Kikuchi-Fujimoto disease is a benign disorder that mainly affects young women, and is characterized by predominantly cervical lymphadenopathy associated with fever and leukopenia. Although of unknown etiology, there is evidence that a viral infection or autoimmune disease can trigger the disease. An uncommon case in Colombia is presented of Kikuchi-Fujimoto disease in a patient with Systemic Lupus Erythematosus.
La enfermedad de Kikuchi-Fujimoto es un trastorno benigno que afecta principalmente a mujeres jóvenes, se caracteriza por adenopatías de predominio en la región cervical, asociadas a fiebre y leucopenia. Aunque de etiología desconocida, hay evidencia de que una infección viral o una enfermedad autoinmune puede desencadenar la enfermedad. Se reporta un caso infrecuente en Colombia de enfermedad de Kikuchi-Fujimoto en una paciente con lupus eritematoso sistémico.
Generalized lymphadenopathy is a frequent manifestation in patients with systemic lupus erythematous (SLE), with a prevalence of up 26%.1 In addition to infections, Castleman disease, sarcoidosis, lymphoma and Kikuchi-Fujimoto Disease (KFD) – also called histiocytic necrotizing lymphadenitis – shall also be considered in these patients.2 KFD is a benign disorder that mainly affects young women and is characterized by lymphadenopathies, predominantly in the cervical region, associated with fever and leucopenia.3 Although its etiology is unknown, there is evidence that the disease may be triggered by a viral infection or an autoimmune disease.4 There are case reports in the literature of SLE coexisting with KFD that give rise to the controversy of whether they represent a clinical manifestation typical of SLE or a concomitant process.2 An important consideration when evaluating KFD is that the histology may reveal groups of immunoblasts and some lymphocytes with nuclear atypia that are mistaken by T-cell lymphoma,4 a diagnosis that is finally considered in up to 30% of the cases of KFD, thus being its primary differential.5 Following is the discussion of a case of a young patient with polyarthralgias and generalized lymphadenopathies, diagnosed with SLE and histological confirmation of KFD.
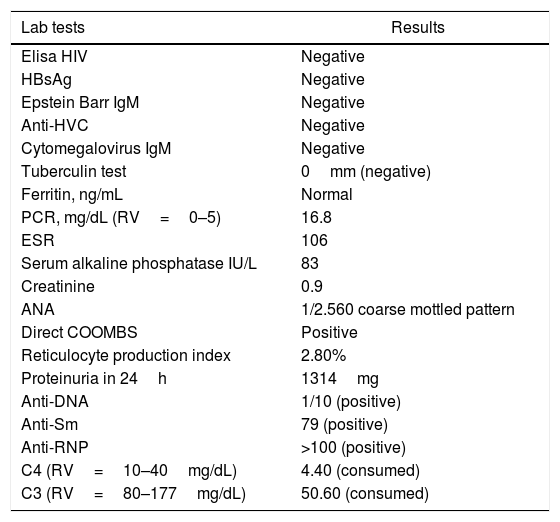
Case presentationA 23-year old woman, with unremarkable personal or family history, with a clinical presentation of one-year evolution of symmetrical polyarthralgia of the hands and knees, associated to edema and morning stiffness. In the 15 days prior to admission, the patient developed increased joint pain and subsequent functional limitation that required hospital admission for studying. The systems review documented diffuse alopecia, xerophthalmia, xerostomia, xeroderma, paresthesia, and occasional dysesthesias of the limbs. There was no history of weigh loss, fever, diaphoresis, or any other symptoms. The vital signs were normal at admission. The physical examination revealed tender cervical adenomegaly, with soft and mobile lymph nodes less than 1.5cm in size; hands edema and symmetrical synovitis with a positive bilateral squeeze test in the metacarpophalangeal joints in the 2–4 digits. Absence of arthritic signs in the elbows, knees or ankles. The rest of the physical examination was normal. The laboratory tests are shown in Table 1.
