Leukoencephalopathy is a myelin disorder caused by multiple agents, including substance abuse. A 28-year-old man arrived at the emergency department having suffered from asthenia, dizziness, disorientation and ataxia for two months. He had a two-year history of heroin inhalation. He arrived in a normal physical condition. Brain magnetic resonance showed bilateral diffuse hypointense lesions in the white matter. At day 3 after admission, he presented neurological deterioration, stupor, haemodynamic instability, respiratory failure, and died. Toxic leukoencephalopathy symptoms start with inattention, memory and personality changes, and may eventually cause dementia and death. Heroin inhalation is a common practice and can lead to leukoencephalopathy. Leukoencephalopathy associated with heroin inhalation is a rare entity that mainly affects young adults and has a high social impact. Its aetiology is unclear, it has no effective treatment and there is a high mortality rate. Heroin consumption is on the rise in Colombia, so TL should be considered by medical staff.
La leucoencefalopatía es una patología de la mielina producida por múltiples agentes, incluidas las sustancias de abuso. Un varón de 28 años llegó urgencias por 2 meses de astenia, mareo, desorientación y ataxia. Tenía antecedentes de consumo inhalado de heroína por 2 años. Presentaba condiciones físicas regulares. La resonancia magnética cerebral mostró lesiones hipointensas difusas bilaterales en la sustancia blanca. Al tercer día presentó empeoramiento de su estado neurológico, estupor, inestabilidad hemodinámica, insuficiencia respiratoria y muerte. Los síntomas de leucoencefalopatía tóxica (LT) comienzan con falta de atención, cambios en la memoria y la personalidad, y finalmente demencia y muerte. El consumo de heroína inhalada es una práctica frecuente con riesgo de que produzca LT. La leucoencefalopatía asociada con el uso de heroína inhalada es una entidad rara que afecta principalmente a adultos jóvenes y tiene un alto impacto social. Su etiología no está clara, no tiene un tratamiento efectivo y tiene altas tasas de mortalidad. El consumo de heroína está aumentando en Colombia, por lo que el personal médico debe tener en cuenta la LT.
Leukoencephalopathy is the structural damage of cerebral white matter due to the destruction of myelin. Multiple conditions may lead to leukoencephalopathy, such as genetic disorders, primary demyelinating diseases, infections, metabolic disorders, brain trauma (diffuse axonal damage), and vascular diseases, among others;1 although toxins remain as a prevalent and disabling cause.2
Toxic leukoencephalopathy (TL) is caused by the exposure of a wide variety of agents including environmental toxins, toluene, cranial irradiation, substance abuse or medications such as chemotherapy.3,4 TL may be due to idiosyncratic reaction as well as dose or time exposure related. TL prevalence remains unknown, and it is considered a rare entity.
However, an over increasing frequency has been reported due to industrial chemicals use, chemotherapy, or psychoactive substances abuse.2,4 Inhaled heroin use has been associated with the incidence of TL since the 1980s.5 Brain damage mechanism remains unknown, but some suspected hypothesis include toxins derived from heroin molecular modification induced by heating, or and hypoxic-ischemic pathology.6,7 In the present report, we present a fatal case of TL in a young man with inhaled heroin consumption.
Case PresentationA 28 years-old man from the urban area of Pereira (Colombia) was admitted to the emergency department presenting a rapid and progressive onset of asthenia, adynamia, dizziness, disorientation, muscle weakness and ataxic gait, installed over the past two weeks. He had no medical or surgical record, except for substance abuse such as marijuana and cocaine since he was 15 years old. He reported inhaled heroin use over the last two years, with an increasing pattern in the last six months.
He was admitted in regular physical conditions, emaciated, distractible, with hypomimia, bradylalia, bradypsychia, fluctuating akinetic mutism, abulia, with apathy, impaired immediate memory, slowness of movement, hypotonia, slightly decreased generalized muscle strength and ataxic gait. Osteotendinous reflexes were normal and no Babinski sign was found. Hemodynamics parameters were stable, and no signs of respiratory difficulty were reported.
Total blood count showed mild leukocytosis. The other laboratory tests (urinary function, blood gases, serum sodium, infectious diseases test such as HIV, syphilis, hepatitis B virus, and hepatitis C virus) were unremarkable. Cranial computed tomography scan (CT) showed spread white matter (WM) hypodense images located at the semi-oval centers, posterior limb of the internal capsules, corticospinal aces, occipital regions, and cerebellum.
