lost their jobs, which could have negative effects on the mental health of students related to the concern about how they will continue to pay for their studies.
The possible mechanisms underlying the mental health impact of the COVID-19 pandemic on medical students are complicated. We must also take into consideration the specific characteristics of each culture. For example, in the Chinese culture, education is highly valued and seen as an important path to success, so university students in that country are under great pressure.35 Peruvian universities are organized in disciplinary and vertical terms that classify knowledge according to the hegemony of certain theoretical orientations.36 In contemporary Peru, mercantilism follows the general pattern of the university pattern as part of the globalization process that covers society.36 The prolonged closure of these universities and concerns about academic progress and loss of economic investment could be important factors in the impact on the mental health of these students.
These results lead us to recommend that the mental health of medical students should be carefully evaluated. Medical students should be taught how to improve their sense of self-worth and to adapt to difficult situations to have a mean for effective management of their depressive tendencies.37 Some universities provide mental health services, but they may be restricted because they do not provide long term help, this being a limitation, but the solution to this situation is ideally to provide therapeutic information that can help university students during this period of COVID-19, that is, doctors can use telemedicine, because university students in these times of pandemic are familiar to the use of the internet because of the online classes they receive, therefore telemedicine can be used, that can help treat some anxiety and depression through apps and/or using text messaging, because if left untreated, anxiety and depression will worsen, may even lead to other mental and physical health problems, or problems in daily and/or college life, thus hindering academic success, and may even affect high-risk behaviours, prolonged alcohol and tobacco use increases, use and abuse of other substances, having unprotected sex and increasing the risk of suicide.38 Besides, future longitudinal studies are required in this regard. In circumstances of considerable uncertainty, both medical students and educators need to be flexible and resilient.33
This study has some limitations; first, due to the limited resources and the need to generate information on the mental health effects of this pandemic, we performed a sampling of convenience, which limits the generalization of these results; second, our sample had mostly participants from universities in Lima, so we cannot generalize our results to all medical schools in Peru, and third, being our study cross-sectional, we can only describe correlations but not causality. However, an important strength of this study is that it is the largest study examining the mental health of medical students during the pandemic in Peru.
ConclusionsThe results of this study, conducted during the initial peak phase of the COVID-19 pandemic in Peru, indicate a high prevalence of mental symptoms in medical students. The most important factors associated with the development of moderate-severe depressive, anxiety, and distressing symptoms are not having family economic stability, being in the first years of medical training, being female, and expressing fear that their medical training will be delayed and impaired. All these variables could be useful when identifying vulnerable students who require timely psychiatric care. Universities should provide psychological counselling services and adapt them to the current circumstances to mitigate the mental health problems of medical students.
FundingThis research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author contributionsJHV designed the study. JHV, CEF, and JS wrote the initial manuscript. DCZ, LVZ, AP, AT, GH, DC, CNB, and EA collected the data. JS assisted with statistical analysis and interpreted the data. All authors contributed to the article and approved the submitted version.
Conflicts of interestsThe authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
We are grateful to Graciela S. Alarcón, MD, MPH, MACR, and David Villarreal, BSC MPH, for providing expert assistance in the review of earlier versions of this manuscript.