To evaluate the clinical and electrophysiological results in the medium term of the arthroscopic release of the proximal entrapment of the suprascapular nerve.
Material and methodIt is a retrospective study that includes 75 patients with idiopathic entrapment of the suprascapular nerve in the suprascapular notch in whom conservative treatment has failed. All patients underwent electrophysiological tests (EMG) as well as clinical test (Constant and DASH test) preoperatively and during follow-up.
Results75 patients (53 women and 22 men) with a mean age of 44,1±10,7 years met study criteria with a mean follow-up of 63,7±29,1 months. Preoperatively the DASH value was 78,6±10,2, the Constant test value was 37,1±8,8 and the EVA value was 8, 8±1.1 while the values in the last revision were 19,4±15,8 for DASH, 80,2±9,6 (for the CS and 2±1,3 for the EVA scale; the differences were significant in all cases (p<0.001). Regarding the results of the electrophysiological test, preoperatively there were 21 very severe grades (28%), 32 severe (42,6%), 17 moderate (22,6%) and 5 mild (6,6%). While in the last review there were 3 severe degrees (4%), 6 moderate (8%), 40 mild (53,3%) and 26 normal (34,6%). There was no very severe grade (0%). 3 patients(4%) had to be reoperated due to persistent symptons.
ConclusionsThe arthroscopic release of idiopathic entrapment of the suprascapular nerve in the superior scapular notch achieved good clinical and electrophysiological results in the medium term.
Level of evidenceLevel IV; Case series; Treatment study.
Evaluar el resultado clinico y electrofisiológico a medio plazo de la liberación artroscópica del atrapamiento proximal del nervio supraescapular
Material y métodoEs un estudio retrospectivo que incluye 75 pacientes con atrapamiento idiopático del nervio supraescapular en la escotadura escapular superior en los que ha fracasado el tratamiento conservador. Todos los pacientes fueron sometidos a pruebas electrofisiológicas (EMG/ENG) así como a test clínicos (EVA, test de Constant y DASH) preoperatoriamente y durante el seguimiento.
Resultados75 pacientes (53 mujeres y 22 hombres) con una edad media de 44,1±10,7 años cumplieron criterios de estudio con un seguimiento medio de 63,7±29,1 meses. Preoperatoriamente el valor del DASH fue de 78,6±10,2, el del test de Constant de 37,1±8,8 y el de la EVA de 8,8±1,1 mientras que los valores en la última revisión fueron de 19,4±15,8 para el DASH, de 80,2±9,6 para el CS y de 2±1,3 para la escala EVA siendo en todos los casos las diferencias estadísticamente significativas (p<0,001). En cuanto a los resultados de la prueba electrofisiológicas, preoperatoriamente hubo 21 grados muy graves (28%), 32 graves (42,6%), 17 moderados (22,6%) y 5 leves (6,6%). Mientras que en la última revisión hubo 3 grados graves (4%), 6 moderados (8%), 40 leves (53,3%) y 26 normales (34,6%). No hubo ningún grado muy grave(0%). 3 pacientes (4%) tuvieron que ser reintervenidos por persistencia de los síntomas.
ConclusionesLa liberación artroscópica del atrapamiento idiopático del nervio supraescapular en la escotadura escapular superior tiene buenos resultados clínicos y electrofisiológicos a medio plazo.
Nivel de evidencia: IV. Serie retrospectiva de casos.
Traditionally considered a diagnosis of exclusion, supra-scapular neuropathy is an increasingly more recognised cause of omalgia (2%-3% in the last series),1 with diagnosis posing a challenge due to the subtlety of its symptoms. The supra-scapular nerve (SSN) arises from the upper trunk of the brachial plexus, primarily drawing from branches C5 and C6 (on occasions also from C4).2,3 It is responsible for the innervations of the supraspinatus and infraspinatus muscles and sensory branches to the skin, the coracohumeral and coracoacromial ligaments, supra-acromial bursa and acomioclavicular and glenohumeral joints.4 Its anatomical trajectory makes it particularly vulnerable to compression or traction either, statically or dynamically.5,6
Although conservative treatment is initially chosen, especially in absence of space-occupying lesions,7 early action should be considered to avoid neurological damage and irreversible muscular atrophy, although it is unclear how much time is required for this.8 Surgery is reserved for when conservative treatment fails and has evolved from an open to an arthroscopic approach.9 Most results on treatment are case series and retrospective reviews, dealing with few patients and limited evolution periods.
The aim of this study was to assess the medium-term clinical and electrophysiological results of arthroscopic release of proximal supra-scapular idiopathic nerve entrapment when this was the only identifiable cause of omalgia.
Material and methodA retrospective, controlled, non-randomised study of patients with idiopathic entrapment of the SSN in the supra-scapular notch in the General University Hospital Los Arcos del Mar Menor, in Murcia, from January 2010 until January 2018. The study was appraised and approved by the ethics committee of Area VIII of the Region of Murcia (RET-01-2020).
