Adult-onset Still’s disease is a rare inflammatory disorder with multiple forms of manifestation; however, the onset with myocarditis or pericarditis is even less common (7% prevalence). Herein, we present a case of a previously healthy 30-year-old man, who consulted for chest pain. During his clinical evolution, he was diagnosed with myopericarditis. Various aetiologies were evaluated and after multiple studies adult-onset Still’s disease was diagnosed. Treatment with corticosteroids was established evidencing an adequate response.
La enfermedad de Still es una enfermedad inflamatoria infrecuente, con múltiples formas de presentación; sin embargo, el debut con miocarditis o pericarditis es aún menos común (prevalencia de 7%). A continuación, se presenta el caso de un hombre de 30 años, previamente sano, que consultó por dolor torácico. Durante su evolución clínica fue diagnosticado con miopericarditis, se indagó en diversas etiologías, pero luego de múltiples estudios se diagnosticó con enfermedad de Still del adulto; se instauró tratamiento con corticoesteroides, el cual tuvo una adecuada respuesta.
Adult-onset Still's disease (AOSD) is a rare inflammatory disorder. Its worldwide prevalence ranges between 0.16−0.4/100,000 people,1 and in Colombia, although the prevalence has not been established, a series of cases from 2016 reported 17 cases in 5 years of follow-up.2 Its clinical expression generally consists of fever ≥39 °C, salmon-pink evanescent rash, and joint involvement.3 It could be accompanied by disseminated intravascular coagulation, macrophage activation syndrome, lymphadenopathy, hepatomegaly, splenomegaly, purpura, pneumonitis, and, in exceptional cases, serositis or myocarditis.3–5 Pleuropericardial affection appears in between 15 and 40% of cases, mainly as pericarditis,5,6 and the disease onset with myocarditis has been reported isolatedly, with an estimated prevalence of 7% worldwide, but with potentially fatal outcomes.3,5 Considering its exotic manifestation, a brief description of a case with myopericarditis in the context of AOSD is presented.
Case presentationA 30-year-old male (1.75 m, 70 kg) was admitted to the emergency department reporting retrosternal chest pain of 10 h evolution, intensity 8/10 on the visual analog scale, constant, even at rest, associated with dyspnea that worsened when breathing.