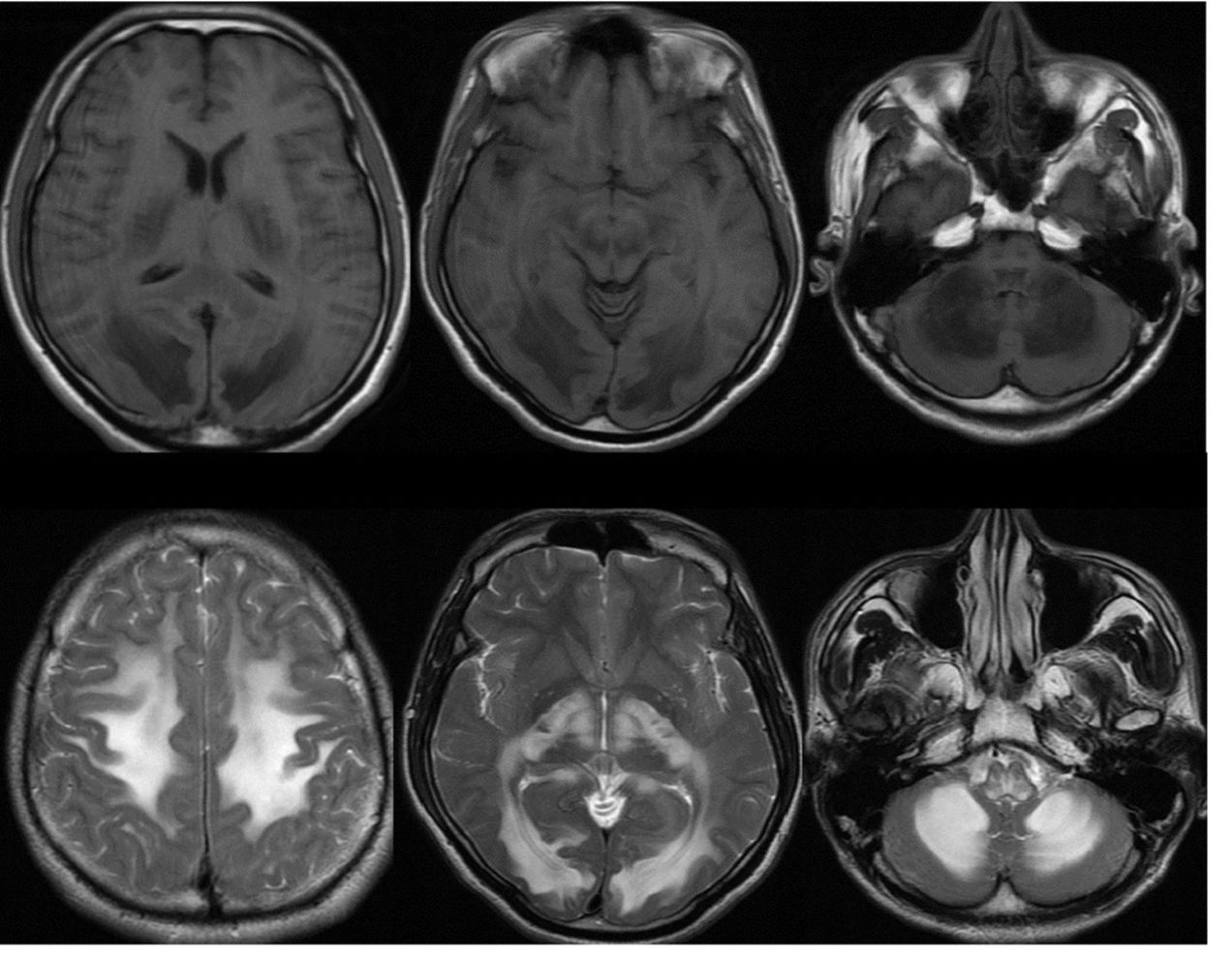
Brain magnetic resonance (MR) revealed hypointense lesions in T1 sequences, hyperintense and symmetric T2 sequence lesions in WM at the semi-oval centers, basal nuclei, corticospinal tracts, cerebellum, the posterior area of the corpus callosum as well as in mesencephalic and bulbar regions (fig. 1). The patient worsens three days after admission, with neurological impairment, stupor, hemodynamic instability, respiratory failure, and death.
