Cogan's syndrome is a chronic inflammatory disease typified by interstitial keratitis and Meniere-like auditory involvement, and it can be accompanied by systemic vasculitis. It is a rare disease and its diagnosis is difficult and often late, which increases the risk of sequelae, such as visual loss or deafness. In addition, its treatment is not well-established and is based on case reports that have observed efficacy of drugs such as cyclophosphamide, anti-TNF or tocilizumab. A case of Cogan's syndrome is presented that did not respond to methotrexate, cyclophosphamide, or anti-TNF, but with a partial response to tocilizumab.
El Síndrome de Cogan (SC) es una enfermedad inflamatoria crónica, caracterizada por queratitis intersticial y síntomas vestibuloauditivos similares al síndrome de Meniere, acompañado o no de vasculitis sistémica. Es una enfermedad poco frecuente y su diagnóstico es difícil y a menudo tardío, lo que aumenta el riesgo de secuelas como pérdida visual o cofosis. Además, su tratamiento no está bien establecido y se basa en reportes de casos donde se ha observado la eficacia de fármacos como la ciclofosfamida, antiTNF o tocilizumab. Presentamos un caso de SC sin respuesta a metotrexato, ciclofosfamida ni antiTNF, y respuesta parcial a tocilizumab.
Cogan's syndrome (CS) is a rare disease characterized by ocular inflammation and audiovestibular symptoms, sometimes accompanied by vasculitis or aortitis. The diagnosis is often complex due to its low incidence, which leads to late diagnosis that can condition a poor functional prognosis. There is also no consensus on the most appropriate treatment, so its management is based on case reports, which have shown efficacy of disease modulating drugs (DMARDs) and biological agents in some patients.
Clinical observationA 48-year-old male with large vessel vasculitis diagnosed in March 2015 in another hospital based on the clinical picture of general involvement with sustained fever, facial paralysis, hearing loss in the right ear, significant elevation of acute phase reactants (APR) in the absence of infectious processes ruled out by cultures, and vascular affectation in PET/CT with uptake of common carotids with right predominance, abdominal aorta, external iliac arteries and left internal iliac artery. No biopsy was done to confirm the diagnosis. The patient received treatment with boluses of 1g of methylprednisolone followed by prednisone 100mg in descending doses and 6 boluses of cyclophosphamide 900mg (doses of 500mg/m2 bsa), with improvement in the APRs and disappearance of vascular uptake in PET/CT in October, 2015.
In April 2016, the patient was admitted to our hospital due to fever, red left eye, sudden left hearing loss, left peripheral facial paralysis and elevation of APR. He was assessed by ophthalmology: left eye with flat scleritis throughout the temporal area with ciliary hyperemia, Tyndall ++++ and Flare ++, pupil with synechiae and cyclitic membrane adhered to crystalloids, all compatible with acute anterior uveitis and scleritis of the left eye, without evidence of interstitial keratitis. Also assessed by otorhinolaryngology, it was performed an otoscopy which was normal and a tonal audiometry: right ear with deafness, left ear with sensorineural hearing loss with an average threshold in 72dB, with improvement in low frequencies of 15dB, being compatible with sudden sensorineural hearing loss in the left ear.
Microbiological and serology samples were taken to rule out infection, and suspecting a reactivation of vasculitis, 3 boluses of methylprednisolone (the first of 500mg and the following two of 1g each one) and subsequently intravenous corticosteroids at 1mg/kg/day were administered, without any improvement.
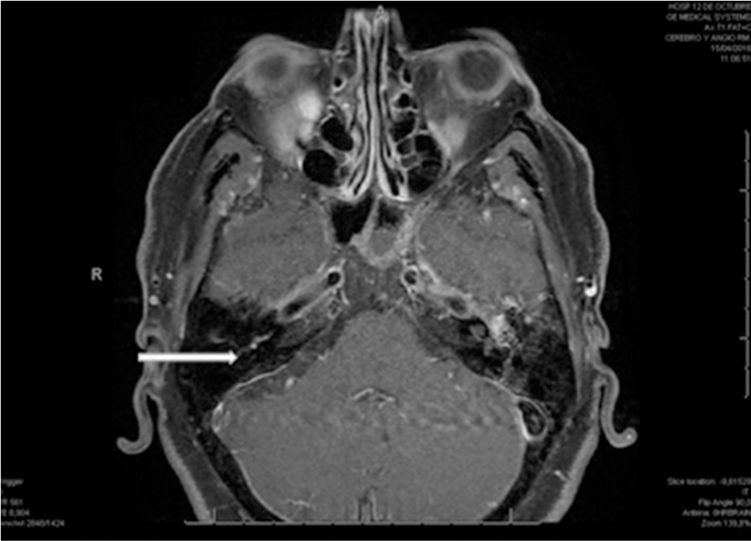
Analyzes were carried out with negative rheumatoid factor, antinuclear antibodies, (ANA), antibodies against extractable nuclear antigens (anti-ENA), complement, anticardiolipins and anti-neutrophil cytoplasmic antibodies (ANCA); negative serologies, Mantoux (tuberculin skin test), Booster (tuberculin skin test repeated 10 days later) and lumbar puncture; nuclear magnetic resonance imaging (MRI) of the brain with contrast uptake in the vestibule, semicircular canals and basal turn of the cochlea of the right side, and lower uptake in the basal turn of the cochlea of the left side, compatible with CS in the active phases of the disease (Fig. 1); cervical and cerebral MR-angiography without vascular involvement, and abdominal MR-angiography and PET/CT with aortitis predominantly infrarenal and in primitive iliac arteries.
