Brodie's abscess is a bone infection which usually presents as a subacute course. Surgical debridement followed by intravenous antibiotics has been the classical therapeutical approach. This report describes a case of a 12-year-old boy who presented with clinical, analytical, and radiological features of subacute osteomyelitis affecting distal tibia, and who was successfully managed with a prolonged course of exclusively oral antibiotics avoiding a surgical procedure. An exclusively oral antibiotherapy approach for Brodie's abscess could provide comparable success rates to surgical debridement followed by intravenous antibiotics in selected pediatric patients.
El absceso de Brodie consiste en una infección del tejido óseo que suele presentarse con un curso subagudo. El desbridamiento quirúrgico seguido de antibióticos por vía intravenosa ha sido el enfoque terapéutico clásico. Reportamos el caso de un niño de 12 años que presentó características clínicas, analíticas y radiológicas de osteomielitis subaguda en la tibia distal y que fue tratado exitosamente con antibioterapia por vía oral sin precisar desbridamiento quirúrgico. El enfoque de antibioterapia exclusivamente por vía oral para el absceso de Brodie podría proporcionar tasas de éxito comparables al desbridamiento quirúrgico seguido de antibióticos intravenosos en pacientes pediátricos seleccionados.
Brodie's abscess presents as a subacute osteomyelitis usually located at the metaphysis of tubular bones, with the tibia and femur being the most common involved bones.1,2 The classic therapeutic management has consisted of surgical debridement followed by a cycle of long-term intravenous antibiotics.3–5 This approach leads to prolonged hospitalization, increasing health costs and being a significant inconvenience for the family and work routines. We report a substantially different approach, performing exclusively oral treatment followed by complete resolution of the process.
Case presentationA 12-year-old boy presented with a one-month history of limping and continuous pain affecting his left ankle. He presented fever (maximum 38°C) during 3 days at the time of symptom onset, afterwards remaining afebrile. At physical examination, edema of the involved limb without erythema was observed. The patient was healthy and no history of trauma or red flags were reported (fever, weight loss, sweats), but an infected whitlow on his left toe was present at onset.
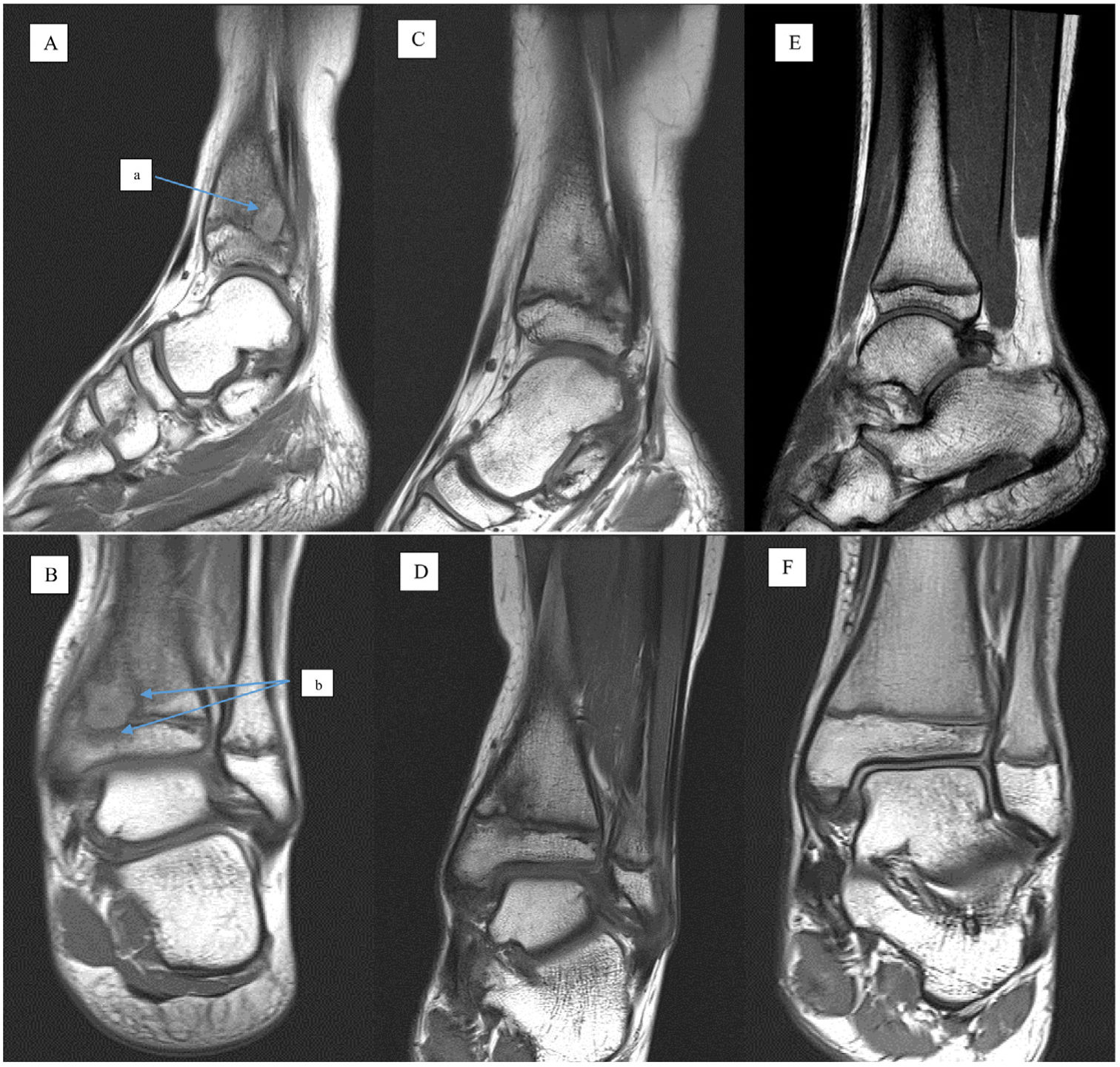
A plain radiograph was performed showing an osteolytic lesion on the left distal tibial metaphysis. A subsequent MRI revealed an endomedullary lesion appearing hypointense in T1, well defined by a slight rim enhancement, sized 14mm×15mm×12mm, further associated with surrounding low signal intensity in relation to bone tissue edema and reactive sclerosis (Fig. 1: images A and B). These findings were therefore considered as suggestive of Brodie abscess in relation to osteomyelitis affecting the