Takayasu arteritis is a large vessel vasculitis that affects the aorta and its main branches, leading to arterial stenosis, and occasionally, thrombosis. There is also aneurysm formation in the general circulation. There is no specific treatment. The therapy of choice is corticosteroids, followed by other immunosuppressants in cases where adequate control of the inflammatory process is not achieved.
A case is presented of a patient with Takayasu arteritis and the unusual presence of giant aneurysm of pulmonary artery.
La arteritis de Takayasu es una de las vasculitis de grandes vasos que afecta a la aorta y a sus ramas principales, llevando a estenosis arterial y, en ocasiones, a trombosis. También se observa la formación de aneurismas en la circulación general. No tiene un tratamiento específico. La terapia de elección son los corticoides, seguidos de otros inmunosupresores en casos de no lograrse un control adecuado del proceso inflamatorio.
Se reporta el caso de un paciente con arteritis de Takayasu, con formación inusual de aneurisma gigante de la arteria pulmonar.
Takayasu arteritis (TA) is a type of large vessel vasculitis which affects especially the aorta producing occlusive ectatic changes, dilatation or formation of aneurysms, especially in the main circulation (aorta and its immediate branches), as well as in the pulmonary artery.1
In the second decade of the 20th century, the ophthalmologist Mikito Takayasu documented alterations in the flow of the central retinal vessels in the ocular fundus of a young woman.2 Later, the absence of pulses in the extremities, associated with the ocular changes described by Takayasu, configured the disease that bears his name.3
TA is considered a rare disease that mostly affects young women in the third and fourth decades of life (82.9–97%),4,5 mainly Asians, being higher the prevalence in Japan with 40 cases per million,6 while in the Western world there is a reported incidence of 0.4–2.6 cases per million.7,8 In Latin America the largest series of patients was described by Soto et al., with 110 Mexican patients, in whom the disease has a behavior and prognosis similar to that of the Eastern patients.9 It is noteworthy that in the local context Cañas et al., describe similar results in 35 Colombian patients.
In Colombia the age of onset ranges between 13 and 47 years; the age of the patients at the time of diagnosis was 30.6±9.4 years. Likewise, it was found a predominance of the disease in women (ratio 2.9:1).10
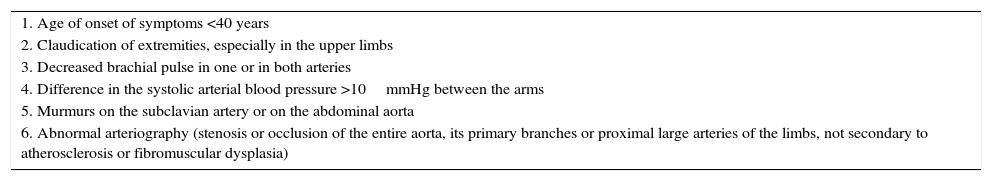
It is crucial to make a timely diagnosis of TA, since the inflammation and progressive arterial remodeling increase the chances of developing stenosis, occlusion, dilatation or formation of aneurysms.11 Although there are several diagnostic criteria, those of the American College of Rheumatology,12 published in 1990, which establish 6 simple and practical criteria are frequently used (Table 1).
Diagnostic criteria for Takayasu arteritis published in 1990 by the American College of Rheumatology.
| 1. Age of onset of symptoms <40 years |
| 2. Claudication of extremities, especially in the upper limbs |
| 3. Decreased brachial pulse in one or in both arteries |
| 4. Difference in the systolic arterial blood pressure >10mmHg between the arms |
| 5. Murmurs on the subclavian artery or on the abdominal aorta |
| 6. Abnormal arteriography (stenosis or occlusion of the entire aorta, its primary branches or proximal large arteries of the limbs, not secondary to atherosclerosis or fibromuscular dysplasia) |
The presence of 3 or more of these criteria demonstrated a diagnostic sensitivity of 90.5% with a specificity of 97.8%.
The purpose of this article is to present the case of a patient with diagnosis of aneurysms in the pulmonary artery which, although is usually affected, rarely is the main manifestation of the disease. Options for study and treatment to be followed in these cases will also be discussed.
Case descriptionA 62-year-old black female patient, from Cartago, Valle, Colombia, with a history of chronic hepatitis C infection with liver cirrhosis Child–Pugh stage B under treatment. In addition, pulmonary tuberculosis recently treated. 2 years ago, diagnosis of thoracic aortic aneurysm due to TA, corrected with endoprosthesis in another institution, under treatment with oral prednisolone by the Rheumatology outpatient service. She consulted to a level IV institution in Cali, due to a clinical picture of 3 months of evolution of pleuritic pain associated with dyspnea upon medium efforts, palpitations, asthenia, adynamia, nonspecific abdominal pain and intermittent claudication in lower limbs. She also presented weight loss of 15kg.
At the initial physical examination the patient is in a fair to middling general condition, afebrile, with the following vital signs: weight: 45kg, respiratory rate: 22×min, heart rate: 110×min, blood pressure: 130/90mm/Hg in the left upper limb, 120/80mm/Hg in the right upper limb, 110/75mm/Hg in the left lower limb and 110/76mm/Hg in the right lower limb. The significant findings include a grade IV systolic murmur audible in all cardiac foci and peripheral pulses reduced in the lower limbs.
