Previous studies suggest that the severity of alterations in cognitive functions in people with a diagnosis of bipolar I disorder (BP-I) are directly related to the deterioration in overall functioning and life quality. Altered cognitive function is associated with a worse prognosis of BP-I, however little is known about the relationship between cognitive functions and the clinical features of BP-I.
ObjectiveTo establish possible associations between cognitive function and the clinical and socio-demographic characteristics of patients with BP-I.
MethodsCognitive function was evaluated by applying a neuropsychological battery to a group of patients with a BP-I diagnosis, who did not have affective episodes for at least 6 months, and who were outpatients treated at the San Juan de Dios Clinic in Manizales. The statistical analysis involved using clustering methodology in order to divide those patients with the best and worst cognitive function and it was later correlated with the clinical and socio-demographic variables.
ResultsA statistically significant correlation was found between the number of years of education and the age the disorder started with alterations in the level of cognitive function (p=0.002 and p=0.017 respectively). No significant correlations were found with other variables.
ConclusionsAn early onset of the pathology and fewer years of education seems to be risk factors associated with poorer cognitive function in patients with BP-I.
Estudios previos indican que la gravedad de las alteraciones de las funciones cognitivas de los diagnosticados de trastorno bipolar tipo I (TBI) están directamente relacionadas con el deterioro del funcionamiento general y la calidad de vida. Un funcionamiento cognitivo alterado se asocia con peor pronóstico del TBI, pero se conoce poco de la relación entre las funciones cognitivas y las características clínicas del TBI.
ObjetivoEstablecer posibles asociaciones entre el funcionamiento cognitivo y las características clínicas y sociodemográficas de los pacientes con TBI.
MétodosSe evaluó el funcionamiento cognitivo a través de la aplicación de una batería neuropsicológica a un grupo de pacientes con diagnóstico de TBI que se encontraran en ausencia de episodios afectivos durante al menos 6 meses, atendidos ambulatoriamente en la Clínica San Juan de Dios de Manizales. El análisis estadístico implicó la metodología de clasificación en clusters para dividir los pacientes con mejor y peor funcionamiento cognitivo, y después se correlacionó con las variables clínicas y sociodemográficas.
ResultadosSe encontró asociación estadísticamente significativa entre el número de años de estudio y la edad de inicio del trastorno con alteraciones en el nivel de funcionamiento cognitivo (p=0.002 y p=0.017 respectivamente). No se encontraron asociaciones significativas con otras variables.
ConclusionesEl inicio temprano de la afección y un menor número de años de estudio serían factores de riesgo asociados con un peor funcionamiento cognitivo de los pacientes con TBI.
The World Health Organisation (WHO) has classified BP-I as the sixth cause of disability in the 15–44 age group and ninth across all ages. It is also one of the conditions that causes the highest number of years of life lost to disability.1,2 In Colombia, the 2015 National Mental Health Survey estimated a BP-I prevalence of 0.4% in adolescents and 0.3–0.7% in adults over the past 12 months.3 Studies carried out in the Caldas department have found a 0.5% prevalence of BP-I in the past 12 months and a lifetime prevalence of both types of bipolar disorder of 8.1%, significantly higher than the figure reported in other parts of Colombia and the world.4 The fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5)5 includes—among the diagnostic criteria required for the diagnosis of BP-I—affective, psychomotor, cognitive and vegetative symptoms in depressive and manic episodes, but does not take into account the presence of disorders that persist during periods with no affective episodes, while cognitive impairments are a frequent and significant finding in a large proportion of patients with BP-I, both in affective episodes and euthymic states.6 Impaired cognitive functioning in BP-I is related to difficulties regarding working capacity, social interaction and the family environment; they also correlate with a reduced hedonic capacity and autonomy and a permanent disability in around 20% of patients.7–9
