Raynaud’s phenomenon is a sentinel event in systemic sclerosis; it is generally long- lasting, and repeated attacks produce, ultimately, structural consequences and complications, such as digital ulcers. Nailfold videocapillaroscopy is a non-invasive tool that allows assessing accurately these changes. Digital ulcers are the most aggressive and frequent microvascular complication in this disease, causing severe pain and significant functional sequelae. This literature review focuses on Raynaud's phenomenon as a central event in systemic sclerosis, its peculiarities in this entity, the role of capillaroscopy as a biomarker in this vasculopathic phenomenon, as well as a on a clinical and pharmacological approach to digital ulcers in this illness.
El fenómeno de Raynaud es un evento centinela en la esclerosis sistémica; por lo general es de larga duración, y los ataques repetidos producen, en última instancia, consecuencias estructurales y complicaciones tales como úlceras digitales. La videocapilaroscopia del lecho ungueal es una herramienta no invasiva que permite evaluar en forma precisa estos cambios. Las úlceras digitales son la complicación microvascular más agresiva y frecuente en esta enfermedad, causando dolor severo y secuelas funcionales importantes. Esta revisión de la literatura se centra en el fenómeno de Raynaud como evento central en la esclerosis sistémica, sus peculiaridades en esta entidad, y el papel de la capilaroscopia como biomarcador para este fenómeno vasculopático, así como en un enfoque clínico y farmacológico de las úlceras digitales en esta enfermedad.
Systemic sclerosis (SSc) is a connective tissue disease characterized by small vessel vasculopathy, generating an inflammatory and autoimmune response with dysfunction of fibroblasts, leading to abnormal extracellular matrix production and marked fibrosis in various organs and tissues.1 The sentinel clinical event preceding for several years the onset of many organic manifestations is Raynaud phenomenon (RP), which, in this disease, is severe and frequently progresses to digital ulcers (DU) and/or critical ischemia; however, complications of this disorder can be micro or macrovascular and involve organs, such as the kidney and pulmonary arterial circulation.2 The objective of this review is to deepen and update the latest evidence of RP and digital ulcers in SSc.
