Sarcoidosis is a multi-system disease that involves the lung in 90% of cases. Skeletomuscular involvement of sarcoidosis may involve joints, muscles and/or bones, the latter affecting 3-13% of patients. Its clinical presentation is asymptomatic in half of the cases, in the other half there is pain, soft tissue edema, and decreased limb function. Radiographically it is accompanied by osteolysis, osteosclerosis, cystic lesions and pathological fractures in advanced stages. A final diagnosis is made by tissue biopsy, finding non-caseating granulomatous process accompanied by Langhans giant cells. The main indication of medical management is the control of symptoms, associated with an improvement in the functioning of the affected limb and quality of life of the patient. The case is presented of a patient with digital sarcoidosis with classic radiographic pattern with no other extra-skeletal involvement.
La sarcoidosis es una enfermedad multisistémica que involucra en el 90% de los casos el pulmón. El compromiso osteomuscular de la sarcoidosis puede incluir articulaciones, músculos o huesos; este último caso afecta al 3-13% de los pacientes. Su presentación clínica es asintomática en la mitad de los casos, el restante se presenta con dolor, edema de tejidos blandos y disminución en la funcionalidad de la extremidad. Radiográficamente se acompaña de osteólisis, osteoesclerosis, lesiones quísticas y fracturas patológicas en estadios avanzados. Su diagnóstico definitivo se realiza por medio de una biopsia tisular, en la que se encuentra un proceso granulomatoso no caseificante acompañado de células gigantes de Langhans. La principal indicación del manejo médico es el control de los síntomas, lo que se asocia con una mejoría en el funcionamiento de la extremidad afectada y en la calidad de vida del paciente. Se presenta el caso de un paciente con sarcoidosis digital con patrón radiográfico clásico, sin otro compromiso extraesquelético.