The cognitive functions most commonly reported as impaired in patients with BP-I are information processing speed, executive functioning and verbal memory, even in affective episode-free periods,10–12 which could explain the difficulties these people face in their daily lives to a great extent.11,13
Different study groups on BP-I have highlighted the importance of dividing the evolution of the condition into stages, using clinical variables and biomarkers, in order to refine diagnosis, direct treatment and assess prognosis.14–17 In such staging models, the clinical variables proposed are the number of episodes, time since onset of the disorder, psychosocial functioning, interepisode functioning and cognitive functioning.14,15,17 Among these variables, cognitive functioning is hard for patients to express in a reliable manner, even when they use self-reporting forms.18 As a result, we opted to assess it using neuropsychological batteries.18,19 The possible association between a progressive disorder and a decline in cognitive functioning is not clearly established and the results of the research carried out indicate that not all patients follow said course.20 It is therefore important to understand the relationship between cognitive functioning and the variables involved in staging BP-I. Moreover, cognitive functioning is an indicator of neuronal integrity, a predictor of the patient's prognosis and a therapeutic objective aimed at reducing dysfunctionality.21–23
One BP-I staging model proposes diving the disorder into early stage, characterised by better functioning, fewer episodes and a late age at onset, and a late stage, characterised by worse functioning, more episodes and an early age at onset. Taking into account the importance of assessing cognitive functioning in patients with BP-I, the study hypothesis is that cognitive functioning may be related to the clinical variables proposed in staging models. The objective is to determine the association between cognitive functioning and the clinical variables related to the staging of BP-I patients.
MethodsThis is a cross-sectional analysis study. As a test unit, it used euthymic BP-I patients attending the outpatient programme of the San Juan de Dios Clinic in Manizales and the University of Caldas. 55 patients with a diagnosis of BP-I were included, which was confirmed by a clinical interview, analysis of their clinical history using DSM-5 criteria5 by two psychiatrists and a diagnostic interview for genetic studies (DIGS), validated in the Columbian population.24 A state of euthymia was defined as a period of at least six months with no diagnosis of affective episodes or changes to psychopharmacological prescriptions, as well as the attendance of psychiatry-led controls, in which clinical stability and scores <6 in the Hamilton Depression Rating Scale (HDRS)25 and Young Mania Rating Scale (YMRS)26 were confirmed at the time of assessment. Patients of both genders were included, aged from 18 to 60, who voluntarily agreed to take part in the study and signed the informed consent. Patients with comorbidities due to mental disorders related to the use of psychoactive substances, learning disability, history of severe neurological diseases or severe traumatic brain injury were excluded, along with those who were illiterate.
The project was approved by the Research Ethics Committee of the University of Caldas and informed consent was obtained taking into account the ethical guidelines set forth in Colombian legislation.27
Assessment instrumentsNeuropsychological tests were obtained in a session lasting 45min, on average. They were applied by psychiatrist interns from the University of Caldas, who were trained and supervised by a Neuropsychology lecturer from the same university. Said tests assessed: attention, memory and executive functions. The Rey Auditory Verbal Learning Test (RAVLT)28,29 was employed, alongside the letter and number sequencing, digit-symbol coding, arithmetic and digit span subtests from the Wechsler Adult Intelligence Scale (WAIS III)30; the Trail Making Test (TMT) A and B,31 Stroop Colour and Word Test (SCWT),32 Wisconsin Card Sorting Test (WCST)33 and semantic verbal fluency and phonological verbal fluency subtests of the Neuropsi Attention and Memory34 were also used. Values were adjusted by age for RAVLT, letter and number sequencing, digit-symbol coding, Stroop, arithmetic, digit span and working memory index; they were adjusted by age and education for semantic verbal fluency, phonological fluency and the WCST total score, with raw scores for TMT A and B.
