The term amyloidosis has been applied to a group of diseases which produce a deposit of extracellular material in organs and tissues. The joint symptoms appear due to the destruction process, with the development of erosions and significant joint effusions. The diagnosis and treatment of amyloidosis are based on histopathological and immunohistochemical studies of the amyloid deposits.
Clinical caseWe present the case of a 58 year-old male, with a history of peritoneal dialysis 15 years ago and currently on haemodialysis treatment. He came to our clinic complaining of inguinal pain which began a year ago and was refractory to analgesic treatment. The radiology study showed a massive destruction of the coxofemoral joint. The study was extended by using magnetic resonance, which showed the presence of erosions with a sclerosing border in the iliac region and the presence of an abundant joint effusion; data suggestive of an erosive inflammatory arthritis associated with an infectious process or amyloid deposit. A joint biopsy using open surgery enabled the diagnosis of hip amyloidosis to be made using Congo red stain. After ruling out a septic process, it was decided to perform a hip replacement.
ConclusionAmyloidosis mainly in the bone and joint is an uncommon manifestation of this disease; the diagnostic suspicion is fundamental to be able to direct the histopathologist to its definitive diagnosis, since these stains are not used routinely.
El término amiloidosis se ha aplicado a un grupo de enfermedades que producen un depósito extracelular de material en órganos y tejidos. Cuando produce manifestaciones articulares genera una destrucción de las mismas con desarrollo de erosiones e importante derrame articular. El diagnóstico y el tratamiento de la amiloidosis se funda en el diagnóstico histopatológico e inmunohistoquímico de los depósitos de amiloide.
Caso clínicoPresentamos un varón de 58 años, con antecedente de diálisis peritoneal hace 15 años y en tratamiento con hemodiálisis en la actualidad. Acude a nuestra consulta por dolor inguinal de un año de evolución y refractario a tratamiento analgésico. El estudio radiológico muestra una destrucción masiva de la articulación coxofemoral. Se amplió el estudio mediante resonancia magnética observando la presencia de erosiones con borde escleroso en la región ilíaca y la presencia de derrame articular abundante, datos sugestivos de artropatía inflamatoria erosiva en relación con proceso infeccioso o depósito de amiloide. Una biopsia articular mediante cirugía abierta permitió el diagnóstico de amiloidosis de cadera mediante el uso de tinción rojo Congo. Tras descartar proceso séptico se decidió la colocación de una artroplastia de cadera.
ConclusiónLa amiloidosis de predominio osteoarticular es una manifestación poco frecuente de esta enfermedad, el diagnóstico de sospecha es fundamental para poder orientar al anatomopatólogo a su diagnóstico definitivo, ya que el uso de estas tinciones no se realiza de rutina.
Amyloidosis can be defined as the extracellular deposit of amyloid fibril proteins at one or more locations in the body. They may be deposited locally in areas where they do not bring about any clinical consequences or they may affect practically all the organs in the body and cause serious pathophysiological alterations.1,2
There are multiple clinical forms of amyloidosis that are classified according to their characteristic fibrillar structure. From a clinical perspective, the following is the most useful classification: (1) primary systemic amyloidosis (AL type) is a dyscrasia of plasma cells that gives rise to a clonal proliferation of these cells in bone marrow, although fatigue and weight loss are its most frequent initial manifestations; myocardiopathy and neuropathic compromise are the predominant features of this kind of amyloidosis3; (2) amyloidosis associated with multiple myeloma (AL type), the prevalence of amyloidosis in multiple myeloma is 10%4; (3) secondary reactive amyloidosis (AA type) associated with chronic infectious or inflammatory