Psoriasis is a common cutaneous disease with a world prevalence of 0.9–8.5%. It is a chronic, inflammatory, immune mediated condition that leads to epidermal hyperplasia and an array of clinical presentations. Psoriasis ostracea is a rare hyperkeratotic variant of psoriasis. Although frequently associated with psoriatic arthritis, there are few reports in the literature. Psoriatic arthritis is a chronic, seronegative, inflammatory arthritic disease, in which the symptoms usually emerge years after skin lesions appear. The case is presented of a patient, who after 10-years of adequate infliximab treatment, had an unusual presentation of psoriatic arthritis associated with psoriasis ostracea.
La psoriasis es una enfermedad cutánea común, con prevalencia mundial entre el 0,9-8,5%. Es una condición inflamatoria crónica, inmunológicamente mediada, que lleva a hiperplasia epidérmica con gran variedad de formas clínicas. La psoriasis ostrácea es una variante hiperqueratósica infrecuente, reportada pocas veces en la literatura y que con frecuencia se asocia a artritis psoriásica, una artropatía inflamatoria, seronegativa, crónica, cuyos síntomas usualmente comienzan después de las lesiones cutáneas. Este es el caso de un paciente con una presentación inusual de artritis psoriásica asociada a psoriasis ostrácea posterior a 10 años de manejo adecuado con infliximab.
Psoriasis is a common cutaneous disease, it is estimated that its worldwide prevalence ranges between 0.9 and 8.5%.1 It is a chronic inflammatory, immune mediated condition that leads to epidermal hyperplasia with a wide variety of clinical forms, being plaque psoriasis the most frequent.2,3 Psoriatic arthritis is an inflammatory chronic seronegative arthropathy, with a world prevalence of 0.16–0.25%.2 It occurs in 20–30% of patients with psoriasis and the symptoms usually begin after the skin lesions.2 Psoriasis ostracea is an infrequent variant of psoriasis which has been reported very few times in the literature. This is the case of a patient with an unusual presentation of psoriatic arthritis associated with psoriasis ostracea, after 10 years of management with infliximab.
Clinical caseA 35-year-old male patient hospitalized due to bleeding of the lower digestive tract, secondary to cholestatic jaundice due to ascaris. During the hospitalization, the patient was assessed by the dermatology service due to a clinical picture of 8 months of evolution of generalized asymptomatic skin lesions. On the interrogation, the patient reported low back pain of 8 years of evolution, predominantly in the morning, which over the years had spread to the knees and ankles, with preference for the left side, associated with edema, and to the cervical region and metatarsophalanges. The pain was disabling, and for this reason he had been in bed for 7 months and managed it with nonsteroidal anti-inflammatory drugs without improvement. His joint pains had been previously studied (negative rheumatoid factor in 4.6IU/mL [NL<15IU/mL], C3 in 232mg/dL [NL 88–252], normal C4 in 13.3mg/dL [12–72], ANA 1/40 with fine speckled pattern, HLA-B27 was not taken) and had been managed as rheumatoid arthritis with prednisolone and chloroquine without improvement of the clinical picture. In addition, the patient had 2 previous hospitalizations, 6 years earlier, due to acute diarrheal disease managed as intestinal amebiasis.
