The Raynaud phenomenon is a clinical disorder, characterized by episodic attacks of vasospasm of peripheral arteries and arterioles, causing tissue ischemia of distal portions of the body, such as hands and feet, causing changes in skin color such as pallor, cyanosis and hyperemia. The occurrence of the Raynaud phenomenon in people who handle organic solvents or vibratory tools has been associated for a long time, and it has even been described that the solvents may be triggering some immune diseases such as scleroderma, however, as far as we know there are no reports of exposure of chemical compounds used in metallurgy, such as nitric acid and the development of scleroderma-spectrum diseases. This article presents a clinical case related to the appearance of Raynaud's phenomenon against exposure to chemical compounds used in metallurgy, especially nitric acid.
El fenómeno de Raynaud es un trastorno clínico, caracterizado por ataques episódicos de vasoespasmo de arterias y arteriolas periféricas, causando así isquemia tisular de porciones distales del cuerpo, como manos y pies, produciendo cambios en la coloración de la piel como: palidez, cianosis e hiperemia. Se ha asociado la aparición del fenómeno de Raynaud en personas que manipulan solventes orgánicos o herramientas vibratorias por un largo período, incluso se ha descrito que los solventes pueden ser gatilladores de algunas enfermedades inmunológicas como la esclerodermia, sin embargo, hasta donde conocemos no existen reportes de la exposición de compuestos químicos utilizados en la metalurgia, como el ácido nítrico y el desarrollo de enfermedades de espectro esclerodérmico. En el presente artículo se presenta un caso clínico relacionado con la aparición de fenómeno de Raynaud frente a la exposición a compuestos químicos utilizados en la metalurgia, en especial al ácido nítrico.
The Raynaud phenomenon (RP) was described for the first time in the thesis of Maurice Raynaud, in 1962, as local ischemia of the hands, feet, nose and tongue, that may be accompanied by pain and which was due to obliteration of the vessels; he also described that this mechanism was associated with the microvascular commitment due to a defective innervation that leads to a loss of vascular tone.1
Hutchinson described the difference between the primary and secondary RP in different diseases,2 Brown and O’Leary demonstrated in 1965 the capillaroscopic abnormalities in patients with diagnosis of scleroderma who presented RP.3
Currently, the RP is defined as an episodic ischemic disorder in the fingers and toes, manifested by pallor, cyanosis and redness or the skin in response to stimuli such as cold or emotional stress.4 The pathophysiology of RP is not well defined, however, it has been established that it may be primary or secondary to a number of underlying clinical entities such as scleroderma. Among the possible pathophysiological mechanisms of RP there are three: vascular, neural and intravascular, described below:
- A.
Vascular: it involves the structure and function.
- •
Structural abnormalities: it is believed that there is a release of adhesion molecules, cytokines and growth factors, apoptosis of endothelial cells and activation of pericytes, which generate thickening of the vascular wall and decreased flow.5
- •
Functional abnormalities: endothelial damage is responsible for the functional alteration, due to the imbalance between vasodilation and vasoconstriction.6
- B.
Neural: it involves the deficiency of vasodilators (calcitonin gene-related peptide), activation of alpha-2-adrenoreceptors and components of the central nervous system.7,8
- C.
Intravascular: it involves abnormal platelet activation, altered fibrinolysis, activation of white blood cells, increased blood viscosity and oxidative stress.7
The exposure to organic solvents has been associated with the development of diseases of scleroderma pattern.9 The relationship with chlorinated solvents has been well established as a risk factor for the development of scleroderma and, generally, they are occupational exposures,10 however, there is no evidence of the association between exposure to chemicals used in metallurgy (nitric, sulfuric, phosphoric, hydrofluoric acids, sodium chloride, etc.) and the development of scleroderma-spectrum diseases. For this reason, we want to make known the clinical case of a patient who presented diffuse manifestations of scleroderma spectrum, after a prolonged occupational exposure to chemicals used in the detection and screening of gold, also called Pickling.
Clinical caseA 36-year-old female patient who attends the outpatient clinic or Rheumatology for presenting poorly defined generalized pain, sleep disorders, RP and arthralgia in the hands. She does not report personal or family pathological antecedents, and she consumes tobacco and alcohol occasionally.
