Spondyloarthritis is a group of chronic inflammatory diseases. Several factors of the disease remain unknown, including clinical and radiological behavior, the demographic characteristics and burden of disease in Colombian patients.
ObjectiveTo characterize the demographic aspects, the clinical and paraclinical behaviour, and the therapeutic requirements of a cohort of patients with spondyloarthritis followed-up in the Hospital Pablo Tobón Uribe from January 1, 2005 to December 31, 2017.
MethodologyCohort study. The population was characteriszed using descriptive statistics, qualitative variables using simple and relative frequencies, and quantitative variables using means and standard deviation or medians with their interquartile ranges.
ResultsThe cohort consisted of 181 patients, 100 men (54.9%) and 81 women (44.5%). Just under one half (45.1%) had ankylosing spondylitis, 18.1% undifferentiated spondyloarthritis, 17.1% psoriatic arthropathy, 14.8% reactive arthritis, and 4.4% inflammatory bowel disease. More than two-thirds (69.8%) of the patients had peripheral manifestations, and 67% had axial. A positive HLAB27 was observed in 55.6% of patients. The MRI showed acute and chronic changes in the sacroiliac in 69% and 37%, respectively, with radiological sacroiliitis being observed in 59.5% of cases. The large majority (91.1%) of the patients were treated with NSAIDs, 60.1% with sulfasalazine, 43.4% with COX2 inhibitors, and 33.7% with methotrexate. TNFα inhibitors were required by 56.6% of the subjects 3 years after the onset of symptoms. The most commonly used biological drugs were Adalimumab (31.1%), etanercept (21.7%), infliximab (13.1%), golimumab 6.1%, and certolizumab 0.5%.
ConclusionsOur population was characterized by a high activity and functional compromise demonstrated by the high scores of BASDAI and BASFI, and because 56.6% of the patients required anti-TNFα agents.
Las espondiloartritis son un grupo de enfermedades inflamatorias crónicas. Se desconoce su comportamiento en nuestro medio, al igual que el comportamiento clínico y radiológico, las características demográficas y la carga de enfermedad en los pacientes colombianos.
ObjetivosCaracterizar los aspectos demográficos, el comportamiento clínico y paraclínico y los requerimientos terapéuticos de la cohorte de pacientes con espondiloartritis seguidos en el Hospital Pablo Tobón Uribe desde el 1.o de enero del 2005 hasta el día 31 de diciembre del 2017.
MetodologíaEstudio de cohorte. La población se caracterizó mediante estadística descriptiva, las variables cualitativas mediante frecuencias simples y relativas, en tanto que para las cuantitativas se emplearon medias y desviación estándar o medianas con sus rangos intercuartílicos.
ResultadosLa cohorte está constituida por 181 pacientes, 100 hombres (54,9%) y 81 mujeres (44,5%). El 45,1% tenía espondilitis anquilosante, el 18,1% espondiloartritis indiferenciada, el 17,1% artropatía psoriásica, el 14,8% artritis reactiva y el 4,4% enfermedad inflamatoria intestinal. El 69,8% de los pacientes tenía manifestaciones periféricas y el 67% axiales. El 55,6% de los pacientes tuvo HLAB27 positivo. La RMN mostró cambios agudos y crónicos en las sacroilíacas en 69% y 37%, respectivamente; en el 59,5% de los casos se observó sacroileítis radiológica.; el 91,1% de los pacientes se trató con AINE, el 60,1% con sulfasalazina, el 43,4% con inhibidores COX2 y el 33,7% con metotrexate. El 56,6% de los sujetos requirió inhibidores-TNFα 3 años después del inicio de los síntomas. Los biológicos más utilizados fueron adalimumab (31,1%), etanercept (21,7%), infliximab (13,1%), golumimab (6,1%) y certolizumab (0,5%).
ConclusionesNuestra población se caracterizó por una alta actividad y gran compromiso funcional, lo que se refleja en altos puntajes de Basdai y Basfi y en que el 56,6% de los pacientes requirió agentes anti-TNFα.