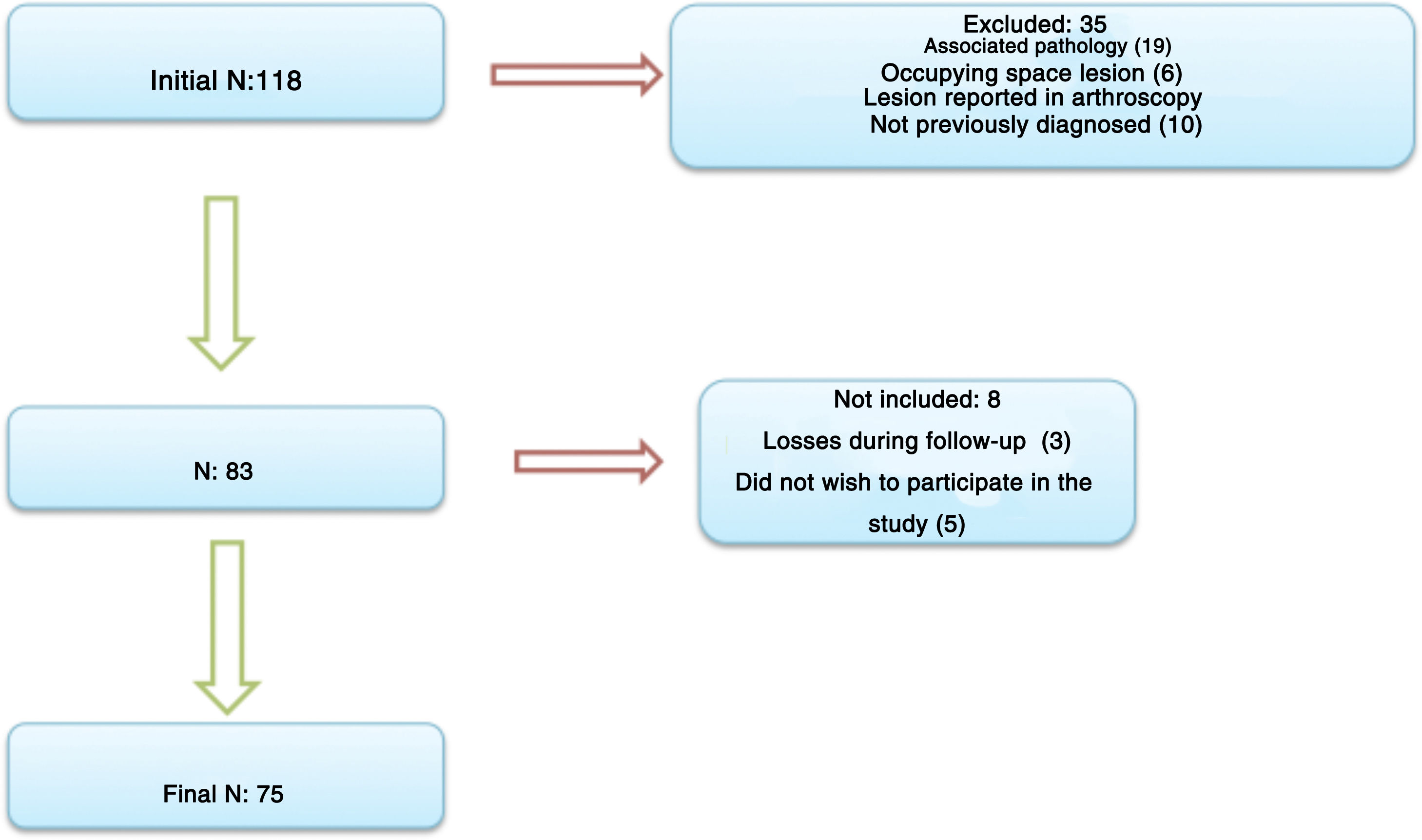
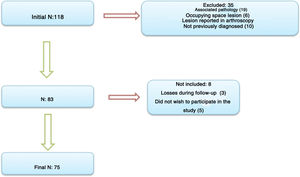
Inclusion criteria were: patients with omalgia refractory to conservative treatment for at least 6 months, whose additional imaging tests (radiology, magnetic resonance, computerised tomography or scan) showed no anatomical lesions, and the completion of an electromyography or electroneurography (hereinafter EMG/ENG) in keeping with an entrapment of the SSN. They were all offered arthroscopic relapse of this nerve, and after signing the relevant informed consent, were operated on during the previously referred to period. Minimal follow-up for study participation was 2 years. Exclusion criteria were: patients who had undergone previous surgery or fractures in the affected shoulder, rotator cuff arthropathy, glenohumeral instability, known neuropathy or previous reported disease of the brachial plexus or ipsolateral cervical nerve, space-occupying lesions, such as cysts or spinoglenoid tumours, and all patients who were shown to have a previously undocumented lesion during arthroscopy and which could have been the cause of the shoulder pain (labral lesion, spinoglenoid cyst, rotator cuff tear, os acromiale, etc.). Those patients who were lost to follow-up were not included in the study, along with those who did not wish to participate in it. Neither were those who presented with an intervention or trauma in the same shoulder during follow-up. Initially 118 patients took part, 35 of whom were excluded in the previous selection (19 due to an associated pathology, 6 for space-occupying lesions and 10 for associated lesions found during arthroscopy). Of the remaining 83 patients, 5 did not wish to participate in the study and 3 could not complete follow-up, resulting in a final study sample of 75 (Fig. 1).