Upon review by systems, he mentioned intermittent fever of 4 days of evolution, without predominance of time, non-pruritic evanescent plaques that disappeared with acupressure over extremities, thorax, abdomen, and buttocks that worsened with fever; in addition, he refers myalgia, migratory polyarthralgia of small and large joints without synovitis, for 2 weeks. The patient was previously healthy and worked as a police officer in the Colombian tropics. Vital signs on admission revealed tachycardia (140 bpm) and fever (38.4 °C); the rest of the physical examination was unremarkable.
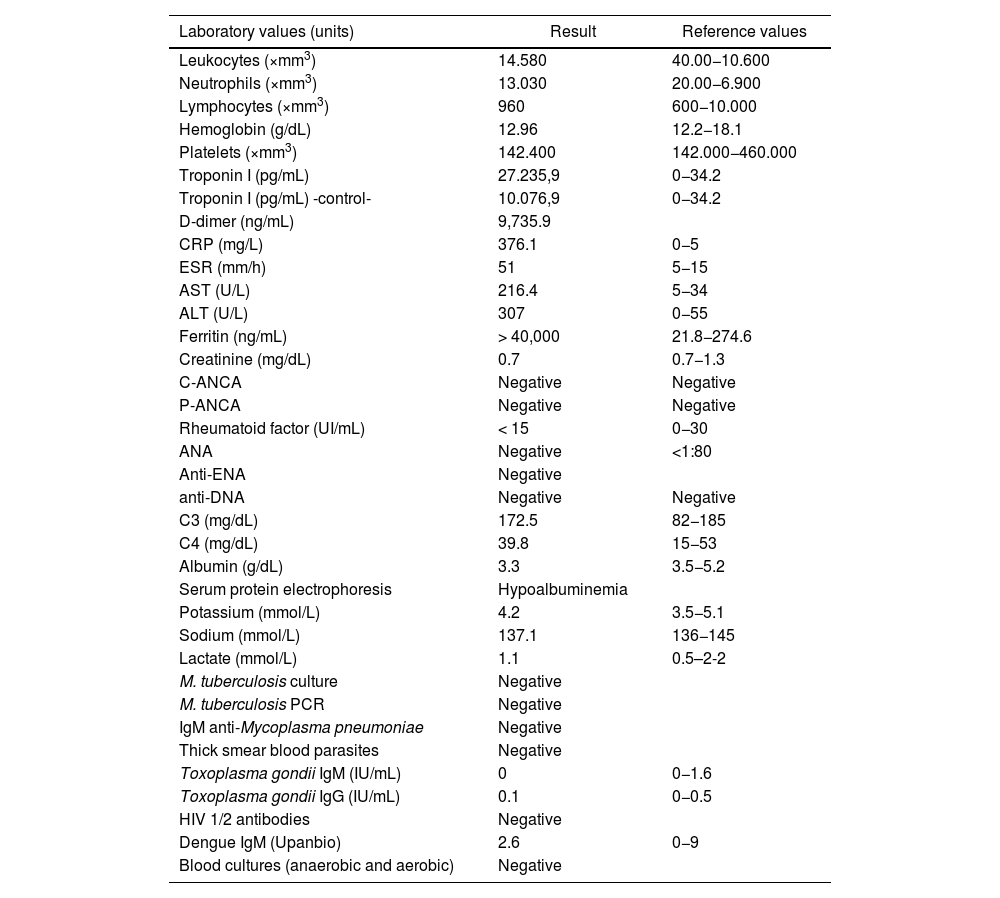
The 12-lead electrocardiogram revealed sinus tachycardia and repolarization disorder in the inferior face. Lab tests showed positive troponin I (27.235.9 pg/dL) and delta −63% (10.076.9 pg/mL), with D-dimer at 9.735 ng/mL, elevated transaminases, and acute-phase reactants (RCP, leukocytes, ESR) (Table 1). Chest X-rays depict a bilateral pleural effusion (PE) persistent on the tomography at this level, as well as pericardial effusion (PeE), and the echocardiogram revealed left ventricular midsegment lateral hipokynesia, left ventricular ejection fraction (LVEF) of 58%, mild tricuspid regurgitation, and PeE.
Paraclinical findings of the patient.
| Laboratory values (units) | Result | Reference values |
|---|---|---|
| Leukocytes (×mm3) | 14.580 | 40.00−10.600 |
| Neutrophils (×mm3) | 13.030 | 20.00−6.900 |
| Lymphocytes (×mm3) | 960 | 600−10.000 |
| Hemoglobin (g/dL) | 12.96 | 12.2−18.1 |
| Platelets (×mm3) | 142.400 | 142.000−460.000 |
| Troponin I (pg/mL) | 27.235,9 | 0−34.2 |
| Troponin I (pg/mL) -control- | 10.076,9 | 0−34.2 |
| D-dimer (ng/mL) | 9,735.9 | |
| CRP (mg/L) | 376.1 | 0−5 |
| ESR (mm/h) | 51 | 5−15 |
| AST (U/L) | 216.4 | 5−34 |
| ALT (U/L) | 307 | 0−55 |
| Ferritin (ng/mL) | > 40,000 | 21.8−274.6 |
| Creatinine (mg/dL) | 0.7 | 0.7−1.3 |
| C-ANCA | Negative | Negative |
| P-ANCA | Negative | Negative |
| Rheumatoid factor (UI/mL) | < 15 | 0−30 |
| ANA | Negative | <1:80 |
| Anti-ENA | Negative | |
| anti-DNA | Negative | Negative |
| C3 (mg/dL) | 172.5 | 82−185 |
| C4 (mg/dL) | 39.8 | 15−53 |
| Albumin (g/dL) | 3.3 | 3.5−5.2 |
| Serum protein electrophoresis | Hypoalbuminemia | |
| Potassium (mmol/L) | 4.2 | 3.5−5.1 |
| Sodium (mmol/L) | 137.1 | 136−145 |
| Lactate (mmol/L) | 1.1 | 0.5–2-2 |
| M. tuberculosis culture | Negative | |
| M. tuberculosis PCR | Negative | |
| IgM anti-Mycoplasma pneumoniae | Negative | |
| Thick smear blood parasites | Negative | |
| Toxoplasma gondii IgM (IU/mL) | 0 | 0−1.6 |
| Toxoplasma gondii IgG (IU/mL) | 0.1 | 0−0.5 |
| HIV 1/2 antibodies | Negative | |
| Dengue IgM (Upanbio) | 2.6 | 0−9 |
| Blood cultures (anaerobic and aerobic) | Negative |
CRP: C-reactive protein; ESR: erythrosedimentation rate; ANCA: anti-neutrophil cytoplasm antibodies; ENA: extractable nuclear antibodies; PCR: polymerase-chain reaction.