Spondyloarthritis (SpA) is a heterogeneous group of diseases that share a broad clinical and immunogenetic spectrum and that, due to the diversity of their manifestations constitute a challenge for the diagnosis in early stages. This group of entities includes ankylosing spondylitis, reactive arthritis, psoriatic arthritis, spondyloarthritis associated with inflammatory bowel disease, juvenile-onset spondyloarthritis, and undifferentiated spondyloarthritis.1,2
The development and evolution of new classification criteria have allowed their earlier identification, based on imaging (radiographic or magnetic resonance) or genetic (presence of HLA-B27) aspects coupled with a series of clinical and laboratory manifestations. In addition, patients are classified into those with predominantly peripheral or axial involvement; the latter are subdivided into those forms with radiographic or non-radiographic evidence.3
This new classification has allowed the introduction of the term «non-radiographic axial spondyloarthritis», which refers to patients with clinical, laboratory or genetic manifestations suggestive of spondyloarthritis in the absence of signs of axial involvement or sacroiliitis on the plain radiography, but evident on nuclear magnetic resonance images. This evidence has given rise to a new taxonomy in SpAs in order to facilitate their understanding as follows: axial SpA with radiographic sacroiliitis, axial SpA without radiographic sacroiliitis (sacroiliitis in MRI or positive HLA-B27 with clinical manifestations); peripheral SpA with psoriasis, with inflammatory bowel disease (Crohn’s disease, ulcerative colitis or undifferentiated colitis); SpA with preceding infection (reactive), without psoriasis, inflammatory bowel disease or preceding infection (undifferentiated SpA). In recent decades, it has been of great interest to improve early diagnosis and timely treatment to stop the devastating effect that these diseases have in young people in full productive capacity.4,5
There are immunogenetic, etiopathogenic, clinical, radiological and treatment aspects that have aroused the interest of researchers worldwide.6,7 However, the topics that have evolved the most in this group of diseases are genetic factors, inflammatory low back pain as a crucial cardinal sign in the classification criteria and diagnostic images, especially magnetic resonance imaging, essential for the early diagnosis and treatment of the SpAs.8,9
Ankylosing spondylitis, the most common of all types of SpA, usually begins in the third decade of life, 5 years earlier in HLA-B27 positive patients than in those who are HLA-B27 negative. In the Spanish Regisponser registry, the average age of onset was 30 years. It occurs more frequently in men than in women, with a 2−3:1 ratio, while in patients with non-radiographic axial spondyloarthritis, the distribution by sex is equal.10
SpAs have a high prevalence in Caucasian populations, far from the equatorial regions or from the tropics. The estimated prevalence of axial spondyloarthritis is about 0.32–1.4%, according to the population studied, while the prevalence for all types of spondyloarthritis, including the peripheral forms, varies between 0.2% in Southeast Asia and 1.6% in the Northern Arctic populations. In African-American and Japanese populations these are very rare diseases. Spain has a reported prevalence of 1.8% and in the United States is close to 1%.11–13
In Colombia there are still great questions regarding the behavior of this group of diseases, the largest cohort studies reported were conducted at the Central Military Hospital (Hospital Militar Central) in Bogotá (139 and 218 patients) and at the Pablo Tobón Uribe Hospital (HPTU) in the city of Medellin (71 patients).14,15
Londoño et al.16 described the prevalence of different rheumatic diseases (osteoarthritis, fibromyalgia, rheumatoid arthritis, gout, lupus, Sjögren’s syndrome, dermatomyositis, systemic sclerosis and SpAs), in addition to various musculoskeletal disorders (soft tissue rheumatism or appendicular regional pain, unspecified musculoskeletal discomfort and non-rheumatic diseases) in Colombia, based on the application of a widely validated instrument: the Copcord model, and interviewed 6,693 individuals in the 6 most important capital cities of the country. The aforementioned researchers established that the prevalence of ankylosing spondylitis in people over 18 years of age in cities such as Bogota was 0.08%, in Medellin 2.2% and in Cali 0.47%; more than 64% of the people interviewed were women.