MRI of the brain T1 fat+c sequence, axial section, where subtle uptake is observed at the level of the right cochlea (indicated by the arrow). This contrast uptake has been described in Cogan's disease in the active phases of the disease by leakage of contrast in the membrane of the labyrinth.
20mg of subcutaneous methotrexate weekly were associated to the treatment and 2 doses of infliximab at 5mg/kg were administered without clinical or analytical improvement, developing severe anemization which required transfusions, ruling out bleeding, hemolysis and hemophagocytic syndrome at this time by bone marrow biopsy. In addition, the patient developed uveitis also in the right eye and collapse of the nasal pyramid, and thereby the treatment was changed to tocilizumab 8mg/kg/every 4 weeks, staying afebrile, with normalization of the analytical parameters and was discharged.
One month later he developed bilateral coxalgia, tibioastragalar arthritis and elevated APR, and therefore, the dose of prednisone was increased to 50mg/day, subcutaneous methotrexate was also increased to 25mg/weekly and treatment with tocilizumab was intensified to 8mg/kg every 3 weeks. In the PET/CT of control, vascular uptake was not observed, although there was an increased metabolic activity in the sacroiliac joints. Later, he was admitted to the ICU of another hospital due to acute respiratory insufficiency and bilateral perihilar pulmonary infiltrates, and died from cardiac arrest without being able to complete the study. Necropsy was not performed.
DiscussionCS is a rare chronic inflammatory disease, with a peak incidence between the third and fourth decades of life, without predominance by gender.1 It is characterized by involvement of the eye and the inner ear, being the most typical interstitial keratitis and audiovestibular dysfunction with Meniere's syndrome and/or sensorineural hearing loss. Other ocular manifestations such as uveitis, scleritis, episcleritis or vasculitis can occur. Less than 5% of patients present with systemic manifestations and up to 15–20% may present small, medium or large vessel vasculitis or aortitis,1–3 which can cause stenosis, dilation or aneurysms.3
Given the variability of the clinical presentation, the diagnosis is complex and usually late, and requires the exclusion of other diseases. It is based on the presence of characteristic inflammatory ocular disease and vestibular-auditory dysfunction, in the presence or absence of vasculitis. The PET/CT plays an important role in the diagnosis of vasculitis, since several studies have shown that is effective for the detection of large vessel vasculitis and for the evaluation of the disease activity and extent, with a sensitivity ranging between 77 and 100% and a specificity of 89–100%.4,5
In the case we present, the diagnosis was reached by the presence of scleritis and uveitis, which although they are not the typical characteristic of CS, they may appear, sensorineural hearing loss with a Meniere-like syndrome, general clinical symptoms with malaise, fever and aortitis. Throughout the evolution, the differential diagnosis with granulomatosis with polyangiitis was considered due to the collapse of the nasal pyramid and arthritis, but the ANCAs were negative, and there were no pulmonary involvement or alterations in the urinary sediment. It was also made a differential diagnosis with other entities such as sarcoidosis (unlikely in the absence of pulmonary affectation) or infections that could occur with aortitis such as tuberculosis or syphilis (unlikely given the cultures and serologies negative for these diseases).
The treatment for CS is not well established; it is linked to the severity of the organic affectation and is based on case reports. Steroid treatment is the most widely used, with good response of the systemic and ophthalmologic manifestations; however, it often requires the association of a DMARD.6 The auditory affectation commonly leads to hearing loss, but the cochlear implants contribute to improve the quality of life.
Of the DMARDs, methotrexate, azathioprine and mycophenolate mofetil are the most widely used, showing efficacy as steroid sparing agents in ocular inflammation,7,8 hearing loss and vasculitis.9 Cyclophosphamide has also been used for the induction and maintenance therapy for medium and large vessel vasculitis.9
As for the biological drugs, infliximab seems to be the most effective of the anti-TNFs for the induction and maintenance therapy of the CS resistant to glucocorticoids and immunosuppressants,10 being more effective if it is introduced early,11 and etanercept increases the word recognition in hearing impairment.12 Rituximab appears to have been effective in improving hearing in a patient with interstitial keratitis and vestibular symptoms resistant to methotrexate, cyclophosphamide, cyclosporine and adalimumab, achieving audiometric improvement and in all clinical manifestations.6
Finally, improvements in inflammatory markers and quality of life with tocilizumab have been observed in some patients with CS with large vessel vasculitis or aortitis and ineffectiveness of other immunosuppressants such as methotrexate or infliximab,9,13 as occurred with our patient.
In cases that are resistant or with side effects to other therapeutic options, given that CS is currently considered a vasculitis, plasmapheresis may be justified in order to avoid irreversible ocular or audiovestibular damage.14
ConclusionWe present a case of CS with poor response to immunosuppressive treatment with prednisone, methotrexate and infliximab and partial response to tocilizumab. We highlight the importance of performing retrospective studies and meta-analyzes to establish which would be the best treatment in this rare and potentially serious disease.
Conflict of interestThe authors state they do not have any conflict of interest.
Please cite this article as: de la Cámara Fernández I, Molina Larios RA, Ibáñez BJ. Síndrome de cogan: descripción de un caso con respuesta parcial a tocilizumab y revisión de la literatura. Rev Colomb Reumatol. 2018;25:298–300.