The different bony and soft tissue reference points and the micro and macroscopic structures of the knee continue to be the object of focused study and analysis. Upon reviewing the most recent literature, we saw the wide spectrum of studies that seek to define the different anatomical aspects of the anterior cruciate ligament (ACL).
PurposeThe purpose of this paper is to review the most recent publications on the ACL and its morphology in which its microscopic composition and macroscopic anatomy are addressed.
ResultsThe ACL consists of type I (90%) and type III (10%) collagen matrix. Its length ranges from 27 to 38mm and its width from 10 to 12mm. The ACL cross-section area measures an average of 44mm2, and its shape resembles that of an hourglass or a bow tie. ACL bundles have been defined as anteromedial, intermediate, and posterolateral. Femoral and tibial footprints were seen to present a high degree of variability in shape and size. Furthermore, the blood supply is given by the medial genicular artery and innervation by the tibial nerve branches. Additionally, the ACL functionally prevents anterior translation of the tibia and stabilizes against the internal rotation of the tibia and valgus angulation of the knee.
ConclusionsThere is great variability in the anatomy of the ACL as well as its attachment sites. At the same time, the shape and size of its footprint has become a factor in determining individualized ACL reconstruction. The persistence of morphological variability in the aging of the ACL and important aspects of surgical planning and decision making with respect to anatomical risk factors suggest that further studies are called for.
Los diferentes puntos de referencia óseos y de tejidos blandos y las estructuras micro y macroscópicas de la rodilla siguen siendo objeto de estudio y análisis. Al revisar la literatura más reciente observamos el amplio espectro de estudios que buscan definir los diferentes aspectos anatómicos del ligamento anterior cruzado (LAC).
ObjetivoEl objetivo de este trabajo es revisar las publicaciones más recientes sobre el LAC y su morfología en las que se aborda su composición microscópica y su anatomía macroscópica.
ResultadosEl LAC está formado por matriz colágena tipoI (90%) y tipoIII (10%). Su longitud oscila entre 27 y 38mm y su anchura, entre 10 y 12mm. El área de sección transversal del LAC mide una media de 44mm2 y su forma se asemeja a la de un reloj de arena o una pajarita. Los haces del LAC se han definido como anteromedial, intermedio y posterolateral. Se ha observado que las huellas femoral y tibial presentan un alto grado de variabilidad en cuanto a forma y tamaño. Además, el riego sanguíneo viene dado por la arteria genicular medial, y la inervación, por las ramas del nervio tibial. Además, el LAC impide funcionalmente la traslación anterior de la tibia y estabiliza frente a la rotación interna de la tibia y la angulación en valgo de la rodilla.
ConclusionesExiste una gran variabilidad en la anatomía del LAC, así como en sus lugares de fijación. Al mismo tiempo, la forma y el tamaño de su huella se han convertido en un factor determinante a la hora de individualizar la reconstrucción del LAC. La persistencia de la variabilidad morfológica en el envejecimiento del LAC y los aspectos importantes de la planificación quirúrgica y la toma de decisiones con respecto a los factores de riesgo anatómicos sugieren la necesidad de realizar más estudios.
The earliest known descriptions of ligamentous structures and soft tissues of the knee are found in Egyptian papyrus scrolls from around 3000 BC. Further on in the Roman era, Claudius Galen (199–129 BC) used the term “ligamenta genucruciate” for what we now denominate as the anterior cruciate ligament (ACL).1 Historically, anatomists have continuously been coming up with morphological and biomechanical descriptions. In 1836, Wilhelm and Eduard Weber2 published an article on the anatomy and physiology of the lower extremity. Nearly a century later, in 1921, Testut and Jacob described the flat midsubstance of the ACL and its relationship to the anterior horn of the lateral meniscus and the tibial ACL insertion. In the latter case, emphasis was placed on the relationship of knee structures normal physiology and the functional complications of this joint after injury.3
Nowadays, the different bony and soft tissue reference points and the micro and macroscopic structures of the articular elements of the knee continue to be described and analyzed. This is reflected in the fact that more than 2700 articles on ACL anatomy and around 14,900 articles covering different ACL related topics have been published over the last ten years. The complexity of its biomechanics in healthy individuals, after an injury or following surgical treatment have also been extensively studied over the decades. Moreover, the possible risk factors due to anatomical predisposition in some groups of individuals along with the resulting modifications in the techniques of reconstruction following an ACL injury have also been looked into.4
The purpose of this work was to review the most recent publications, from over the last 5 years, on the ACL and its morphology. The focus was on looking at its microscopic composition and macroscopic anatomy, its femoral and tibial insertion points, the most relevant bone reference points, the biomechanics as well as the blood supply, and innervation of this anatomical structure.