Patient evaluation included examinations performed and a final revision relating to this study in the medical practice, made by an independent surgeon (FPM).
Variables such as age, sex, side and affected dominant arm, follow-up time, duration of surgery, complications or need for further surgery were collected. We also assessed the time from when the patient began to have symptoms until the time they sought a practitioner’s advice. Possible complications were taken on board, such as the presence of infection, vascular involvement, neurological involvement or any directly derived from the anaesthesia (reported cerebral hypoperfusion in patients operated on in reclining position). Another defined complication was that of patients who had to undergo further surgery due to the persistence of symptoms and with an electrophysiological test confirming this during the first postoperative year, with no other justifiable cause.
The visual analogue scale (VAS hereinafter)10 for pain was applied to all patients with scores from 0 (absence of pain) to 10 (unbearable pain); the Disabilities of the arm, shoulder and hand (DASH hereinafter)11 test, with a range from 0 (maximum possible function of the shoulder) to 100 (no function), and the Constant scale test (CS hereinafter)12 with scores from 0 (minimum, worst possible result) to 100 (maximum score). The 3 tests were applied preoperatively, after one month, and at 3,6,12 and 24 months; from then onwards, biannual tests were performed up until the final revision. The contralateral shoulder in the final revision was also assessed as a comparison. All patients had to have a preoperative electrophysiological test which verified SSN compression and which was repeated after one year, at 2 years and at the final revision. There were 5 possible results from lesser to greater severity (normal, light, moderate, severe and very severe). The typical findings of peripherical neuropathy of the supra-scapular nerve include denervation changes with reduction of impulse speed, fibrillation and p-waves when resting, and increase of distal motor latency. All patients were given a satisfaction questionnaire (highly satisfied, satisfied, indifferent, not satisfied or not satisfied at all) and they were asked if they would undergo further surgery (yes or no).
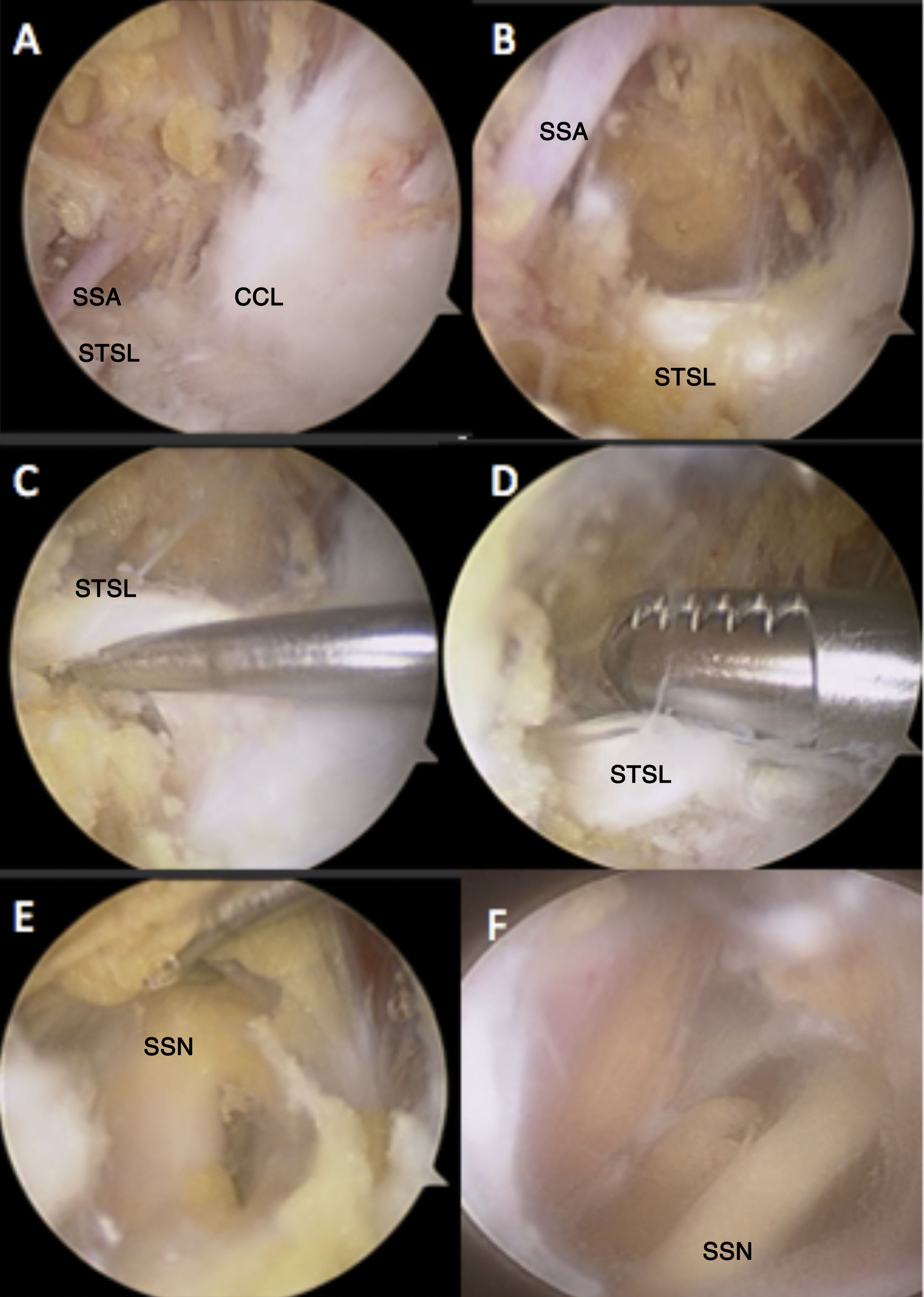
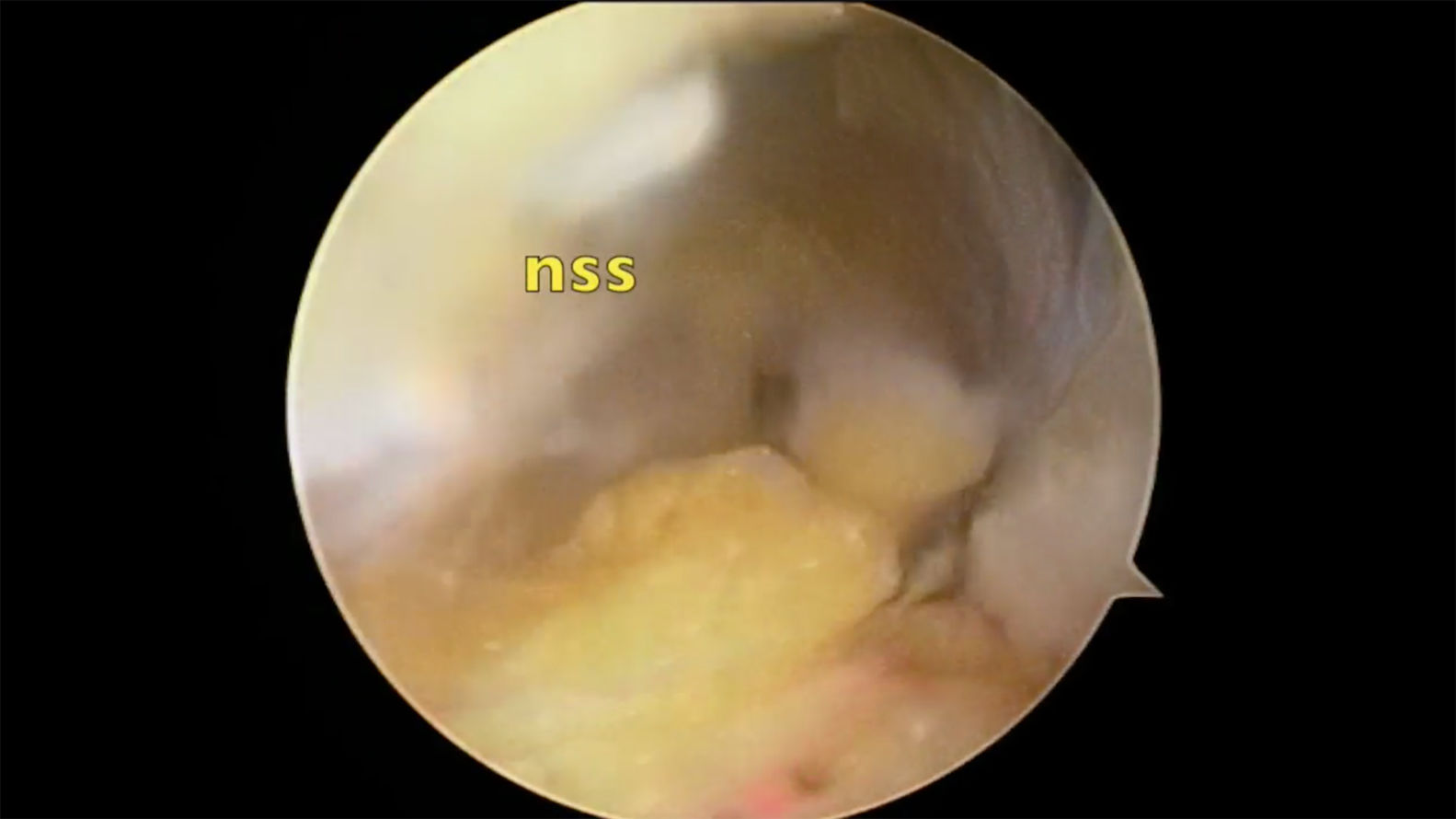
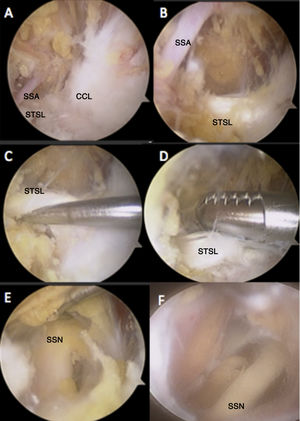
The surgical technique used was arthroscopic release of the SSN in reclining position, under general anaesthesia and brachial plexus block. Antibiotic prophylaxis was administered in all cases with cefazolin. Four portals were used: one standard posterior view portal, the Neviaser portal, an anterolateral portal and another anterosuperior one, similar to the technique described by Lafosse and Tomasi13 and Lafosse et al.14 (details of this technique are presented in Fig. 2 and the Appendix B video 1, appendix). Care must be taken when identifying the supra-scapular artery, because if it is inadvertently damaged haemostasis and successful surgical completion may become complicated.
