Elastofibroma dorsi (ED) is an infrequent benign, slow growing, soft tissue tumour that is usually located in the scapular zone.
Materials and methodsA series of 37 ED patients diagnosed and treated in our hospital between August 1993 and November 2009 were retrospectively reviewed. The average follow-up was 7 years. Ten of them presented bilaterally. The male/female ratio was 4:3, and the mean age was 57 years. An MRI was performed, and the diagnosis confirmed by histopathology. Seven cases were treated conservatively. The clinical results were evaluated using a visual analogue score (VAS) for pain and a comparison of the range of movement during follow-up.
ResultsSome 18% of the patients worked or practiced sports that called for the use of the affected limb. A post-operative transfusion was required by 40% of the patients, due to having a haemoglobin <8g/d. The VAS improved from 6 to 2 after the surgery. The range of movement improved on an average of 40. The complications included an infection, 1 hyperalgesic scar, 8 haematomas and 3 seromas, which were resolved in the follow-up without incidence. All the patients were free of illness after a mean follow-up of 85 months.
ConclusionsGood results were achieved with a long follow-up. Based on these results and a literature review of the current state of this pathology, an algorithm for its diagnosis and treatment is suggested.
El elastofibroma dorsi (ED) es una tumoración benigna infrecuente de partes blandas, crecimiento lento y localización preferentemente escapular.
Material y métodoRevisión retrospectiva de 37 ED diagnosticados y tratados en nuestro centro entre agosto de 1993 y noviembre de 2009, con un seguimiento medio de 7 años. La presentación clínica, los resultados anatomopatológicos y los estudios por imagen han sido revisados. En 10 ocasiones la presentación fue bilateral. El ratio varón/mujer fue (4:23) con una edad media de 57 años. La duración media de los síntomas fue de 14 meses. En todos los casos se realizó estudio de RM y confirmación del diagnóstico mediante anatomía patológica. Siete casos fueron tratados conservadoramente. Los pacientes fueron estudiados por un traumatólogo especialista en oncología, así como por un radiólogo experimentado. Los resultados clínicos fueron evaluados mediante Escala Visual Analógica (EVA) para el dolor y comparación del rango de movilidad durante el seguimiento.
ResultadosNo se halló ningún caso de antecedentes familiares de ED. El 18% de los pacientes realizaban trabajos o deportes que implicaban la extremidad afectada. El 40% de los pacientes requirieron transfusión postoperatoria por hemoglobina < 8 g/dl. La EVA mejoró de 6 preoperatoriamente, a 2 postoperatoriamente. El rango de movilidad mejoró de media en 40°. Las complicaciones incluyen una infección de la herida, un caso de cicatriz hiperálgica, 8 hematomas y 3 seromas posquirúrgicos que se solucionaron sin incidencias en el seguimiento. Tras un seguimiento medio de 85 meses todos los pacientes se encuentran libres de enfermedad.
ConclusionesSe han obtenido buenos resultados con un amplio seguimiento. Basándonos en estos resultados y en una revisión bibliográfica del estado actual de esta patología sugerimos un algoritmo para su diagnóstico y tratamiento.
Elastofibroma was first described in 1961.1 It is a benign and rare connective tissue tumour, with a slow growth. It is known as ED due to its location in the inferior section of the scapula (in 99% of cases), deep within the anterior serratus and latissimus dorsi musculature, and sometimes attached to the periosteum of the ribs. Although its aetiology is still under debate, it is considered that its development may be influenced by continued mechanical friction between the scapula and the ribs and even by a certain genetic component.