MethodsA qualitative, systematic review of the literature was conducted, according to published recommendations,3 using the following research strategy in PubMed and Google Scholar, restricting as Major Topic: (("Raynaud Disease"[Majr]) AND "Scleroderma, Systemic"[Majr]) AND "Skin Ulcer"[Majr] (("Raynaud Disease"[Majr]) OR "Scleroderma, Systemic"[Majr]) OR "Skin Ulcer"[Majr], from 2012 to 2017, only in English.
Systemic sclerosis: prototype of vascular diseaseThere is a close pathophysiological and clinical correlation in SSc; organic manifestations are the result of an injury and endothelial dysfunction, which appear to be secondary to the action of free radicals, infectious or chemical agents; this alteration results in the activation of the immune, vascular and coagulation systems, producing microthrombosis, intimal hyperplasia of the small arteriolar vessels, generating a vicious cycle of tissue hypoxia and chronic ischemia, activation of resident fibroblasts, with subsequent increased fibrosis of the vascular wall.4
Vascular findings in SSc are crucial for diagnosis; in 2013, new classification criteria were published in consensus among the American College of Rheumatology and the European League Against Rheumatism, where nine points are required to classify a patient with SSc; the pre-ulcerative lesions ("pitting scars") and RP brings three points; DU, abnormal videocapillaroscopy, teleangiectasia and the presence of pulmonary arterial hypertension, each represent two points.5
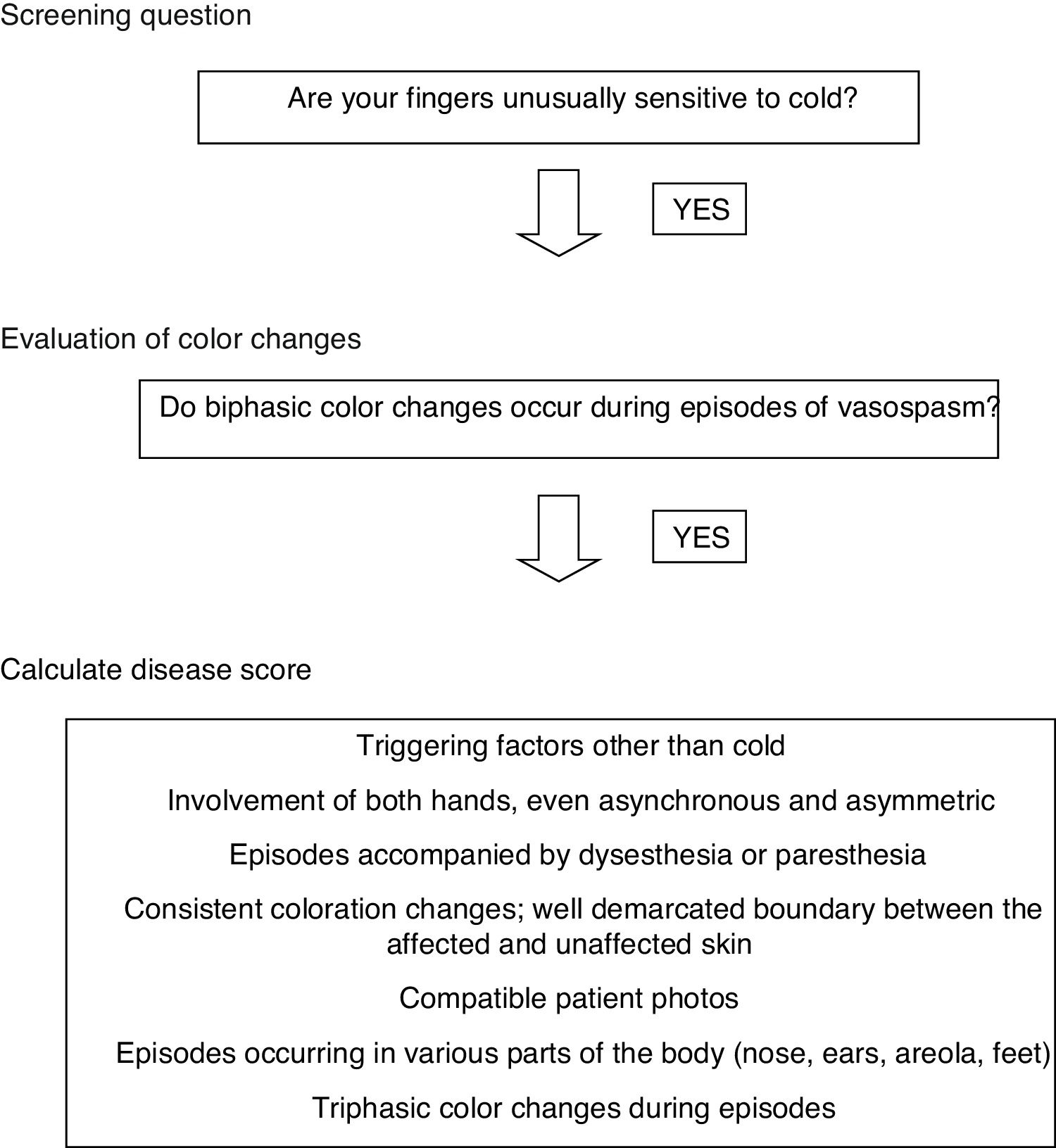
Raynaud's phenomenon in SScThis is undoubtedly the sentinel clinical event in this disease; it is generally long- lasting and, initially, similar to primary RP, only generating functional sequelae; repeated attacks produce, ultimately, structural consequences and complications.6 As RP precedes the diagnosis of SSc on several occasions, it is crucial for the clinician to know when to suspect that this phenomenon is not primary, in order to establish an early diagnosis, avoid complications, decide additional work-up, with the purpose of making an early referral to rheumatology. An international expert consensus was recently published, where a three - step scheme for the diagnosis of RP was proposed7 (Fig. 1).