Statistical analysisUnivariate analysis was performed by measuring frequencies for qualitative variables, and mean±standard deviation for quantitative variables. The Kolmogorov–Smirnov normality test was applied and, for variables that had no normality criteria, a log transformation (log10) was used for the parametric analysis. Cluster analysis was then carried out, which consists of identifying groups of objects which are similar to each other, but different from other groups. Based on the results, the data obtained were divided into two groups, those referred to as having better cognitive functioning and worse cognitive functioning. The grouping method used was K-means clustering, which is based on specifying distances between cases to form a number (K) of groups on finding the best distance between the groups’ sites and where each variable belongs to the group closest to the mean. The variables selected from the bivariate analysis were typified to avoid the impact generated by distances between variables with small values in the case grouping. Demographic and clinical variables were then compared between the better cognitive functioning and worse cognitive functioning groups and, finally, a multivariate logistic regression analysis was performed, using worse cognitive functioning as the result variable. Statistical analyses were performed with the IBM-SPSS Statistics 18.0 package.35
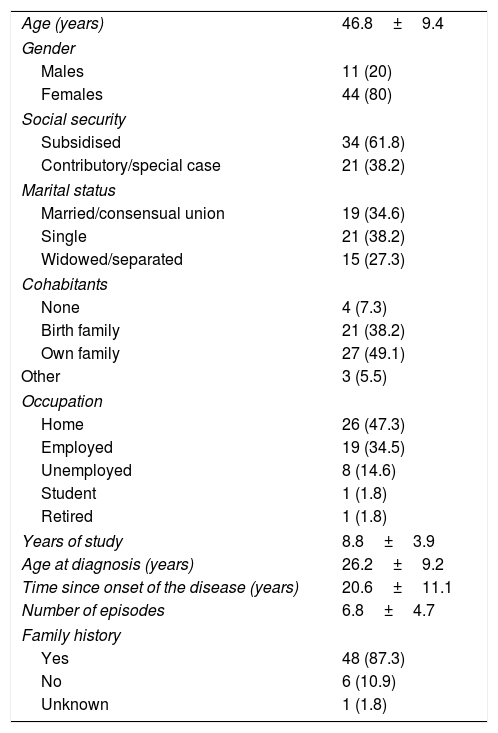
ResultsClinical and sociodemographic characteristicsThe sample comprised 55 individuals, the clinical and sociodemographic characteristics of whom are described in Table 1. At the time of the study, 8 patients were undergoing treatment with valproic acid (14.5%); 27 with valproic acid plus an antipsychotic (49.2%); 6 with lithium carbonate plus an antipsychotic (10.9%); 4 with lithium carbonate plus valproic acid plus an antipsychotic (7.3%); 4 with an antipsychotic (7.3%); 2 with lithium carbonate plus valproic acid (3.6%); 2 with valproic acid plus an antihistamine (3.6%); 1 with lithium carbonate plus an antihistamine (1.8%); and 1 was not taking medication (1.8%). Six were also taking antidepressants (10.9%) and 11 were also receiving levothyroxine (20%).
Demographic and clinical characteristics of the sample studied.
| Age (years) | 46.8±9.4 |
| Gender | |
| Males | 11 (20) |
| Females | 44 (80) |
| Social security | |
| Subsidised | 34 (61.8) |
| Contributory/special case | 21 (38.2) |
| Marital status | |
| Married/consensual union | 19 (34.6) |
| Single | 21 (38.2) |
| Widowed/separated | 15 (27.3) |
| Cohabitants | |
| None | 4 (7.3) |
| Birth family | 21 (38.2) |
| Own family | 27 (49.1) |
| Other | 3 (5.5) |
| Occupation | |
| Home | 26 (47.3) |
| Employed | 19 (34.5) |
| Unemployed | 8 (14.6) |
| Student | 1 (1.8) |
| Retired | 1 (1.8) |
| Years of study | 8.8±3.9 |
| Age at diagnosis (years) | 26.2±9.2 |
| Time since onset of the disease (years) | 20.6±11.1 |
| Number of episodes | 6.8±4.7 |
| Family history | |
| Yes | 48 (87.3) |
| No | 6 (10.9) |
| Unknown | 1 (1.8) |
Values are expressed as the n (%) or mean±standard deviation.
