Autoimmune polyglandular syndrome (SPA) is a rare disorder that leads to endocrine gland dysfunction and can affect other organs. Several types of polyglandular syndrome are described. Type III may be associated with skin disorders of autoimmune origin such as vitiligo. Although the relationship between psoriasis and vitiligo has been widely documented, the association between psoriasis and SPA is rare and fewer than five cases have been reported in the literature. We present the case of a 34-year-old woman with SPA III associated with vulgar psoriasis and vitiligo.
El síndrome poliglandular autoinmune (SPA) es un trastorno raro que lleva a la disfunción de las glándulas endocrinas y puede afectar a otros órganos. Se describen varios tipos de síndrome poliglandular, el tipo III puede estar asociado con trastornos cutáneos de origen autoinmune como el vitiligo. Si bien la relación de psoriasis y vitiligo ha sido ampliamente documentada, la asociación entre psoriasis y SPA es rara y se han reportado menos de cinco casos en la literatura. Presentamos el caso de una mujer de 34 años con SPA III asociado con psoriasis vulgar y vitiligo.
A 34-year-old female patient, with a history of primary hypothyroidism and mild plaque psoriasis for more than 10 years, initially treated with topical therapy began to present acral achromic macules. A diagnosis of vitiligo was established and treatment with calcineurin inhibitors (tacrolimus 0.1%) and antioxidants was started. Due to the progression of both disorders (psoriasis and vitiligo), it was decided to initiate UVA and NB-UVB phototherapy, with no satisfactory response, with a PASI of 12 and DLQI of 18.
Within the vitiligo study, a diagnostic work-up was requested to rule out other autoimmune diseases: anti peroxidase and microsomal antibodies were positive, fasting blood glucose was normal; antinuclear (ANA), extractable nuclear antibodies (ENA), rheumatoid factor, and antiphospholipid antibody profile were negative. Furthermore, due to generalized pruritus, an abdominal ultrasound was requested, which revealed signs of chronic liver disease. This finding, coupled with positive mitochondrial antibodies, led to the diagnosis of primary biliary cirrhosis by hepatology. The patient, after being diagnosed with more than two autoimmune disorders, was referred to endocrinology, where a diagnosis of polyglandular autoimmune syndrome type III was confirmed, due to the presence of hypothyroidism, primary biliary cirrhosis, and vitiligo.
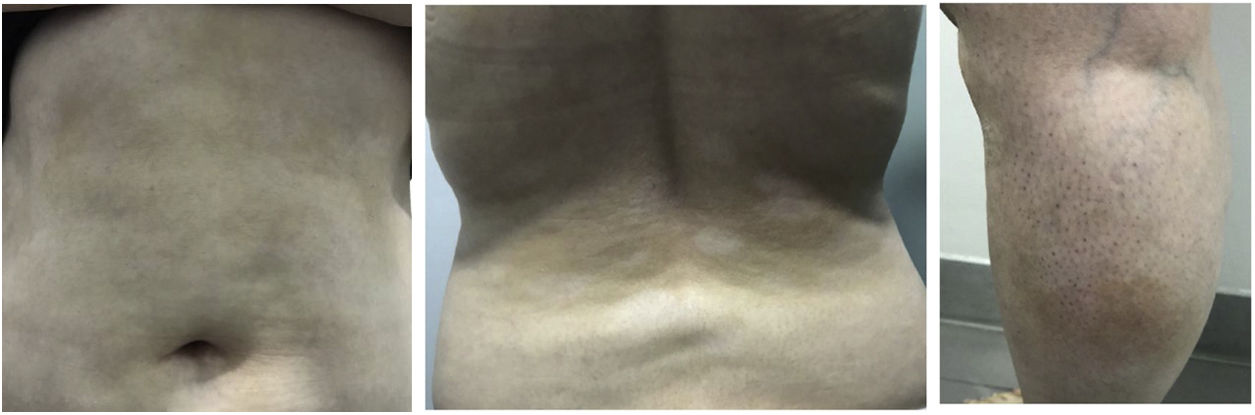
The use of methotrexate was contraindicated by hepatology due to the diagnosis of primary biliary cirrhosis; hence, biological anti-IL12/23 therapy (ustekinumab) was started, with a significant improvement in psoriasis (PASI 100) and quality of life. On the contrary, vitiligo showed rapid progression and became generalized (Fig. 1). However, the patient decided not to continue with the treatment, since vitiligo had little impact on her quality of life.
