La fibromialgia es una enfermedad crónica caracterizada por la presencia de dolor músculo esquelético, usualmente asociada a otros síntomas como depresión, fatiga, trastornos del sueño, entre otros. Los conceptos y las percepciones sobre el diagnóstico y el tratamiento de la fibromialgia, entre médicos reumatólogos no se conocen objetivamente. El propósito de este estudio es describir los conceptos y percepciones sobre el diagnóstico y tratamiento de la fibromialgia, entre un grupo de médicos reumatólogos en Colombia.
MétodosEstudio descriptivo de corte transversal. A través de un grupo focal en el que participaron dos reumatólogos y un experto en métodos de investigación cualitativa, se diseñó una encuesta para evaluar las percepciones y conceptos que los médicos reumatólogos tienen sobre el diagnóstico y el tratamiento de la fibromialgia. La encuesta se aplicó de forma autoadministrada y anónima a médicos reumatólogos pertenecientes a la Asociación Colombiana de Reumatología.
ResultadosEncuesta aplicada a 139 reumatólogos. 25,2% (n = 35) considera que no hay suficiente evidencia para considerar la fibromialgia como una enfermedad. 32,4% (n = 45) usa los criterios ACR (American college of Rheumatology) de 1990 para diagnosticar pacientes con fibromialgia, a pesar de que el 92,1% (n = 128) considera que estos criterios no son suficientes para el diagnóstico de fibromialgia. Los medicamentos más formulados para manejo de fibromialgia son los antidepresivos, prescritos por el 90,6% (n = 126) de los encuestados, seguido por anticonvulsivantes 64,7% (n = 90) y analgésicos 26,6% (n = 37). 76,3% (n = 106) de los reumatólogos considera que el manejo del paciente con fibromialgia debe tener un enfoque multidisciplinario. 81,3% (n = 113) de los reumatólogos considera que el paciente con fibromialgia debe tener como médico tratante principal a un especialista distinto al reumatólogo.
ConclusiónEl presente estudio muestra información acerca de las percepciones acerca del diagnóstico y tratamiento de fibromialgia entre un grupo de reumatólogos colombianos, documentándose un frecuente uso de los criterios de clasificación ACR 1990. En cuanto a tratamiento se observa un alto porcentaje de uso de medicamentos, en especial antidepresivos y analgésicos. La mayoría de los reumatólogos considera que los médicos fisiatras, deben ser los líderes del manejo interdisciplinario en el tratamiento del paciente con fibromialgia.
Fibromyalgia is a chronic disease characterized by the presence of widespread and persistent musculoskeletal pain associated with various symptoms such as depression, fatigue, sleep disorders, inter alia. The concepts and perceptions of rheumatologists around the diagnosis and treatment of fibromyalgia are not objectively known. The purpose of this study is to describe the concepts and perceptions on the diagnosis and treatment of fibromyalgia among a group of Colombian rheumatologists.
MethodsCross-sectional descriptive study using a focus group, comprised of two rheumatologists and one expert in qualitative research methods. A survey was designed to assess the perceptions and concepts that rheumatologists have on the diagnosis and treatment of fibromyalgia. The survey was self-administered and anonymous, to be completed by rheumatologists members of the Colombian Association of Rheumatology.
ResultsA total of 139 rheumatologists completed the survey. 25.2% (n = 35) considered that there is not enough evidence to recognize fibromyalgia as a disease; 32.4% (n = 45) follows the 1990 ACR (American College of Rheumatology) criteria to diagnose patients with fibromyalgia, although 92.1% (n = 128) believe that these criteria are not sufficient to diagnose fibromyalgia. The most widely used medications for managing fibromyalgia are antidepressants, prescribed by 90.6% (n = 126) of the responders, followed by anticonvulsants 64.7% (n = 90) and analgesics 26.6% (n = 37). 76.3%, (n = 106) of rheumatologists consider that there should be a multidisciplinary approach to the patient with fibromyalgia. Moreover, 81.3% (n = 113) of the rheumatologists believe that the treating physician for patients with fibromyalgia should be a specialists other than a rheumatologist.
ConclusionThis study shares information about the various perceptions of a group of Colombian rheumatologists with regards to the diagnosis and treatment of fibromyalgia, reporting frequent use of the ACR 1990 classification criteria. In terms of treatment, there is a high percentage of use of medications, in particular antidepressants and analgesics. Most rheumatologists believe that physiatrists should be the leaders in the multidisciplinary management approach for treating patients with fibromyalgia.