Knowledge of the clinical and radiological behavior, as well as of the demographic characteristics and the burden of the disease in Colombian patients with spondyloarthritis, is important to promote timely diagnosis and treatment, in addition to planning comprehensive and correctly targeted strategies in the healthcare services.17–19
ObjectiveTo characterize the demographic aspects, the clinical and immunogenetic behavior of the acute phase reactants, the radiological behavior and the therapeutic requirements of the cohort of patients with SpA followed-up in the HPTU from January 1, 2005 to December 31, 2017.
DesignDescriptive cross-sectional study that follows-up a previously described cohort, which includes all patients with SpA who were diagnosed and followed-up for at least one year in the HPTU between January 2005 and December 2017.
Patients and methodsAll patients over 18 years of age with spondyloarthritis who met the ASAS criteria (Ankylosing Spondilytis Assessment Study) and consulted the emergency rheumatology services, who were evaluated by a rheumatologist, from January 1, 2005 to December 31, 2017 were included. Those patients with other rheumatic diseases that could interfere with clinimetrics, such as rheumatoid arthritis, lupus, arthrosis of the spine and fibromyalgia, were excluded. Patients with autoimmune diseases, viral infections (HIV, hepatitis), and neoplasms were also excluded. The protocol was approved by the research and ethics committee of the HPTU.
The variables included in the analysis were: demographic (age, gender, age at onset of symptoms, personal and family history of SpA, psoriasis, uveitis, IBD); clinical (initial manifestation of SpA: talalgia, uveitis, calcaneal enthesitis, dactylitis, cutaneous psoriasis, nail psoriasis, diarrhea, urethritis, arthritis, Crohn's disease, ulcerative colitis, inflammatory low back pain, gluteal pain, morning stiffness, psoriasis, inflammatory bowel disease, and the type of spondyloarthritis); clinimetric (Basdai and Basfi score at baseline, maximum and average during the evolution of the disease and at the initiation of the tumor necrosis factor inhibitor [TNF-i]); laboratory (acute phase reactants [ESR and CRP], HLA-B27); imaging (MRI [spinal and sacroiliac joint bone marrow edema], presence of erosions, syndesmophytes, fusion of the sacroiliac joints and plain radiographs thereof to apply the New York classification); and treatment (NSAIDs, oral steroids, COXIBS, methotrexate, sulfasalazine, TNF-i).
MethodologyCohort study. The population was characterized by descriptive statistics, the distribution of the continuous variables was determined with the Kolmogorov–Simirnoff method for those with n of 50 or more, and with the Shapiro–Wilk method for those with n less than 50. The parametric variables were summarized with means and standard deviations (SD) and the non-parametric variables with medians and interquartile ranges (IQR). The SPSS software, version 22, HPTU license, was used. The research was approved by the ethics committee of the institution and did not confer risk to the patients.
ResultsThe cohort consisted of 181 patients, 81 women (44.5%) and 100 men (54.9%), with a mean age of 45.3 years (SD = 13.39 years) and a range between 20 and 83 years. 24.2% (44) of the subjects were 35 years old or younger, 40.6% (74) between 36 and 50 years old and 35.2% (64) were older than 50 years.
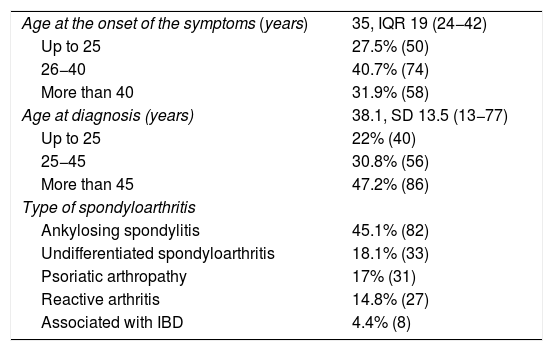
The average age at admission to the cohort was 39.31 (SD = 12.32 years), with a range between 17 and 77 years. 24.7% (45) were 30 years old or younger, 54.4% (99) between 30 and 50 years old and 20.9% (38) were older than 50 years. The median follow-up time of the patients was 5 years (IQR = 32.0−32). 46.2% (84) were followed-up for more than 6 years, 30.8% (56) between 3 and 6 years and 23.1% (42) for less than 3 years. The duration to establish the diagnosis since the onset of the symptoms was around 5 ± 7 years, similar to what happened in the different cohorts worldwide (6 years). The demographic characteristics of the population are described in Table 1.