Given the findings and clinical manifestations of the patient, it was decided to rule out an infectious cause of pericarditis and acute myocarditis; toxoplasmosis, human immunodeficiency virus, malaria, tuberculosis, hepatitis B and C, dengue, and Trypanosoma cruzi, among others, were discarded; blood cultures for aerobic and anaerobic microorganisms were negative (Table 1) and abdominal images (ultrasound and contrast-enhanced tomography) were normal.
After a 15-day hospital length of stay, persistent fever with a temperature up to 39−40 °C (1–2 episodes per day) occurred, without a documented infectious etiology. An autoimmunity work-up was requested: ANA, ENA, anti-DNA, ANCA, rheumatoid factor, and complement reports were negative. Ferritin was above 40,000 μg/L and C-reactive protein was elevated (376.1 mg/dL) (Table 1). Cardiac magnetic resonance imaging (C-MRI) was not performed.
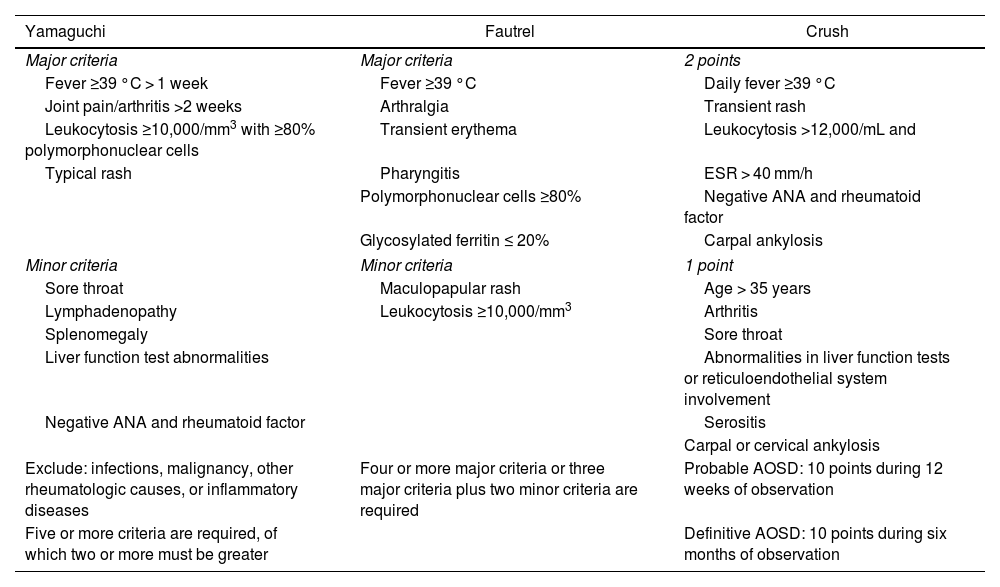
As described, AOSD was diagnosed according to the Yamaguchi et al.7 and Fautrel et al.8 criteria (Table 2). Prednisolone 50 mg QD and naproxen 250 mg TID were started, with clinical improvement in the following 72 h, disappearance of skin lesions, absence of fever, and improvement of joint pain. He was discharged at this term with follow-up by Rheumatology.