Fibromyalgia is a chronic disease characterized by generalized musculoskeletal pain, usually associated with a broad range of symptoms affecting the quality of life of patients.1 In 1992, the World Health Organization recognized fibromyalgia as a clinical syndrome of unknown etiology, that causes chronic, diffuse and disabling musculoskeletal pain, usually accompanied by fatigue, sleep disorders, headache, irritable bowel, among other disorders.2 The prevalence of fibromyalgia varies between 2% to 4% of the general population, with a higher proportion of females (female: male ratio of 9:1).3,4 In Colombia, the estimated prevalence is 0.72% (95% CI 0.47–1.11%), based on a study using the COPCORD (Community Oriented Program in the Rheumatic Diseases) methodology and screening questionnaire, after assessing 6,693 people from 6 cities in Colombia5. The criteria for the classification of fibromyalgia were initially defined in 1990 by the American College of Rheumatology (ACR).6 Over the next 20 years, several observations were made from various authors, including the principal author of the 1990 criteria, with a view to identifying a new approach to the classification of these patients.7 In May 2010, new classification criteria were suggested8, intended to include not just pain-associated considerations, but also the broad spectrum of symptoms affecting these patients.
Fibromyalgia represents a diagnostic and therapeutic challenge for the physician, regardless of the area of specialization, because of the complexity of a disease characterized by generalized pain as the main symptom, associated with other clinical findings which are difficult to quantify, such as fatigue, sleep disorders, and cognitive dysfunction.9 A topic frequently discussed among rheumatologists in Colombia and in other countries around the world, is the difficult approach to patients with fibromyalgia, since the symptoms and signs may be mistaken with other diseases compromising the musculoskeletal system, and often these are patients who have previously seen other doctors from different areas of specialization; according to Ubago et al., in average up to four different specialists before the rheumatologist.10,11 Hence, patients with fibromyalgia, in addition to visiting multiple specialists for years, with the hope of being diagnosed, they receive a treatment that is still uncertain and many times frustrating, both for the patient and for the physician, because of the failure to improve the patient’s symptoms.12 There is no objective information about the concepts and opinions of the Colombian rheumatologists with regards to diagnostic and therapeutic aspects for patients with fibromyalgia, considering the peculiarities and the clinical challenges of these patients. Only informal and subjective information is currently available; so, this study is intended to collect objective information on this matter.
MethodsDescriptive, cross-sectional study based on a focus group comprising two rheumatologists and one expert in qualitative research. A survey was designed with four domains: the first referring to general considerations and physician identification (age, gender, time of experience, city of practice); the second domain asked questions about some diagnostic aspects of the disease; the third domain dealt with the therapeutic options used (pharmacological and non-pharmacological treatments, and alternative therapies); the fourth domain asked about their views about a multidisciplinary approach to fibromyalgia, and referral to other specialists. The choices of answers were presented as a Likert scale. A pilot test was conducted with five rheumatology residents to assess the survey time and the level of understanding of the questions. The survey was self-administered and anonymous and it was distributed during the meetings of the Colombian Association of Rheumatology. The information was collected in a database and was analyzed using Microsoft Excel®. A descriptive analysis was conducted, using frequencies and percentages for the qualitative variables and central tendency measures for the quantitative variables.
Results139 rheumatologists completed the survey. 82.7% (n = 115) of the responders were males, with a mean age of 44 years (±8.9). The average experience in the practice of rheumatology was 11.6 years (±8.2). 25.2% (n = 35) of the rheumatologists feel that there is not enough evidence to consider fibromyalgia as a disease, and 32.4% (n = 45) use the 1990 ACR criteria for the diagnosis of patients with fibromyalgia, although 92.1% (n = 128) believe that they are insufficient for the diagnosis of fibromyalgia, and only 3.6% (n = 5) of the responders said they use the 2010 classification criteria. 70.5% (n = 98) of the responders believe that the patient with fibromyalgia feels rejected by rheumatologists, and 84.9% (n = 118) consider that the patients are dismissed by physicians of other specialties.