diseases including rheumatoid arthritis, idiopathic juvenile arthritis, ankylosing spondylitis, familial Mediterranean fever, chronic infections and neoplasias. The organ most frequently affected in amyloidosis (AA) is the kidney (∼80%). It usually presents as an amyloid glomerular deposit, triggering a nephrotic syndrome in the patient5; (4) inherited familial amyloidosis constitutes a group of dominant autosomal illnesses characterized by the extracellular deposit of amyloid fibrils in various organs and tissues, predominantly affecting the peripheral nerves; (5) local amyloidosis, and (6) amyloidosis secondary to chronic haemodialysis, a type of amyloidosis associated with the deposit of β2-microglobulin. Its prevalence reaches 80% in patients undergoing dialysis for more than 15 years. It is characterized by major osteoarticular compromise and is more often associated with haemodialysis than with peritoneal dialysis.6
The incidence of AA amyloidosis in autopsy studies varies between 0.5% and 0.86%.7 This incidence has come down thanks to disease modifying drugs and the biological therapy used by rheumatologists. Prior to 1990, when only NSAIDs and corticosteroids were used to control autoimmune diseases, it was frequent to observe cases of amyloidosis in these patients, mainly in rheumatoid arthritis. Rheumatoid arthritis and idiopathic juvenile arthritis continue to represent the largest number of cases of amyloidosis, with 48–56% of the total. Ankylosing spondylitis affects 5–8% of cases and psoriatic arthritis between 4% and 5% of amyloidosis cases.8
Amyloid material nay directly affect joint structure through its presence in membranes, synovial fluid or in the cartilage of the joint. Amyloid arthritis may simulate a rheumatic process because it may course as a symmetric arthritis of small joints with nodules, early-morning stiffness and fatigue. Most patients with amyloid arthropathy are ultimately diagnosed as having multiple myeloma. Synovial fluid usually presents a low white cell count, an adequate level of mucin and dominance of mononuclear cells in the absence of crystals.9 Amyloid infiltration of the muscle may cause pseudomyopathy.
The specific diagnosis of amyloidosis is reached through the pathology study and is demonstrated using appropriate staining. When these manifestations occur in a patient with a chronic disorder predisposing to amyloidosis, such as rheumatoid arthritis, tuberculosis, paraplegia, or multiple myeloma, amyloidosis must be ruled out. Primary systemic amyloidosis must be ruled out in anyone presenting a non-inflammatory diffuse infiltrative process.
Case reportWe present a 58-year-old male patient with a history of 15 years of peritoneal dialysis and currently under treatment with haemodialysis; he attended our clinic presenting coxalgia lasting for one year without any history of trauma and gradual onset.
A radiographic study was made of the pelvis and both hips, revealing destruction of the left coxofemoral articulation and presenting osteolytic lesions on the upper part of the acetabulum and almost total destruction of the head of the femur (Fig. 1). The study was extended to include magnetic resonance, which revealed extensive destruction of the iliac region and the head of the femur with the presence of an extensive articular effusion (Fig. 2). In view of the progressive course of this process and the lack of a definitive diagnosis, it was decided to perform an open bone and joint biopsy of the coxofemoral articulation to rule out any tumoural or infectious process and accumulation disease.
The aggressive evolution of this process forced us to carry out a differential diagnosis in which we had to rule out infectious arthritides, micro-crystalline arthritides or accumulation disease such as amyloidosis. In addition to these pathologies, we must also rule out the presence of any tumoural process, with the most frequent diagnostic possibility considering the patient's age and the location being multiple myeloma or metastatic disease. Such an extensive involvement of the acetabulum reduces the possibility it might be an osteonecrosis of the femur head.
