Patients with pediatric lupus nearing transition to adult care are expected to take responsibility for their care. Nevertheless, many are not prepared for this, and thus have a poorer prognosis. Using the self-regulation model, the perception of a condition determines the emotional responses and guides coping efforts, appraisal, feedback, and assimilation strategies.
ObjectiveTo describe how adolescents nearing transition perceive lupus.
Materials and methodsEleven semi-structured interviews were conducted using a hermeneutic approach with techniques from grounded theory. Interviews took place between July 2013 and September 2014. The participants were nine adolescents with diagnosed lupus.
ResultsA total of 1800 codes were obtained that emerged as the following preliminary categories: “Attempting to explain the origin”, where the cause of the disease is interpreted as immunosuppression, autoimmunity, association with cancer, guilt and influence of emotional factors, along with the diagnosis process. “What is lost”, which includes changes, being treated differently, and having limitations. The last category was “positive aspects” deals with illness as a behavioral moderator, acquiring qualities, learning about bodily functioning and secondary gain.
ConclusionAdolescents perceive their condition based on the implications of the changes experienced in their lives as a result of the diagnosis. Lupus affects several aspects of their lives and brings uncertainty and a need to adjust, leading them to look for explanations. More awareness of these perceptions is required because the latter, along with other factors, determine the strategies that adolescents develop to ensure their self-care and adaptation to any situations arising from living with the condition.
Se espera que pacientes con lupus pediátrico próximos a la transición asuman responsabilidades de su cuidado, pero muchos no están preparados, lo cual empobrece su pronóstico. Según el modelo autorregulatorio, las percepciones de la enfermedad determinan las respuestas emocionales, guían las conductas de afrontamiento, su evaluación, retroalimentación y estrategias de asimilación.
ObjetivoDescribir las percepciones sobre el lupus en adolescentes próximos a la transición.
Materiales y métodosDesde un enfoque hermenéutico y utilizando técnicas de la teoría fundada, se realizaron 11 entrevistas semiestructuradas entre junio de 2013 y septiembre de 2014 a 9 adolescentes con diagnóstico de lupus.
ResultadosSe obtuvieron 1.800 códigos. Emergieron como categorías preliminares: «Intentando explicar el origen», donde se interpreta la causa de la enfermedad en términos de inmunosupresión y autoinmunidad, asociación con cáncer, culpa e influencia de factores emocionales, además el proceso diagnóstico. «Lo que se pierde», enmarcado en cambios, trato diferencial y límites. Finalmente, los «aspectos positivos»: enfermedad como modulador de la conducta, adquisición de cualidades, aprendizaje sobre el funcionamiento corporal y ganancia secundaria.
ConclusiónLas percepciones de la enfermedad en estos adolescentes, expresan en la experiencia de cambio las implicaciones del diagnóstico, las cuales impactan múltiples aspectos de sus vidas y traen consigo incertidumbre y necesidad de ajustes que les llevan a la búsqueda de explicaciones. Se requiere mayor conciencia sobre estas percepciones, debido a que, junto con otros factores, determinarán las estrategias que los adolescentes desarrollen para garantizar su autocuidado y adaptación a situaciones derivadas del vivir con la enfermedad.
Systemic lupus erythematous (SLE) is a “multisystem autoimmune disease, characterized by the presence of autoantibodies and multiple organ involvement”.1 Its clinical presentation features periods of remission and activity. Around 15 to 20% of the new cases of SLE are diagnosed during childhood.2,3 Generally speaking, pediatric SLE (pSLE) has a more severe onset, with higher probability of organ damage, particularly renal and neuropsychiatric.3 Thanks to the advancement of medicine and related sciences, the 10-year survival is over 90% for pediatric SLE patients, in contrast with the 40% survival rate of the seventies.4 However, the cost has been high: children with SLE must endure strict medical control regimens, exams, multiple drug therapy, and lifestyle changes, within the context of a complex healthcare system that provides coverage for some “basic conditions” that often fail to meet the needs of a comprehensive therapy.