posteromedial region of the tibial metaphysis. Laboratory examinations showed normal blood cell count and blood smear lacked abnormalities of leukocytes and erythrocytes. Erythrocyte sedimentation rate (ESR) was 9mm/h and C-Reactive protein (CRP) 0.06mg/L. Multidisciplinary assessment with pediatric orthopedic surgeons was undertaken, deciding to initiate oral clindamycin (50mg/kg/day every 8h) and eluding bone biopsy, since the patient had a good general health and laboratory data lacked of abnormal results.
The MRI evolution of the subacute osteomyelitis in distal tibia is shown. (A, B) Sagital and coronal T1-weighted images at diagnosis: Unenhanced image indicating the central abscess cavity with slight hyperintense rim (a) further associated with surrounding low signal intensity corresponding to bone tissue edema and reactive sclerosis (b). (C–F) Subsequent sagital and coronal T1-weighted images showing a decrease of the size of both the lesion and the surrounding edema.
The patient showed a clinical response and left ankle pain disappeared after two weeks of treatment initiation. A second MRI was carried out after 6 weeks of treatment, which revealed a frank decrease of the size of both the lesion and the surrounding edema (Fig. 1: images C and D). Given the satisfactory outcome and adequate tolerance to prolonged oral antibiotics, conservative handling was maintained eluding surgery. Clindamycin was finally withdrawn after 16 weeks of sustained treatment, checking no abnormalities on laboratory tests (which showed normal blood cell count, ESR of 5mm/h and CRP<0.03mg/L) and sustained absence of symptoms.
Six months after antibiotic discontinuation, the patient continued asymptomatic and acute phase reactants remain negative. A third MRI was performed, showing a complete radiological resolution (Fig. 1: images E and F). After 3 years of follow-up, no impaired growth of affected bone due to destruction of epiphyseal growth plate was observed.
DiscussionTo the best of our knowledge, we hereby present the first pediatric patient with Brodie's abscess successfully treated entirely with oral antibiotics. Brodie's abscess is considered to be a type of subacute osteomyelitis which is defined as any infectious process affecting bone tissue persisting for more than 2 weeks in absence of symptoms of acute illness.1–3 Regarding pathogenic mechanisms, the hematogenous spread is the most frequently related to Brodie's abscess albeit it may also occur in the setting of trauma.6
Patients usually present a history of recurrent dull pain and local sensitivity. Swelling, erythema, or limping may be found. Occasionally, it associates fever or malaise. However, the common lack of such systemic signs often leads to misdiagnosis. The duration of symptoms ranges from 1 month to 3 years.7 It is generally observed in patients younger than 25 years of age, and there is a slight male predominance (male to female ratio of 3:2).8 Our patient was a 12-year-old boy.