Sarcoidosis is a multisystem disease, histopathologically characterized by non-caseating granulomas, whose etiology and pathophysiology are not fully known so far. It can involve different organs or systems. However, 90% of patients have lung and intrathoracic lymph node involvement, they are usually asymptomatic and, to a lesser extent, they have symptoms such as cough, dyspnea, or chest tightness.1,2 Musculoskeletal involvement, which is rare, occurs in between 25% and 33% of patients3 and it can present in an acute transient form as Löfgren's syndrome or as a chronic arthropathy.4–7
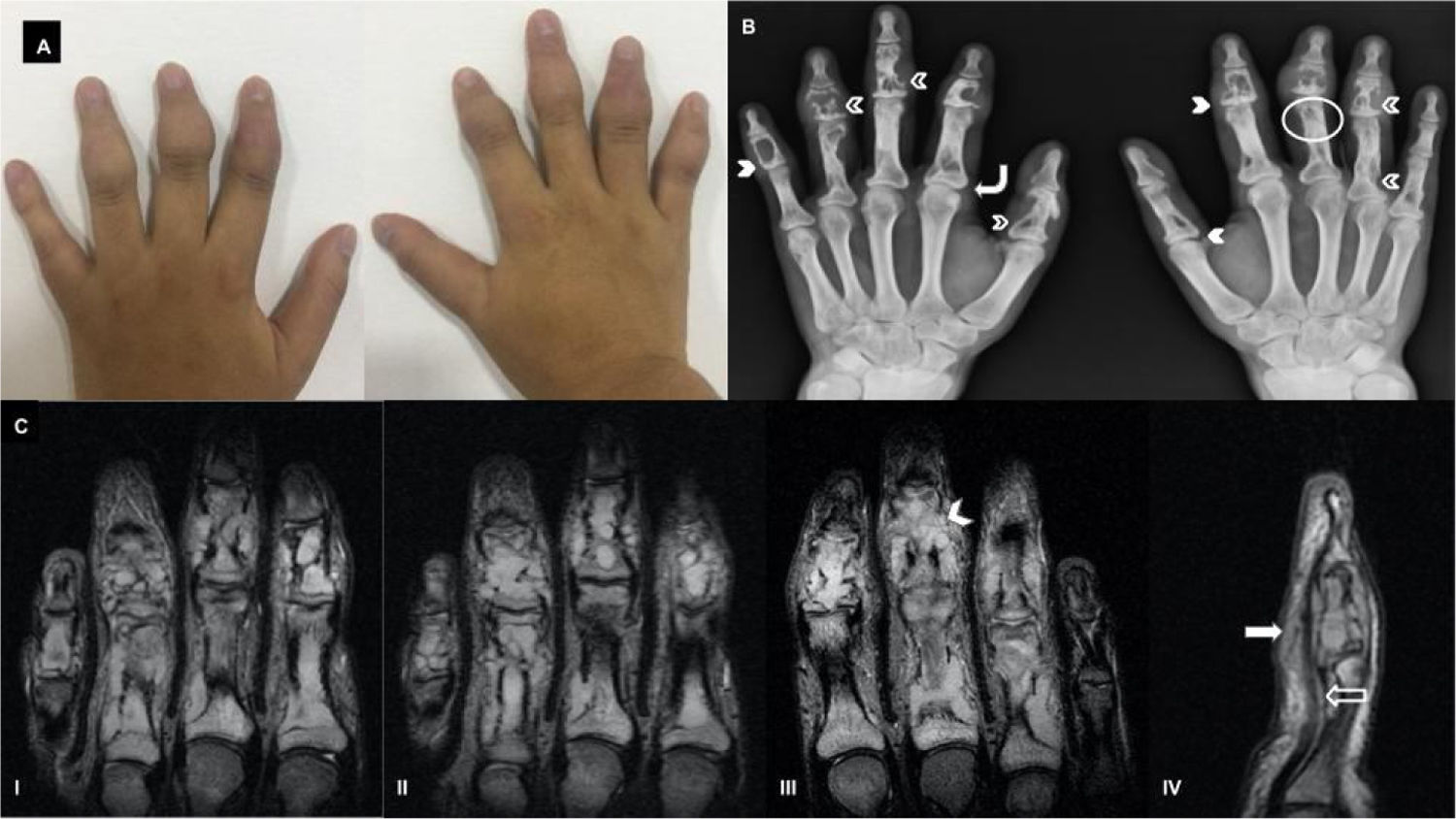
Clinical observationA 22-year-old male Colombian patient who attended consultation, reported the appearance of masses in all the middle phalanges of the hands and in the axillary and cervical regions since he was 15 years old, without previous treatment or study, with an exacerbation of the clinical picture in the last few months due to greater pain intensity, increased volume of the fingers and mobility problems. The review of symptoms by systems did not yield positive data. The physical examination revealed severe infiltrative involvement of the middle phalanges in both hands, with inflammation of the soft tissues and superficial erythema without joint involvement. Pain on palpation and increased volume of the fingers were observed. There were no lymphadenopathies or masses in other body areas.
Studies were performed, beginning with X-rays of the hands, which showed severe osteolytic involvement in the middle and proximal phalanges of both hands (Fig. 1). The ultrasound of the hands provided the finding of hypoechoic material with Doppler signal inside at the periarticular and articular levels in the proximal interphalangeal joints, with cortical disruption in the diaphysis of the second phalanx in all the fingers and tenosynovitis of the flexor tendons. Finally, the MRI of the hands revealed multiple expansile lytic lesions in the proximal and middle phalanges in all the fingers of the hands, with perilesional soft tissue involvement. A biopsy of the bone lesion was performed and as a result, multiple non-caseating granulomas were found with some giant multinucleated Langhans-type cells. Extension studies were carried out looking specifically for pulmonary involvement. The chest x-ray and the computed tomography did not reveal pathological findings.