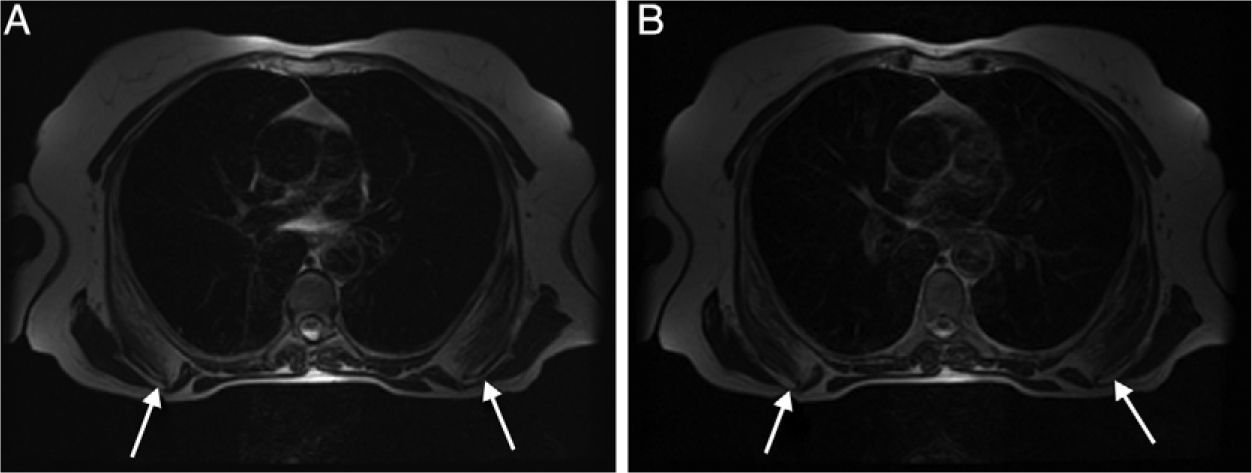
It generally debuts as a tumour, occasionally painful, which appears as an infrascapular soft tissue mass in magnetic resonance imaging (MRI) (Fig. 1). It is predominantly fibrous, with discrete fatty contents, isointense and with no signs of infiltration of the adjacent musculature.2
The purpose of this study is to present the clinical and functional results obtained in the review of our series and to suggest a diagnostic and therapeutic algorithm.
Materials and methodsWe conducted a retrospective study of 37 ED cases (27 patients) diagnosed and treated at our centre between August 1993 and November 2009, with a mean follow-up period of 7 years (range: 17–161 months). The cohort was composed by 23 females (85%) and 4 males (15%), with a mean age of 57 years (range: 42–78 years). Presentation was bilateral in 10 cases whilst in unilateral cases the dominant arm and the contralateral arm were equally affected. All tumours were found in the lower part of the scapula, deep within the serratus anterior muscle, becoming visible for clinical examination by combining flexion and adduction of the affected arm when reaching out to touch the contralateral scapula (Fig. 2).
All patients attended consultation due to the appearance of a mass in the lower edge of the scapula, with pain in 81% of cases, predominantly at night. In turn, 70.3% cases (26 out of 37) presented “spring” scapula.