The prospect of a longer life expectancy presents challenges for children with chronic conditions that reach adolescence and are transferred over to adult care. The expectation is that when they reach this stage in life, they should take responsibility for their self-care and should have the necessary skills to properly cope with all matters related to the disease and the healthcare system.5 However, the reality is different; many children with chronic diseases may not be ready to take on such responsibility when they reach adolescence.6 Some studies have shown that the lack of an adequate transition process, defined as “an active, multidimensional, process that is appropriate for age and development, and meets the medical, psychosocial and educational/vocational needs of adolescents when transferred from pediatric to adult care”,7 reflects on a poor prognosis that hinders the development of their full potential, and is detrimental to the healthcare system because of the ensuing complications.8,9
Leventhal et al.10 refer to the effects of chronic illnesses and say that while in some people the “psychological stress is minimal”, others have difficulties in adapting to their condition; they suggest a framework of reference as the basis for analysis of this phenomenon. Later, Pimm and Weinman11 adapted this framework to rheumatology diseases and called it the “self-regulatory model”. According to this framework, the perceptions about the disease – which are in fact “cognitive organized representations or believes that patients have about the disease”,12 determine the emotional responses, guide “disease coping behaviors”h, its evaluationi, feedback, and additional internalization strategies.13
The development of skills that facilitate the process of accepting responsibility for the disease and the care required, involves having a consolidated autonomy, which in a way is related to the perception about your body, and in this particular case, of the disease.
Notwithstanding the fact that over the past few years14–16 several research projects with qualitative methodologies have been conducted about the experience of living with SLE, and about the meaning of the disease for patients,17 there is little qualitative research exploring these matters in adolescents about to be transitioned.18,19 The objective of this paper was to describe the perceptions about SLE among a group of adolescents about to transition, and is part of a larger trial exploring the way in which adolescents with SLE, nearing transition, acquire the skills associated with self-care.
Materials and methodsBased on a hermeneutic approach, several grounded theory techniques20 were used. The grounded theory relies on symbolic interactionism,21 which as a sociological school of thought, allows for understanding people's behavior based on what things mean to them; understanding that such meanings are the result of the interaction with other individuals, and these meanings are further modified by interpretation.
The study population comprised adolescent patients between 14 and 18 years old, with a diagnosis of SLE, pursuant to the criteria of the American College of Rheumatology (ACR),22 with at least three control visits and minimum 8 months after the diagnosis. Patients with cognitive impairment and those that refused to participate in the trial were excluded. The study sampling process was not probabilistic but based on convenience, inviting key informants from a referral center in Medellin, and captured from the pediatric rheumatology clinic, to participate.
The information was captured using a semi-structured interview based on a script designed to explore the meanings they attribute to lupus and “living with lupus”. All interviews were recorded – upon obtaining the informed consent – and analyzed using the methodology proposed by Strauss and Corbin,20 implementing initially open coding. Each code resulting from the analysis was identified with an alphanumeric label identifying the consecutive code number (C...), the interview identification (I1-I11), and the transcription page number to find the interview (P...). Subsequently, the axial coding process was conducted,20 giving rise to the preliminary categories; these emerging categories were then analyzed in terms of attributes and dimensions. Some of these preliminary results are described herein. This paper was approved by the Ethics Committee of the Hospital Pablo Tobón Uribe and was funded by the Colombian Association of Rheumatology.
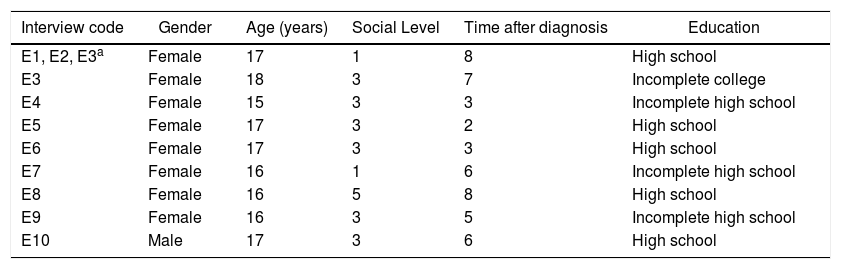
Results11 interviews were conducted in 9 patients, between June 2013 and September 2014 (7 in females and 2 in male patients), aged between 15 and 18 years old, with an average of 5 years after being diagnosed (Table 1). 1800 codes were obtained as a result of open coding.