She stated that her occupation is metallurgy, focused on gold screening with nitric acid and sodium chloride; she has been carrying out this activity for approximately 24 months. The patient refers changes of coloration in the hands that were triggered since the beginning of the contact with these substances despite she was using latex gloves.
On physical examination she presented hypersensitivity of 18/18 fibrositic points, RP, hypersensitivity in proximal interphalangeal joints without articular tumefaction.
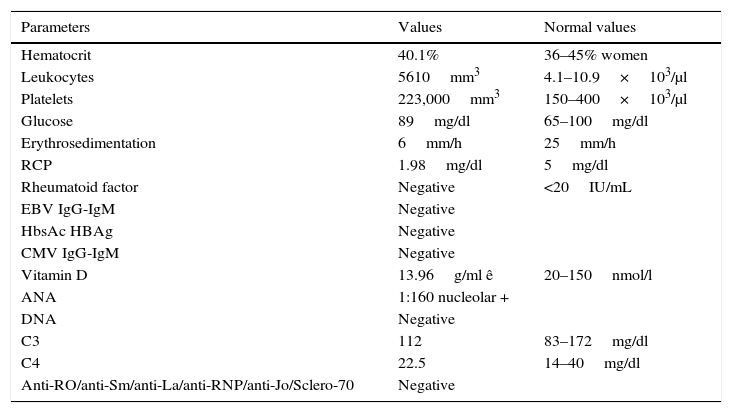
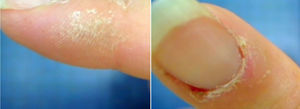
Scaly lesions were evident at the level of the fingers of the hands (Fig. 1), complementary laboratory studies (Table 1) and a videocapillaroscopy were requested. Two weeks later she returns to consultation because the generalized pain has increased; the physical examination showed tumefaction of the metacarpophalangeal and proximal interphalangeal joints (Fig. 2), accompanied by hypersensitivity in carpal joints and elbows, and also continued with all positive fibrositic points.
Complementary tests.
| Parameters | Values | Normal values |
|---|---|---|
| Hematocrit | 40.1% | 36–45% women |
| Leukocytes | 5610mm3 | 4.1–10.9×103/μl |
| Platelets | 223,000mm3 | 150–400×103/μl |
| Glucose | 89mg/dl | 65–100mg/dl |
| Erythrosedimentation | 6mm/h | 25mm/h |
| RCP | 1.98mg/dl | 5mg/dl |
| Rheumatoid factor | Negative | <20IU/mL |
| EBV IgG-IgM | Negative | |
| HbsAc HBAg | Negative | |
| CMV IgG-IgM | Negative | |
| Vitamin D | 13.96g/ml ê | 20–150nmol/l |
| ANA | 1:160 nucleolar + | |
| DNA | Negative | |
| C3 | 112 | 83–172mg/dl |
| C4 | 22.5 | 14–40mg/dl |
| Anti-RO/anti-Sm/anti-La/anti-RNP/anti-Jo/Sclero-70 | Negative | |
The patient reports that during the period between the first and the second visit she had palpebral edema on a trip to a cold weather area.