While reviewing the most recent literature, we were able to see the wide spectrum of ongoing studies that seek to define each of the anatomical features of the ACL, its differences in specific populations and the growing consensualization of the terminology and features specific to the ACL. They include the structure, shape and location of femoral and tibial insertion sites, the number of bundles and mid-substance characteristics, blood supply and innervation among the different anatomical variants of this ligament and their reported percentages.
General anatomical characteristicsAs a broad definition, the ACL has been described as a single structure connecting the tibial and femoral joint.5 It originates at the tibial plateau, anterior to and between the intercondylar eminences and continues posteriorly to attach to the posteromedial portion of the lateral femoral condyle.6,7
The ACL has its own synovial membrane but is still considered an intra-articular structure.6 Characterized by its singularity, the ACL is immanently subject to both anatomic and morphological variations as well as physiological aging.8,9
Microscopic anatomyRegarding it histology, the ACL consist of highly organized type I (90%) and type III (10%) collagen matrices, which account for approximately 75% of its dry weight. This collagen is organized into multiple bundles of fiber of 20lm that are made up of groups ranging from 20lm to 400lm in diameter. Other substances that make up the remaining one-fourth of the ACLs’ dry weight. Water makes up 60% of the net weight under physiological conditions.1
Ligament and tendon insertions into bone have a distinct structure consisting of collagen fibrils that abut with the fibrils in the bone.10 This insertion sites are divided into a 4-layered structure of mixed histology that is composed of chondrocyte-like cells integrated with typical-appearing tenocytes. These layers also include ligamentous, fibrocartilaginous, and mineralized fibrocartilage, as well as the subchondral bone plate.1
ACL bundlesAt first, the ACL was viewed as a single homogenous structure. In 1938, Ivar Palmer made the first description of the two-bundle ACL.11 However, this double bundle description was not well known for several decades.1 These two bundles are classically defined as the anteromedial (AM) and posterolateral (PL) bundles.5,6,10 They are often distinguished by a tissue sheath between the bundles and the disparate locations of their insertion sites.5 Both bundles are named according to their relative attachments on the tibia. Specifically, the medial and lateral intercondylar tubercles of the tibia have been described as the distal attachment sites for both ACL bundles.6
While the existence of the anteromedial and posterolateral bundles of the ACL is broadly accepted, recent research findings suggest that the ACL is a triple-bundle structure.4–6,10,12 In those studies, the bundles have usually been defined as anteromedial, intermediate, and posterolateral bundles. Previous research has found that up to 26% of knees have a single bundle12 whilst Mac Kay et al.23 results showed an intermediate bundle was found by means of magnetic resonance imaging (MRI) visualization in approximately 20% of 73 patients.5 However, several studies were unable (anatomically or histologically) to confirm the presence of a distinct intermediate bundle in human specimens.12