The duration of symptoms before diagnosis ranged from 3 to 28 months, with a mean value of 14 months. Diagnosis was confirmed by an MRI scan in 89% of cases. Closed “tru-cut” biopsy was performed in 4 cases due to the heterogeneous aspect of the tumour on MRI scans, which forced us to rule out the possibility of a sarcoma. In 7 patients we observed clinical improvement of pain associated with ED, so we conducted regular monitoring. Patients who suffered severe or persistent pain (30 cases) required surgical intervention. The mean hospital stay of patients undergoing surgery was 7.3 days (range: 5–14 days) with a mean duration of postoperative pain of 3.2 days (range: 2–7 days).
Statistical data were obtained during outpatient visits and through medical records. We used a visual analogue scale (VAS) where 0 represented no pain and 10 represented excruciating pain. The range of motion was analysed pre- and postoperatively, especially in posterior flexion (this movement was limited by the presence of the tumour).
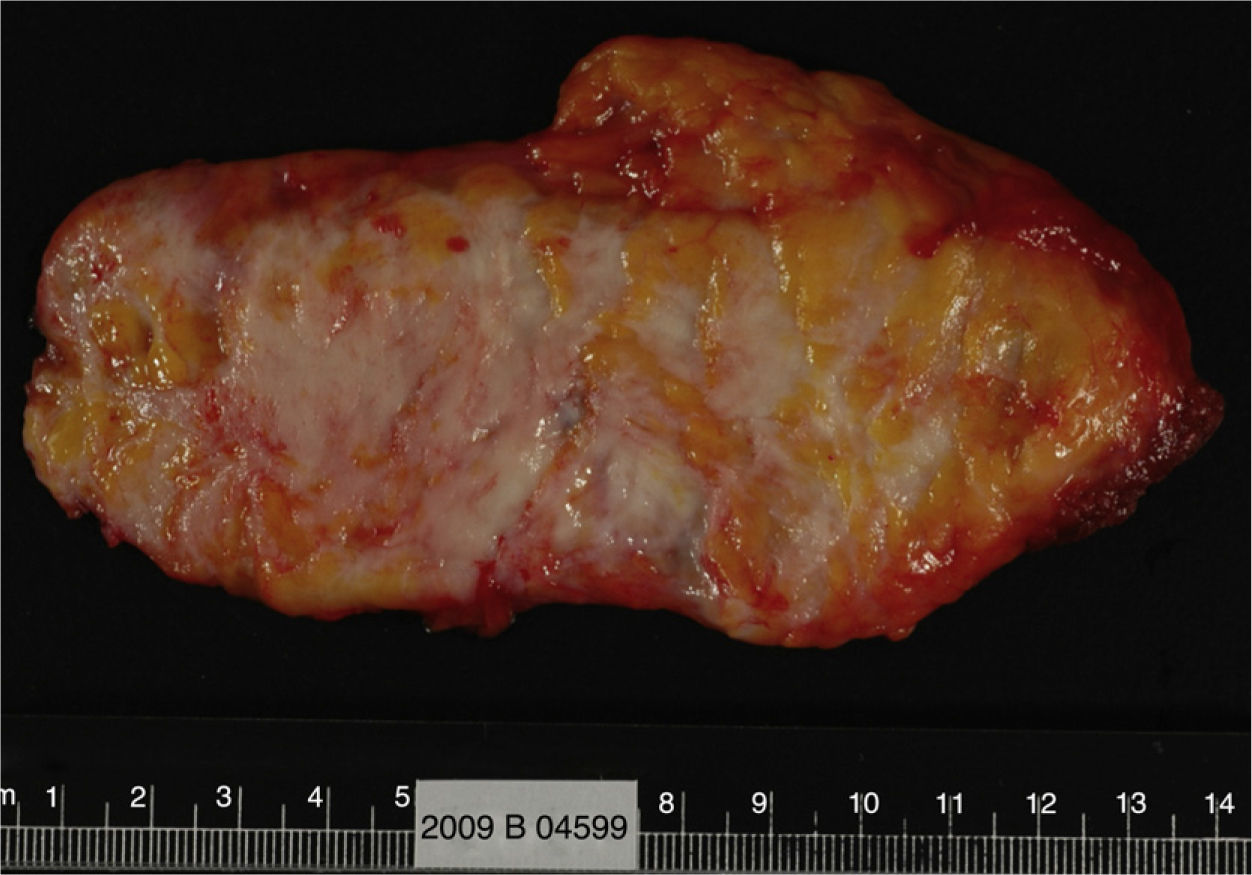
Surgical techniqueWe conducted an oblique approach on the inferior edge of the scapula under general anaesthesia and carried out complete macroscopic resection, adding a small muscle margin in cases of peripheral adhesion. All samples were sent to the anatomical pathology department for histological analysis. Postoperative immobilisation with a sling was maintained for 2 weeks. After this period, patients started assisted and passive exercises of the shoulder and scapula, which then became active movements according to tolerance.