Staphylococcus aureus (30–60%), Pseudomonas (5%), Klebsiella (5%) and coagulase-negative Staphylococcus (5%) are the most frequently isolated pathogens in bone abscess samples.9 Regarding our patient, no blood culture or abscess sample were taken due to the long period of time since symptom onset and to the lack of fever at admission in our hospital. Accordingly, no biopsy of the lesion was either performed because of the absence of red flags (fever, weight loss, sweats) in addition to normal hematological and biochemical parameters.
About plain radiography, Brodie abscess usually presents as an intramedullary rounded lucent lesion, usually eccentric, varying in size with surrounding sclerosis and some periosteal thickening.4 On MRI, Brodie's abscess is a metaphyseal, well defined intraosseous lesion with central core which represents the abscess cavity. This central cavity is composed of a high protein component and appears as low signal intensity on T1-weighted and high on T2-weighted and STIR images. A peripheral rim of higher signal intensity than the central abscess cavity is found at T1 sequences due to highly vascularized granulation tissue. Finally, an outer layer is defined by a peripheral halo of low signal intensity ring on T1-weighted images due to bone edema.10 Differential diagnosis of Brodie abscess includes benign and malignant bone lesions such as cysts, osteoid osteoma, giant cell tumor, chondroblastoma and Ewing sarcoma.11
The basis of osteoarticular infections (OAI) treatment in pediatric patients includes a short course of intravenous antibiotics from two to four days followed by an oral course for two to three weeks.12,13 The Pediatric Rheumatology Department of our hospital has a large experience using exclusively oral antibiotics for treatment of OAI (acute hematogenous osteomyelitis and septic arthritis). This therapeutic approach for OAI is offered to patients who meet the following criteria: good general health, oral tolerance, possibility of close follow-up, CRP value less than 100mg/L and processing of microbiological samples previous to antibiotherapy initiation (arthrocentesis when septic arthritis, blood culture, real-time polymerase chain reaction (PCR) of Kingella kingae from synovial fluid when suspected).14 On the other hand, patients in which Staphylococcus aureus infection is suspected (generally poor health, high fever, CRP value of more than 100mg/L, coming from high methicillin-resistant Staphylococcus aureus endemic sites or surgery indication) required initial intravenous antibiotics in order to avoid complications and sequelae.15
In this way, Alcobendas et al. performed a prospective study that compared 25 outpatients who received just oral antibiotics at our hospital, with 228 hospitalized children who received both intravenous and oral antibiotics from other hospitals in the Spanish Network of Osteoarticular Infections. The study showed that outpatients with OAI had favorable outcomes without complications or sequelae in 100% of cases when they received oral antibiotics without intravenous antibiotics.15
In the line with above-mentioned evidence, we decided a conservative management of our patient with entirely oral treatment given the absence of risk factors for complications or sequelae (no fever, good general health, normal CRP, oral tolerance and possibility of close follow-up). Although conventional treatment of Brodie's abscess entails the combination of surgical debridement and prolonged intravenous antibiotherapy,1,5,6 the excellent clinical outcome of the patient and the progressive radiological improvement observed by MR controls, allowed to maintain the antibiotic treatment exclusively avoiding a surgical approach during the course of the disease. So far, no other therapeutic approaches have been reported, being this patient the first case of Brodie's abscess managed with exclusively oral antibiotics.
The management carried out in our center allows a less invasive approach for the patient and reduces the sanitary costs derived from hospital admission and from school absenteeism. For this reason, oral treatment of Brodie's abscess should be considered in pediatric patients without risk factors for complications or sequelae previous mentioned. Further studies are necessary to investigate the efficacy and safety of our therapeutic approach with exclusively oral antibiotics in pediatric patients diagnosed with this type of osteoarticular infection.
Ethical considerations- •
A written informed consent was requested from patient's parents to participate in the research described.
- •
The research complies with current regulations on bioethics research and it obtained the authorization of the institution's ethics committee.
- •
The authors declare that this article does not contain personal information that allows to identify the patients.
No specific funding was received from any bodies in the public, commercial or not-for-profit sectors to carry out the work described in this article.
Conflicts of interestThe authors have declared no conflicts of interest.