Demographic characteristics of the participating adolescents with systemic lupus erythematous.
| Interview code | Gender | Age (years) | Social Level | Time after diagnosis | Education |
|---|---|---|---|---|---|
| E1, E2, E3a | Female | 17 | 1 | 8 | High school |
| E3 | Female | 18 | 3 | 7 | Incomplete college |
| E4 | Female | 15 | 3 | 3 | Incomplete high school |
| E5 | Female | 17 | 3 | 2 | High school |
| E6 | Female | 17 | 3 | 3 | High school |
| E7 | Female | 16 | 1 | 6 | Incomplete high school |
| E8 | Female | 16 | 5 | 8 | High school |
| E9 | Female | 16 | 3 | 5 | Incomplete high school |
| E10 | Male | 17 | 3 | 6 | High school |
A number of the adolescents interviewed said that lupus was “a disease of defenses”, indirectly referring to immunosuppression and autoimmunity. Some adolescents referred to the idea of immunosuppression as the “first explanation” they heard about the disease. It is not easy to grasp medical concepts such as autoimmunity and to understand that the very things that play a protective role (immune system or defenses) finally and for reasons not fully understood, attack us. Thus, some adolescents find it “more logical” to understand the disease in terms of immunosuppression, a representation that may be the result of the information they receive about the effect of some therapies that are immune system modulators and their potential adverse effects. It should be kept in mind that often patients fail to distinguish between the clinical manifestations of the disease activity and the effects caused by treatment-associated complications; in both cases, patients refer to their condition as “being ill”, as evidenced by the following code: «Having your defenses low makes you sick more often» C125E10P18
In the case of other adolescents interviewed, one could think that the interpretation that helps them to shape the experience of the onset of the disease is that the “defense system” instead of playing its “protective” role inflicts harm; so they refer to some aspects of their condition in terms of perceiving an internal battle that is associated with the medical term autoimmunity. Lupus: “a senseless battle” C110E6P13 and “self-attack to your organs” C88E9P15
The conflict in daily living leads to making associations and interpretations, as expressed by one of the patients who used a metaphor extracted from the armed conflict experienced in the country, in order to try to explain with more clarity her idea about the disease: “This is like when the army and the guerillas engage in battle, or when the people themselves fight against the army and attack each other, though they are aware that they are both good people; this is what causes my platelets to drop. This is my understanding.” C111E6P13.
The concept of lupus being like “cancer” is an extended believe mentioned by several adolescents. However, the young patients interviewed fail to recognize the differences between the two conditions, and although they are just able to express very rudimentary concepts about the pathophysiology, both conditions differ in terms of the “potential consequences.” “Lupus: “A cancer, but tinier” C109E6P13 “I tell them it is not really cancer, it is a disease of the blood in which cells attack other cells; however, I say it is not that severe, though it may affect other organs but cannot be that serious.” C96E7P20
The expression “cannot be that serious”, though it can be a subjective conclusion of experiencing the SLE symptoms, also correlates with the perceived impending therapeutic response and stationary evolution of the disease, in contrast with the progress of a malignant disease.
Coping with a high impact diagnosis such as SLE gives rise to a number of reactions in the individual affected; there may be mood changes associated with cognitive elaborations of the situation experienced or expressions that convey the suffering caused by the interpretations of the event and associated changes. Guilt, with its underlying emotional connotation, emerged in some interviews and suggests, based on the expressions of some adolescents, that it is an option to find not just an explanation, but the potential source of the disease. Accepting responsibility for the disease is one of the nuances of guilt. A number of adolescents associated their condition with punishment, a consequence of misbehaving, doing things against the advice of their superiors (family and society), or the result of counterproductive actions in the context of the disease: Looking for culprits: “I caused my lupus” C103E4P10, I am the one to blame for causing such thing” C100E4P10 “Because I disobeyed my mother's recommendations I got lupus” C106E4P10 “I got lupus because I went to the pool too often and got too much sun exposure” C97E4P10
Another example is that of an adolescent who related lupus to nutrition; this association is not rare, since many people think that “most diseases are the result of what you eat”, and this may be valid in some cases. The association between the development of lupus and food may also generate a feeling of guilt. If you are a teenager and have enough resources, you may choose what you eat, but sometimes the choices are contrary to what parents and doctors expect for a healthy nutrition.
We cannot neglect the psychological phenomena that go hand in hand with physiological changes. All of the above statements express in a veiled manner the personal reaction to a sick body, taking on the responsibility for the condition.