Statistical analysisAll variables were described. We used the number of cases and percentage for categorical variables and the mean and standard deviation for quantitative variables. Reliability statistics were employed throughout the process with a Cronbach alpha greater than 0.95 for all measures. Inference was performed using the Student t test. All tests performed were bilateral. The significance level was the usual 5% (alpha=0.05). The statistical package used in this project was SPSS® v.19 (SPSS® Inc., Chicago, IL, USA).
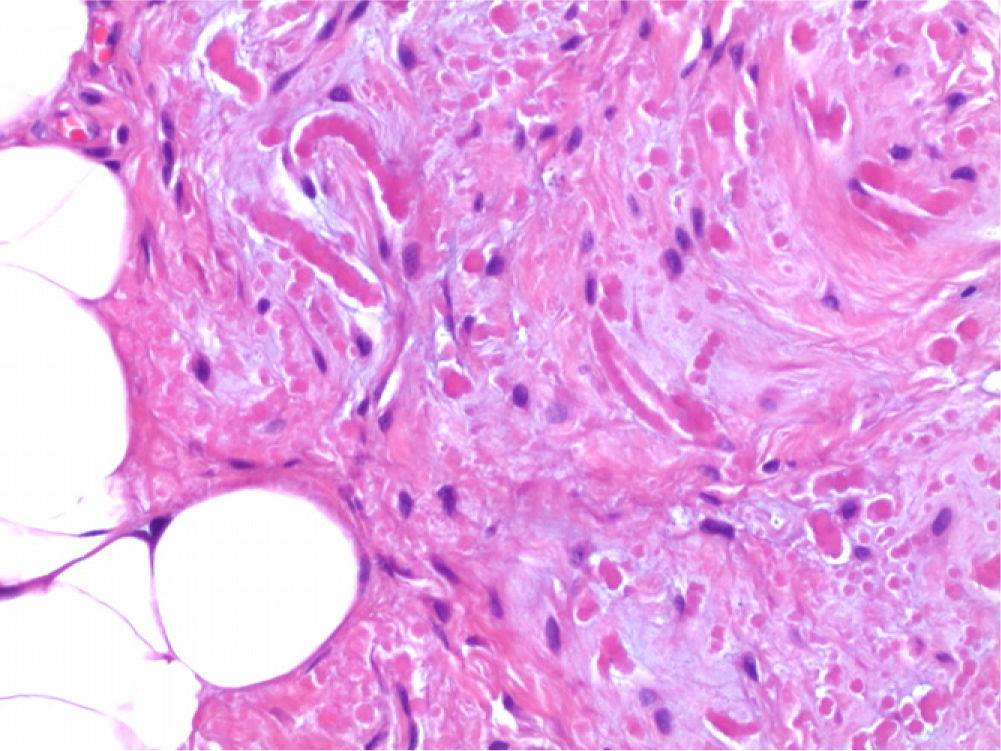
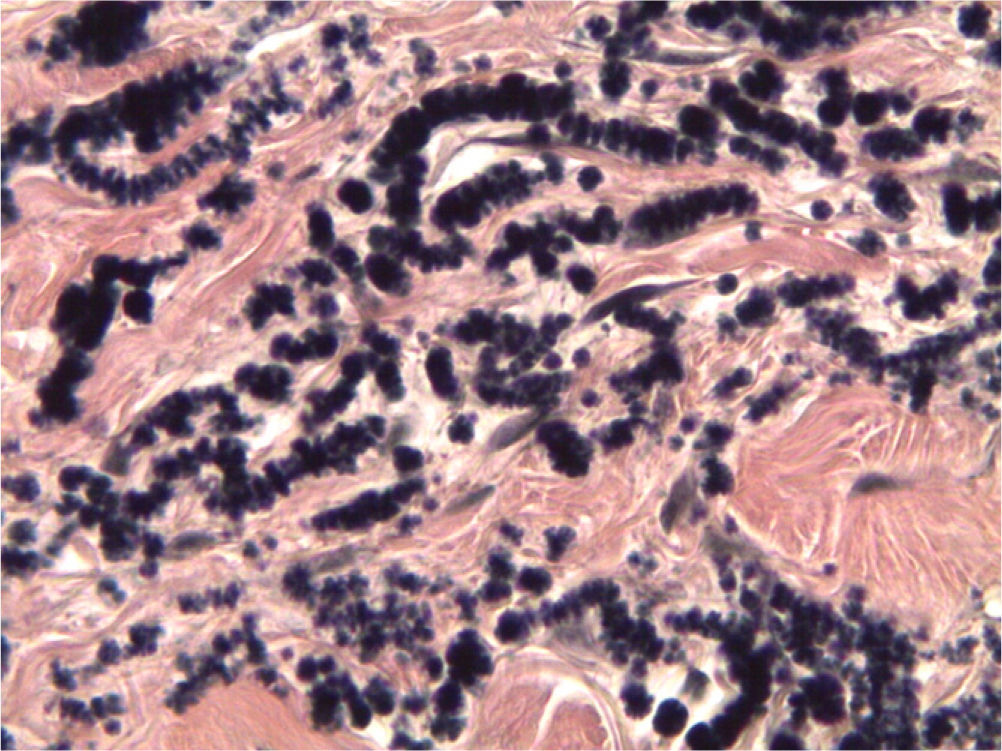
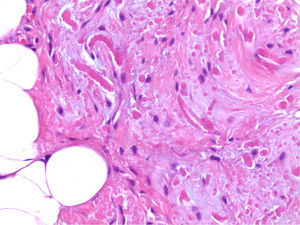
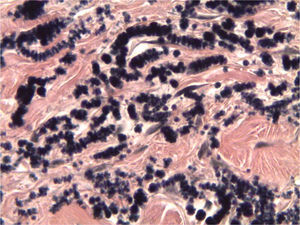
ResultsNone of the patients had a family history of ED. Up to 18% of patients had physically demanding jobs or practiced sports involving the upper body. The pathological study of the resected tumours confirmed the diagnosis of elastofibroma in all cases (Figs. 3–5).
In the clinical assessment of operated patients (30 tumours), the mean preoperative pain measured by VAS was 6 (range: 3–9), decreasing to 2 (range: 0–7) postoperatively (P<.005). When assessing shoulder functionality, shoulder antepulsion improved from a mean preoperative value of 125° (range: 75–170°) to 168° (range: 110–180°) postoperatively (P<.005). Up to 40% of operated patients required a transfusion with a mean of 1.17 packed red blood cells (range: 1–2) due to postoperative haemoglobin <8g/dl.