Primary RP is confirmed if there is an affirmative answer to the two initial questions and, at least, three of the items available in the third question for calculating score, absence of clinical stigmata, no history of connective tissue disease, negative antinuclear antibodies and normal videocapillaroscopy.7
It is also essential to establish a proper differential diagnosis of RP: acrocyanosis, livedo reticularis, peripheral neuropathy, erythromelalgia, among others.8
If you are suspecting secondary RP, remember that SSc is not the only ailment that has been associated with this clinical condition; other illnesses, such as: systemic autoimmune and myeloproliferative disorders, chronic atherosclerotic arterial occlusive disease, thromboangiitis obliterans, thoracic outlet syndrome, embolic or thrombotic phenomena, vibration-induced trauma or medications, should be ruled out.9
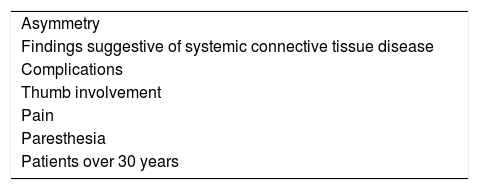
If secondary RP is confirmed (Table 1), the next step is the application of two diagnostic aids: erythrocyte sedimentation rate and antinuclear antibodies; if they are positive, along with the detection of diffuse edema of the fingers ("puffy fingers") in the physical examination, early SSc diagnosis can be established.10
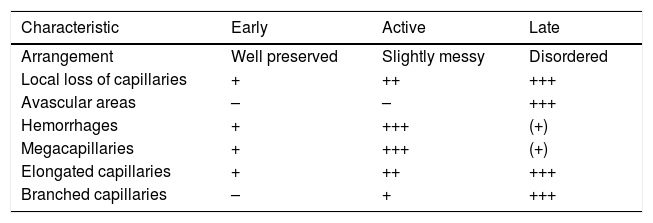
Capillaroscopy asa biomarker in SScThere is also a correlation between the evolution time of SSc and vascular changes; these variations can be assessed through a non-invasive tool, which is nailfold videocapillaroscopy (NVC); these alterations range from an inflammatory response with increased angiogenesis to its reduction, with generation of avascular areas11 (Table 2). This instrument, now available in our midst, enables early diagnosis of SSc, monitors its progression, predicts organ specific involvement, and aids in drug treatment settings; it is also a prognostic marker: large avascular areas are an independent predictor of mortality, and late patterns are associated with increased likelihood of lung and esophageal affection.12,13
Capillaroscopic patterns in systemic sclerosis.
| Characteristic | Early | Active | Late |
|---|---|---|---|
| Arrangement | Well preserved | Slightly messy | Disordered |
| Local loss of capillaries | + | ++ | +++ |
| Avascular areas | – | – | +++ |
| Hemorrhages | + | +++ | (+) |
| Megacapillaries | + | +++ | (+) |
| Elongated capillaries | + | ++ | +++ |
| Branched capillaries | – | + | +++ |
Calcium channel antagonists remain the first line of therapy; there is also sufficient evidence with other drugs, such as angiotensin receptor antagonists and alpha-adrenergic blockers, nitrates, statins, serotonin reuptake inhibitors, prostacyclin analogues, phosphodiesterase inhibitors, antagonists of endothelin receptors and invasive options, as botulinum toxin and microsurgery.14 Experts also recommend pharmacological alternatives depending on the intensity of RP attacks: mild (about 5 weekly attacks) and severe (between 5 and 25 attacks); it is also common to adopt combination therapies rather than staggered and there is a tendency to use, as second line after calcium antagonists, phosphodiesterase inhibitors.15,16 Bear in mind, that in case of refractoriness, differential diagnosis and macrovascular disease should be considered.17
Digital ulcers in systemic sclerosisIt is estimated that at least 40–50% of all subjects with SSc experience one or more digital ulcers (DU) at some point in the course of their illness, causing severe pain and significant functional sequelae; of these individuals, 31–71% will have recurrent DU and 30% of patients with persistent DU will have permanent tissue loss.18
In the VEDOSS cohort, 68% of the individuals with RP had positive antinuclear antibodies. The baseline presence of teleangiectasia, digital ulcers and pitting scars were the most common clinical findings.10
The pathogenesis of digital ischemia leading to DU is similar to the general pathophysiology of RP: abnormalities in neuroendocrine control mechanisms, vascular structural changes (easily assessable non-inflammatory microangiopathy by the NVC and digital arterial disease) and hematological factors (hypercoagulability in association with antiphospholipid syndrome).19 The absence of response of arteriovenous anastomosis to peripheral nerve-mediated vasoconstriction was described, especially in the finger pulp, a frequent anatomic site where digital ulcers were present.20