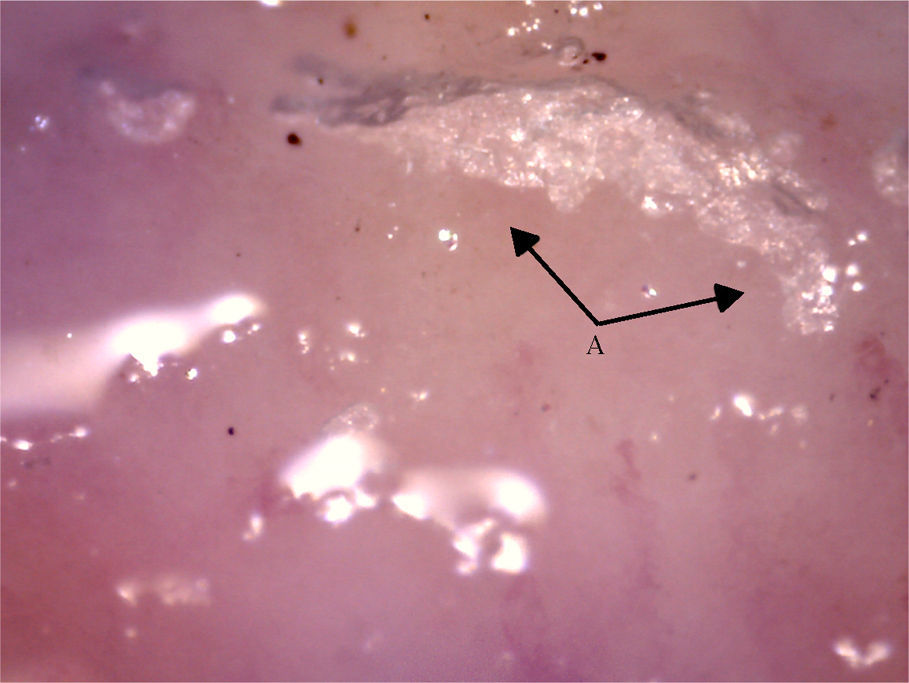
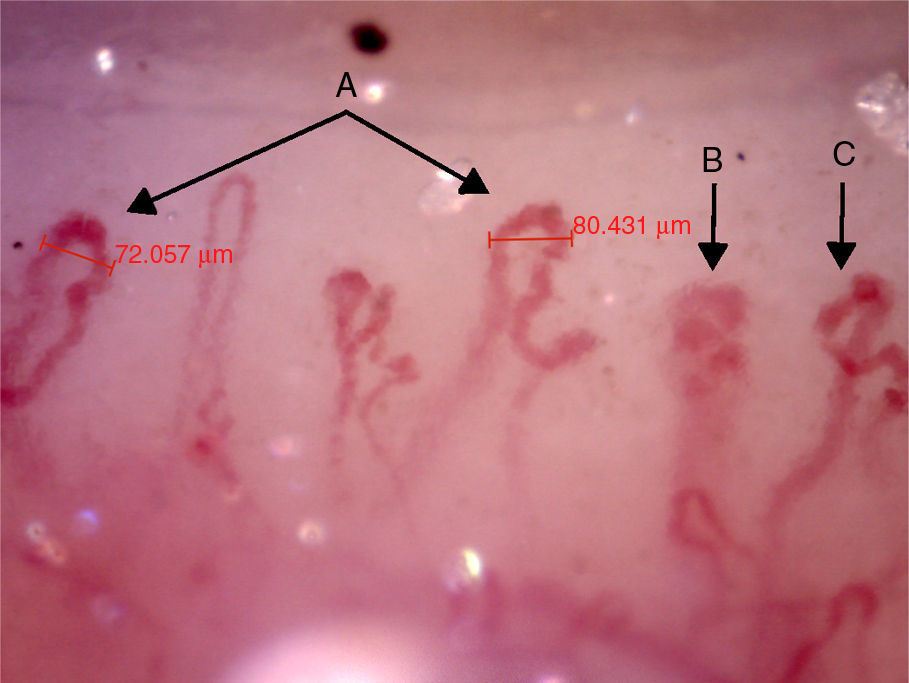
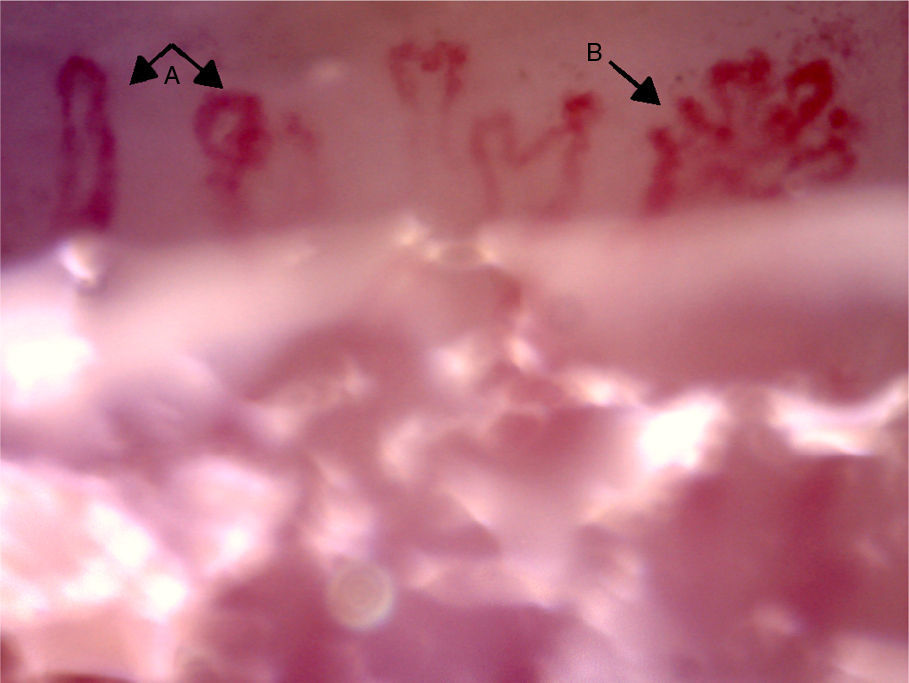
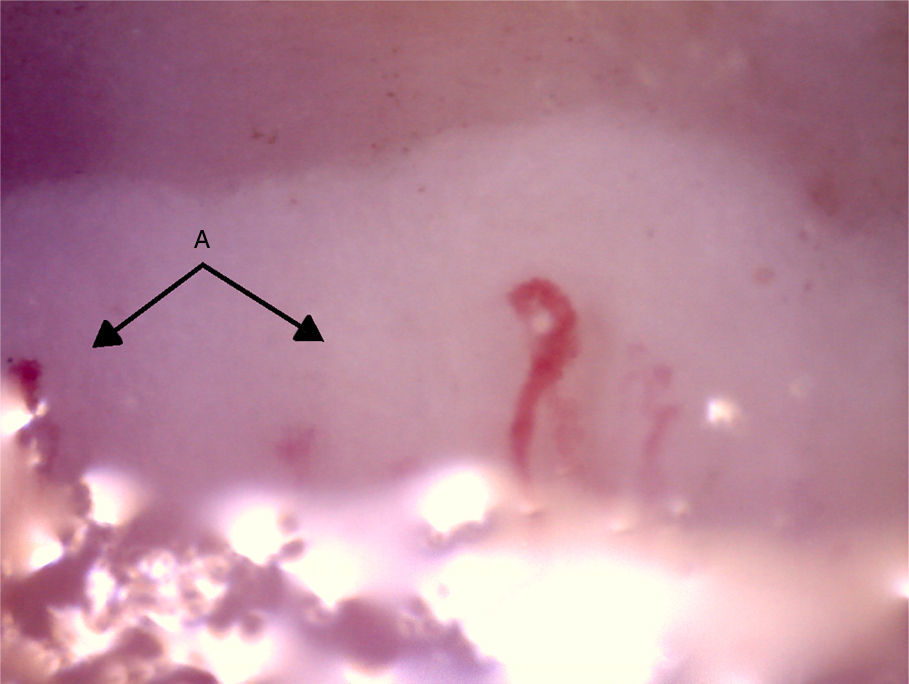
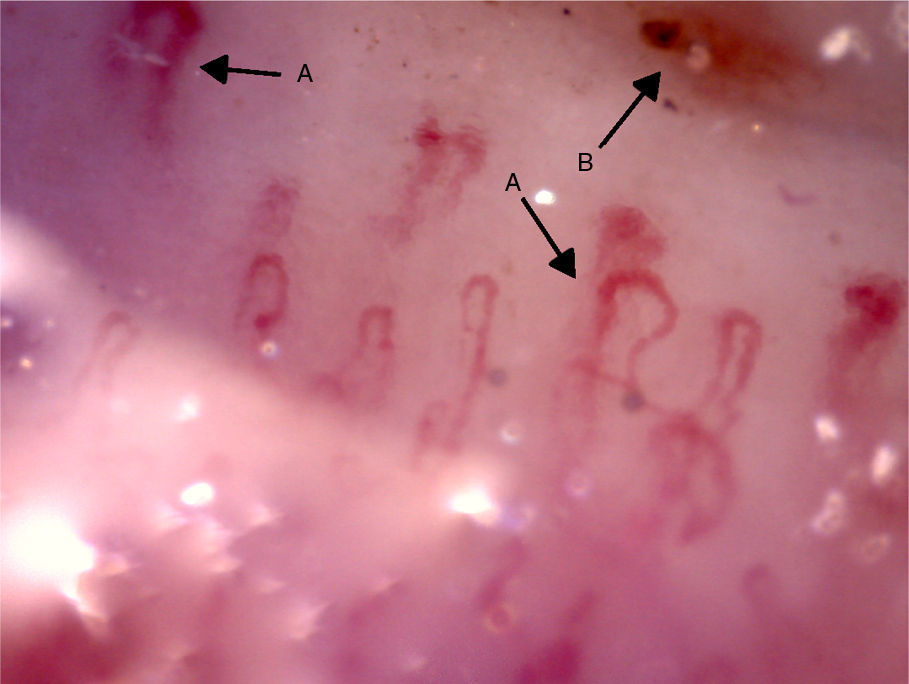
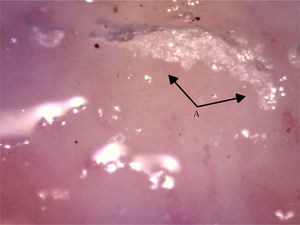
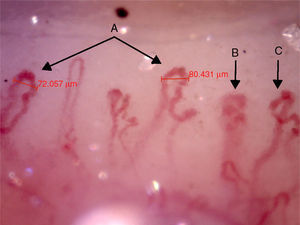
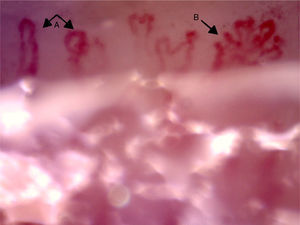
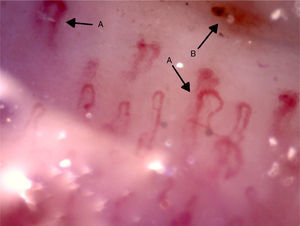
The videocapillaroscopy showed morphological alterations: decreased capillary density, criss-crossed and tortuous arborified capillaries, giant capillaries (72.05μm, 80.43μm), microhemorrhages, avascular zones and deposition of unidentified material; the capillaroscopy was interpreted as a SD-pattern in active status (Figs. 3–7). The patient reported not having used cosmetics or applying acrylics in a period of time longer than 12 months.