One case presented infection by Pseudomonas aeruginosa and another case developed a hyperalgesic scar. Both cases were resolved without sequelae during follow-up. Up to 8 cases presented local haematoma and 3 cases presented seromas which were resolved conservatively.
In the 7 cases undergoing regular controls, the mean pain measured by VAS was 5 (range: 2–7) at the time of diagnosis, improving to 2 (range: 0–3) during follow-up.
After a mean follow-up period of 85 months (range: 17–161 months) all patients were symptom-free, with no evidence of relapse. All patients returned to their normal daily activities.
DiscussionThe clinical and functional results obtained were satisfactory, coinciding with those described in the literature. We found no differences regarding percentage and type of complications.3–5
The literature reports an incidence of ED around 2%,4 although this increases in autopsy series, where it stands at 24% in females and 11% in males aged over 55 years.6 It appears predominantly in females between the fifth and seventh decades of life, and is extremely rare in children.4 Our series showed a predominance of females (85%) with a mean age of 57 years. Presentation is frequently bilateral (60%)7,8 with exceptional reports of elastofibromas in the elbows, deltoids, near the ischial tuberosity, inguinal region, feet, orbits, stomach and intraspinal space.9,10 All elastofibromas in our series were located in the scapular region, with a 37% rate of bilaterality, which was significantly lower than that reported in the literature. It is important to conduct MRI scans including both scapulae in order to detect these bilateral cases.
Although elastofibroma may be asymptomatic, it typically appears as a painful mass which can cause stiffness at the level of the shoulders, a scapular “snapping” or simulate a subacromial syndrome. Pain was the predominant clinical sign in our series. Patients presenting tolerable symptoms should be treated through regular controls, reserving surgical excision for those cases where symptoms are severe and limiting.
ED is usually considered as a connective tissue tumour, benign and slow-growing. However, because its pathogenesis is still unknown, some authors consider it as a pseudotumor and others only define it as lesion.11 Histopathologically, some authors suggest that there is degeneration of collagen fibres,4 while others advocate an abnormal fibrillogenesis process.3 Furthermore, a genetic theory has been proposed since the chromosomal regions Xq12-q22 and 19 were identified as possible containers of genes involved in certain tumuors.12 This theory would explain the familial predisposition observed in 32% of ED cases. We did not find any familial cases in our series.
Another theory proposes microtrauma as the origin of elastofibroma, considering that it develops in response to mechanical stress processes and that it does not really present a neoplastic process.3,13,14 In our series, this relationship was found in 18% of cases.
Despite not being pathognomonic, the radiographic appearance of ED in CT and/or MRI scans3,15,16 is so characteristic that it is considered diagnostic and preoperative biopsy is only conducted when there is suspicion of soft tissue sarcoma or in cases where the tumour has grown rapidly within a few months. Some authors advocate a fresh intraoperative biopsy in selected cases.17 Some published series accept ultrasound as a diagnostic method.18 All our cases were studied and diagnosed by MRI and, in the 4 cases in which MRI left open the possibility of underlying soft tissue sarcoma, “tru-cut” biopsy was performed in order to rule out malignancy prior to surgery.
Our study has some limitations. This was a retrospective study with a moderate sample size. The study was not randomised since the symptoms determined the treatment to be followed. Likewise, there was no control group.
We suggest a diagnostic and therapeutic algorithm consisting in suspecting the presence of ED in adults (especially females between the fifth and seventh decades of life) who report pain or mass sensation in the scapulae, with or without stiffness, snapping sound or subacromial syndrome at the shoulder level. Clinically, it is possible to detect a palpable mass in the lower edge of the scapula or infrascapular area when the patient reaches out to touch the contralateral scapula. Diagnostic MRI scans should include both scapulae and “tru-cut” biopsies should be reserved for those cases in which there is suspicion of soft tissue sarcoma or rapid growth within a short period of time. The treatment of choice should be conservative, with periodic clinical controls, although surgical excision should be considered in cases of severe pain or disabling symptoms. The excised specimen should be systematically sent to the anatomical pathology department for its histological study.
Level of evidenceLevel of evidence IV.
Ethical disclosuresProtection of human and animal subjects. The authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of data. The authors declare that no patient data appears in this article.
Right to privacy and informed consent. The authors declare that no patient data appears in this article.
Conflict of interestsThe authors have no conflicts of interest to declare.
Please cite this article as: Abat F, et al. Elastofibroma dorsi: 7 años de seguimiento de 37 casos y revisión de la literatura. Rev Esp Cir Ortop Traumatol. 2012;56:295–300.