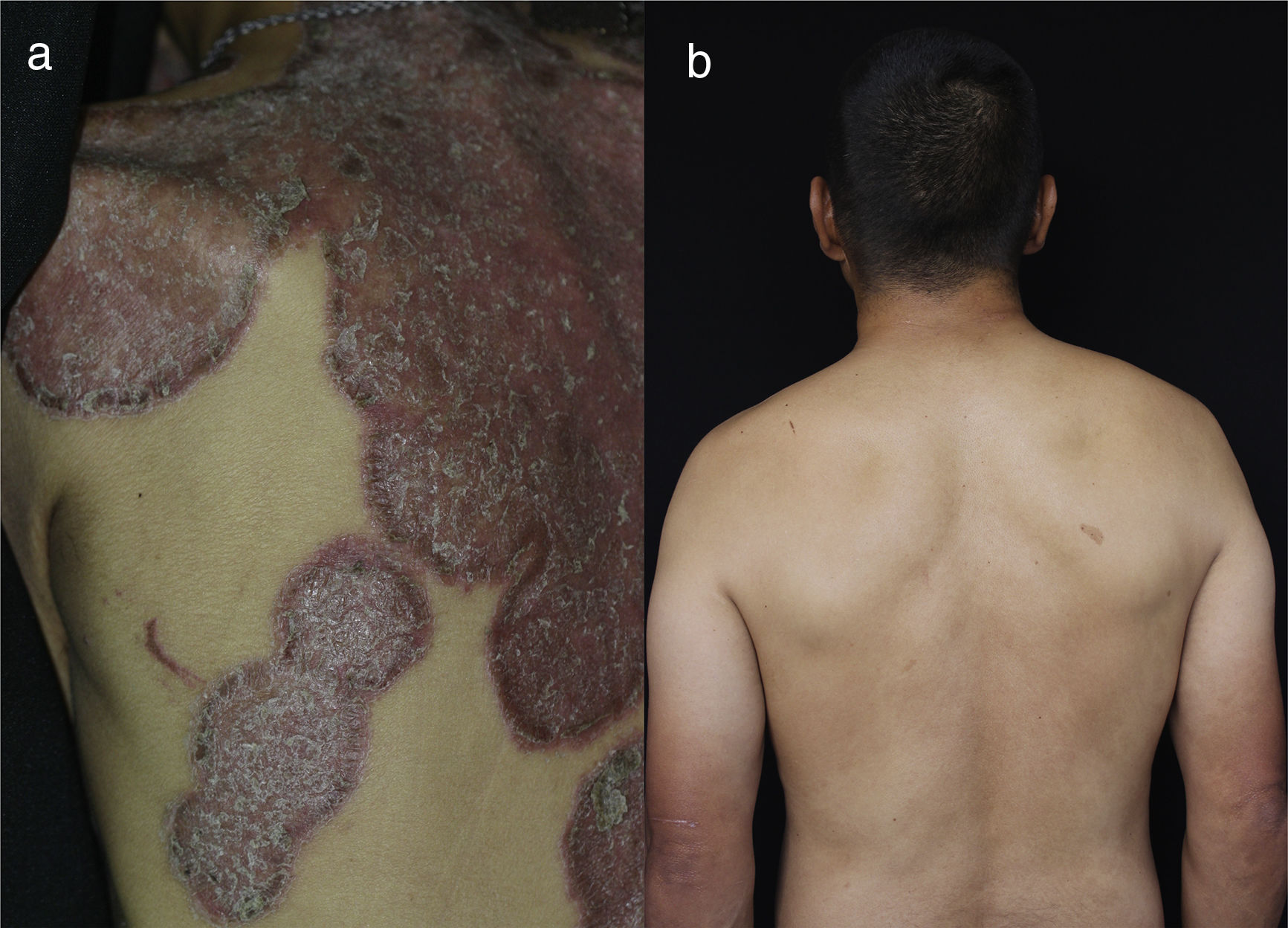
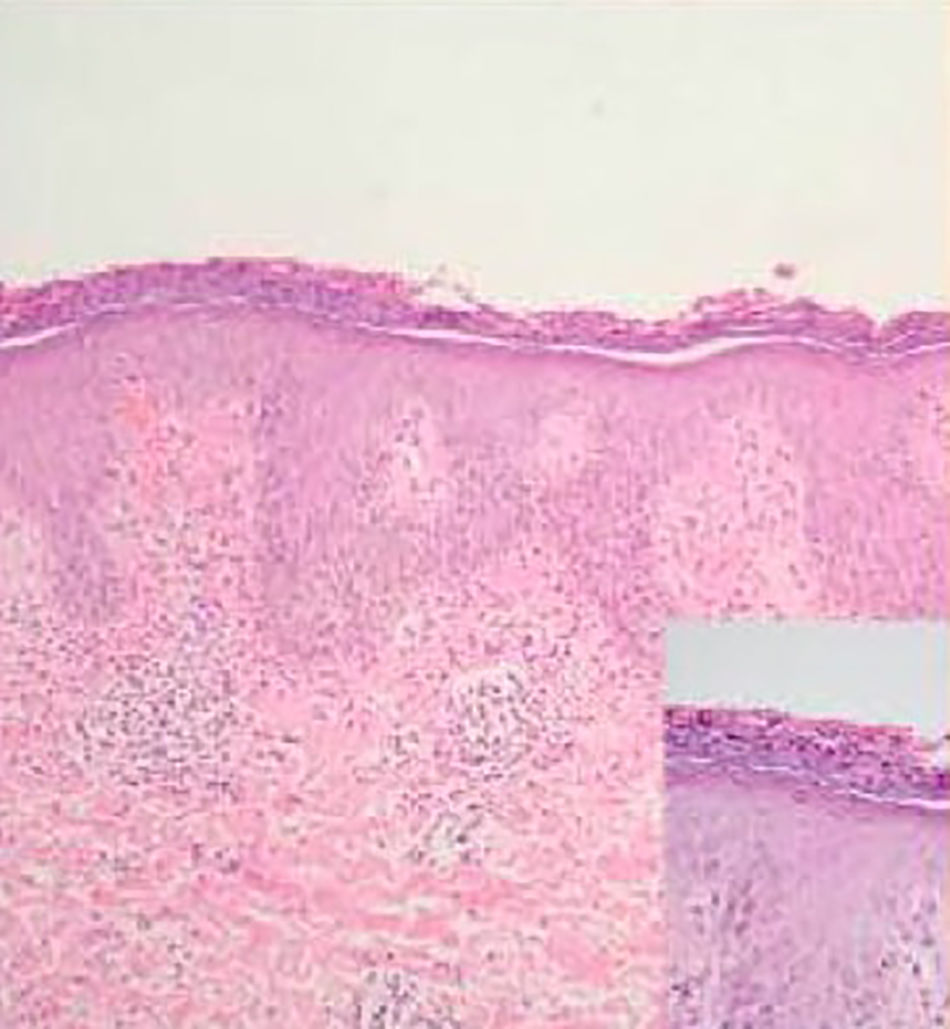
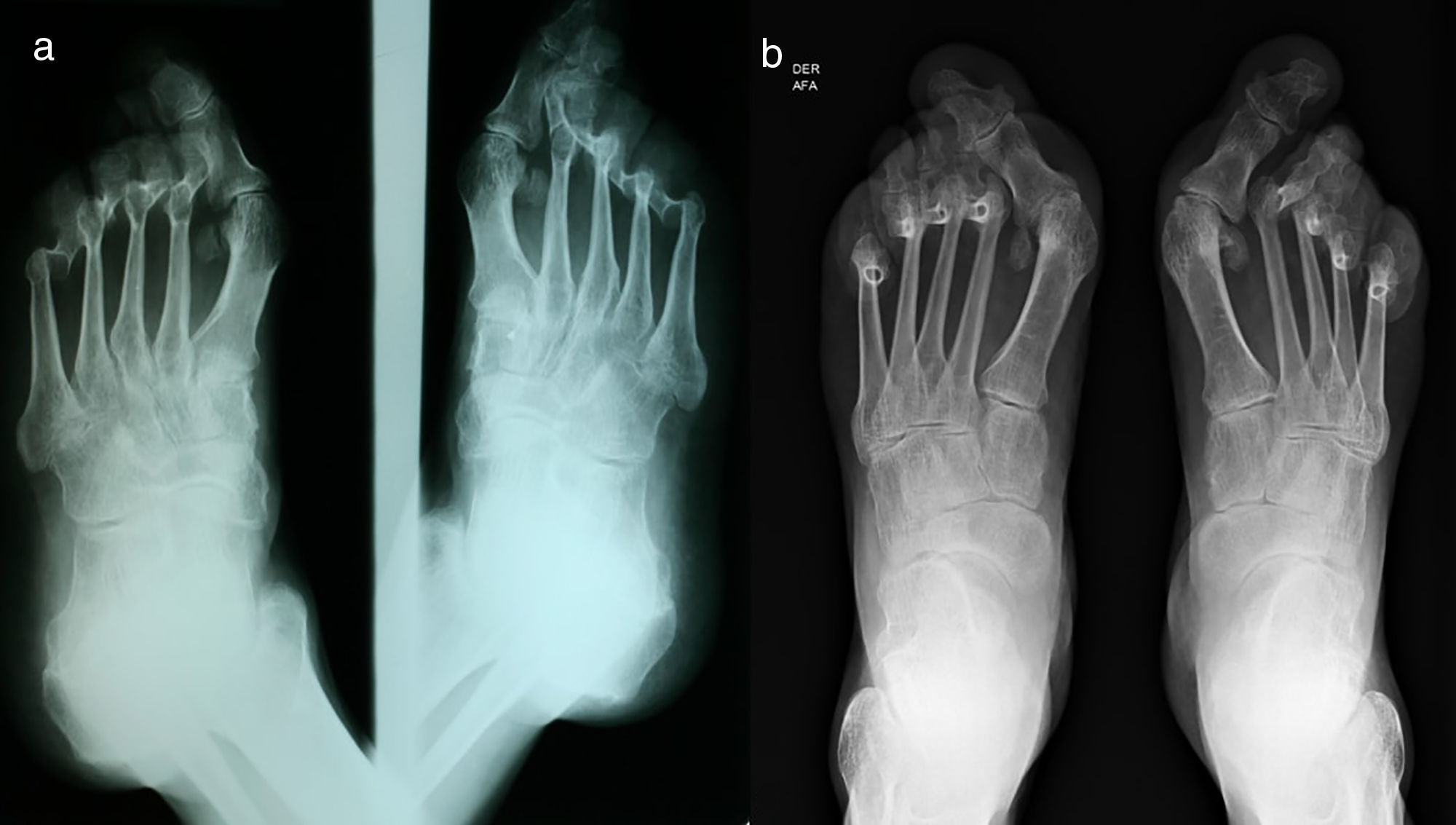
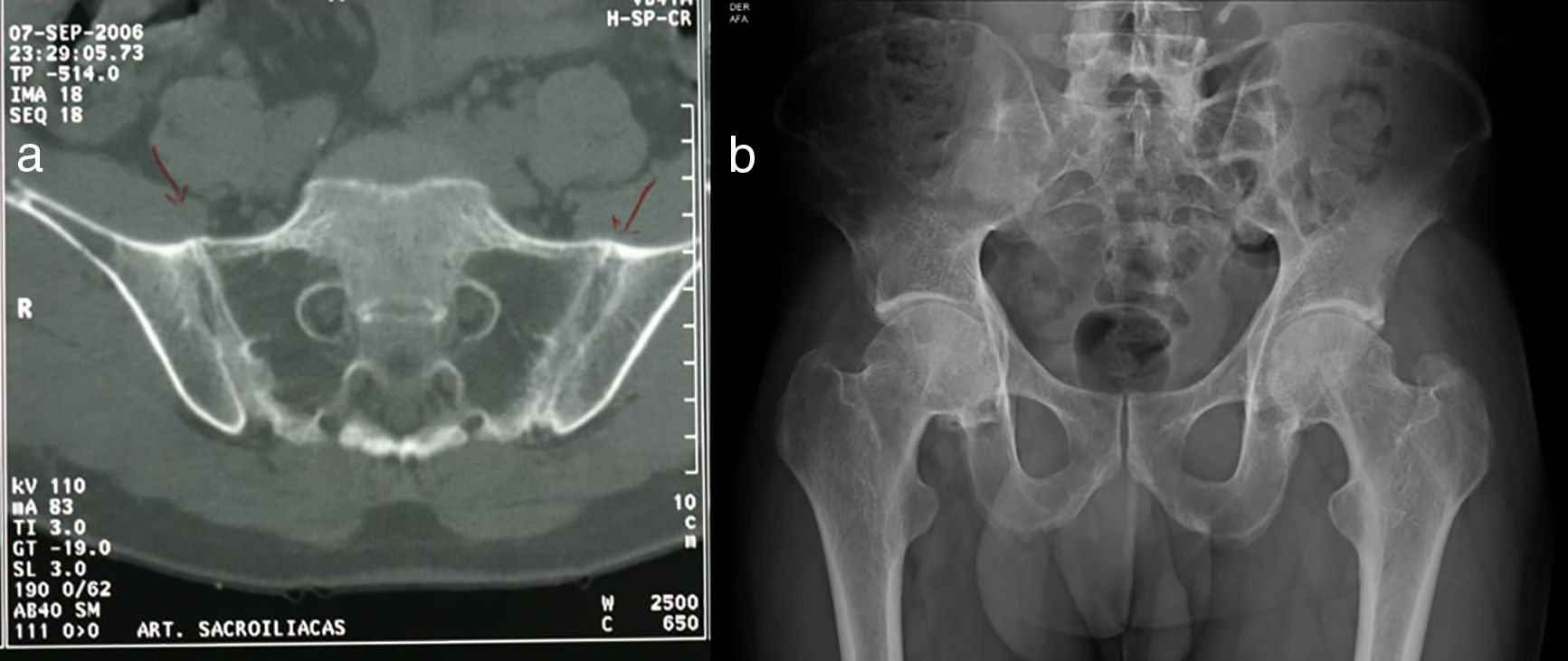
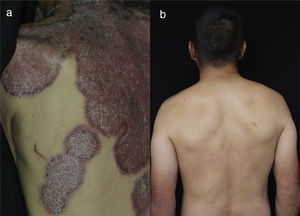
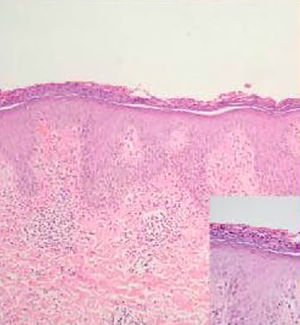
The physical examination showed circumscribed erythematous plaques, with raised edges and thick desquamation which compromised the entire body surface (Figs. 1a and 2a). On the scalp there were plaques with adherent desquamation, type false tinea amiantacea, extending beyond the anterior hair implantation edge. On some nails there was onycholysis, subungual hyperkeratosis and oil drop sign (Fig. 3a). A skin biopsy was performed which showed parakeratosis and intracorneal pustules (Fig. 4), findings compatible with psoriasis. A PASI (psoriasis area and severity index) of 48 was calculated. With these new findings, imaging studies were performed, finding in the radiography of the hands diffuse osteopenia of the right carpal bones with narrowing of the proximal interphalangeal joint spaces of the 5th finger bilaterally and of