Capillaroscopy of the nail bed. A: giant capillaries; B: tortuous capillary; C: criss-crossed capillaries. The unidentified glue-like material affected the quality of the image by causing the reflection of light, and for this reason the images contain light reflections and dispersion.
Capillaroscopy of the nail bed. A: dilated capillaries; B: arborified capillary and loss of the capillary structure. The unidentified glue-like material affected the quality of the image by causing the reflection of light, and for this reason the images contain light reflections and dispersion.
As for the radiological evaluation, there was no evidence of joint damage and the bone structures were preserved, the performance of a skin biopsy was also suggested, however, the patient refused the procedure.
The patient was presenting a fibrositic picture and therefore she was receiving pregabalin 300mg/day; in addition, vasodilators (nifedipine 30mg/day) and mycophenolate mofetil (1.5g/day) were indicated, with improvement of the symptomatology.
DiscussionThe establishment of the true prevalence of RP is hampered by lack of a reproducible “gold standard” diagnostic test; however, according to the population surveys of different ethnic groups, its estimated prevalence is 3–20% in women and 3–14% in men, and the geographic variations reflect differences according to the local weather.11,12
Primary and secondary RP affects mainly the hands, the patients usually do not report symptoms in the lower limbs,13 and they describe a sudden episode of cold feeling in the fingers of the hands associated with a marked change in the skin coloration, which begins with pallor due to vasoconstriction, followed by cyanosis which indicates tissue hypoxia. This episode lasts approximately 15–20min until the patient heats the hands and the skin acquires a reddish color due to the reperfusion.