In some other interviews, the cause of the disease was attributed to external events that generated emotional stress and occurred close to the time of diagnosis, identifying those events as the culprits. One case in point is a young girl who described a difficult family event as the likely cause for her SLE: “The stress caused by my father when I lived with him” C104E9P1
Blaming external factors, or even themselves, for causing the disease seems to fill in part the information gap that still prevails. However, another teenager decided not to speak about causes or culprits, and rather spoke about chance as the main factor that led to the development of the disease: “No body is to blame; anyone may experience such thing” C201E6P22
We found that some teenagers share the perception that there are several classes of lupus. Such believe is the result of the evaluation of the impact of the disease on their lives, as compared to other more or less severe forms; the less severe condition may even be considered a normal status: whether the life of the patient is affected or not will make lupus is a normal condition to live with. “I think that there are different types of lupus” C86E9P15 “Lupus may be normal if nothing is affected” C89E7P15
“The disease is made invisible because you don’t feel it”; this could be the expression with which several teenagers try to describe their perception of the disease. Not experiencing relevant symptoms or the impact of those symptoms on their lives, could make the disease invisible: “Since you don’t feel anything, it doesn’t matter” C56E11P21 “I don’t see any change, in other words, normal (the disease…) it is there, but it is stationary” C41 and C46 P12E2
The relationship with the disease, and particularly experiencing the disease, may cause in some teenagers a feeling of exclusivity in the way they experience the severity of the symptoms, giving rise to the idea that there are different types of lupus, but ratifying the opinion of several adolescents that the existence of SLE in their lives is conditioned by how aggressive the pathology is. “I believe that there are several types of lupus, but mine is like… I don’t know… tougher… The disease affects the body, but the most affected organs are the brain, the heart, the kidneys, and your vital signs.” C87E9P15
However, other adolescents seem to believe that lupus is a threatening disease and their involvement with their care could determine the behavior of the disease; this approach ignores invisibility or chance as factors at stake. This remark of being an active participant with regards to a chronic condition is interesting and suggests that autonomy is a relevant factor in the evolution of the disease. “If I don’t take care of my lupus, it will fight back” C52E11P21
Most adolescents mentioned the existence of unspecific symptoms at the onset of the disease. This perception is concerning, particularly during pre-adolescence, which is an evolving phase characterized by being sensitive to new experiences and ambivalence. Restlessness is then expected to prevail, as a manifestation of how confusing the onset of symptoms may be.
During the interviews, there is evidence of feeling adrift, going from one doctor to another, or frequent visits to the emergency department, trying to look for an answer. The feeling of distress and frustration present during this period of time, particularly when they have to go through multiple tests “that were always OK”, increased their perception of uncertainty because they felt ill bet there was nothing specific to explain their symptoms. “Yes, I was very sick since around September 2009, I was vomiting, with very severe joint pain, terrible headaches, so I had to go to the hospital very often…I always ended up in the emergency room” C19E4P5 “They said they never found anything” C49E9P11
Patients often expect that the test results will be final to make a diagnosis. When several adolescents discuss the fact that the initial paraclinical tests were not final, or that these were usually interpreted as “normal”, this is an indication that doing a lot of tests, does not necessarily mean “doing the right tests”, or that the results are properly interpreted in the light of the clinical presentation. “In the hospital they told me they were going to do some studies to find out whether it was arthritis, because my hands were swollen and extremely painful. But that was it, and they never did anything” C22E4P5
A diagnostic process may be complex, not just due to the characteristics of the physical symptoms that occasionally may be vague, but also due to the expectations and perceptions of those experiencing the symptoms. A number of the adolescents interviewed referred to time and a stationary evolution of the disease, as another contributing factor to the feeling of uncertainty and being “adrift”: “Feeling that time moves on without any improvement of symptoms” C23E4P5
The expectations regarding the evolution of a particular clinical condition depend not only on the emotions unleashed at the time the diagnosis is received, but also on the information communicated and the adequate guidance to deal with the symptoms and signs you exhibit when you go to the doctor. In the case of the teenagers interviewed, the following seemed to be the relevant aspects: “We were told that probably I had dengue, but it was hemorrhagic dengue. But how could it be hemorrhagic dengue if I had never experienced any bleeding? So that was not an explanation for the rapid drop in platelet count… that's what they said and the continued doing tests, inserting needles, and then… a lady doctor told my mother that she had to be very careful with me because my symptoms were similar to leukemia” C93-95E6P13.