ACL lengthLength is one of the most commonly reported metrics of ACL morphology. Early studies of ACL length involved the use of radiographs, Kirschner wires, or a digitizer to collect measurements. Recently, MRI has emerged as the standard for its measurement.5,8
Anatomic studies of the ACL and its bundles have shown that the ACL length ranges from 27 to 38mm in length (a length that may vary depending on the position of the knee) and 10–12mm in width, whereas the anteromedial and posterolateral bundles range from 6 to 7mm and 5 to 6mm in width, respectively.1,6,8,13
Mid-substance morphologyIn 2012, the ACL Study Group described the ACL as a structure with a ‘ribbon-like’ appearance.4 The midsubstance of the ligament has a rounded or elliptical cross-section, with an oval isthmus and larger insertion areas. Thereby, the ACL has also been described as having the shape of an hourglass or a bow tie in studies conducted on the cadavers of elderly specimens.5 When flexed and viewed from the front, the ACL has a twisted appearance, and this twist untwines as the knee extends.4
Cross-sectional areas of the ligament vary over the length of the ACL, with a mid-substance cross-section measuring approximately 44mm2, whereas the origin and insertion sites of the ACL can be more than 3 times the size of this area.1 In several studies with combined male and female data, the average ACL cross-sectional area has ranged from 30 to 53mm2.5
Degenerative histopathological changes in the ACL bundles have been also described with aging in osteoarthritic knees, presenting a weaker and thinner ligament in those patients.8
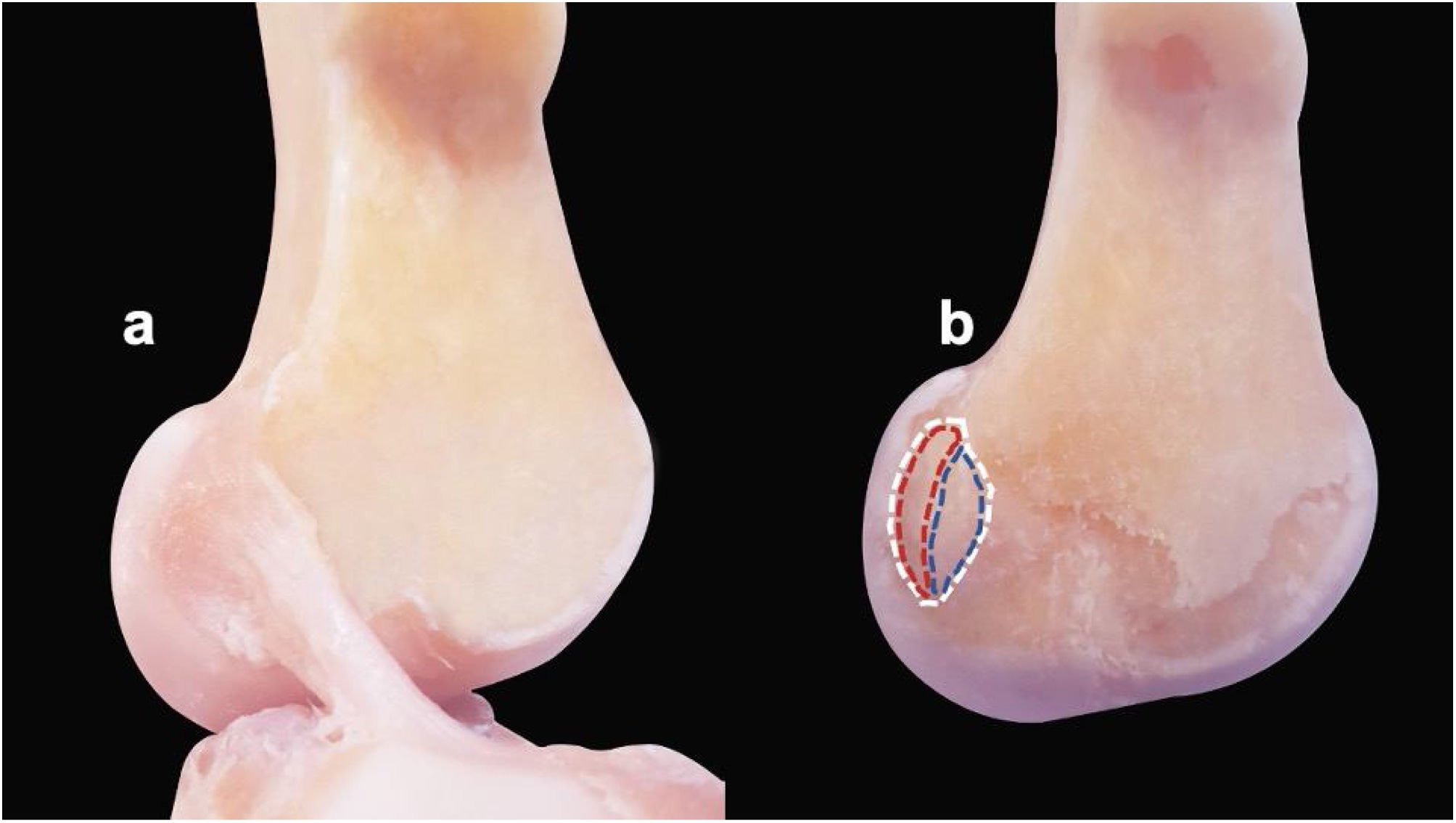
Femoral and tibial footprintsThere is great variation in the footprints of the ACL on the tibia and femur among individuals.8 On the femur, the lateral intercondylar ridge (also referred to as the resident's ridge) and the lateral bifurcate ridge (also referred to as the cruciate ridge) can be used to identify the precise attachment points for both bundles on the lateral femoral condyle. These attachment sites for the two bundles are separated by the lateral bifurcate ridge, which is located just posterior to the lateral intercondylar ridge6 (Fig. 1).
Femoral insertion sites of the ACL in the specimens before and after the ligament is cut. (a) ACL with an oval/elliptical morphology with its intact tibial and femoral attachments. (b) ACL removed showing the femoral footprint (white dashed line) with its anterior border formed by the lateral intercondylar ridge (resident's ridge) and posterior articular margin of the lateral femoral condyle forming its posterior border in continuity with the posterior femoral cortex. Dashed blue line marking direct insertion and red dashed line representing indirect fan-like insertion.