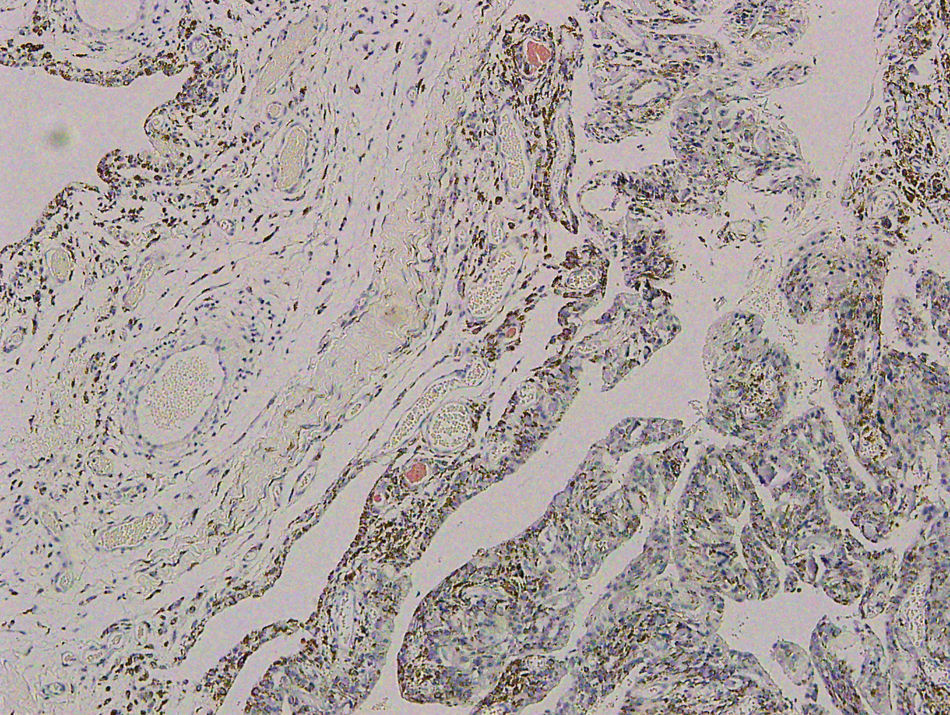
With the suspicion of accumulation disease, a specific sample was requested to detect an amyloid deposit and this was positive for Congo Red staining (Fig. 3). In the same figure, we can observe the extracellular location of amyloid deposit in the synovial membrane. After the diagnosis of secondary amyloidosis, probably due to his kidney replacement therapy and after first ruling out any infectious or tumour-related process, it was decided to perform total hip replacement arthroplasty. During the surgery, the presence of a deficit was observed in the upper wall of the acetabulum and it was decided to use trabecular metal supplements in the same to cover the defect (Fig. 4).
After three years of evolution, the patient is asymptomatic and no radiographic mobilizations of his arthroplasty have been observed. He is currently monitored by the Rheumatology and Nephrology Departments and follows a specific treatment for his amyloidosis.
DiscussionAmyloidosis with osteoarticular predominance is an infrequent manifestation of this disease, so a suspected diagnosis is fundamental in order to guide the pathologist to a definitive diagnosis as these staining techniques are not routinely used.10
The possible musculo-skeletal manifestations of amyloidosis may include involvement of muscle, bone and joints.
When “muscular involvement” occurs, the amyloid deposit in muscles may cause an increase in size, producing a pseudohypertrophy that is observed in 25% of cases. Another important form of muscle compromise is amyloid inclusion body myopathy, the most common cause of metabolic myopathy in individuals over 50 years of age.11
When amyloidosis produces “articular involvement”, microdeposits occur in the joint similar to those occurring in rheumatoid arthritis; however, this involvement usually courses in a sub-acute and slowly progressive form with a preference for shoulders, knees, wrists, metacarpophalangeal (MCP) joints and proximal interphalangeal (PIP) joints, followed by the elbows and hips. Generally speaking, there is little early-morning stiffness and the joints are slightly painful, allowing its differentiation from arthrosis. Nonetheless, the articular compromise is on occasions so similar to rheumatoid arthritis that it is difficult to distinguish it from this ailment.12
Synovial fluid usually presents a low white cell count, an adequate level of mucin and dominance of mononuclear cells in the absence of crystals. The definitive diagnosis is reached using Congo Red staining.
When “bone involvement” occurs, solitary or multiple pseudotumoural lesions are noted, usually occupied by amyloid material and possibly associated with pain or pathological fractures.13
Amyloidosis secondary to renal dialysis is due to the inability of the cellulose membranes to remove β2-microglobulin. Under normal conditions, it is filtered out in the glomerule. In patients with kidney failure receiving haemodialysis, this substance accumulates and turns into an amyloid material that stains with Congo Red and is positive to birefringence in polarized light. This is different from the amyloid material appearing in chronic infections and some neoplasias. The characteristic radiographic findings include articular erosions that can be confused with hyperparathyroidism.14–17 When the accumulation takes place in the bones, most patients develop asymptomatic sub-chondral cysts.18
Prior suspicion is important in this process which, albeit rare, is difficult to diagnose as, unless a definite request is made for detection of the amyloid protein using specific staining techniques, it may go unnoticed when examined by the pathologists.
Level of evidenceLevel of evidence IV.
Protection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Please cite this article as: Parrón Cambero R, et al. Amiloidosis de cadera. Presentación de un caso y revisión de la bibliografía. Rev Esp Cir Ortop Traumatol. 2011; 55(5):385–388.