the 3rd finger of the right hand with minimal soft tissue edema, in the cervical spine X-ray there was fusion of the facet joints C7 to T1 and, in the feet, metacarpophalangeal subluxation of all fingers and valgus deformity (Fig. 5a). The computerized axial tomography of the sacroiliac joints showed fusion of the lower 2/3 and sclerosis of the upper 1/3 (Fig. 6a).
(a) Comparative foot X-ray, oblique projections: generalized diffuse osteopenia, degenerative changes of the metatarsophalangeal joints of all the toes with subluxation associated with valgus deformity, left calcaneal spur, mild degenerative changes of the joints of the forefoot with the midfoot. (b) Comparative foot X-ray, anteroposterior projections: generalized diffuse osteopenia, the changes described in the previous radiograph persist with progression thereof.
(a) CT scan of sacroiliac joints, axial section: fusion of the sacroiliac joints in the lower 2/3 due to bilateral ankylosis and bilateral sclerosis of the upper 1/3. (b) Hip X-ray, anteroposterior projection: complete fusion of sacroiliac joints, the coxofemoral joint relationships and in the pubic symphysis are preserved, decreased bone density.
The patient was evaluated by rheumatology ruling out rheumatoid arthritis and considering that he might have a psoriatic arthritis with mixed component: sacroiliitis and symmetric polyarthritis, due to the presence of early commitment of sacroiliac joints for the first one and subsequently cervical involvement, as well as of the hands, knees and feet for the second. VDRL, ELISA for HIV, antibodies against hepatitis B, and ANA were performed which were negative, and liver and renal profile which were normal, albumin/globulin ratio of 0.4 compatible with malnutrition. With the above, management with methotrexate (MTX) 15mg/week was started. Three months later, in an outpatient control, a slight improvement was observed, and therefore the dose of MTX was increased to 20mg/week. A month later, the patient was considered a candidate for management with a biological agent given the persistence of the joint symptomatology and the skin lesions. A PPD test was requested, which was negative (0) and treatment with infliximab 200mg/week 0, 2, 6 and then every 8 weeks together with MTX 15mg/week was started. Two months later it was evident an improvement of the skin lesions, reduction of joint pain and great improvement of the range of motion of the joints, allowing the patient to walk again. One year later there was a reactivation of the cutaneous disease, so the dose of infliximab was increased to 300mg/8 weeks and the dose of MTX was reduced to 12.5mg/week. Since then the doses of MTX had been progressively decreased until reaching 7.5mg/week. 10 years have passed and the patient has a stable clinical picture, including a PASI of 0 (Figs. 1b, 2b, 3b) and almost total recovery of his movements, being able to be self-sufficient in his daily life and needing only a walking stick since the bone damage presented was not reversed with the treatment (Fig. 5b and 6b). The above, despite the fact that the current conditions of the healthcare system to which the patient is affiliated do not allow the timely application of the medication.