Images where several details for arthroscopic observation of the process are noted. Observation in anterolateral portal. A) View of the whole working framework with anatomical reference of the medial edge of coracoclavicular ligaments. B) More detailed view, where the supra and perpendicular ligament location of the supra-scapular artery is appreciated with respect to the superior transverse scapular ligament of the scapular. C) Release of the lower edge of the ligament with respect to the nerve running underneath it. D) Section with ligament synovectomy. No aspiration to be used. E) View of nerve before removing adjacent tissues. F) Final image of the nerve once attachments and tissues were released.
SSA: supra-scapular artery; CCL: Coracoclavicular ligaments, medial edge; STSL: superior transverse scapular ligament; SSN: supra-scapular nerve.
After surgery, the patient had their arm in a sling for 3 weeks in neutral rotation and with slight abduction (30°). They were able to remove their arm 3 times a day for 10min to carry out pendular exercises from the 7th to 10th day. After removing it, an active mobility programme begann, but no force was used until the 3rd postsurgical month. Particular emphasis was placed on recovering external rotation strength.
Statistical analysis was carried out with the SPSS system, version 19.0 (IBM Corp, Armonk, NY, U.S.A.). Quantitative variables were shown as mean, ± standard deviation and range in parenthesis. The Kolmogorov-Smirnov test was used to confirm their normality. Qualitative variables were shown as absolute frequencies and percentages. To confirm whether any differences existed between the variables means, the student’s t-test was used for paired data. Verification of relationships between quantitative variables was made with the Pearson correlation. A p value under .05 was considered statistically significant.
ResultsMean age±standard deviation of the 75 study participants was 44.1±10.7 years (range from 22 to 61), of whom 53 were women (70.6%) and 22, men (29.4%). The dominant side (54 cases, 72%) was more frequently affected than the non dominant (21 cases, 28%), whilst the most frequently affected shoulder was the right one, with 48 cases (64%).
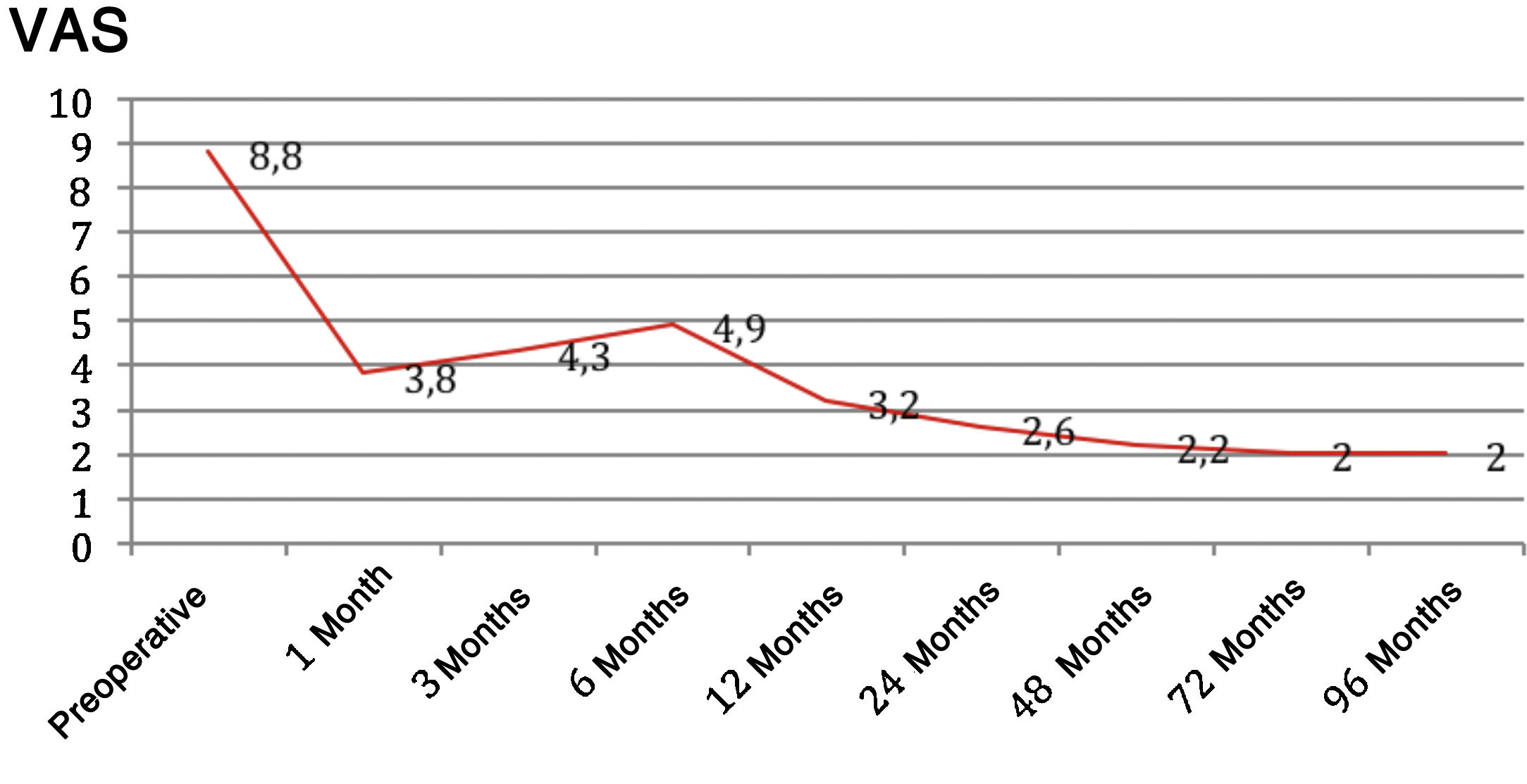
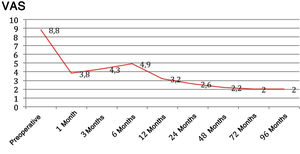