Demographic characteristics of the pupulation of patients with spondyloarthritis.
| Age at the onset of the symptoms (years) | 35, IQR 19 (24−42) |
| Up to 25 | 27.5% (50) |
| 26−40 | 40.7% (74) |
| More than 40 | 31.9% (58) |
| Age at diagnosis (years) | 38.1, SD 13.5 (13−77) |
| Up to 25 | 22% (40) |
| 25−45 | 30.8% (56) |
| More than 45 | 47.2% (86) |
| Type of spondyloarthritis | |
| Ankylosing spondylitis | 45.1% (82) |
| Undifferentiated spondyloarthritis | 18.1% (33) |
| Psoriatic arthropathy | 17% (31) |
| Reactive arthritis | 14.8% (27) |
| Associated with IBD | 4.4% (8) |
SD: standard deviation; IBD: inflammatory bowel disease; IQR: interquartile range.
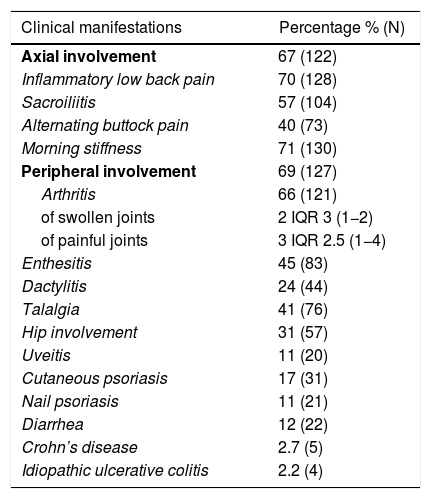
7.7% (14) of the patients with ankylosing spondylitis had a family history of SpA, which was observed in 3.8% (7) of those with psoriatic arthropathy, 1.1% (2) with reactive arthritis and in 0.5% (1) of those diagnosed with IBD or undifferentiated spondyloarthritis; 84% of the subjects (153) did not have a family history of spondyloarthritis. Table 2 shows the clinical characteristics of the population.
Clinical manifestations in the population of patients with spondyloarthritis.
| Clinical manifestations | Percentage % (N) |
|---|---|
| Axial involvement | 67 (122) |
| Inflammatory low back pain | 70 (128) |
| Sacroiliitis | 57 (104) |
| Alternating buttock pain | 40 (73) |
| Morning stiffness | 71 (130) |
| Peripheral involvement | 69 (127) |
| Arthritis | 66 (121) |
| of swollen joints | 2 IQR 3 (1−2) |
| of painful joints | 3 IQR 2.5 (1−4) |
| Enthesitis | 45 (83) |
| Dactylitis | 24 (44) |
| Talalgia | 41 (76) |
| Hip involvement | 31 (57) |
| Uveitis | 11 (20) |
| Cutaneous psoriasis | 17 (31) |
| Nail psoriasis | 11 (21) |
| Diarrhea | 12 (22) |
| Crohn’s disease | 2.7 (5) |
| Idiopathic ulcerative colitis | 2.2 (4) |
IQR: interquartile range.
The median maximum value of the erythrocyte sedimentation rate (ESR) was 21 mm/h, IQR 40 (2–75). 43.4% (79) of the patients had a normal ESR (up to 20 mm/h), 26.4% (48) between 21 and 49, and 30.2% (55) of 50 (74) mm/h, or higher. CRP was found to be elevated in 40.7% (74) of the cases (normal value1 mg/dL) and the median maximum value during the evolution was 1.7 mg/dL, IQR 5 (0.5–24).
