Elbow dislocation associated with ipsilateral fracture of the distal radius and a brachial artery injury is an uncommon traumatic entity. The two references of this injury combination appeared in 2015, although both authors did not realise that they were the first two cases published in the medical literature. Although mentioned in the text of the articles, no mention was made of the fracture of the distal radius in the titles.
The purpose of this paper is to present three cases with this new traumatic pathological entity, explaining its pathogenetic mechanism, the treatment used, and the results obtained.
La luxación de codo asociada a fractura ipsilateral del radio distal y lesión de la arteria braquial constituye una patología traumática infrecuente. Las 2 referencias de esta asociación de lesiones aparecieron en 2015, aunque en ambas, los autores no advirtieron que constituían los 2 primeros casos publicados en la literatura médica; incluso en el título de sus artículos, no se hizo mención de la fractura del extremo distal del radio, pero sí en sus textos.
El objeto de este trabajo es dar a conocer 3 casos con esta nueva entidad patológica traumática, explicar su posible mecanismo patogénico, el tratamiento utilizado y los resultados obtenidos.
Elbow dislocation associated with ipsilateral fracture of the distal radius1–5 or with a brachial artery injury on the same side6–47 are very rare conditions of traumatic origin, although they are known and reported in the literature. However, elbow dislocation with ipsilateral fracture of the distal radius associated with a brachial artery injury on the same side is a new entity. The only two references of this injury combination appeared in 2015, although both authors did not realise that they were the first two cases to be published in the medical literature. Although mentioned in the text of the articles, no mention was made of the fracture of the distal radius in the titles.48,49
The purpose of this paper is to present three cases with this new traumatic pathological entity, explaining its pathogenetic mechanism, the treatment used, and the outcomes obtained.
Material and methodDuring the period between January 2007 and December 2015, 3 cases of elbow dislocation with ipsilateral fracture of the distal radius associated with a brachial artery injury on the same side were diagnosed and treated in our Orthopaedic and Trauma Surgery Service, corresponding to 1.8% of all simple and complex elbow dislocations which we have attended to throughout these last 8 years.