A. Handsof the patient before the start of treatment. There is an increase in the thickness of the soft tissues of all the fingers with greater involvement of the middle phalanx. B. AP radiograph of both hands showing the different patterns of bone involvement in sarcoidosis: lytic pattern with localized well-defined cystic defects, accompanied by nodular soft tissue lesions (solid arrowheads); permeative pattern with enlargement of the nutrient canal of the phalanx (circles); destructive pattern that can generate scalloped or punched out lesions (empty arrowheads); honeycomb pattern with diffuse trabecular alteration (curved arrows); C. Non-contrasted nuclear magnetic resonance. (I) and (II) right hand, coronal section STIR sequence: extensive involvement of the proximal and middle phalanges by conglomerates of hyperintense intramedullary masses (corresponding to non-caseating granulomas), with cortical destruction and infiltration of adjacent soft tissues. Mild soft tissue edema is seen. (III) Left hand coronal section STIR sequence: in the middle phalanx of the third finger (solid arrowhead) fine hypointense lines perpendicular to the destroyed bone cortex (also called "ghost cortex") are observed, corresponding to the periosteal extension of granulomas; it should not be confused with periosteal reaction. Note the absence of intra-articular and distal phalangeal involvement, as well as the preserved joint relations. (IV) Sagittal T2-weighted image of the fifth finger of the right hand: increased signal intensity of the flexor tendon (empty arrow) and encapsulation therein by granulomatous infiltration (solid arrow).
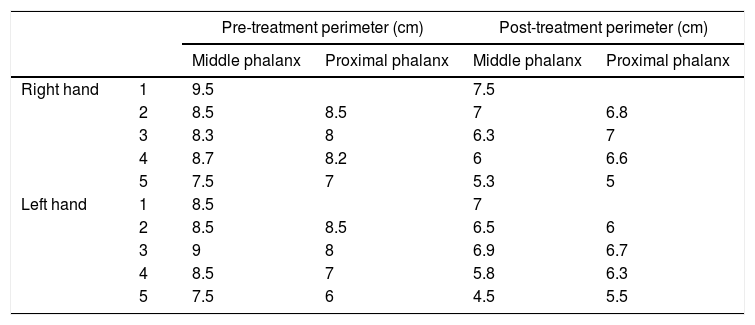
A diagnosis of sarcoidosis with isolated bone involvement was considered and management was started with prednisolone 50 mg/day, as a result of which the pain and the volume of the fingers decreased. However, there was a relapse when the dose was adjusted to less than 25 mg/day, and for this reason methotrexate was added, and adjusted up to 25 mg/week. In addition, the patient received folic acid 5 mg/week, calcium and vitamin D. The response to treatment was adequate, with control of pain and functionality, due to the decrease in soft tissue inflammation. Therefore, progressive steroid weaning was started. Fig. 1 shows the radiological images and photographs of the patient's hands before the start of treatment, while Table 1 describes the decrease in digital volume after treatment. The recorded measurements were taken 10 months after the beginning of the treatment.
Diameters of middle and distal phalanges of the patient before and after treatment.
| Pre-treatment perimeter (cm) | Post-treatment perimeter (cm) | ||||
|---|---|---|---|---|---|
| Middle phalanx | Proximal phalanx | Middle phalanx | Proximal phalanx | ||
| Right hand | 1 | 9.5 | 7.5 | ||
| 2 | 8.5 | 8.5 | 7 | 6.8 | |
| 3 | 8.3 | 8 | 6.3 | 7 | |
| 4 | 8.7 | 8.2 | 6 | 6.6 | |
| 5 | 7.5 | 7 | 5.3 | 5 | |
| Left hand | 1 | 8.5 | 7 | ||
| 2 | 8.5 | 8.5 | 6.5 | 6 | |
| 3 | 9 | 8 | 6.9 | 6.7 | |
| 4 | 8.5 | 7 | 5.8 | 6.3 | |
| 5 | 7.5 | 6 | 4.5 | 5.5 | |
In sarcoidosis, musculoskeletal disorders are classified as acute or chronic. Löfgren's syndrome is an additive symmetric acute oligoarthritis that predominantly affects large peripheral joints and occurs with the classic triad of bilateral hilar lymphadenopathy, erythema nodosum, and periarthritis (of the elbows, wrists, knees, shoulders, metacarpophalangeal joints, and ankles). Its symptoms, the result of periarticular soft tissue edema, in most cases occur concomitantly with the development of erythema nodosum and resolve spontaneously within weeks or months. Chronic sarcoid arthropathy, less frequent, can be present in a variety of ways: non-deforming arthritis with granulomatous synovitis, non-erosive Jaccoud arthropathy, joint edema adjacent to the bone lesion, or dactylitis. It is usually accompanied by a worse prognosis and generates erosive changes, deformity and compromised joint functionality.8,9
Regarding the bone involvement, it has classically been described that the appendicular skeleton, specifically the hands and feet, is the most affected.3 However, the axial skeleton may be affected and there are current reports in which its involvement comes to be equal or even more frequent.2 In general, when bone involvement occurs, there are accompanying extraosseous manifestations, being the most frequent mediastinal lymph node involvement (93%), followed by pulmonary involvement (90%), extrathoracic lymph nodes (66%) and skin involvement (44%).2,3 No associated extraosseous manifestation has been documented in this patient throughout follow-up.