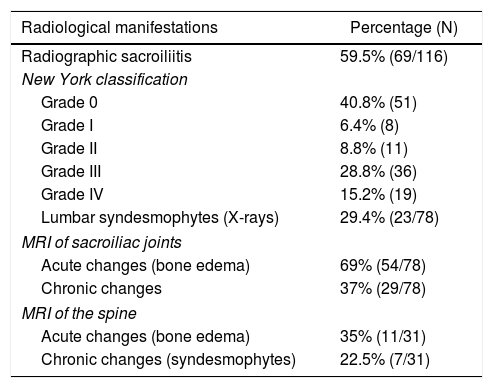
8.8% (16) of the patients had a CRP of 5 mg/dL or lower, 4.9% (9) between 5.1 and 10 mg/dL and 86.3% (157) higher than 10 mg/dL. HLA-B27 was positive in 55.6% (59/106) of the patients. Table 3 describes the radiological manifestations of the studied population, while Table 4 shows the clinical characteristics in the different types of SpAs.
Radiological manifestations in 181 patients with spondyloarthritis.
| Radiological manifestations | Percentage (N) |
|---|---|
| Radiographic sacroiliitis | 59.5% (69/116) |
| New York classification | |
| Grade 0 | 40.8% (51) |
| Grade I | 6.4% (8) |
| Grade II | 8.8% (11) |
| Grade III | 28.8% (36) |
| Grade IV | 15.2% (19) |
| Lumbar syndesmophytes (X-rays) | 29.4% (23/78) |
| MRI of sacroiliac joints | |
| Acute changes (bone edema) | 69% (54/78) |
| Chronic changes | 37% (29/78) |
| MRI of the spine | |
| Acute changes (bone edema) | 35% (11/31) |
| Chronic changes (syndesmophytes) | 22.5% (7/31) |
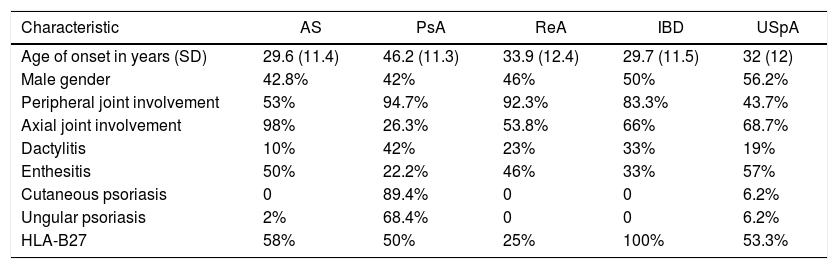
Clinical characteristics of the different forms of spondyloarthritis.
| Characteristic | AS | PsA | ReA | IBD | USpA |
|---|---|---|---|---|---|
| Age of onset in years (SD) | 29.6 (11.4) | 46.2 (11.3) | 33.9 (12.4) | 29.7 (11.5) | 32 (12) |
| Male gender | 42.8% | 42% | 46% | 50% | 56.2% |
| Peripheral joint involvement | 53% | 94.7% | 92.3% | 83.3% | 43.7% |
| Axial joint involvement | 98% | 26.3% | 53.8% | 66% | 68.7% |
| Dactylitis | 10% | 42% | 23% | 33% | 19% |
| Enthesitis | 50% | 22.2% | 46% | 33% | 57% |
| Cutaneous psoriasis | 0 | 89.4% | 0 | 0 | 6.2% |
| Ungular psoriasis | 2% | 68.4% | 0 | 0 | 6.2% |
| HLA-B27 | 58% | 50% | 25% | 100% | 53.3% |
PsA: psoriatic arthritis; SD: standard deviation; AS: ankylosing spondylitis; IBD: inflammatory bowel disease; ReA: reactive arthritis; USpA: undifferentiated spondyloarthritis.
The population was characterized by having high activity both upon entry to the cohort and during the follow-up. The initial Basdai score was of 4 IQR 3 (0–8) and 89% of the patients had a score of 4 or more. During follow-up the average Basdai score was 3.3 SD 1.9 (0–8).