Mean follow-up was 63.7±29.1 months (range 24–117)and time in surgery was 46.8±15.9min (range 25–78). Mean time from the appearance of symptoms until consulting a practitioner was 17±3 months (range 6–31). Preoperative VAS score was 8.8±1.1 (range 7–10) and that of final follow-up was 2±1.3 (range 0–4), with a statistically significant difference (p<.001). Preoperatively, the DASH value was 78.6±10.2 (range 66.7–100) and the CS was of 37.1±8.8 (range 5–33), whilst the values in the final review were 19.4±15.8 (range 5–45) for the DASH and 80.2±9.6 (range 58–93) for the CS, with significant differences existing in both cases (p<.001). Scores for the contralateral shoulder in the final revision were 5.1±1.7 in the DASH (range 0–108), 92±3.4 in the CS (range 84–100) and 0.5±.2 in the VAS (range 0–3). In none of the 3 tests were differences statistically significant regarding the healthy side.
With regard to the preoperative electrophysiological test results, there were 21 very severe grades (28%), 32 severe (42.6%), 17 moderate (22.6%) and 5 mild (6.6%). During the last revision there were 3 severe grades (4%), 6 moderate (8%), 40 mild (53.3%) and 26 normale (34.6%). There were no very severe grades (0%). Out of the 21 initially very severe cases, at the final revision there were 3 severe cases (14.2%), 2 moderate (9.5%), 16 mild (7.,4%) and none normal. Of the 32 severe cases, in the last revision there were 4 moderate grades (12.5%), 15 mild (46.8%) and 13 normal (40.6%). Of the 17 moderate cases, the results in the final revision were 6 mild cases (352%) and 11 normal (64.7%). And of the 5 mild grades, 3 remained the same (60%) and 2 became normal (40%). In the 75 study cases one patient presented with a complete ossification of the superior transverse scapular which required reaming to access the nerve.
There were 6 complications (8%) during follow-up, 2 of which were superficial infections (2.6%) of arthroscopic portals which responded to local cures and antibiotics; one musculocutaneous nerve paresis (1.3%) reported in the EMG as neuropraxis and with clinical weakness to forearm flexion-supination which completely recovered between the 6 and 12 months after surgery and 3 patients who due to persistence of pain had to be operated on again (4%) for review of the nerve and release of subacromial fibrosis before one year. No vascular or central neurological deficits were reported.
No statistical relationship existed between the results of the clinical tests or the degree of entrapment and the presence of complications. Neither was the need for further surgery related to previous lesion grading. With regard to satisfaction level, 15 patients stated they felt highly satisfied (20%), 38 satisfied (50.6%), 5 indifferent (6.6%), 15 not satisfied (20%) and 2 not satisfied at all (2.6%); 57 patients (76%) agreed to undergo further surgery.