It is important to highlight that, despite the adequate clinical evolution of psoriasis, the rest of the autoimmune diseases have evolved unsatisfactorily with thyroid function outside of goals and complications associated with portal hypertension secondary to liver disease.
DiscussionPolyglandular autoimmune polyglandular syndrome (PAS) is a rare, heterogeneous disease, characterized by an alteration of the immune system that leads to inflammation and damage of at least 2 endocrine glands.1 Additionally, there may be non-endocrine organ disease due to autoimmune mechanisms.2 It begins with a stage in which circulating antibodies are detected but there is no functional alteration, followed by a subclinical phase with lymphocytic infiltration of the glands that leads to progressive destruction. Lastly, in the final stage, the clinical manifestations corresponding to glandular insufficiency occur.3
PAS is caused by the loss of immunotolerance to autoantigens due to alteration, either by the suppression of autoreactive cells or the presence of foreign antigens.4 Multiple autoimmunity is due to shared epitopes as external agents or as autoantigens present in several endocrine tissues; it is hypothesized that organs derived from the same germ layer express specific autoantigens that turn them potential target organs.3
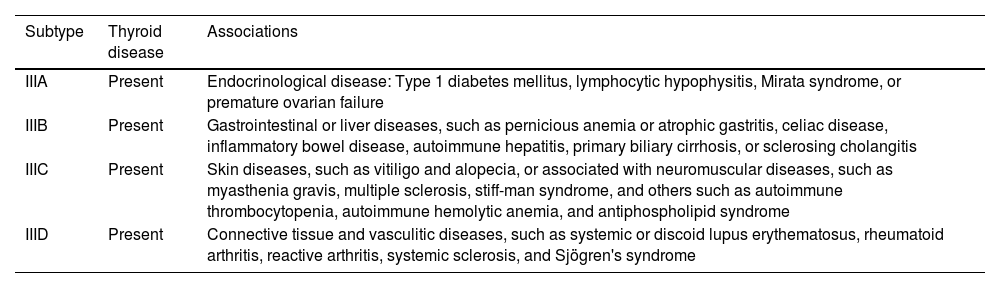
To date, four different types of PAS have been described, distinguished by the age of presentation, the combination of clinical features, and their genetic transmission.5 Concerning our patient, PAS type III (autoimmune thyroid disease associated with other autoimmune disorders) occurred. It has an estimated prevalence of 3.5–4% in the population; in different studies, specific human leukocyte antigens (HLA) have been detected in this disease.5 This type of PAS, in turn, is divided into four subtypes according to Betterle's reclassification,6 which is presented in Table 1.
The 4 subtypes of polyglandular autoimmune (PAS) type III.
| Subtype | Thyroid disease | Associations |
|---|---|---|
| IIIA | Present | Endocrinological disease: Type 1 diabetes mellitus, lymphocytic hypophysitis, Mirata syndrome, or premature ovarian failure |
| IIIB | Present | Gastrointestinal or liver diseases, such as pernicious anemia or atrophic gastritis, celiac disease, inflammatory bowel disease, autoimmune hepatitis, primary biliary cirrhosis, or sclerosing cholangitis |
| IIIC | Present | Skin diseases, such as vitiligo and alopecia, or associated with neuromuscular diseases, such as myasthenia gravis, multiple sclerosis, stiff-man syndrome, and others such as autoimmune thrombocytopenia, autoimmune hemolytic anemia, and antiphospholipid syndrome |
| IIID | Present | Connective tissue and vasculitic diseases, such as systemic or discoid lupus erythematosus, rheumatoid arthritis, reactive arthritis, systemic sclerosis, and Sjögren's syndrome |
In the current case, the patient would have a mixed PAS: type IIIB (due to a history of primary biliary cirrhosis) + type IIIC (psoriasis and vitiligo). Although the relationship between psoriasis and vitiligo has been widely documented, the association between psoriasis and PAS is rare, with less than 5 cases reported in the literature. The autoimmune disorder most frequently reported with PAS is vitiligo.