RP represents the first clinical sign of an alteration of the systemic vascular tone and the capillaroscopy is a non-invasive safe method that allows the visualization of the capillaries at the level of the nail bed,14 being a tool that allows to distinguish between the primary and secondary RP through microvascular patterns.4
The exposure to organic solvents has been associated with the development of diseases of scleroderma pattern,9 the relationship of chlorinated solvents has been well established as a risk factor for the development of scleroderma and, generally, they are occupational exposures,10 in which are handled solvents for paints, chemicals used in metallurgy, detergents or diluents whose active compounds are benzenes, toluenes, xylenes, aliphatic hydrocarbons, epoxy resins, perchloroethylene and vinyl chloride.9,15 Rein and Walder described, in 1957, the first case of systemic sclerosis associated with organic solvents16; a meta-analysis conducted by Barragán-Martínez demonstrated the relationship between organic solvents and different rheumatic diseases such as scleroderma, mixed connective tissue disease and systemic vasculitis.17
López carried out capillaroscopies in subjects exposed to vinyl chloride during 10 years and observed more capillaroscopic lesions than in the control group, among them dilated, criss-crossed, tortuous and arborified capillaries.18
In the field of metallurgy, chemical compounds are used for gold screening and treatment of impurities; these compounds include nitric, sulfuric, hydrochloric acids and sodium chloride. In the case of our patient, she was in direct contact with nitric acid and sodium chloride for approximately 24 months; during that period he was gradually presenting RP, polyarticular pain and tumefaction, palpebral edema and erythema accompanied by constitutional symptoms.
Nitric acid (HNO3), an inorganic compound, may come into contact with the user through inhalation or direct contact with the eyes or the skin; there are short-term adverse effects such as irritation of the eyes, mucosae and skin, and in its liquid presentation it can generate significant burns with permanent damage. A clinical sign of toxicity is the change in the coloration of the skin, intense yellow pigmentation is evident as it is the case of our patient, likewise, the long-term effects of this compound include erosion of the teeth19 and important pulmonary sequelae such as the adult respiratory distress syndrome; there are cases of this association described20–22; however, our patient did not provide data of breathing difficulty.
The symptomatology of the patient suggests that it is scleroderma-spectrum disease due to the presence of capillaroscopic alterations that make up an active SD pattern,23,24 positive antinuclear antibodies (1:160 nucleolar pattern) and puffy hands.
The patient presented antinuclear antibodies, nucleolar pattern, low titers, while the anti-Sclero-70 marker was negative; the presence of ANA nucleolar pattern in scleroderma is of 25–50%,25,26 the studies have demonstrated that the presence of a positive ANA and capillaroscopic alterations has a predictive value for the development of scleroderma-spectrum diseases of 12.6%.27
The videocapillaroscopy demonstrated capillary damage and capillaroscopic alterations suggestive of a connective tissue disease. According to the studies of Wu, the negative predictive value of capillaroscopy is approximately 94.12% for scleroderma, 80.77% for systemic lupus erithematosus, 96.30% for polymyositis/dermatomyositis, and 93.10% for mixed connective tissue disease.28
The differential diagnosis with other collagenopathies such as systemic lupus erythematosus was ruled out because the anti-DNA, anti-SM, anti-RNP, anti-Ro and anti-LA antibodies were negative; the serum complement levels were within the normal range and she did not presented any other clinical or laboratory manifestation that suggested any additional diagnosis.
We associate the occupational exposure of the patient with the clinical manifestations because prior to this she did not mentioned any symptoms and, in addition, she did not comply with the protection for handling these substances. As far as we know, we did not found previous reports of this association.
ConclusionThe use and handling of compounds used for gold screening (Pickling) for a prolonged period of time could be considered an external trigger of connective tissue diseases, being RP the first clinical manifestation.
The realization of immunological studies and videocapillaroscopies should be considered in patients who handle these substances and who present clinical manifestations suggestive of connective tissue diseases.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflict of interestThe authors declare they do not have any conflict of interest.
Please cite this article as: Maldonado G, Ríos C. Fenómeno de Raynaud asociado a ácido nítrico: reporte de un caso. Rev Colomb Reumatol. 2017;24:48–53.