Systematic reviews including anatomical, cadaveric, and radiological studies independently helped to clarify the anatomy of the ACL femoral and tibial footprints.12
Femoral footprintThe central location of the femoral footprint is approximately 43% of the proximal-to-distal length of the lateral femoral condyle within the intercondylar notch.12 Studies of the femoral insertion site have shown that its cross-sectional area ranges in size from 60 to 130mm.8
The ACLs’ femoral footprint is crescent-shaped. Its anterior border is delineated by the lateral intercondylar ridge (resident's ridge). The posterior articular margin of the lateral femoral condyle delineates its posterior border in continuity with the posterior femoral cortex.4 Two types of insertions of the fibers of the ACL at their femoral attachment have been described. There is the ‘direct type’ that consists of dense mid substance fibers that are attached to a narrow oval area on the lateral condyle, allowing for the gradual dissipation of forces with a stronger bond. Then, there is the ‘indirect type’. It is a thin, membranous, peripheral attachment of fibers that spread out toward the posterolateral condyle in which the ligament is inserted into bone by collagen fibers without a transitional zone increasing the area of the insertion site (fan-like extension). In that way it makes a weaker connection.9,15 The fibers of the intermediate bundle spiral around the middle of the ACL and then narrow and flatten mediolaterally near the femoral footprint.13
In a previous study, we stated that the femoral insertion of the ACL presents variations in its morphology over time. It goes from being large and semicircular in shape in young subjects to a smaller and flattened ribbon-like shape in older subjects.9 This finding as well as findings in various other several publications emphasizes the need to do further research in young specimens.8,9,16,20
Tibial footprintThe centrum of the ACL tibial footprint is 15mm anterior to the posterior cruciate ligament and two-fifths of the medial-to-lateral width of the interspinous distance.12 The tibial insertion site is larger, with recent studies finding the cross-sectional area ranging between 100 and 160mm2.8
Three main tibial insertion site shapes (oval/elliptical, triangular, and C-shaped) have been described, being wider posteriorly and situated anteriorly in the intercondylar area. Other kinds of morphologies have also been reported like the boot-like shaped, L-shaped, J-shaped, and double C-shaped. However, most individuals present elliptical insertion site shapes followed by the triangular and C-shaped.4,8,16
The tibial attachment is oriented in an oblique direction. It is wider than the femoral attachment and it is inserted in a well-marked slip adjacent to the anterior horn of the lateral meniscus.10,13
The anteromedial bundle is positioned on the anteromedial aspect of the tibial insertion where its medial border is the anteromedial margin of the articular surface of the medial tibial condyle. The posterolateral bundle is believed to be situated in the posterolateral aspect of the intercondylar area, with its lateral border being the medial margin of the articular surface of the lateral tibial condyle.4 The intermediate bundle has an attachment in the central region of the tibial footprint.13
The tibial insertion footprint width was found to be an average of 12.6mm (7.7–16.3) with a mean thickness of 3.3mm (2.5–3.9).4
The tibial ACL footprint also shows morphological variations between young and old cadaveric specimens.16
Blood supplyThe middle genicular artery is the primary blood supply to the ACL. However, there is also some contribution of both inferior genicular arteries and via diffusion through the ACL's synovial sheath.6,10
A septum of connective tissue containing vascular stem cells separate the AM and PL bundles. This membrane contains periligamentous vessels that transversely penetrate the ligament and anastomose with a longitudinal network of endoligamentous vessels that vascularize the ACL.1
InnervationThe ACL is innervated by the tibial nerve, which presents nerve endings that perforate the posterior capsule and run along the ligamentous path next to the synovial membrane. This innervation is also provided by vessels that bring in mechanoreceptors that contribute to the ACL's proprioceptive function.6,17,18 There are minimal pain fibers in the ACL, which explains why there is rarely pain after an acute ACL tear until the development of a hemarthrosis.6
BiomechanicsFunctionally, the ACL serves several purposes. It prevents anterior translation of the tibia on the femur, acts as a secondary stabilizer against the internal rotation of the tibia and valgus angulation of the knee. It sustains normal biomechanical knee motion to prevent meniscal damage. The two bundles that comprise the ACL have unique functions that allow for the ACL's normal biomechanics. The anteromedial bundle is tight in flexion, whereas the posterolateral bundle is tight in extension.6 The anatomical and biomechanical properties of the intermediate bundle are similar to that of the AM bundle.1
In full extension, the ACL absorbs 75% of the anterior translation load and 85% between 30 and 90 degrees of flexion. Loss of the ACL leads to a decreased magnitude of this coupled rotation during flexion and an unstable knee. The average tensile strength of the ACL is ∼2200N but is altered with age and repetitive loads.6