91.1% of the patients (164/181) were treated with NSAIDs, 60.1% (107/178) with sulfasalazine, 43.4% (76/175) with selective cyclo-oxygenase-2 inhibitors NSAIDs, 33.7% (59/175) with methotrexate and 20–45% (36/176) with steroids. The use of TNF-i was required in 56% of the cases (101/181). The most widely used biological drug was adalimumab, in 31.1% of the cases (56), followed by etanercept, in 21.7% (39), and infliximab, in 13.9% (25). 30.8% (31) of the patients required more than one TNF-i.
DiscussionSpAs are characterized by a broad clinical and immunogenetic spectrum that varies according to the study population. The present cohort includes 181 patients from Northwestern Colombia. A description of 2 cohorts had been made previously in Colombia, one at the Bogota Military Hospital, with 139 patients, and the other of the HPTU, with 71 patients.14,15
There was a predominance of men in the population, and in 124 patients the onset of symptoms was before the age of 40, a finding consistent with what is described in the literature, affecting mainly young people in the productive stage. The mean age at diagnosis was 45.3, SD = 13.39 years, higher than the age of onset of the symptoms, which represents an average delay in the diagnosis of 6 years, as has been described in the different cohorts studied worldwide.20–22 Possibly, the delay in the diagnosis is associated with multiple factors such as the sensitivity of primary care physicians in detecting patients with inflammatory low back pain, socioeconomic conditions, and access to health systems in each population23,24. Various aspects can explain the delay or the difficulty in making a timely diagnosis: in our environment, the lack of knowledge of the disease, even by health personnel or non-rheumatologist physicians, the shortage of rheumatologists nationwide, the difficulties for patients to obtain a timely specialized consultation in rheumatology through their health provider, the difficulty in accessing imaging studies such as magnetic resonance imaging or immunogenetic such as HLA-B27, due to the cost or lack of availability. Even, more than 60% of our consultation in the HPTU corresponds to patients that attend private consultation, seeking a second option in the face of the diagnostic and therapeutic uncertainty. If the migration of the patients by the different health provider institutions is added to all the above, due to the hiring up and downs, the follow-up of this group of diseases in Colombia becomes more difficult.
Ankylosing spondylitis was the most frequent, followed by undifferentiated spondyloarthritis and psoriatic spondyloarthritis. Inflammatory low back pain, morning stiffness, enthesitis and dactylitis were the most frequent clinical manifestations, just as we had described it in 2010.15
In the analysis by groups, ankylosing spondylitis begins earlier, between the second and third decades of life, unlike psoriatic arthritis that classically begins after 40 years of age. Dactylitis was more frequent in the group with psoriatic arthritis, while enthesitis was more prevalent in those with undifferentiated spondyloarthritis and ankylosing spondylitis (see Table 4).
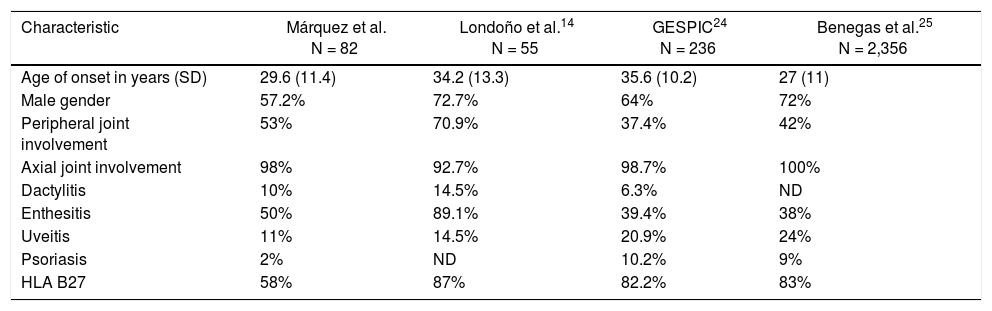
In the group of patients with ankylosing spondylitis, peripheral involvement was frequent, arthritis was present in 53%, followed by enthesitis (50%) and dactylitis (10%), similar to the other Colombian series by Londoño et al.14 This situation differs from the European cohorts such as Gespic24 and the binational Regisponser/Aspect et al.,25 in which the peripheral manifestations were fewer. In this group, the difference in frequency between men and women was 1.3/1, in contrast to the Londoño et al.14, Gespic26 and Regisponser/Aspect25 cohorts which showed a higher frequency of presentation in men, with a man/woman ratio between 1.8 and 2.7/1.