In the initial studies, a right pleural effusion with concomitant basal atelectasis is found in the chest X-ray. Also, transthoracic echocardiogram with findings of left ventricular hypertrophy, LVEF: 69%, and as other important findings, pulmonary valve with dilatation of the ring and moderate pulmonary insufficiency, severe dilatation of the trunk of the pulmonary artery (51mm), with normal systolic pressure in the pulmonary artery (20mm/Hg). The most relevant laboratory studies were the hemogram, which reported mild leukopenia, without anemia, elevated erythrocyte sedimentation rate (44mm/H) and a positive d-dimer (2780). Due to suspicion of pulmonary thromboembolism is performed an angiotomography of the pulmonary arteries with the following findings: marked dilatation of the pulmonary artery and its branches, compatible with pre-capillary hypertension. Study negative for pulmonary thromboembolism. Aneurysm of the descending aorta with signs of dissection, without evidence of rupture. Right pleural effusion of 30ml (Figs. 1 and 2).
Coronal view of chest CT-angiography. Dilatation of the branches of the pulmonary artery which reaches a diameter of 73mm at the level of its trunk of exit. There is a big aneurysmal dilatation of the descending portion whose diameter in PA is 40mm with formation of a big mural thrombus and there is an associated hypodense linear image that corresponds to a dissection of the pulmonary artery.
During hospitalization she presents a marked elevation of blood pressure values, chest pain and increased dyspnea. An acute coronary event is ruled out, but due to myocardial dysfunction is transferred to the intensive care unit, requiring inotropic support with milrinone. The patient evolved adequately without presenting new episodes of dyspnea or chest pain and with better control of the blood pressure.
The case is reviewed jointly with the services of Cardiology, Infectious Diseases, Internal Medicine and Rheumatology, considering, given the findings of aneurysmal dilatation of the thoracoabdominal aorta and the pulmonary artery, with presence of myocardial dysfunction, arterial hypertension, diminished pulses in the lower limbs and elevation of the erythrocyte sedimentation rate, that the patient presents a picture of dyspnea secondary to a giant pulmonary artery aneurysm associated with TA. In a medical–surgical meeting she is considered a patient with a very high surgical risk, with great hemodynamic compromise, without any option of a new surgical or endovascular intervention, especially due to the antecedent of a previously implanted aortic endoprosthesis. In addition, a history of hepatitis C infection under antiviral therapy and tuberculosis recently treated. In view of the above is decided to optimize the medical treatment with prednisolone at 1mg/kg/day and tocilizumab at 8mg/kg. After 7 months of follow-up and with a low dose of prednisolone (10mg per day), the symptoms of dyspnea and chest pain are controlled, with better control of the blood pressure values.
DiscussionTA is a granulomatous vasculitis that affects large vessels, mostly the aorta and its main branches, especially in young women. Given the infrequency of this disease, no randomized controlled trials are available, and therefore its treatment is based on retrospective observational studies. An early diagnosis is required for a better prognosis of the patient. Inflammatory markers such as the erythrocyte sedimentation rate and the C-reactive protein are very useful for its detection in the initial phase or in the active phase. Multislice computed axial tomography angiography is the study of choice to establish the diagnosis. Meanwhile, ultrasound and angioresonance allow to detect changes in the thickness of the vessel wall, location, length and severity of the lesions, as well as to determine if the vascular obstruction is secondary to atheromatous plaques. In addition, there are new imaging modalities such as positron emission tomography,13,14 which help to achieve an early and accurate diagnosis.
The treatment of choice for TA is the use of corticosteroids, which, while inducing an initial remission in 90% of patients, it is estimated that approximately half of those affected will be resistant to them, in addition of the toxicity secondary to long-term high doses of steroids. For this reason other immunosuppressants (azathioprine, methotrexate or mycophenolate mofetil) are frequently used, although the few existing studies are not conclusive to determine that one of them is more effective than other.15 Recently, in patients refractory to conventional treatment, it has been observed a high efficacy of biological therapies such as tocilizumab.16,17
We publish this case given the unusual clinical compromise secondary to pulmonary artery aneurysm, in addition to the multiple associated comorbidities that make it difficult the treatment of this patient. Due to the impossibility of surgical or endovascular intervention and the infectious antecedents of the patient, tocilizumab was considered as the best treatment option in this case, previous consultation with the Service of Infectious Diseases of the institution.
The studies conducted until now with tocilizumab have limitations, since they are retrospective studies, with small sample sizes and without control groups.18 However, tocilizumab is considered a good therapeutic option in patients with difficult to control TA.19 In our case, the follow-up of the patient has shown an adequate resolution of the symptoms, as well as a better control of the blood pressure and decrease of the dose of prednisolone, with adequate tolerance.
The prognosis of TA is uncertain and is generally associated with the vascular commitment presented, as well as the necessity or not of surgical treatment, which is based in some characteristics of the patients, such as visual disorders, vertigo, cerebral infarction, claudication of the extremities and even severe hypertension. The morbidity and mortality has decreased in recent years due to the development of more sophisticated techniques for diagnosis and control, which have allowed a more appropriate treatment and in cases where is required, a better planning of the surgery.20
ConclusionTA is still a rare pathology in our environment. It can manifest clinically in an aggressive form as is the pulmonary artery aneurysm, which is a rare and barely published affection, as happened to the patient in this case. Although a variety of diagnostic aids are currently available and there is a greater number of therapeutic options, the high suspicion by the clinician and, consequently, a timely diagnosis is the main determinant of the prognosis of these patients.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflict of interestThe authors declare they do not have any conflict of interest.
Please cite this article as: Izquierdo Loaiza JH Díaz Giraldo JA. Arteritis de Takayasu y formación inusual de aneurisma gigante de arteria pulmonar, reporte de un caso. Rev Colomb Reumatol. 2017;24:40–43.