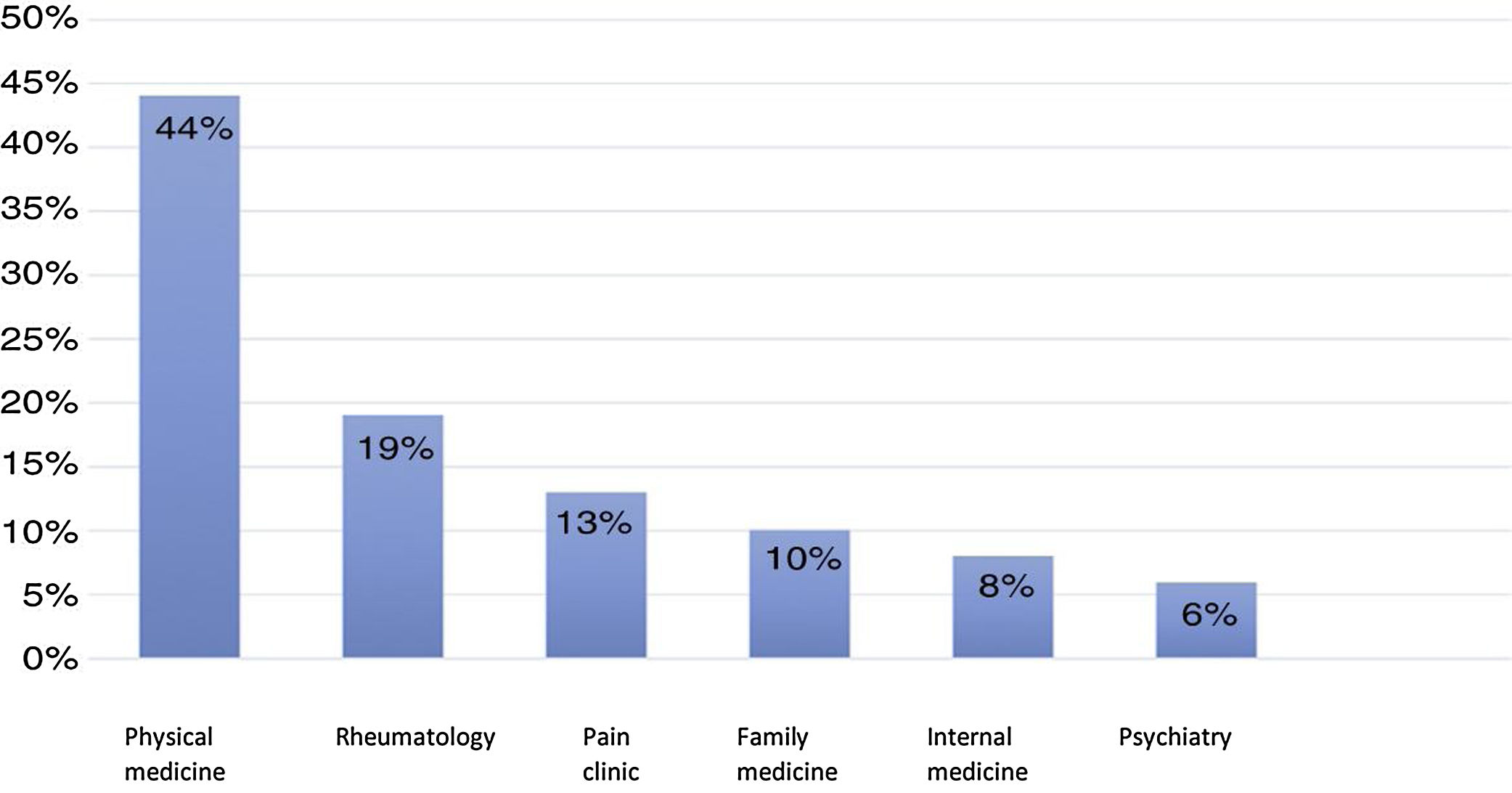
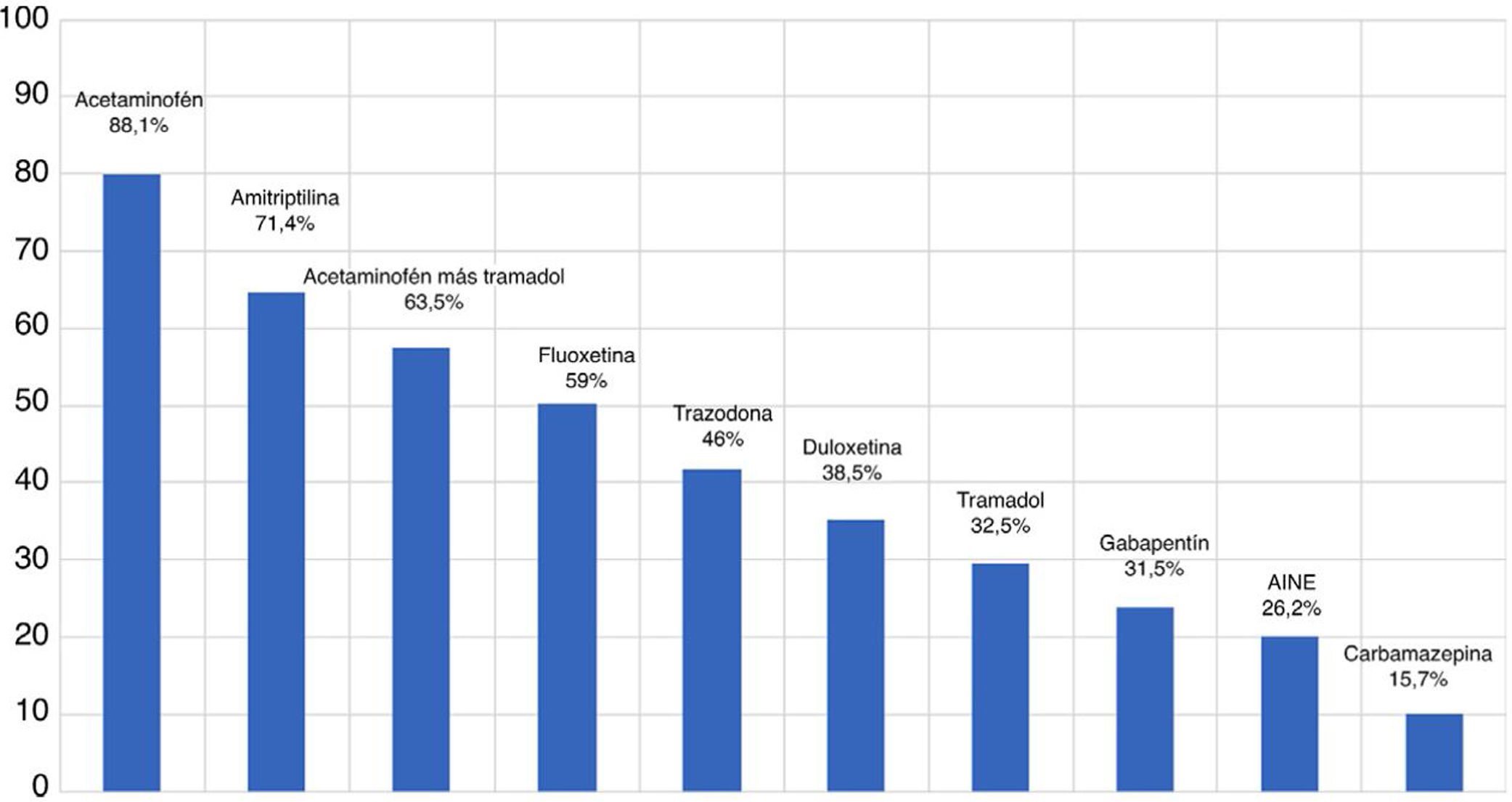
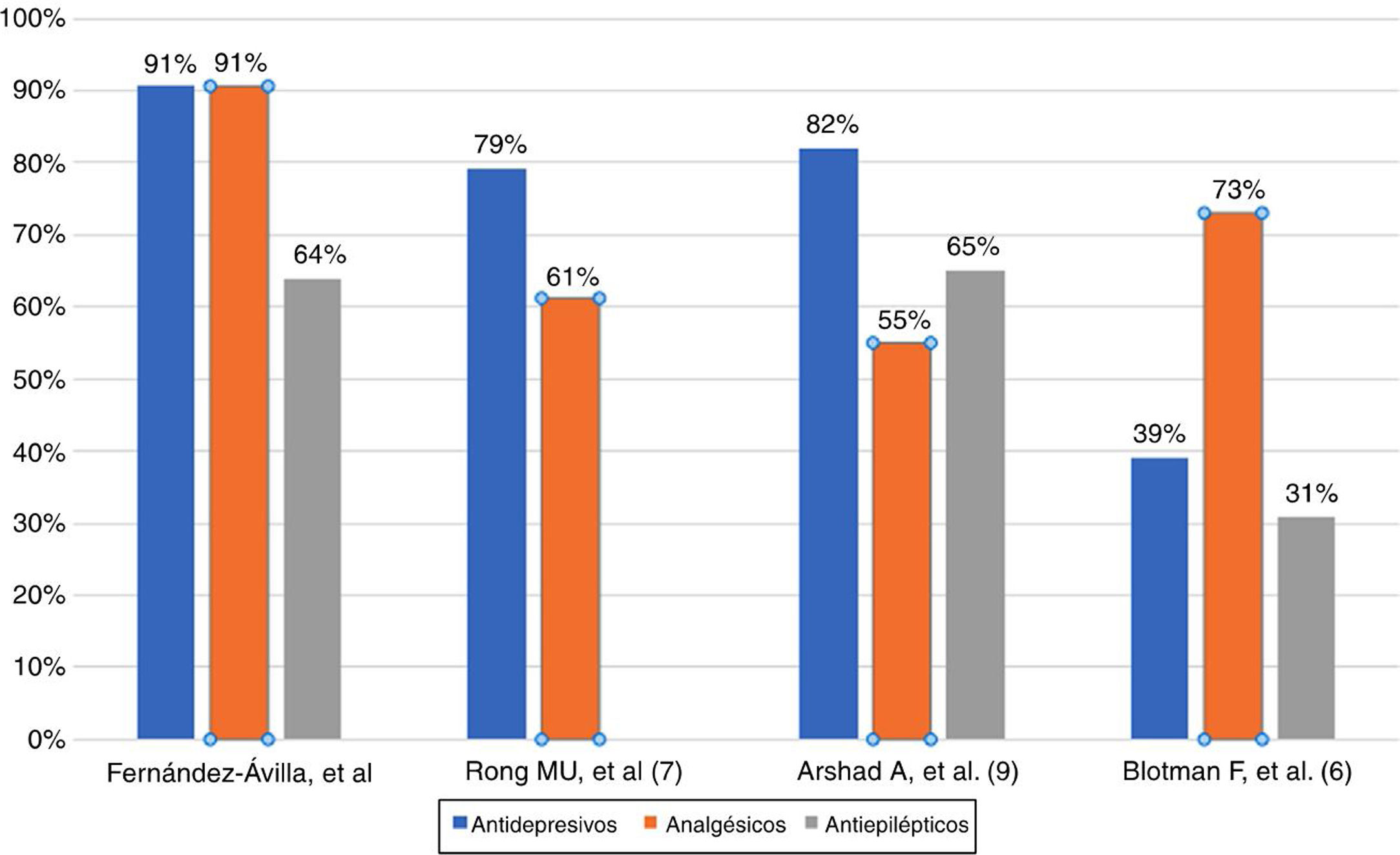
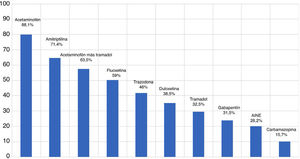
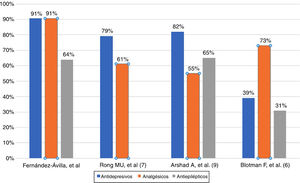
With regards to therapy, the most frequently used medications by rheumatologists in the management of fibromyalgia are antidepressants and analgesics. Both of these medications are used by 90.6% (n = 126) of the responders, followed by antiepileptics 64% (n = 89). The most commonly prescribed analgesic was acetaminophen (88.1%), followed by the combination of acetaminophen with tramadol (63.5%), tramadol (32.5%), and non-steroid anti-inflammatory drugs (NSAID) (26.2%). The most frequently prescribed antidepressant was amitriptyline (71.4%) followed by fluoxetine (59.5%), trazodone (46%) and duloxetine (38,9%). In the anticonvulsants group, pregabalin is the most widely prescribed drug (78.7%), followed by gabapentin (31.5%) and carbamazepine (15.7%) (Fig. 1). With regards to non-pharmacological management, 36% (n = 50) of rheumatologists prescribe non-pharmacological therapy to patients with fibromyalgia. Some of the non-pharmacological measures recommended included physical therapy (80.6%), followed by hydrotherapy (38.1%) and occupational therapy (18.7%). Among the alternative therapies suggested by rheumatologists, homeopathic medicines were prescribed (33.1%), acupuncture (13.7%) and neural therapy (6.5%). In terms of referrals to other specialists for interdisciplinary management, 80.6% (n = 112) of the responders refer the patient to physiatry and 71.2% (n = 99) refer patients to psychiatry, for joint management. Finally, 81.3% (n = 113) of the rheumatologists believe that the patient with fibromyalgia should have as their principal treating physician a specialist other than a rheumatologist. (Fig. 2).