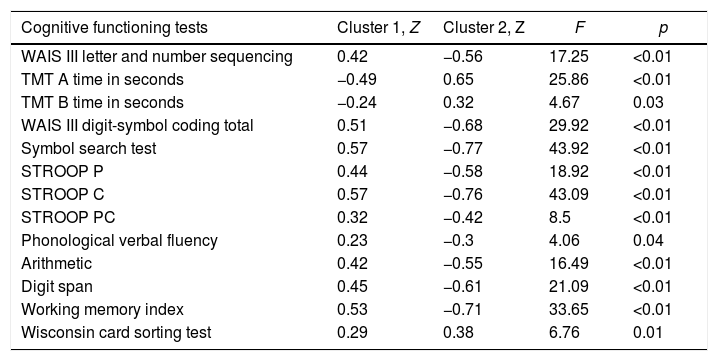
The sample was empirically divided using the neurocognitive test variables to describe cognitive functioning determined as either better cognitive functioning or worse cognitive functioning. The result was two groups of relatively equal patients, 31 (56.3%) with better cognitive functioning and 24 (43.7%) with worse cognitive functioning. The results of the neurocognitive tests were rated taking into account age, education and gender, using the applicable reference values recommended for that purpose by the authors. The variables pertaining to the RAVLT memory test and semantic verbal fluency test scores were excluded because the results were not statistically significant in the initial model. However, said exclusion did not generate changes regarding the pertinence of the cases to each of the groups.
The analysis of variance (ANOVA) revealed significant differences between the central values of both clusters and the values described in Table 2. In this comparison, the F test is only used with a descriptive purpose, since the groups were chosen through the cluster analysis in order to maximise the differences between sites.
Cluster analysis.
| Cognitive functioning tests | Cluster 1, Z | Cluster 2, Z | F | p |
|---|---|---|---|---|
| WAIS III letter and number sequencing | 0.42 | −0.56 | 17.25 | <0.01 |
| TMT A time in seconds | −0.49 | 0.65 | 25.86 | <0.01 |
| TMT B time in seconds | −0.24 | 0.32 | 4.67 | 0.03 |
| WAIS III digit-symbol coding total | 0.51 | −0.68 | 29.92 | <0.01 |
| Symbol search test | 0.57 | −0.77 | 43.92 | <0.01 |
| STROOP P | 0.44 | −0.58 | 18.92 | <0.01 |
| STROOP C | 0.57 | −0.76 | 43.09 | <0.01 |
| STROOP PC | 0.32 | −0.42 | 8.5 | <0.01 |
| Phonological verbal fluency | 0.23 | −0.3 | 4.06 | 0.04 |
| Arithmetic | 0.42 | −0.55 | 16.49 | <0.01 |
| Digit span | 0.45 | −0.61 | 21.09 | <0.01 |
| Working memory index | 0.53 | −0.71 | 33.65 | <0.01 |
| Wisconsin card sorting test | 0.29 | 0.38 | 6.76 | 0.01 |
Cluster 1: better cognitive functioning.
Cluster 2: worse cognitive functioning.
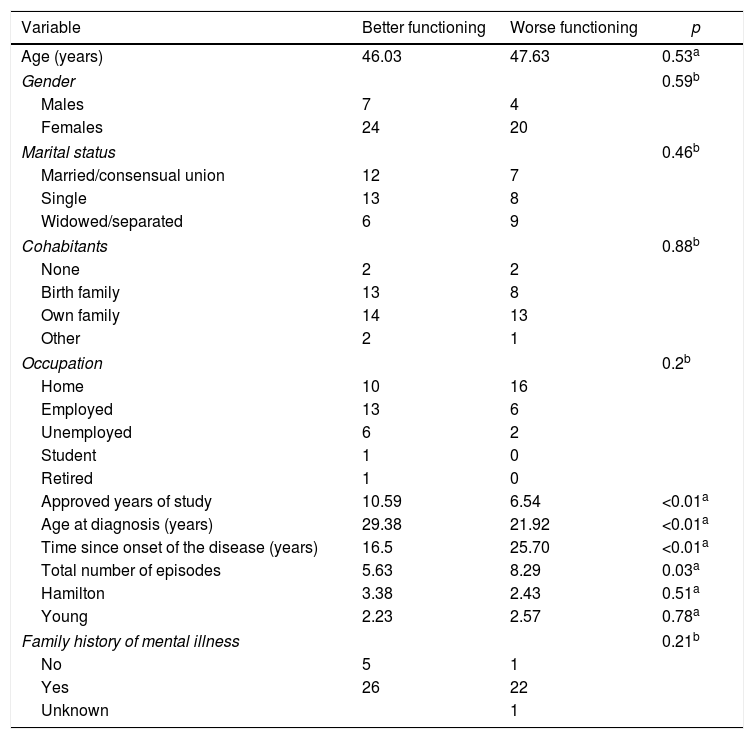
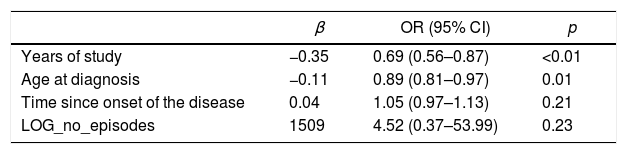