Laboratory tests in a patient with Kikuchi-Fujimoto Disease and SLE, Pereira, 2017.
| Lab tests | Results |
|---|---|
| Elisa HIV | Negative |
| HBsAg | Negative |
| Epstein Barr IgM | Negative |
| Anti-HVC | Negative |
| Cytomegalovirus IgM | Negative |
| Tuberculin test | 0mm (negative) |
| Ferritin, ng/mL | Normal |
| PCR, mg/dL (RV=0–5) | 16.8 |
| ESR | 106 |
| Serum alkaline phosphatase IU/L | 83 |
| Creatinine | 0.9 |
| ANA | 1/2.560 coarse mottled pattern |
| Direct COOMBS | Positive |
| Reticulocyte production index | 2.80% |
| Proteinuria in 24h | 1314mg |
| Anti-DNA | 1/10 (positive) |
| Anti-Sm | 79 (positive) |
| Anti-RNP | >100 (positive) |
| C4 (RV=10–40mg/dL) | 4.40 (consumed) |
| C3 (RV=80–177mg/dL) | 50.60 (consumed) |
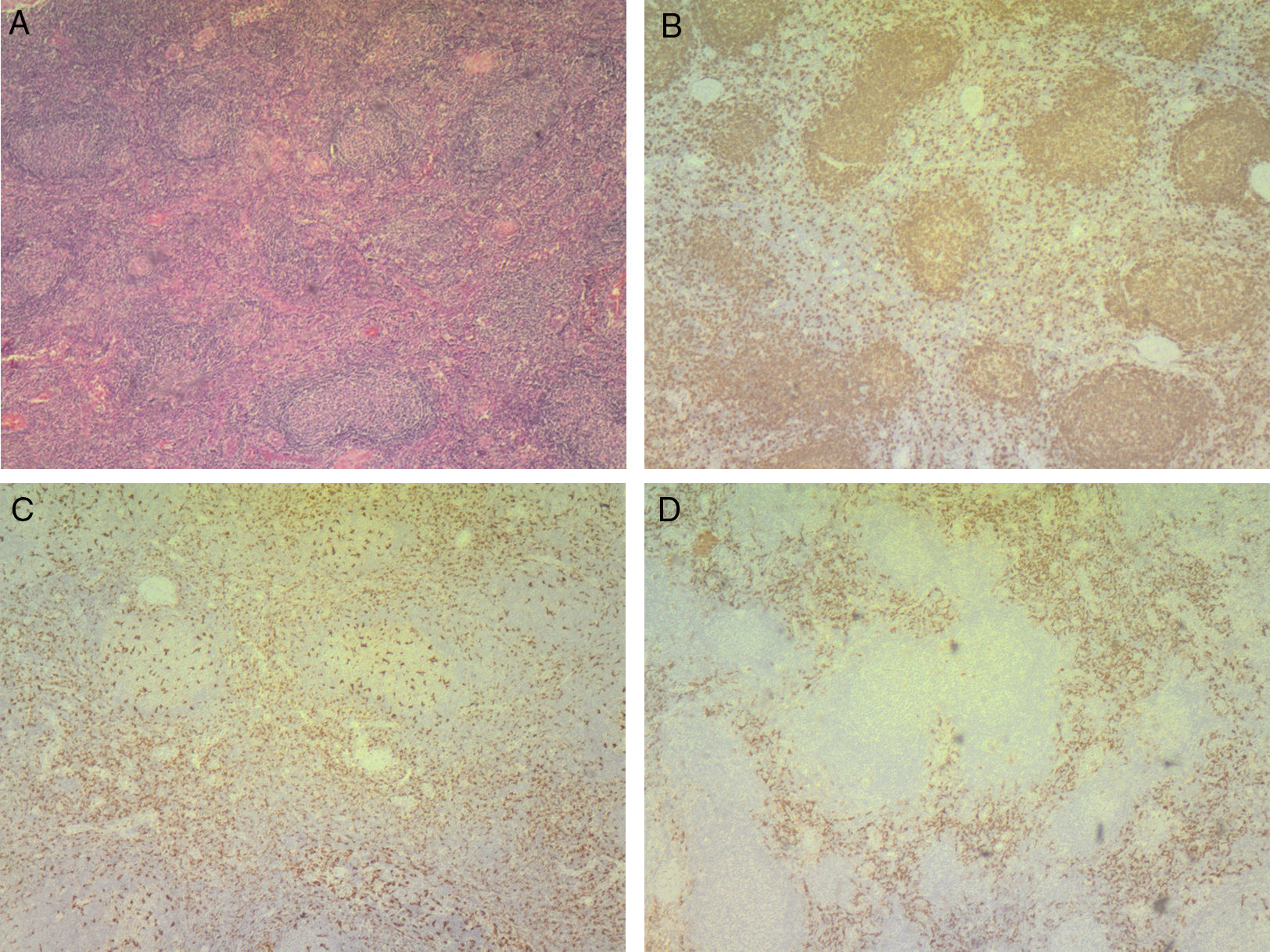
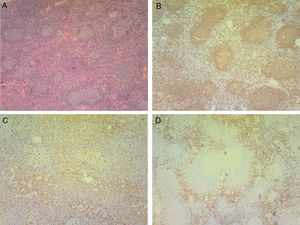
A diagnosis of SLE is made based on the presence of 9/17 SLICC criteria, with high activity of the disease (SLEDAI 14 points). The imaging studies showed multiple reactive type lymphadenopathies at the intraparotid level, in bilateral cervical segments I, II, III, IV, and V, on both axillary regions in the left iliac fossa, anterior to the psoas muscle, with the largest measuring 1.5cm (Fig. 1). A biopsy of the cervical lymph node reported hyperplasia and cell changes indicative of potential lymphoma (Fig. 2A), with similar findings observed in the bone marrow study. Nevertheless, the immunohistochemistry ruled out the diagnosis of lymphoma (Fig. 2B) and confirmed lymphoid hyperplasia with positive labeling for interfollicular histiocytes, compatible with KFD (Fig. 2C and D).
Lymph node biopsy.
A. Hematoxylin and eosin stain: small necrotic foci and nodal and interfollicular hyperplasia with mononuclear cells showing mild atypia, intermixed with neutrophils and histiocytic cells.
B–D. Immunohistochemistry: CD20 positive staining showing normal distribution lymphocytes, with evidence of hyperplasia (B). CD68 positive staining (C) and CD163 (D) of mostly interfollicular histiocytic cells. The cell proliferation rate measured by Ki67 is normal.