DiscussionThe arthroscopic release of proximal supra-scapular nerve entrapment, once conservative treatment has failed, obtains good clinical results in the medium and long term, especially in moderate and severe cases. The first description of SSN dates back to 1886,15–17 and was defined as a nosological entity in 1959 by Kopell and Thompson.18 Aiello et al.19 differentiated between proximal entrapment (supra-scapular notch) and distal entrapment (spinoglenoid notch). Proximal nerve entrapment affects the supra and infraspinous muscles, whilst the distal entrapment only affects the latter, with the main cause of it being a spinoglenoid cyst20–22 linked to type II SLAP tears.23–25
Among the injury mechanisms reported for proximal entrapment, which is the object of this study, are micro embolisms of the supra-scapular artery, compression in the supra-scapular notch which narrows or becomes ossified, repetitive traction, surgical iatrogenesis, fractures or tear and retraction of the rotator cuff.26 In any event, the great anatomical variability in both nerve pathway and the notch itself, where the nerve is relatively fixed, make them highly vulnerable.27,28
Clinical identification of an entrapment of the SSN is not simple when it is not associated with a rotator cuff rupture, since 38% of rotator cuff tears carry an SSN-associated pathology, whilst in only 3% isolated damage to the nerve occurs where there is no rotator cuff tear.29,30 Our series was formed of idiopathic cases which are more difficult to identify due to the subtlety of symptoms they present. Posterosuperior dull pain and weakness in muscle function (external abduction and rotation with elbow tight against the body)19 are common to other pathological processes. Clinical tests, such as that of Lafosse et al.,31 are very low on sensitivity and muscular atrophy is infrequent. Electrophysiological tests should complete the study since although diagnosis is not excluded by them being negative, as occurs for example in patients with sarcopenia, positive testing helps to guide physicians towards accurate therapeutic decisións.32
There are few studies in the literature which have reported the results of isolated surgical release of the SSN.13,33 It is more common to find this release as an add-on to the rotator cuff tear repair to remove tension to the nerve34 which increases the rate of tendon repair,35 but it is unclear whether the clinical course actually improves.36
In our study we obtained a statistically significant improvement in all the clinical tests. The parameter which improved the most was pain, in over 90% of cases, as with the larger part of studies described which ranged between 80% and 95%,37 although patients were rarely asymptomatic. The second parameter which improved the most was mobility, and above all in abduction, elevation and external rotation. Internal rotation is usually slow to recover and is not always recovered completely. Most daily life activities were carried out almost normally. Strength is the parameter which was most difficult to recover, especially in external rotation, where most of the time it remained at 80% compared with the healthy arm. Atrophy was infrequent but when it did present it was difficult to fully revert (especially in the infra spinus nerve).38
After initial improvement, pain remained the same or increased during the first 3-6 months after surgery and began to decline between 6 months to a year, where it stabilised and rarely underwent any major changes (Fig. 3). This data is new in this study, since in those already published, initial and final pain was reported but not its evolution over time. This pain may be caused by direct or indirect manipulation of the nerve and the curing process since after surgical aggression the nerve may become irritated and inflamed and this leads to an increase in pain during the first few months.
In fact, only one third of patients obtained electrophysical normality in the final revision in contrast to other studies, where they are usually associated with rotator cur tear repair.39 The severe and moderate grades are what really obtained greater clinical and electrophysiological improvement, with normality in the EMG at the end of treatment of around 40% and 60% respectively. The very severe grade never achieved electrophysiological improvement and although patients had improved, a relatively high residual pain usually remained.40 Nevertheless, the low improvement obtained in the few mild grades operated on (5) necessitates great adjustment to the need for surgery in this subgroup. These 2 last patient groups (very severe and mild) may explain why 25% of patients would not repeat surgery and highlights the need to adjust patient expectations to probable results. Our meticulousness regarding surgical indication could account for why our number of cases over time, following an initial growth period of 3–4 years, stabilised and even diminished.
Arthroscopic technique has proved to be safe and effective compared with standard open surgery,41 and there is only a need to anticipate anatomical variations of the supra-scapular artery (3% subligamentary)42 or ossification of the transverse ligament of the scapula with reported ethnic variability (3% in white Caucasians; 1.3% in our series).43 It is important not to make the Neviaser portal very medial in order to prevent spinal accessory nerve damage,44 with safe blunt dissection up to 2.5cm medial to the acromioclavicular joint (some 5cm medial to the lateral edge of the coracoids), before finding the nerve or the supra-scapular artery.45 Mean time in surgery of the complete arthroscopic process was 46min in our series. According to Yamakado,46 who presents the longest series described in the references (300 patients), 60 cases are required to learn the technique (in our series we stabilsed the time to around 30–40 cases). The technique has a learning curve rate of 70%, which means that in the second case we would use approximately 70% of the time invested in the first case and so on and so forth. The main criticism of this article is that it neither reports clinical results nor previous electrophysiological tests to confirm diagnosis, which limits the extrapolation of results.