(a) In the left foot we can observe the nail of the thumb with subungual hyperkeratosis associated with onycholysis and yelowish chromonychia. In the nail of the third toe an oil drop spot is observed. Valgus deformity in the first and second toes. (b) 10 years later there is evidence of persistence of valgus deformity in the first toes of both feet, and also in the second toe of the left foot. Remarkable decrease in subungual hyperkeratosis, onycholysis and yellowish chromonychia is evident. Oil drop spots are no longer seen.
Psoriasis is an inflammatory, polygenic, immune-mediated cutaneous disease, which can be influenced by environmental factors and, therefore, has a course of remissions and relapses.4,5 It is considered to have a great negative impact on the quality of life of patients as there are often periods of exacerbation, and although there are effective treatments, these must be maintained for long periods.3,4 It is typically characterized by erythematous, desquamative plaques, with silvery scales very well defined and in occasions itchy.4 It is traditionally classified according to the different morphological types of the lesions that include plaque, guttate, inverse, erythrodermic and pustular psoriasis.3,4 There are 5 rare hyperkeratotic clinical variants known as psoriasis elephantine, pseudocorneal, ostracea, rupioid, and with minimal differences between them.6 The patient exhibits a typical picture of psoriasis ostracea.
Hyperkeratotic psoriasis is a morphological subtype of plaque psoriasis.7 Its name is derived from the Greek word rhupos which means dirt.7,8 The term has been used to describe thick, hyperkeratotic, well-delimited plaques with dark scabs, adherent on the surface, arranged as lamellae that give the appearance of a sea oyster.7,8 In rupioid psoriasis, plaques with scales in concentric circular layers are observed, one over the other, forming a conical shape.8,9 Psoriasis ostracea is very similar because it is characterized by plaques with desquamative layers of various colors, with a characteristically concave surface, with raised edges as are evident in our patient. The patients with hyperkeratotic psoriasis are usually men with a greater body surface area compromised and a higher incidence of nail involvement and psoriatic arthritis, compared with patients with common plaque psoriasis (Table 1).7 The patient exhibits the 3 characteristics associated with hyperkeratotic psoriasis.
Comparison between plaque psoriasis and psoriasis ostracea.
| Characteristic | Plaque psoriasis | Psoriasis ostracea |
|---|---|---|
| Frequency | The most common type | Very rare |
| Morphology | ||
| Main lesion | Plaque | Plaque |
| Color | Erythematous | Erythematous |
| Scale | Silvery | Dark, dirty appearance, adherent |
| Elevation | Flat | Concave with raised edges |
| Shape | Circular, oval, polycyclic | Circular, oval, polycyclic |
| Edges | Well defined | Well defined |
| Ungual involvement | +++ | ++++ |
| Scalp involvement | ++++ | ++++ |
| Associated psoriatic arthritis | + | +++ |
| Histologya | ||
| Epidermis | Acanthotic epidermis with psoriasiform pattern, parakeratosis, agranulocytosis, micropustules of Kogoj, Munro's microabscesses | |
| Dermis | Edema in the tips of dermal papillae, tortuous capillaries that ascend to dermal papillae, mixed perivascular infiltrate | |
Psoriatic arthritis is an inflammatory, seronegative, chronic arthropathy, which corresponds to the group of spondyloatropathies.2,10 It is characterized by the presence of synovial hyperplasia secondary to immune infiltrate both in the skin and the synovial membrane.2 This results in stiffness of morning predominance, pain and edema that includes the tissues that constitute the joints (dactylitis and enthesitis).10 The patients report pain and edema that causes restriction to perform daily tasks, so it also generates a big negative impact on the quality of life.2,10 In the case of the patient, the pain and restriction of movement were so severe that he was confined to bed, which led him to malnutrition. In addition, he had an Achilles tendon enthesitis, which is considered the most typical enthesitis of psoriatic arthritis.