There have been risk factors identified for its presentation: the diffuse variety of SSc, early onset of RP, high modified Rodnan skin score values (indicating extent of skin involvement), the rapid emergence of non-Raynaud’s organ compromise, male gender, the presence of anti-centromere and anti Scl-70 antibodies, as well as the late pattern and the rapid pattern change in the NVC, along with alterations in macrovascular endothelial dysfunction (lower flow-mediated dilation), peripheral atherosclerosis and hypercholesterolemia.21–23
Clinical approach to the patient with SSc and DUYou should always keep in mind, as it occurs in refractory RP, to rule out macrovascular disease (involved arteries: ulnar and popliteal, among the most common, which is more frequent in patients with SSc than in the general population).17 In order to establish this diagnosis, the clinician should inquire about the presence of risk factors for atherosclerotic disease. Other critical issues to identify in the anamnesis are: the increased frequency, duration and severity of RP attacks, permanent discoloration of the fingers (imminent sign of critical ischemia); additionally, if symptoms affect daily activities and persistence of night pain should be questioned.19
On physical examination, it is crucial to identify local aggravating factors such as: sclerodactyly, calcinosis and prominent capillaries in the NVC; evaluation of peripheral pulses for early detection of macrovascular disease is critical. DU most often affect anatomical sites as follows: fingertips, extensor surfaces and any location on fingers and toes.19
You should also rely on diagnostic aids as plain radiographs, which often evidence the presence of acroosteolysis, osteomyelitis or calcinosis; in some cases, you must apply for a MRI if there is early suspicion of osteomyelitis.19
Pharmacological treatment of digital ulcers in systemic sclerosisTwo aspects should be considered for the decision of specific medications: if you are going to do prevention or establish active treatment. In the first scenario, endothelin receptor antagonists are the first line; in the second situation, similar to RP, calcium antagonists are backed by more solid evidence and are the first line; combination therapies are also a common strategy; randomized trials support endothelin receptor antagonists as a second or third line alternative.24–27
Another factor influencing the decision of specific drugs is the severity of DU, which can be determined by the number of DU displayed in one year (4 in mild and more than 10 in serious situations).28,29
Recent evidence supports additional pharmacological therapies: topical glyceryl trinitrate, showing perfusion improvement in the core of the digital ulcer and in blood flow in fingertips and extensor digital ulcers.30 Additionally, intravenous iloprost is considered by several authors, as the first-line treatment option for the acute management of systemic sclerosis-related digital vasculopathy, with significant reduction in the frequency, as well as an increase in the number of subjects free of new digital ulcers.31
ConclusionsSystemic sclerosis is an autoimmune disease where vasculopathy and its clinical translation, Raynaud phenomenon, are sentinel events preceding, in years, visceral involvement. Early identification of secondary Raynaud, as well as identification of specific patterns in the nailfold videocapillaroscopy and early and prompt initiation of combination therapy can prevent the development of complications and in an unfailingly way, the digital irreversible ischemia.
Funding sourceOwn resources.
Conflict of interestThe authors declare absence of any conflict of interest.
Please cite this article as: Velásquez-Franco CJ, Rodríguez-Castrillón JC. Fenómeno de Raynaud, capilaroscopia y úlceras digitales como eventos centinela en la esclerosis sistémica. Rev Colomb Reumatol. 2020;27:170–174.