Among these perceptions during the diagnostic phase, patients also recriminate the healthcare staff for trying to minimize their symptoms, that in the end were manifestations of a severe disease: “They just kept saying that it was a fever, high temperature, a cold, so they send me home with the usual medicines” C48E9P11”
The communication that physicians and nursing staff establish with patients evaluated for diagnosis, may have a strong impact on the patient's perception about whether a systematic interpretation is being done about their symptoms, or if they are being treated randomly, as evidenced by the following code: “They were not looking for this disease; in other words, the tests said I had Lupus, without even thinking about it” C3E8P4
A person that has been previously in contact with SLE may have representations about the disease, its onset, and even its behavior; this makes a difference in the way the onset of SLE is experienced and lessens the feeling of uncertainty, inasmuch as the identification of some signs or signals is facilitated. This was the opinion of a teenager diagnosed with lupus. She said that the family recognized the symptoms early due to her mother's past experiences. “My mother asked for an appointment for me because she suspected the disease since she has the same condition” C2E5P2
Tactfulness in dealing with the information and communicating the diagnosis is essential, not only in terms of how the adolescents feel in the doctor–patient relationship, but also in terms of how they perceive they are being managed: as participating subjects and recipients of information about their disease, or rather excluded, with the family being the exclusive recipients of the information regarding the diagnosis. This aspect should be analyzed afterwards, since it may be one of the foundations that leads to the child or adolescent accepting the SLE diagnosis and assuming responsibility for his/her care. “No, they were addressing my aunt who had been with me over the last few days” C28E10P8
The way the adolescent accepts the diagnosis is not always determined by the initial doctor-patient communication; the role of the family and the attitude to communicate the information, or the filters used with protective or compassionate purposes, also play a role. Sometimes, teenagers interpret their health situation based on reading the gestures or emotions of their parents; this means that information is inferred: “Although my mother never told me anything … you always notice when your mother doesn’t feel well” C95E6P13 “I was told I had lupus and my mother … well she didn’t want to tell me anything” C21E7P7
This category comprises the constructs and expressions of teenagers with regards to their experiences with SLE in terms of change; the following sub-categories emerged: image changes, changes in the way they face life, a feeling of limitation and being treated differently.
Changes in self-image after the diagnosis
The most relevant perceptions in terms of changes were expressed in terms of how adolescents see themselves, their self-representations that make reference to changes in personality and behavior, with characteristics such as introversion, irritability, changes in attitude, and a tendency to be perfect in their academic performance.
The feeling of change even includes behavioral changes, with observations about their ability to communicate spontaneously, expressiveness, and even their personal worth. “After the disease I became extremely perfectionist” C147E4P15 “When I feel sick, generally I just remain silent” C67E1P20 “Lupus made me shy in the sense that I felt inferior to others” C125E6P15
Changes in the way you view your life
There are repeated references to a failure to identify any lifestyle changes after the diagnosis, leading to avoidance in response to the severity of the condition and even in contrast to what was expressed in other categories (see previous paragraphs). Some teenagers claimed that when they became aware of the diagnosis, that did not change their lifestyle at all; however, when doing the analysis, some aspects show the impact on their daily life, the need to change their care routines due to the schedule for taking their medications, the frequency of laboratory tests, extended hospital stays due to complications, and the need for frequent medical control visits, all of which impact their daily life and some aspects of family life. “Taking seven medicines per day is life-changing” C121E6P15 “Having lupus increased the family expenditures” C196E6P2
So, adolescents experience relevant changes in their lives, some of them totally new and affecting their motivation, and others that make a difference in their teenage lives as compared to their peers, specifically affecting their social interactions – for instance, having to stay at home for long periods of time –. In sum, teenagers refer to a “complicated life” after the diagnosis. “Before the diagnosis, there was no need to protect myself against sunlight” C16E9P13 “Living with lupus is complicated because of the medicines and the medical appointments” C33E3P5
Feeling your limitations and being treated differently
In addition to the impact of lupus on their lives, we identified another category expressing the feeling of loss when living with lupus, which teenagers express when referring to things they can no longer do, or giving up things they used to enjoy. After the diagnosis they mention the need to quit some sports – even highly competitive sports – or limiting other leisure activities because they interpret them as risky for their health; they have to take additional precautions and reflect more on their actions. “Having lupus prevents you from doing things you like a lot” C149E5P22 “With lupus, many things are forbidden” C111E9P19
The teenagers interviewed describe representations regarding experiencing the disease, that make them different from the rest or make them feel more vulnerable. This perception of being different from their peers is recognized as a difficult event, as well as the perceived limitation imposed by others as a result of the diagnosis or its complications. “Recognizing yourself as being different is difficult” C34E7P8 “Lupus makes me different” C63E4P8 “Being sick makes others impose limitations on me” C68E4P8 “I couldn’t be like the rest of them” C30E7P8
Some of the interviewees ask themselves questions attempting to find an answer to their new condition, which not only involves or results in losses with regards to their previous lifestyle at the start of the disease, but readapting to new situations and routines that alter their daily life. While questioning anything that changes our lives is natural to the human condition, in the teenagers interviewed this looks like complaining about life as a way to express their dissatisfaction and perplexity, in an attempt to explore whether there are any predetermined events in life that make them eligible to develop a potentially severe disease. Through their questioning, they wonder whether they deserve their lupus. “Why it had to be me when there are so many other children?” C20E1P7 “Why bad things happen to me?” C288E4P36
In their narrative about the experience of living with SLE, there are also references to “the good things about lupus”. While during the interviews the initial reaction in some of the participants was to say “there is absolutely nothing good about lupus”, then they move on to talk about the positives.