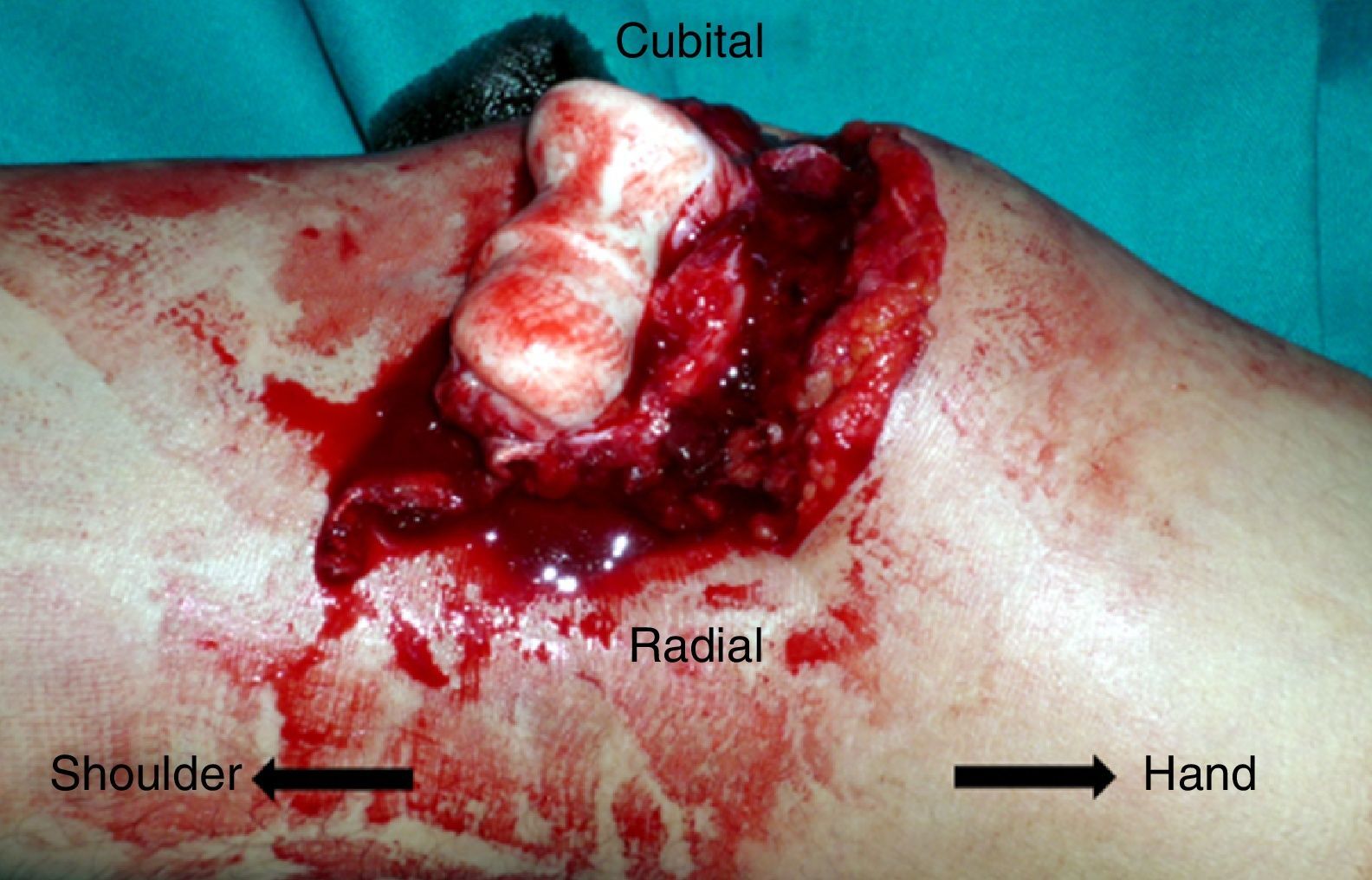
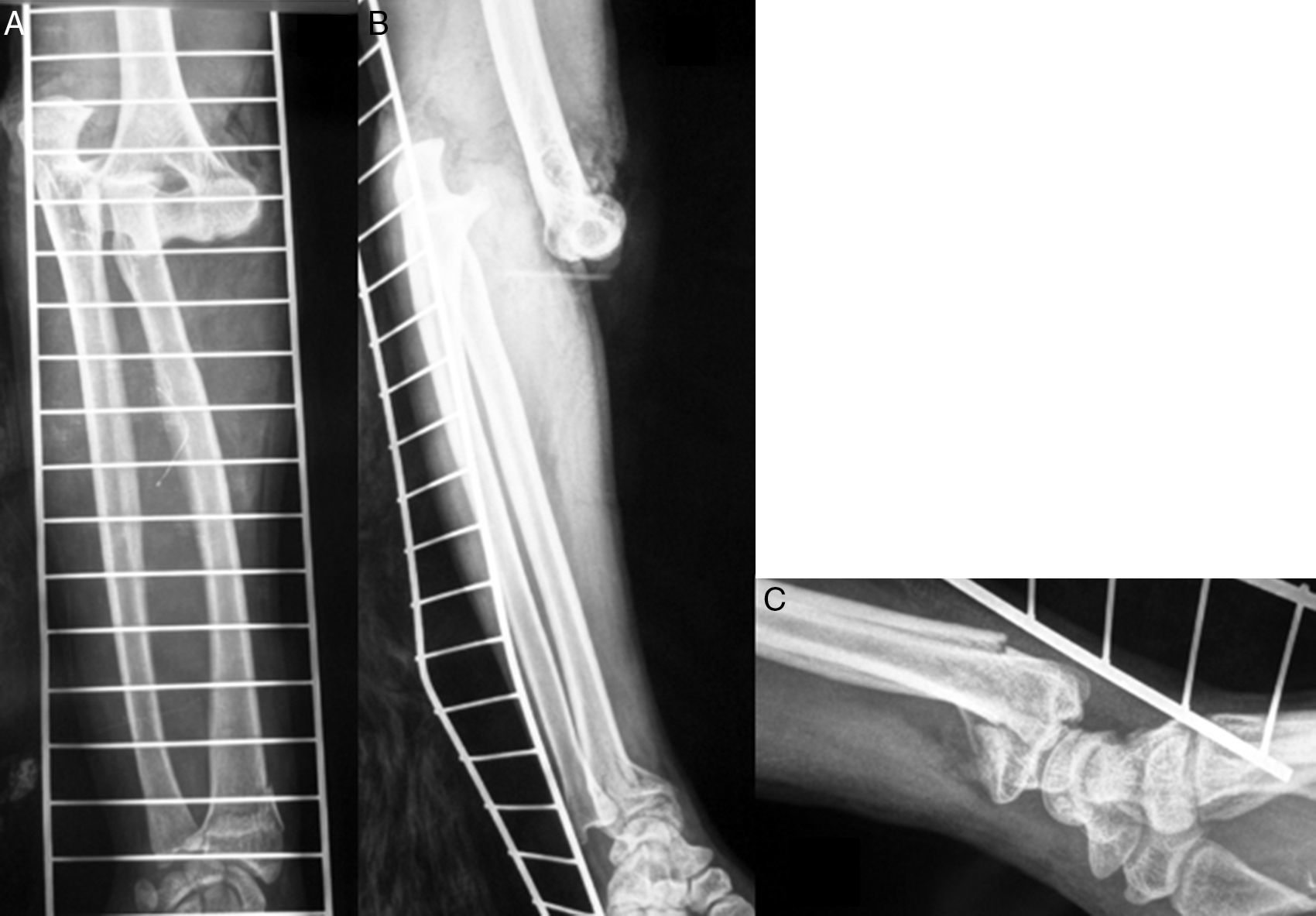
Case 1Male, 36 years of age, who had an accidental fall from a height of 2 metres, supporting the palm of his left hand against the ground. On admittance, a bruised injury was observed at ante-ulnar fossa level from where the distal end of the radius protruded (Fig. 1). The ipsilateral wrist had also been deformed. Physical examination revealed the absence of a radial pulse, but sensitivity had been maintained. An X-ray showed posterior elbow dislocation and a type A2 (AO classification) fracture of the distal radius (Fig. 2). After reduction of dislocation under general anaesthetic, an examination of the vascular injury was made, which showed complete transection of the brachial artery, proximally to its bifurcation into radial and ulnar arteries, respectively. After controlling bleeding, by using vessel loops, the collateral ligaments of the elbow were reinserted and the artery was repaired by means of an autogenous reversed saphenous vein bypass. Finally, closed faciotomy of the anterior compartment of the forearm was performed. Given that the elbow had good stability after reduction, it was immobilised with a brachial-ante-brachial dorsal plaster cast. One week later and after confirming correct perfusion of the extremity, with preventative ischaemia, we proceeded to carry out open reduction and internal fixation (ORIF) of the distal radius fracture with volar plating. Two weeks after this secondary surgery the cast was removed and a rehabilitation programme was pursued, assisted by a physiotherapist.
Six months following intervention, the patient was free from pain and had complete movement of elbow and wrist. Two years later, as a consequence of hospital admittance for pneumonia, the extremity was reassessed, confirming excellent clinical evolution, that it was pain free and the patient was able to carry out active unrestricted working and sports activities.