Classification criteria.
| Yamaguchi | Fautrel | Crush |
|---|---|---|
| Major criteria | Major criteria | 2 points |
| Fever ≥39 °C > 1 week | Fever ≥39 °C | Daily fever ≥39 °C |
| Joint pain/arthritis >2 weeks | Arthralgia | Transient rash |
| Leukocytosis ≥10,000/mm3 with ≥80% polymorphonuclear cells | Transient erythema | Leukocytosis >12,000/mL and |
| Typical rash | Pharyngitis | ESR > 40 mm/h |
| Polymorphonuclear cells ≥80% | Negative ANA and rheumatoid factor | |
| Glycosylated ferritin ≤ 20% | Carpal ankylosis | |
| Minor criteria | Minor criteria | 1 point |
| Sore throat | Maculopapular rash | Age > 35 years |
| Lymphadenopathy | Leukocytosis ≥10,000/mm3 | Arthritis |
| Splenomegaly | Sore throat | |
| Liver function test abnormalities | Abnormalities in liver function tests or reticuloendothelial system involvement | |
| Negative ANA and rheumatoid factor | Serositis | |
| Carpal or cervical ankylosis | ||
| Exclude: infections, malignancy, other rheumatologic causes, or inflammatory diseases | Four or more major criteria or three major criteria plus two minor criteria are required | Probable AOSD: 10 points during 12 weeks of observation |
| Five or more criteria are required, of which two or more must be greater | Definitive AOSD: 10 points during six months of observation | |
Adapted from Giacomelli et al.18
ANA: antinuclear antibodies; ESR: erythrosedimentation rate; AOSD: adult-onset Still disease.
AOSD is a rare inflammatory disorder; it is a diagnosis of exclusion after ruling out other etiologies under the study of fever of unknown origin, as was carried out with the patient in this case, who finally met four major and two minor Yamaguchi et al.7 and Fautrel et al.8 criteria; the Crush et al.9 criteria were not assessed, given the requirement of long period follow-up; our approach, in this case, was acute.
The debut of AOSD with myopericarditis has the lowest prevalence among complications,10 with a lower age of onset than other causes of myocarditis.11 Recent studies suggest that the gender ratio is relatively balanced for AOSD,12 but myocarditis predominates in women.13
The reactive component to infections with the release of inflammatory cytokines has been widely described5 and may be related to elevated acute-phase reactants, as in the current case in which, although consistent with other reports,2,3,5 in this case, are above these.
Troponin was a useful marker in the initial approach to the patient, considering that its elevation has been documented in up to 94% of AOSD myocarditis, but it does not have marked elevation in other etiologies5; in these cases, it is useful to perform C-MRI, which would be expected to have findings compatible with myocardial inflammation and compliance with the criteria described by the International Consensus on Cardiovascular Magnetic Resonance in Myocarditis14; however, this resource was not available at the institution.
Pericardial effusion is expected to be found in up to 40% of cases15 and, although it is not usual, cardiac tamponade has even been reported.16
Treatment is based on corticosteroids, nonsteroidal anti-inflammatory drugs, and antirheumatic drugs, reserving the use of anti-cytokines (IL-1, IL-6, Il-18, TNF) for refractory or life-threatening cases.5,17 The patient, in this case, responded satisfactorily to 50 mg of prednisolone QD, which is compatible with other studies, in which 60% are managed only with this first-line18,19; this allowed early discharge once the diagnosis was reached, avoiding fatal complications described in up to 4.2% per year.5
ConclusionMyopericarditis is a rare manifestation of AOSD, which makes early diagnosis difficult; however, it should be considered, since the establishment of timely treatment leads to good results.
Ethical responsibilitiesThis document was approved by the Ethics Committee of the Hospital Universitario Clinica San Rafael de Bogota, Colombia; the patient signed informed consent for the publication of the case.
FinancingOwn resources.
Conflict of interestsNone.