According to a young girl, lupus becomes a behavior modulator that seems to calm you down. Another teenager said that having the disease enables the development of some traits that then become advantageous for your personality. In the opinion of others, lupus has enabled them to learn about self-care and how your body works: “You become restrained” C103E11P33 “Having lupus helps you in many ways: makes you more responsible” C95P20E2 “Some of the good things about lupus is learning to take care of myself and knowing things about my body” C290E4P37
While breaking the rules in performing any activity may be a problem, not just for the offender but also for the activity itself, a teenager thinks that being ill is advantageous to skirt some school responsibilities; these are “secondary gains” from her condition, for her own benefit: “Taking advantage of the disease as an excuse to bypass the school's rules” C137P34E2
The perceptions of the disease by adolescents with SLE who are about to transition to adult care reflect the experience accumulated from childhood, with a condition that is difficult to understand in terms of its causes and consequences. In a way, their teenage years have been different from their peers as a result of the disease. An isolated event does not make an experience or a moment in life, but rather the representations thereof; in this case, adolescents with SLE experience life differently from their peers.
Leventhal's self-regulation model suggests that illness cognitions derive from an implicit model of disease based on believes about such diseases, knowledge, experience, and information received from third parties.11 Initially three different emerging categories associated with the perceptions about the disease were identified in this paper.
An analysis of the categories referring to the attempt to explain the origin of lupus, contrary to the paper by Goodman et al.,23 in which several patients interviewed wouldn’t dare to speculate, in this paper we were able to identify codes related to the potential causes in almost all of the interviews analyzed. A number of teenagers referred to the poor function of the immune system as the cause of the disease.
The idea of “low defenses” emerges in this context but this was not recorded in other similar studies reviewed.17,18,23 The concept of “low defenses” as the etiology of the disease is inaccurate, and reflects the confusion that teenagers with SLE may experience, with regards to the pathophysiology of the disease and the interpretation of treatment effects.
The characterization of the autoimmune and self-destruction processes which is made evident in our study when analyzing the concept of “defenses” as the cause of the disease, has been reported by other investigators in similar studies.17 Barrier,24 in his work “el Cuerpo Enfermo, el Cuerpo Testigo” (the ailing body, the witness body), when examining the transformation of the representations of the ailing body in a patient with a chronic condition, refers to the idea of “partial organic suicide” when talking about his own experience as a patient suffering from an autoimmune disease; he poses the following question: “Should it be considered the biological end of a pathological identity crisis?” The concepts “self-attack” and “autoimmunity” are consistent with the current pathophysiological concept and most probably, the fact that teenagers talk about them is the result of the information received from the healthcare team.
According to some of the adolescents interviewed, lupus is initially represented as cancer. Some authors have made reference to this fact in other studies,17 explaining that since lupus is not a familiar disease, there is a tendency to compare it to other more frequent chronic conditions such as cancer. In our setting, the use of immunosuppressive agents such as cyclophosphamide and methotrexate in SLE treatment regimes, which are also used in different anti-cancer chemotherapeutic protocols, may contribute to such representation. A similar situation arises with the believes that the people close to the patients and their families share, combining some symptoms, chronic evolution, and physical changes (hair loss) in the context of a malignancy. However, in the mind of adolescents, there is a difference between these two conditions and they even say that lupus is “like cancer, but tinier”, probably referring to the differences in severity and treatment response.