Psoriasis is a chronic and common inflammatory disease that affects approximately 3% of the population. Its pathogenesis involves environmental and genetic factors7 and is characterized by hyperkeratotic plaques that correspond to inflammation and epidermal hyperplasia mediated through a complex interaction of the innate and adaptive immune systems.8 Its association with other autoimmune and inflammatory skin disorders, such as vitiligo and blistering diseases, has been described.7 In a multicenter study, it was reported that the prevalence of inflammatory skin diseases in patients with psoriasis was 21.1%; the most common were rosacea and acne, and vitiligo was associated in 1.6% of the patients in this study.
Patients with psoriasis have a higher risk of developing other autoimmune diseases when compared to the general population.9
Vitiligo is an immune-mediated pigment disorder; its association with psoriasis has been documented. A 2019 meta-analysis refers to the significantly higher probability of having vitiligo in patients with psoriasis, and the risk of having psoriasis is even greater if there is a previous diagnosis of vitiligo.9
The relationship between psoriasis and vitiligo can be explained by a common genetic basis that involves not only shared loci but also alterations in some cytokines that are part of the Th1 and Th17 pathways that lead to a hyperactive cellular response and alterations in the inflammasome.10,11 In both diseases, the intracellular JAK-STAT signaling pathway mediates the expression of cytokines, growth factors, and hormones, which ultimately leads to the activation of T lymphocytes.12 For this reason, JAK kinase inhibitors could be effective by targeting second messengers involved in both disorders.13
Recent advances in the genetics of autoimmune diseases have identified an alteration in multiple common genes, which is why it is frequent to find the association of more than one autoimmune disease.14
Among the few cases reported in the literature of PAS associated with psoriasis, it is worth highlighting that all the cases in adults were PAS type III, except one PAS type I in a 14-year-old child. In none of the articles in the search, the association with primary biliary cirrhosis was found.
An additional problem for the treatment of PAS related to psoriasis or other skin disorders is that, as several conditions do not always share immunological pathways, the use of different medications is necessary, which increases the risk of adverse reactions and decreases therapeutic adherence.15 In the current case, the response in psoriasis has been successful with the use of ustekinumab; however, the other diseases have not evolved satisfactorily (Fig. 1).
In conclusion, the case of a young woman with mixed polyglandular autoimmune syndrome type IIIB+IIIC associated with psoriasis is presented. Given that the genetic and immune basis of psoriasis is known, its strong association with other autoimmune diseases is not surprising; however, the association with PAS is rare, with less than five cases reported in the literature. The relation between psoriasis and vitiligo is well documented since both have a shared genetic basis; however, each disorder has different immune pathways, representing a greater therapeutic challenge. Medications whose therapeutic targets are involved in both diseases can be considered, such as JAK kinase inhibitors, which were not implemented in the patient, since vitiligo did not affect her quality of life. It is important to perform a complete and comprehensive approach in subjects with PAS.
Ethical considerationsInformed consent was requested for the patient to receive treatment in the investigation. This paper complies with current regulations on bioethical research, and authorization from the ethics committee was not necessary since the patient was assessed in private practice. The authors declare that this article does not contain personal information that could identify the patient.
Conflict of interestsThe authors of the article declare no conflict of interest in the preparation of this article.