Cranial computed tomography scan (up) showing spread white matter (WM) hypodense images located at the semi-oval centers, the internal capsules, corticospinal aces, occipital regions, and cerebellum. Brain magnetic resonance (down) revealed hypointense lesions in T1 sequences, hyperintense and symmetric T2 sequence lesions in WM at the semi-oval centers, basal nuclei, corticospinal tracts, cerebellum, the corpus callosum and the mesencephalic and bulbar regions.
After the patient died, the family signed the informed consent to use the clinical and radiological records to present and publish the case for scientific and academic purposes, conserving the privacy and identity of the patient out of the record.
Literature ReviewWM covers approximately half of the brain and it is composed of multiple intra and interhemispheric tracts. WM dysfunction due to myelin damage may produce neuropsychiatric symptoms such as distractibility, memory impairment, personality changes, psychosis, mood changes, and dementia.4 TL must be considered in patients with neurobehavioral deficit who were exposed to toxins or substances.2
Heroin (diacetylmorphine) is a semisynthetic drug, derived from morphine and originated from the poppy (Papaver somniferous), first synthesized in the late 19th century and initially emerged as antitussive medicine. Heroin quickly showed great addictive potential, so it was labeled as an illicit substance.8
“Chasing the Dragon” is the popular name given to inhaled heroin consumption.9 When heated on aluminum folds, heroin becomes a reddish-brown gelatinous substance that releases a thick, white smoke that resembles a dragon tail. This smoke is “pursued” or inhaled through a straw or a tubular structure. This technique is also called “Chinese blow”. This practice was recognized for the first time in Hong Kong in the 1950s, but nowadays it has been extended to users all over the world.9,10
Despite inhaled heroin consumption is frequent, and the association with TL is known, it has rarely been reported.11 The first and largest outbreak of TL associated with the use of inhaled heroin was reported in 1982 in the Netherlands, including 47 cases, of which 11 died.5 Since 1982, sporadic cases have been reported in Taiwan, Hong Kong, the United States, and China, among others5,10-12
Autopsies from TL patients associated with the use of inhaled heroin reveal spongiform degeneration, the formation of vacuoles in the oligodendroglia and myelin sheaths, with demyelination of the brain, cerebral stem, cerebellum, and spinal cord; these findings are called spongiform leukoencephalopathy12,13 Pyrolysate, a compound resulting from the combustion of heroin, seems to be responsible for cerebral damage6,10
In a German study carried out in 2014, eight death patients due to heroin TL showed increased serum lactate, suggestive of cerebral hypoxia; increased choline, suggestive of axonal compromise; and decreased n-acetyl-aspartate, suggestive of mitochondrial dysfunction.7 Image findings in the TL include a compromise of symmetrical dentate nuclei, cerebellum, cerebral WM with bilateral symmetric hypersignal in the posterior limb of the internal capsule.13,14
Heroin TL progress through three stages. Initial symptoms include motor restlessness, apathy, bradyphrenia, and cerebellar ataxia. In the second stage, there is worsening of cerebellar symptoms, hyperactive deep tendon reflexes, myoclonic jerks, and hypertonia. In the final stage, manifestations include stretching spasms, diaphoresis, fever, hypotonia, areflexia, and akinetic mutism, and in some cases death.10-12 Heroin TL mortality ranges between 23 and 25%, and death occurs mainly due to respiratory failure. There is no effective treatment for TL10-12
United Nations Office on Drugs and Crime reported that, worldwide, approximately 5% of the global adult population has used drugs at least once, in the lifetime, another 0.6% suffered from drug use disorders (SUD). About 28 million years of “healthy life” were lost worldwide in 2015 because of premature death and disability caused by SUD. Opioids, including heroin, remain the most harmful drugs and are responsible for 70% of the SUD global burden.15
In Colombia, there were about 32 thousand people consuming heroin in 2013, with an expected increase to date. Medellin, Cali, Pereira, and Armenia are the more affected cities by the heroin-related disorders.16,17 In this epidemiological context, patients with TL due to heroin consumption, just like this clinical case, will be more frequently seen at emergency departments and psychiatric institutions.
ConclusionsInhaled heroin consumption is a risk factor for TL, with severe neurological compromise and high disability and death risk. Since heroin consumption is becoming more frequent, and there have been identified methadone treatment barriers,17 this may be considered a public health issue.
It's necessary to improve programs focused on heroin consumption prevention, consequences treatment, and elimination of the barriers to getting adequate treatment alternatives.
Conflicts of InterestsNone.
Este caso fue presentado en la modalidad de short oral presentation en el 18thWPA World Congress of Psychiatry, en Ciudad de México, entre el 27 y el 30 de septiembre de 2018.