Guilt exists as a sub-category, within the framework of attributing the disease to behaviors that adolescents consider harmful and in their opinion may have triggered the onset of the disease; this gives rise to a significant emotional burden, that sometimes governs their experience with SLE. Usual childhood or teenager activities such as swimming, sun bathing, eating ad lib., may become punitive, inasmuch as these are associated with the limitations – or inability – to perform these same activities as a result of the disease; this helps patients to find their own explanation to the potential origin of their diagnosis. Strauss, quoted by Gaille,25 describes the situation as follows: “Whenever a chronic illness develops, the perceptions derived from the body's failure and the body's physiological function at the cell level (…), a failing body, usually leads the patient to wonder what he/she – or someone else did – to cause such situation.
Sometimes guilt becomes a defensive feeling against the anxiety generated by all the disease-associated changes, in an attempt to find an explanation to the fact that the patient suffers from a potentially risky disease. Occasionally it is even associated with unacceptable ethical behavior or morality, for instance, disobeying your mother. Taïeb et al.,17 also mention this fact in their study saying that a diagnosis of lupus prompts the patient “to look into his/her past to identify improper or inadequate behaviors – in accordance with their individual moral standards – for which they were punished with the onset of their disease”.
The perception among several interviewees that “there are several classes of lupus” may be associated with their cognitive analysis of the experience, so that based on the knowledge acquired about the various disease manifestations, they try to represent it in terms of more or less severe. This intellectual compromise mentioned by Piaget,26 whereby “the individual must reassemble his/her comprehension, integrating both reality and experience”, could be the explanation to their efforts to adapt to a new illness affecting their lives and marks the beginning of their initial understanding of the disease. Tunnicliffe et al.,18 found that the teenagers interviewed “reassess the severity of the disease” and say that they have “normal days”, when the disease is not active, consistent with our findings in terms of “invisible disease”.
The association between the onset of lupus or worsening of the symptoms with stressing events in their personal or family life was mentioned by some of the interviewees. Such events highlight the importance of stress in the development of disease, attempting to find an explanation to their condition, and is perceived as an intruder in their lives. As mentioned by Taïeb at al.17 quoting Williams and Wood: “The object of interpretation is not only the disease itself, but also the disruption in the course of life”.
The feeling of rupture and change marks the onset of the disease, not only as a disrupttor at a particular point in time, but also because the onset of the disease involves another important factor: time. Rocheblave-Spenlé26 argues that teenagers perceive time differently from children; adolescents are aware of the concept of continuity, and this leads them to understand that life is limited. This could explain the concern expressed by some adolescents with regards to extended periods of time with symptoms for which no cause is identified, or mistaken opinions that play down their symptoms or attribute the symptomatology to other illnesses. Sutanto et al.,15 in their summary of qualitative studies on the experiences and prospects of adults with lupus, mention in the category of “identity disruption” how some patients “felt ignored by their doctors and were accused of being hypochondriacs”. The study by Tunnicliffe et al.,18 mentions “resentment” due to the delay in making the diagnosis, which caused confusion and uncertainty. Playing down symptoms due to their “invisible nature”, was also mentioned by these investigators, and is also a fact in our study, not just in terms of symptoms, but also with regards to the tests conducted, which according to the adolescents “were normal”.
The low incidence of SLE in children and youth represents a challenge for primary care doctors who are not familiar with rheumatologic conditions in pediatric patients. This lack of awareness of the disease has been evidenced in another rheumatologic disease: juvenile idiopathic arthritis, and is one of the barriers to access the pediatric rheumatologist and to have a timely diagnosis.27 Dias Araujo and Traverso Yepez,28 in their study on expressions and meanings of SLE, show that even in adults, making a diagnosis is also an issue; partly this may be due to the diversity of symptoms that accounts for potential misdiagnoses – an opinion shared by several other researchers.14
Having a family history of SLE helped the parents of the teenagers interviewed to identify the symptoms because they were able to recognize beforehand the probable onset of lupus. This is not only beneficial for the teenager in terms of early and timely detection of the clinical manifestations of the disease, but also in terms of facilitating the process of adaptation to the changes inherent to living with a chronic and high-impact disease, in addition to not feeling lonely but cared for by a support network, in an environment that gives them confidence to live with their condition. Tunnicliffe et al.,18 also refer to this fact in their study; they say that adolescents feel “indebted” with their families inasmuch as they depend on their support to access treatment and receive information about the disease.