Case 2Male aged 35 who had suffered an accident at work, with his right forearm being trapped in a roller press. On admittance to the emergencies department his elbow and ipsilateral wrist were severely deformed and he also presented with major inflammation of the forearm. Physical examination revealed the absence of radial and ulnar distal pulses, and hypoesthesia of the thumb and index finger. An X-ray showed the presence of posterior dislocation of the elbow with a Morrey type II coronoid process fracture and a type A2 (AO classification) fracture of the distal radius on the same side (Fig. 3).
Closed reduction of dislocation under general anaesthetic was performed, but due to major instability, an external fixator was fitted. Intraoperative Doppler ultrasound revealed the presence of a complete transection of the brachial artery, and we therefore proceeded with a surgical approach to repair it using direct end-to-end sutures. The distal radius fracture was initially treated with manual reduction and percutaneous synthesis with Kirschner needles (Fig. 4). At the end of the procedure, open fasciotomy was performed of the anterior compartment of the forearm, macroscopically confirming integrity of the median nerve. No sutures were performed on the wounds at this stage. During the postoperative period, the patient's pulses were recovered but initially not the sensitivity in the affected fingers. After 2 weeks, skin defects of the surgical wounds were covered with free skin flaps and after 4 weeks, as soon as the fixator had been removed and on observing that the distal radius fracture was not yet showing signs of consolidation, ORIF was practised on it with volar plating, not without some difficulty. The electromyographic study (EMG) performed 2 weeks after this surgery revealed the existence of a median nerve neuropraxia at forearm middle third level. Three months later, due to the persistence of elbow instability, now no longer with the external fixator, plasty of both collateral ligaments was performed with circumferential allograft.50 After 3 weeks immobilisation assisted physiotherapy was initiated. Eight months later, the patient was pain free, with an elbow movement range of 40° de-extension and 100° flexion, whilst that of his wrist had a range of 50° extension and 60° flexion. Both pronation and supination were limited to 60°. One year after the trauma, skin z-plasties were performed at the retractile scar level of the elbow flexura, achieving extension of up to 20°. However, both flexion and pronosupination remained unalterable, as did the hypoesthesia of the fingers. As the patient had no pain, he declined a further intervention to gain better elbow flexion.