The case of a patient in her thirties with generalized lymphadenopathy coexisting with SLE – a rare association in our country – is discussed. KFD was initially independently reported in 1972 by pathologists Kikuchi and Fujimoto, as a lymphadenitis with focal proliferation of reticular cells accompanied by numerous histiocytes, karyorrhexis and fagocitosis.5 The disease affects mainly women in their third to fourth decade of life, and while its prevalence in higher among the Asian population, there have been some cases reported in America, Europe and Africa.4,5 The etiology of the disease is still unknown; however, the most accepted hypothesis is its viral origin, although the evidence associating the disease to viruses such as Epstein-Barr, herpes virus, and other infectious causes is not convincing.5,6 Moreover, there are some reports on the coexistence with autoimmune diseases such as Still's, granulomatosis with polyangiitis, Sjögren's syndrome, polymiositis, relapsing polychondritis, thyroiditis, autoimmune hepatitis, rheumatoid arthritis, and less frequently SLE.2,4
The patient in this case presented with concomitant manifestations of both SLE and KFD, indicating that these 2 conditions may share several clinical and morphological characteristics, which results in a difficult differential diagnosis. KFD may present simultaneously with SLE or may develop before of after SLE has been diagnosed.7 In a series of 91 cases of patients affected by KFD, 11 of the patients had a known history of SLE, 10 patients were concomitantly diagnosed, and 2 patients developed the disease over the course of follow-up.6
The physical examination and imaging studies conducted showed enlarged lymph nodes involving the parotid glands and the cervical, axillary and anterior psoas muscle regions, indicating the presence of generalized lymphadenopathy, in accordance with Ferrer's definition.8 The generalized lymphadenopathy is a rare presentation of KFD4,5 and in contrast, the characteristic finding is unilateral cervical lymphadenopathy, with usually small lymph nodes (<3cm), mobile and tender at palpation. Other symptoms described in this disease include nausea, emesis, weight loss, and arthralgia, with the latter being the cardinal manifestation of the clinical presentation in our patient.