The most frequent extra-articular manifestation in patients with ankylosing spondylitis was uveitis, which occurred in 11% of the population, a lower percentage compared with the Gespic cohort which was 20.9%.23 A possible explanation for this difference is the relationship between uveitis and HLA-B27 and its higher prevalence in the European population.
In general, the behavior of SpA differs between European and Latin American countries; in the latter, peripheral involvement predominates and patients present more enthesitis; NSAIDs, steroids and disease-modifying drugs are more frequently used, while the patients in Europe have a higher frequency of positive HLA-B27, which may also explain the greatest axial involvement.25,26
The differences between the group of patients with ankylosing spondylitis included in this series, together with the other Latin American cohort of Londoño et al.14 and the European Gespic26 and Regisponser/Aspect25 are summarized in Table 5.
Comparison of the Latin American and European AS series.
| Characteristic | Márquez et al. N = 82 | Londoño et al.14 N = 55 | GESPIC24 N = 236 | Benegas et al.25 N = 2,356 |
|---|---|---|---|---|
| Age of onset in years (SD) | 29.6 (11.4) | 34.2 (13.3) | 35.6 (10.2) | 27 (11) |
| Male gender | 57.2% | 72.7% | 64% | 72% |
| Peripheral joint involvement | 53% | 70.9% | 37.4% | 42% |
| Axial joint involvement | 98% | 92.7% | 98.7% | 100% |
| Dactylitis | 10% | 14.5% | 6.3% | ND |
| Enthesitis | 50% | 89.1% | 39.4% | 38% |
| Uveitis | 11% | 14.5% | 20.9% | 24% |
| Psoriasis | 2% | ND | 10.2% | 9% |
| HLA B27 | 58% | 87% | 82.2% | 83% |
SD: standard deviation; AS: ankylosing spondylitis; NA: not available.
In the population, peripheral arthritis was present in 53% of the patients, greater than that was described in the German Gespic and the Spanish Regisponser cohorts, in which it ws observed approximately in 37–42% of the subjects studied.
Like in the other studies in which Colombian patients are described, HLA-B27 is present in 50–60% of the cases, which differs from the European cohorts in which the prevalence is higher than 80%.18
Regarding acute phase reactants, CRP and ESR were elevated in approximately 40% of the cases, and 60% of the patients had radiographic sacroiliitis. This finding is important given that the elevation of the CRP has been associated with structural damage and radiographic progression.14
The population was characterized by having high activity, both upon the entry to the cohort and during the follow-up, similar to that was described in the patients of Regisponser, who had high Basdai and Basfi indices,10 which can explain that 56% of the cases of our population requires the use of TNF-i.
The weaknesses of the study are those inherent to descriptive observational studies, such as the information bias determined by aspects such as incomplete information and irregular follow-up, while the main strength is the inclusion of all subjects with ASp, which allows us to generalize the findings to the population of origin.
ConclusionsA slight predominance of men was observed in the cohort, ankylosing spondylitis was the most frequent disease, axial and peripheral manifestations had a similar frequency, although inflammatory back pain and morning stiffness were the most frequent. The population was characterized by high activity and functional compromise, demonstrated by the high Basdai and Basfi scores and because 56% of the patients required TNF-i agents.
Conflict of interestAll the authors of this manuscript declare that we have no conflict of interest.
We thank all the patients who participate in this cohort and the Hospital Pablo Tobón Uribe.
Please cite this article as: Márquez-Hernández JD, Echeverri-García AF, Restrepo-Escobar M, Álvarez Barreneche MF, Hurtado A, Pinto-Peñaranda LF. Espondiloartritis: caracterización de la cohorte del Hospital Pablo Tobón Uribe, Medellín, Colombia. Rev Colomb Reumatol. 2022;29:31–37.