All of these patients are diagnosed as children, so family plays a very important role in establishing the meaning of the disease; however, the “protective” role can be confusing when expecting that the child should be ignorant of his/her clinical condition, forgetting that the child as “individual in suffering” perceives the changes in his/her routine and associates those changes with something that “is not right”, even if initially he/she is not aware of all the implications of the diagnosis, as mentioned in this paper. In this regard, Grau and Fernández,29 say that the overprotected child captures his/her privileged position in the family, confirming the feeling of a fragile existence. Moreover, the child also acknowledges the issues parents face when discussing the disease and therapy.
Under the “what you miss” category, teenagers make representations about the changes they experience upon the diagnosis of lupus. The changes that involve restrictions make the patients represent the experience of the disease in terms of loss and being different from their peers, in addition to associating any medical complications with future limitations. Coscollá et al.,30 also make reference to the impact of the disease in terms of its limitations, referring to the inability to practice sports and leisure activities. These limitations to perform the same activities as their peers may give rise to social integration issues. Such perception is also mentioned by Tunnicliffe et al.,18 who include “feeling of isolation” and the limitation experienced by children and young adults with LSE as one of their categories, being unable to participate in a number of social activities. Repeatedly these patients feel that having SLE introduces changes in their daily life and in their routines, versus how they used to live before the diagnosis. This may even lead to a feeling of anticipation of those changes and mood reactions. According to Dias Araújo and Traverso-Yépez,28 the effect of these changes on their quality of life will depend on the context, the support they perceive, and coexisting with the disease for some time.
This study identified a few expressions associated with positive aspects in the midst of the negative representations of the disease; McElhone et al.,31 in their research on adult female patients, also identified a number of positive aspects, such as building strong friendships in the framework of the disease, and secondary gains, as previously mentioned. Coscollá et al.,30 mention in their publication personal maturity and social support as positive consequences of the disease. Tunnicliffe et al.,18 identify in their research some categories associated with improved resilience and the ability to cope.
This study discussed the preliminary results of a small sample of adolescents with SLE about to transition into adult care, and is not intended to generalize the perceptions of the disease in this population. Considering that the initial categories are not saturated, probably other relevant categories will emerge in the future, as new interviews are conducted and the script is adapted accordingly. However, the contributions so far are valuable for the objective established and pave the way to further explore the emerging representations in adolescents with SLE and their life experience with the disease.
ConclusionsThe perceptions of the disease among these teenagers with lupus are manifested through the experience of change due to the implications inherent to the diagnosis. Such transformations are experienced daily and have an impact on self-image, on their relationships with parents, friends, treating physicians, and involve feelings of uncertainty and the need to make changes to adapt to new routines imposed by their clinical condition. So many changes and restrictions lead them to seek explanations that sometimes are expressed through guilt of all kinds of nuances, shaping the origin of the disease that has so radically transformed their lives.
Healthcare professionals and families are required to become aware of the perceptions that adolescents with SLE, who are transitioning to adult care, have about the disease; these perceptions, in addition to other factors, shall determine the strategies they will develop to ensure their self-care and adaptation to the situations resulting from living with the disease.
FinancingThis paper was funded by the Colombian Association of Rheumatology.
Conflict of interestThe authors have no conflict of interest to disclose.
Please cite this article as: Hernández Zapata LJ, Alzate Vanegas SI, Eraso RM, Yepes Delgado CE. Lupus, «un cáncer pero más chiquito». Percepciones del lupus eritematoso sistémico en adolescentes próximos a la transición. Rev Colomb Reumatol. 2018;25:151–160.
The term used in the original article is “coping”. According to Pimm,13 “coping, in the context of rheumatology diseases may include the efforts to improve symptoms or reduce the disability (for instance, taking the medication, taking rest, exercising) or to reduce the emotional impact of the disease”.
The term used is “appraisal”. According to Pimm,13 appraisals in the context of rheumatology diseases include the perception of the individual's own ability to display coping behaviors and the evaluation of the success of such strategies in regulating emotional wellbeing, symptoms such as pain and fatigue, and functional capacity”.