The clinical and demographic characteristics of the sample were then compared using clusters, and statistically significant differences were found in relation to the years spent studying, age at diagnosis, time since diagnosis and the number of affective episodes (Table 3). These four variables were included in the logistic regression model due to the fact that they were significant in the bivariate analysis, and worse cognitive functioning was used as the result variable to evaluate the relationship between them. A model was constructed by entering the variables step by step; the variables pertaining to the number of years spent studying and age at onset of the disorder revealed statistically significant values in relation to cognitive functioning (Table 4). The variables time since onset of the disorder and number of episodes were not significant (p=0.22 and p=0.23, respectively).
Sociodemographic and clinical variables with cognitive functioning.
| Variable | Better functioning | Worse functioning | p |
|---|---|---|---|
| Age (years) | 46.03 | 47.63 | 0.53a |
| Gender | 0.59b | ||
| Males | 7 | 4 | |
| Females | 24 | 20 | |
| Marital status | 0.46b | ||
| Married/consensual union | 12 | 7 | |
| Single | 13 | 8 | |
| Widowed/separated | 6 | 9 | |
| Cohabitants | 0.88b | ||
| None | 2 | 2 | |
| Birth family | 13 | 8 | |
| Own family | 14 | 13 | |
| Other | 2 | 1 | |
| Occupation | 0.2b | ||
| Home | 10 | 16 | |
| Employed | 13 | 6 | |
| Unemployed | 6 | 2 | |
| Student | 1 | 0 | |
| Retired | 1 | 0 | |
| Approved years of study | 10.59 | 6.54 | <0.01a |
| Age at diagnosis (years) | 29.38 | 21.92 | <0.01a |
| Time since onset of the disease (years) | 16.5 | 25.70 | <0.01a |
| Total number of episodes | 5.63 | 8.29 | 0.03a |
| Hamilton | 3.38 | 2.43 | 0.51a |
| Young | 2.23 | 2.57 | 0.78a |
| Family history of mental illness | 0.21b | ||
| No | 5 | 1 | |
| Yes | 26 | 22 | |
| Unknown | 1 | ||
Logistic regression. Patients with worse cognitive functioning.
| β | OR (95% CI) | p | |
|---|---|---|---|
| Years of study | −0.35 | 0.69 (0.56–0.87) | <0.01 |
| Age at diagnosis | −0.11 | 0.89 (0.81–0.97) | 0.01 |
| Time since onset of the disease | 0.04 | 1.05 (0.97–1.13) | 0.21 |
| LOG_no_episodes | 1509 | 4.52 (0.37–53.99) | 0.23 |
95% CI: 95% confidence interval; OR: odds ratio.
Goodness of fit, Hosmer–Lemeshow χ2=7.14; degrees of freedom, 7; p=0.414.
This study compared cognitive functioning with some of the clinical variables used to stage patients diagnosed with BP-I. There is evidence of there being cognitive function impairments, even in a euthymic state.6 This highlights the pertinence of dividing them into clusters with the objective of understanding the possible characteristics of their cognitive profile which may help to differentiate them for staging, which could have both diagnostic and therapeutic implications.