Some authors have claimed that KFD may be a characteristic or an incomplete phase of lupus lymphadenitis; however, several case reports with absent SLE characteristics argue in favor of two separate entities that may coexist.7
Laboratory tests are usually normal in KFD6; however, leukopenia may be present in up to 58% of the patients and is the most frequent abnormality.4 Other findings reported include anemia, thrombocytopenia, and elevation of acute-phase reactants.7 In this case, anemia with chronic characteristics of the disease was identified, in addition to elevated erythrocyte sedimentation rate (ESR), which may also be a manifestation of SLE. Therefore, the cause of these alterations is difficult to ascertain in the presence of both diseases.
The radiological appearance of adenopathies is not characteristic. The ultrasound examination may show hypoechoic lymph nodes, with a hyperechoic, thickened and irregular outer rim.4 The CT findings are variable and may mimic lymphoma and other diseases such as tuberculosis or metastasis,5 similar to the imaging reports in this case, where the key differential diagnosis considered was the potential of lymphoproliferative disease. A study in 96 patients with KFD reported that the CT cervical adenopathies were homogeneous and multiple, affecting regions II to V and in 94% of the patients measured less than 2.5cm.9 These characteristics allow for differentiating from lymphoma, which typically affects a smaller number of lymph nodes but of larger size, with perinodal infiltration and necrosis.4
The final diagnosis is made through an excisional biopsy of the affected lymph nodes.2,4,5 A cervical lymph node biopsy was performed in this patient, which reported the characteristic findings of KFD: nodal and interfollicular hyperplasia, intermingled with histiocytic-like cells and small necrotic foci, suggesting, and finally confirming the diagnosis through immunohistochemistry.2–4
The presence of the following morphological characteristics is highly suggestive of a diagnosis of KFD: (a) focal areas of necrosis in the paracortical region, with abundant karyorrhexis; (b) numerous histiocytes and plasmacytoid dendritic cells, and (c) a minority of lymphocytes and immunoblasts inside or around the areas of necrosis.4 Several authors agree that the identification of neutrophils and hematoxylin bodies in the area of necrosis are characteristics in favor of a diagnosis of SLE lymphadenitis.4
The primary differential diagnosis of KFD is CD8+ T-cells lymphoma, since KFD may present immunoblast aggregates and atypical lymphocytes, and these findings are suggestive of lymphoproliferative disease.4 The study by Dorfman et al. revealed that 30% of the 108 lymph node biopsies reviewed were initially misdiagnosed as lymphomas.10 In this case, and consistent with the epidemiological profile and the behavior of both diseases, non-Hodking's lymphoma was suggested as the primary diagnostic option; however, the immunohistochemistry studies conducted finally ruled out this condition.
In conclusion, the patient presented with generalized lymphadenopathy secondary to KFD and concomitant with SLE, which was confirmed based on laboratory tests, imaging studies and histology. Since the treatment for KFD is mainly support therapy, including analgesics and anti-inflammatory agents, it significantly differs from lymphoma therapy and hence it should be considered for the differential diagnosis in patients with local or generalized lymphadenopathies and SLE.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that the procedures followed were in accordance with the regulations of the relevant clinical research ethics committee and with those of the Code of Ethics of the World Medical Association (Declaration of Helsinki).
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
FundingNo funding was received from any government or private institution for this paper.
Conflicts of interestThe authors have no conflicts of interest to declare.
Our gratitude to Carlos Enrique Ramírez Isaza. Md. General Surgeon.
Please cite this article as: López-Villegas VJ, Medina-Morales DA, Alzate-Piedrahita JA, Aguirre AM, Saldarriaga Rivera LM. Enfermedad de Kikuchi-Fujimoto en una paciente con lupus eritematoso sistémico y linfadenopatía generalizada. Reporte de caso. Rev Colomb Reumatol. 2018;25:216–220.