This study is the first approach to describe the concepts and perceptions of rheumatologists in Colombia, with regards to the diagnostic and therapeutic approach of patients with fibromyalgia. The first point highlighted is that one of every four rheumatologists believes that there is not enough evidence to consider fibromyalgia as a disease, as has been shown in other studies that have questioned the actual existence of the condition.13,14,15 There are studies that have discussed the difficulties in making the diagnosis, approaching and treating fibromyalgia by the general practitioner and other specialties such as psychiatry, physical medicine, rehabilitation and rheumatology, reporting that their training in matters associated with fibromyalgia is poor.16,17,18 The most concerning issue for the various specialists is the delay in making a diagnosis, that often gives rise to significant uncertainty with regards to the etiology of the disease, deferring management and obtaining extremely variable outcomes and often unsatisfactory, following the introduction of treatment.10,19 In terms the use of diagnostic criteria, the 1990 ACR diagnostic criteria are used by most rheumatologists for the diagnostic approach to these patients; these data are similar to the reports from other studies, such as the study by Mu R. et al., where 65.5% (463/707 rheumatologists surveyed) still use the 1990 ACR criteria 18 Similarly, in France, 94% of rheumatologists reported the use of these criteria and 79.1% of the general pratitioners17; in Israel, in a study on orthopedists, only 47% used the ACR criteria to diagnose patients with fibromyalgia.20 An investigation compared the use of the 1990 criteria between the rheumatologists in Latin America and in Europe, identifying a use of 61.7% and 35.7%, respectively; these results are consistent with our findings.21 The 2010 classification criteria are less frequently used, probably because it is said that both criteria are valid and are complementary.22 With regards to treatment of patients with fibromyalgia, our study showed a higher use of antidepressants and analgesics, followed by anticonvulsants, which contrasts with the results from other studies, as illustrated in Fig. 3. Patients with fibromyalgia must deal not only with the pain and associated symptoms, but also with the poor acceptance by family members and even doctors involved with their management.23 There is a need to consider that pain is real in patients with fibromyalgia, since notwithstanding the questioning from different medical specialties, there is enough evidence to consider the existence of the disease, and further knowledge is required about its pathophysiology, diagnosis and treatment.24,25 Clearly, the importance given by rheumatologists to the interdisciplinary management of the condition is evident, with high remission rates achieved through joint management with physiatry and psychiatry; however, most rheumatologists felt that the principal treating physician of the patient with fibromyalgia, should be a physiatrist. This study discusses objective information on key aspects of fibromyalgia, since only subjective data were available, mostly limited to informal conversation among specialist. This information may be useful as feedback for our colleagues, and could be the foundation for future studies; for instance, the administration of this same survey to other specialists involved with the management of fibromyalgia, such as psychiatry, internal medicine, physiatry, and family medicine; all of these specialties are involved in the treatment of these patients. Our research group is currently making progress in the administration of this survey to other specialists in Colombia.
ConclusionObjective information is reported on the perceptions about fibromyalgia in a group of rheumatologists, that could be valuable feedback for these practitioners, and may be the foundation for future studies to expand and improve the quality of information for the best approach to this very complex condition.
Compliance with ethical standardsA consent was required to be able to participate in the survey. The survey was self-administered and anonymous, and was completed during the meetings of the Colombian Association of Pain Management Specialists.
Ethical approvalAll the procedures conducted in studies involving human participants are consistent with the ethical standards of the Research and Ethics Committee of the School of Medicine of the Pontificia Universidad Javeriana, and with the Declaration of Helsinki of 1964 and subsequent amendments, or similar ethical standards.
FinancingThis paper was not funded by any private organization.
Conflict of interestsThe authors have no conflict of interests to disclose.
Please cite this article as: Fernández-Ávila DG, Rincón Riaño DN, Ronderos DM, Gutiérrez JM. CONCEPTOS Y PERCEPCIONES ACERCA DEL DIAGNÓSTICO Y TRATAMIENTO DE LA FIBROMIALGIA EN UN GRUPO DE REUMATÓLOGOS COLOMBIANOS. Rev Colomb Reumatol. 2020;27:256–261.