The bivariate analysis in our study showed that the group with worse cognitive functioning has an early age at onset, a longer time since onset of the disorder and a greater number of episodes. Meanwhile, the group with better cognitive functioning has a late age at onset, less time since onset and fewer episodes. This finding reinforces the importance of stage classification systems in BP-I.14,15,17,36
The logistic regression analysis only found a significant association between better cognitive functioning, late onset and a greater number of years spent studying, but not with the number of episodes or time since onset of the disorder. The relationship between better cognitive functioning and a greater number of years spent studying may suggest the greater cognitive reserve37 of the patient, which is in line with other studies that have found said reserve to be an indicator of cognitive and functional prognosis in patients with the disorder.38 Thus, the positive relationship with late age at onset could indicate that better cognitive functioning favours the onset of the condition and/or that said case in particular would progress with a less “aggressive” form of the disorder; it is thus equally likely for there to be a milder cognitive decline. Similar findings from other studies have found that an early age at onset is associated with worse functioning overall, as measured by the FAST scale.13
Another approach to this phenomenon may be that a later onset of the disorder enables the person to study for a greater number of years, thus favouring their cognitive reserve.
It is also possible that cognitive deficits occurring before the disorder may be detrimental to cognitive reserve and overall functioning and, together with vital stressors derived from said situation, that they favour the earlier onset of the condition. In accordance with this hypothesis, literature reviews have found that some cognitive domains of BP-I patients are already impaired before the first affective episode.39 Other studies have found an association between other variables and cognitive functioning. For example, sub-threshold sleep disorders and depressive symptoms in euthymic patients have also been associated with worse cognitive functioning.40
There is evidence that better cognitive functioning has a negative association with the number of episodes and time since onset of the disorder.41 However, in our study, the logistic regression analysis did not detect any such relationship. This may be explained by the fact that our group did not include patients who presented comorbidities in the form of substance use disorders or adherence failures at least in the past six months – conditions that have been associated with greater cognitive decline in other studies.42,43 Obviously, this finding may also be due to the size of our sample and the fact that it is a cross-sectional study.
There are other studies that, despite not measuring overall functioning, indicate a direct relationship between said functioning and cognitive impairments.44,45 The negative finding we observed between the number of episodes and impaired cognitive functions indicates that there may be other variables which we failed to detect or assess that directly impact cognitive performance.
LimitationsThis is a cross-sectional study, so the possibility of establishing causal relationships between the associated clinical and demographic variables and cognitive functioning is limited. Determining the number of episodes that were not treated in hospital or specialist outpatient clinics is difficult, since this is based on the recollections of the patient and his/her relatives, which could lead to inaccuracy when they are recorded. Another significant limitation is that our sample was small and no sample calculation was performed to ensure the adequate power of the study.
ConclusionsThe results of this study indicate that there is an association between the number of years spent studying, age at onset of the disorder and the level of cognitive functioning of patients with BP-I.
Cluster identification in these patients may be of great clinical use, since it facilitates the implementation of diagnostic (staging) and therapeutic strategies that are appropriate for each of them. In this context, we recommend that research be continued in this field in order to identify and refine the characteristics and, in turn, outline possible groups of these types of patients.
Longitudinal studies with a larger sample size are required in order to confirm the staging of BP-I and clarify the causal relationships between the different clinical variables.
FundingThis study was conducted with the resources of the University of Caldas and the support of the San Juan de Dios Clinic in Manizales.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this research.
Confidentiality of dataThe authors declare that they have followed the protocols implemented in their place of work regarding the publication of patient data.
Right to privacy and informed consentThe authors have obtained the informed consent of the patients and/or subjects referred to in the article. This document is in the possession of the corresponding author.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Castaño Ramírez OM, Gómez Montoya SM, Lemos Buitrago R, Valderrama Sánchez A, Castro Navarro JC. Relación del funcionamiento cognitivo con variables clínicas en pacientes con trastorno bipolar tipo I. Rev Colomb Psiquiat. 2018;47:204–210.