Therefore, and although conservative treatment (medication, physiotherapy, injections) must be considered as the initial treatment of choice, those patients with persistent pain after 8–12 weeks and an electrophysiological test to indicate moderate or higher entrapment, should be referred to a specialist to assess surgical release since the results of this study indicate that long delay in this treatment would entail non optimum outcomes.47
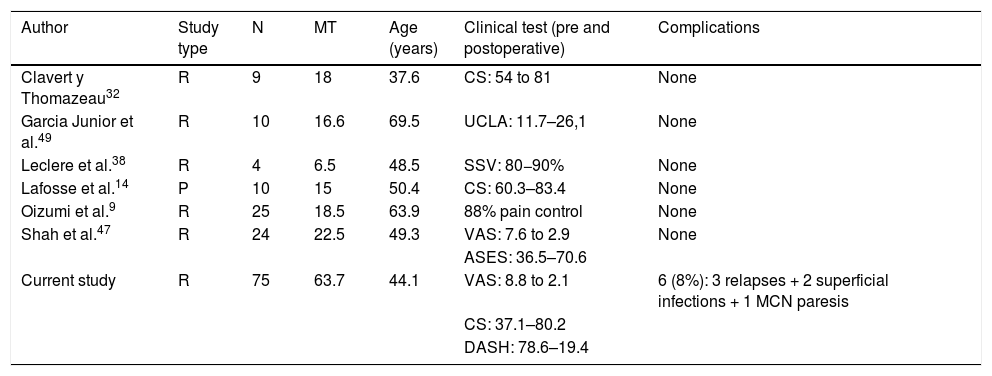
Our study has several limitations. The first is that it was retrospective, which reduces the level of scientific evidence we could extract. The second is that it did not compare 2 types of treatment and we only analysed surgical outcome after conservative treatment had failed. The third is that all operations were performed by surgeons with expertise in shoulders, and this could limit validity for non specialist surgeons. However, the strengths of the study are that mean follow-up was over 5 years and with a number of patients (75) which was very much higher than in almost all related publications.48,49 (Table 1). Also, it eliminated factors of confusion, since it isolated the treatment of isolated proximal and idiopathic compression of the SSN, which is the most frequent, from other associated diseases and above all, from rotator cuff tears or spinoglenoid (distal) cysts. Our study sample comprised neither professional athletes nor people who frequently practised above head sports, which is the most common cause of distal entrapment. In our series this practice was only occasional, as recreation or work-related.
Comparison with published literature.
| Author | Study type | N | MT | Age (years) | Clinical test (pre and postoperative) | Complications |
|---|---|---|---|---|---|---|
| Clavert y Thomazeau32 | R | 9 | 18 | 37.6 | CS: 54 to 81 | None |
| Garcia Junior et al.49 | R | 10 | 16.6 | 69.5 | UCLA: 11.7–26,1 | None |
| Leclere et al.38 | R | 4 | 6.5 | 48.5 | SSV: 80−90% | None |
| Lafosse et al.14 | P | 10 | 15 | 50.4 | CS: 60.3–83.4 | None |
| Oizumi et al.9 | R | 25 | 18.5 | 63.9 | 88% pain control | None |
| Shah et al.47 | R | 24 | 22.5 | 49.3 | VAS: 7.6 to 2.9 | None |
| ASES: 36.5–70.6 | ||||||
| Current study | R | 75 | 63.7 | 44.1 | VAS: 8.8 to 2.1 | 6 (8%): 3 relapses + 2 superficial infections + 1 MCN paresis |
| CS: 37.1–80.2 | ||||||
| DASH: 78.6–19.4 |
All articles have a level of evidence iv. Only studies were included with cases of release of proximal nerve from idiopathic causes, not associated with rotator cuff tear.
ASES: American Shoulder and Elbow Surgeons Shoulder Score; CS: Constant Score; DASH: Disability of the Arm, Shoulder and Hand score; MCN: musculocutaneous nerve; MT: mean time of follow-up (months); N: Number of cases; P: prospective; R: retrospective; SSV: Subjective shoulder value; UCLA: University of California Los Angeles Shoulder Score; VAS: Visual Analogue Scale.
Isolated arthroscopic releases of proximal nerve compression of the SSN after conservative treatment failure obtains satisfactory results in most patients. Despite this improvement, in the medium to long term the patient is rarely asymptomatic, especially when the EMG reveals very severe involvement. This should be explained to the patient when surgery is offered and we should attempt to anticipate this lesion level.
Level of evidenceLevel of evidence iv.
FinancingNo financing was received for conducting this study.
Conflict of interestsThe authors have no conflict of interests to declare.
We would like to thank the Orthopaedic and TraumaUnit of the General University Hospital Los Arcos del Mar Menor.
Thanks also go to the medical specialists who contributed to my training, helping me to develop my critical approach.
Please cite this article as: Cano-Martínez JA, Nicolás-Serrano G, Villodres Corpás J, Bento-Gerard J. Liberación artroscópica del atrapamiento proximal del nervio supraescapular: resultados a medio plazo. Rev Esp Cir Ortop Traumatol. 2021;65:91–98.