Bone sarcoidosis presents as a cystic osteitis of the bones, called osteitis multiplex cystoides or Jüngling's disease, with preservation of the periosteum and cortical margins associated with ungueal dystrophy.9 Its clinical presentation in the hands involves, in order of frequency, the phalanges, the metacarpal bones and the carpal bones.3 It is usually asymptomatic in more than half of patients diagnosed. In patients with isolated bone sarcoidosis involvement, the differential diagnoses include enchondroma, subchondral cyst secondary to osteoarthritis, metastatic disease, hyperparathyroidism, epidermoid inclusion cyst, fibrous dysplasia, and osteomyelitis.10 Pain, stiffness, and loss of function are largely associated with cutaneous lesions, especially in patients with lupus pernio,8,11 known as erythematous lesions of insidious onset on the skin, related to a chronic involvement of sarcoidosis in the upper respiratory tract, plaques in the skin and nasal mucosa, bone cysts, pulmonary fibrosis and chronic uveitis.12
Radiographically, three different patterns of bone involvement are described in sarcoidosis: a lytic pattern, the result of bone resorption and the formation of cysts; a permeative or trabecular pattern, in which the cortex is characterized by having the form of networks or tunnels; and a less frequent pattern, destructive, associated with overlapping with serious pathological fractures or adjacent arthropathy.11,13 Although magnetic resonance imaging is more sensitive for bone involvement in sarcoidosis, it can be confused with malignancy. The presence of intralesional fat is a characteristic that rules out a differential diagnosis of bone metastasis.14 Unfortunately, the radiographic diagnosis of bone sarcoidosis, accompanied by symptoms, is usually characteristic in patients with advanced stages of the disease, with involvement of the structure and functionality of the limb. The definitive diagnosis requires histopathological confirmation that excludes another non-caseating granulomatous entity, since the clinical presentation and the diagnostic images are nonspecific.5
In relation to treatment, acute sarcoid arthropathy is usually self-limited, requiring symptomatic management with high-doses of nonsteroidal anti-inflammatory drugs (NSAIDs) or corticosteroids. In the event that symptoms are not controlled or when NSAIDs are contraindicated, oral corticosteroids can be used. In patients with bone involvement there is no consensus about pharmacological treatment. Corticosteroids are used more frequently, either as monotherapy or in combination with methotrexate. Hydroxychloroquine and sulfasalazine have also been used,1,3,8,11,15 as well as tumor necrosis factor alpha inhibitors such as infliximab and adalimumab. Amputations of the affected limb have been described in patients with severe pathological fractures and bone destruction.1,10
ConclusionThis case provides a brief clinical and radiological review of a rare entity, which constitutes a real diagnostic challenge. It is essential to keep it in mind within the differential diagnosis of dactylitis, since its early recognition allows to improve the quality of life of patients and reduces the impact on disability.
FundingThe research and publication process was financed by the universities to which the authors are affiliated.
Conflict of interestThe authors declare that they have no conflict of interest.
Please cite this article as: Mora-Karam C, Calvo-Páramo E, Tuta Quintero E, Cardona Ardila LF. Sarcoidosis ósea: una manifestación inusual. Rev Colomb Reumatol. 2022;29:151–154.