There are 5 patterns of clinical presentation of psoriatic arthritis: (1) asymmetric oligoarthritis, (2) symmetric polyarthritis, (3) predominant compromise of distal interphalangeal joints, (4) spondyloarthritis or sacroiliitis and (5) mutilating arthritis.11 The pattern of joint involvement is not fixed, as is the case of this patient who presents axial involvement associated with symmetrical involvement of small and medium joints. Joint involvement usually appears after cutaneous involvement; in a study conducted by Gottlieb et al., 84% of patients had cutaneous involvement for 12 years prior the onset of joint symptoms.10 Only 15% of patients have joint commitment as an initial manifestation, as in the case of our patient, who had joint commitment 8 years before the skin involvement, making this an unusual presentation.
The objective of treatment both in psoriasis and psoriatic arthritis is to block the inflammatory cascade. In psoriasis the treatment is chosen according to the degree of skin involvement and the quality of life of the patient.10 The PASI is a tool that measures the severity according to the compromised body surface area, the erythema, the degree of infiltration and the quality of the scales.10 It is used more in clinical studies than in practice, but in general terms a PASI<10 is managed with topical treatments and a PASI>10 with systemic treatments.10,12 For the management of psoriatic arthritis, the European League Against Rheumatism (EULAR) recommends starting with MTX.2,11 If after 3 months the patient does not show improvement, a disease-modifying drug is added unless the patient has an axial compromise in which case a biological drug is added.2,11 In general, both in psoriasis and in psoriatic arthritis, treatment with biological medications is reserved for when an adequate clinical response to first-line systemic treatments has not been obtained.4,10–12
In the case exposed, the management of the patient started with MTX, the first-line systemic treatment for both diseases. Given that at 3 months there was no improvement, the dose of MTX was increased while laboratory tests were performed in order to start biological therapy. Once suitability for biological therapy was confirmed, infliximab was initiated. Infliximab is a humanized anti-TNF chimeric monoclonal antibody approved for use in psoriasis and psoriatic arthritis.2,12 The time of onset of action is 1–2 weeks, shorter than for other biological drugs approved for these same indications.12 Furthermore, according to a recent meta-analysis conducted by Puig et al., infliximab is the second most effective biological agent for the treatment of moderate to severe psoriasis.13
The management with biological treatments presents 3 problems, first, the risk of infections, second, that occasionally some patients have cutaneous reactions and third, the possibility of generating resistance to the treatment, usually secondary to the formation of antibodies against the drug.2,12,14 Some cutaneous reactions secondary to the use of anti-TNF described are: eczema, vasculitis, drug-induced lupus, neutrophilic dermatosis, interface dermatitis and psoriasis.14,15 Psoriasiform reactions secondary to the use of anti-TNF usually occur with small, erythematous plaques with small silvery scales, corresponding to plaque psoriasis; or alternatively as pustular psoriasis with palmoplantar involvement.14,15 It is believed that anti-TNFs can have a paradoxical reaction when they are used for the treatment of diseases such as rheumatoid arthritis or inflammatory bowel disease, since they generate an imbalance between TNF-α and interferon-α.16,17 Seemingly, the decrease in the action of TNF-α produces an overexpression of interferon-α that can trigger or aggravate the psoriasis.16,17 To consider a psoriasiform reaction as secondary to the use of anti-TNF there must be a temporary relationship with exposure, that is, the medication must first be applied and then the reaction appears. In the case exposed it is not a psoriasis secondary to the use of anti-TNF, first, because the patient presented a rare hyperkeratotic variant of psoriasis, and second, because the anti-TNF was started for the management of this disease and the psoriatic arthritis, so there is no temporary relationship. Finally, with respect to the generation of resistance to biological treatment, it is established that, although there are no clinical studies that corroborate it, the use of MTX concomitant with anti-TNF appears to reduce the risk of developing antibodies against anti-TNF and improves its effectiveness.2 This patient is a clear example, since he has been treated with infliximab and MTX for 10 years, obtaining an adequate response both of joint and cutaneous involvement, which indicates that resistance has not been generated.
ConclusionsThis patient is presented as an illustrative case of adequate treatment for a rare presentation of psoriasis, such as psoriasis ostracea, together with the unusual presentation of psoriatic arthritis. The patient has received prolonged treatment with infliximab without the presence of resistance to the treatment or antibodies against it.
Conflict of interestNo conflicts of interest are reported.
Please cite this article as: Cabrera-Salom C, Beltrán AM, Medina Y. Presentación inusual de psoriasis ostrácea y artritis psoriásica: resultados después de 10 años de manejo con infliximab. Rev Colomb Reumatol. 2019;26:194–200.