Clinical relevance of current ACL anatomy studiesIndividualized anatomic ACL reconstructionThe surgical goal in ACL anatomic reconstruction, is to mimic native ligament anatomy as closely as possible to recover the function of the knee. That means restoring the native dimensions, collagen orientation and insertion sites.9,19
Anatomic ACL reconstruction is based on four fundamental principles: (1) restoring the anteromedial and posterolateral bundles; (2) restoring the native ACL insertion sites by aligning the tunnels in proper anatomic positions; (3) correctly tensioning each bundle; and (4) adapting the reconstruction to each patient by ensuring that tunnel diameter and graft size are determined in accordance with the characteristics of their native insertion sites.1
The shape of the insertion sites has become a factor in determining individualized ACL reconstruction. There are studies that suggest that different shapes may require different types of reconstruction to ensure proper footprint restoration.8,16 A “C-shaped” tibial footprint may be better restored using a double-bundle technique, while an “elliptical” tibial footprint may be sufficiently restored using a single-bundle technique.16
Dimitris et al. stated that femoral origin of the AM bundle is located more posteriorly in the same proximo-distal direction, whereas the PL bundle origin was found more distally in approximately the same anterior–posterior direction in ACL-rupture knees when compared to ACL-intact knees. The femoral tunnel for ACL reconstruction should be deep (proximal) and high (anterior) in the intercondylar notch within the region of the anteromedial bundle of the femoral footprint of the ACL as the fibers comprising the remainder of the femoral footprint have a weaker attachment and take less of a load.9
Anatomical double-bundle reconstruction has gained popularity during the last decade. As a result, several biomechanical studies have reported, with a short-term follow up, that it more closely restores healthy knee kinematics. Furthermore, clinical studies have demonstrated superior outcomes in terms of knee laxity and graft failure compared with the single-bundle reconstruction.21 It requires detailed knowledge of the anatomy of the anteromedial and posterolateral bundles in ACL-ruptured patients, as potential differences might exist between ACL-rupture knees and healthy knees. However, most recent studies with at least a 5-year follow-up have shown similar outcomes at the mid-term and long-term. The double-bundle reconstruction was seen to be no more effective in preventing the progression of osteoarthrosis or getting a better clinical outcome than the single-bundle.24–26
ACL agingThe average age and life expectancy as well as the level of physical activity in the elderly population are rising. This has led to an increase in sport-related injuries in older populations with high expectations of returning to their pre-injury level of activity.20
Characterized by individual uniqueness, the ACL is inherently subject to both anatomical and morphological variations as well as physiological aging.8,9,16 Thus, surgical reconstruction of the ACL is more broadly applied. Nowadays, patients over 50 years of age who require surgical ACL reconstruction represent a significant share with studies concluding that this procedure shows good results in terms of symptomatic relief, restoration of function and return to sporting activity.20
Important morphological factors relative to ACL aging are its femoral and tibial footprints, as well as bundle degeneration. Indirect fan-like femoral fibers increase with age due to degeneration of the direct ones, favoring a weaker attachment in older patients.9 Both ACL bundles undergo aging, with degenerative changes in 53% of the AM bundles and 78% of the PL bundles. With the more severe changes in the latter, there is the suggestion of intercondylar notch stenosis and intercondylar notch osteophytes.9,14
Some ACL-reconstruction techniques have modified the conventional femoral round tunnels and replaced them with shapes that resemble a flat, rectangular tunnel using either a rectangular quadriceps tendon graft or a “flat” hamstring graft with the purpose of providing a biomechanical advantage.22 However, it is important to consider the changes in the configuration of the ACL morphology according to patients’ age as different ACL age-related characteristics may not fit with the proposed reconstruction technique.
ConclusionGreat variability exists in both the anatomy of the ACL as well as its attachment sites. At the same time, the shape and size of footprint has become a factor in determining individualized ACL reconstruction. The persistence of morphological variability regarding ACL aging and important aspects for surgical planning and decision making among anatomical risk factors leaves an open door for further studies.
Conflict of interestEach author certifies that neither he or she, nor any member of his or her immediate family, has funding or commercial associations (consultancies, stock ownership, equity interest, patent/licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted study.
FundingThe authors declare that they have received no funding for the conduct of the present research, the preparation of the article, or its publication.