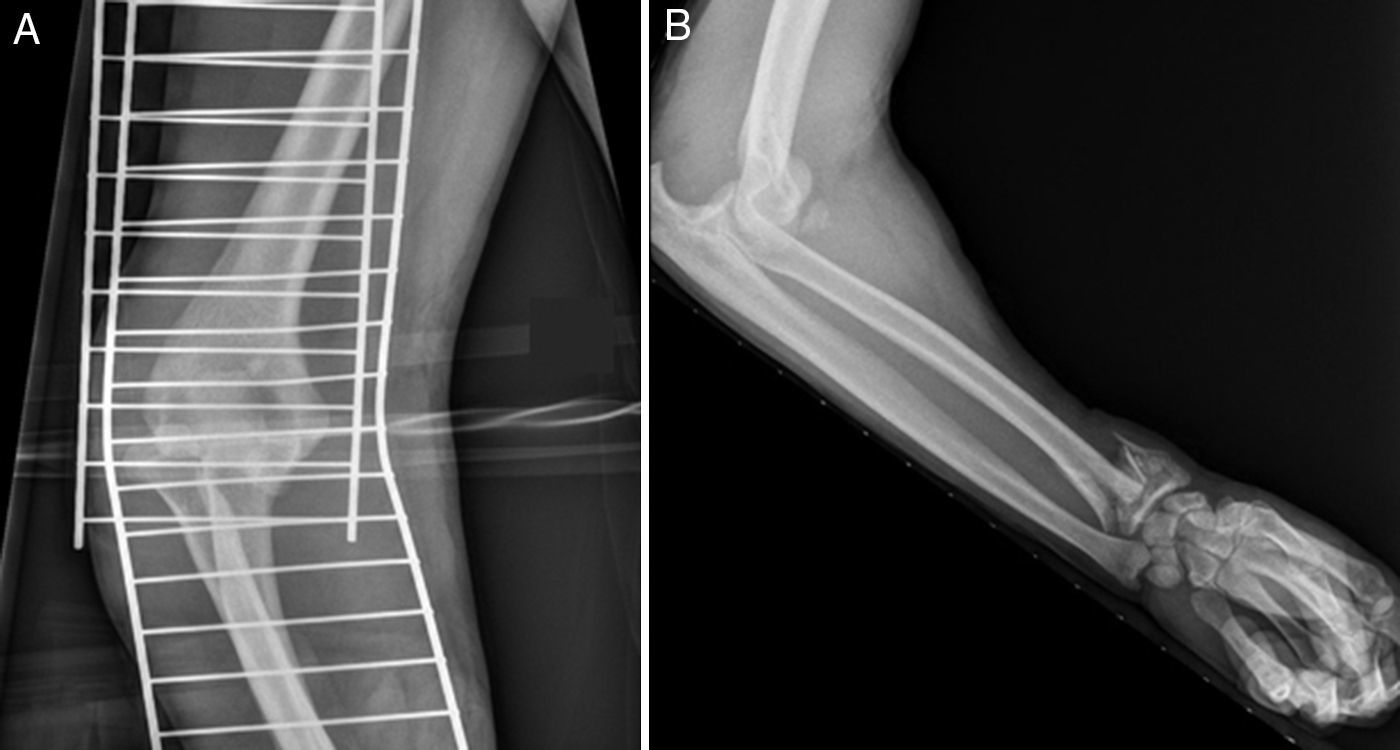
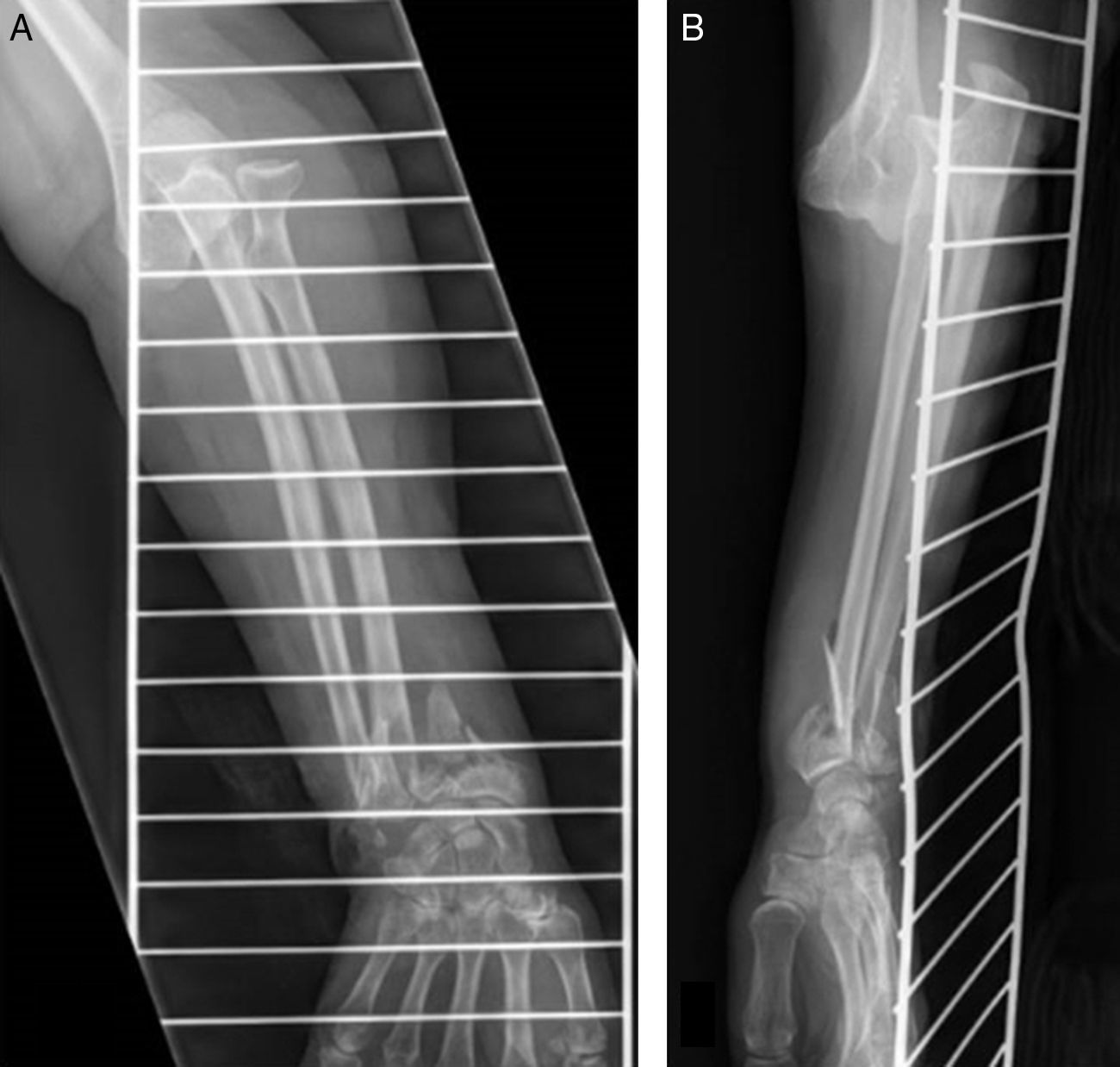
Case 3Female aged 76 who had suffered from a casual fall down the stairs in her home. On admittance to the emergency department, major deformity of both elbow and wrist at the upper right extremity was observed. Physical examination revealed a lack of radial pulse and Doppler ultrasound revealed a lack of blood flow and clear signs of ischaemia in the fingers (Fig. 5). Sensitivity had been preserved, however. An X-ray showed posterior dislocation of the elbow and a C2 (AO classification) displacement fracture of the distal radius (Fig. 6).
Closed reduction technique of the dislocation was performed under general anaesthetic, which was easily achieved by manipulation. Her pulse was recuperated immediately afterwards, with reappearance of continuous blood flow and the disappearances of signs of ischaemia from the fingers. No further studies were performed as a result of this early and satisfactory clinical evolution.
72h later the well perfused limb was confirmed, and surgical intervention was performed on the wrist. ORIF of the distal radius with volar plating was performed using preventative ischaemia and pneumatic sleeve. Six months later, the patient was pain free and had complete movement in her elbow and wrist, and was able to return to her daily activities with no restrictions.
DiscussionElbow dislocations are classified as simple when they are not accompanied by associated fractures, and complex when they are accompanied by fractures, such as those of the radial head, the coronoid process and/or humeral condyle.51 However, either a simple dislocation or a complex one may also be associated with a distal radius fracture or a brachial artery injury of the same side. These are injuries which, although infrequent, have been published in the medical literature. Nevertheless, the simultaneity of an elbow dislocation with ipsilateral fracture of the distal radius, associated with a brachial artery injury is a unique pathological trauma entity, even though this was not acknowledged as such by its authors when they published the first and only 2 cases in 2015.48,49
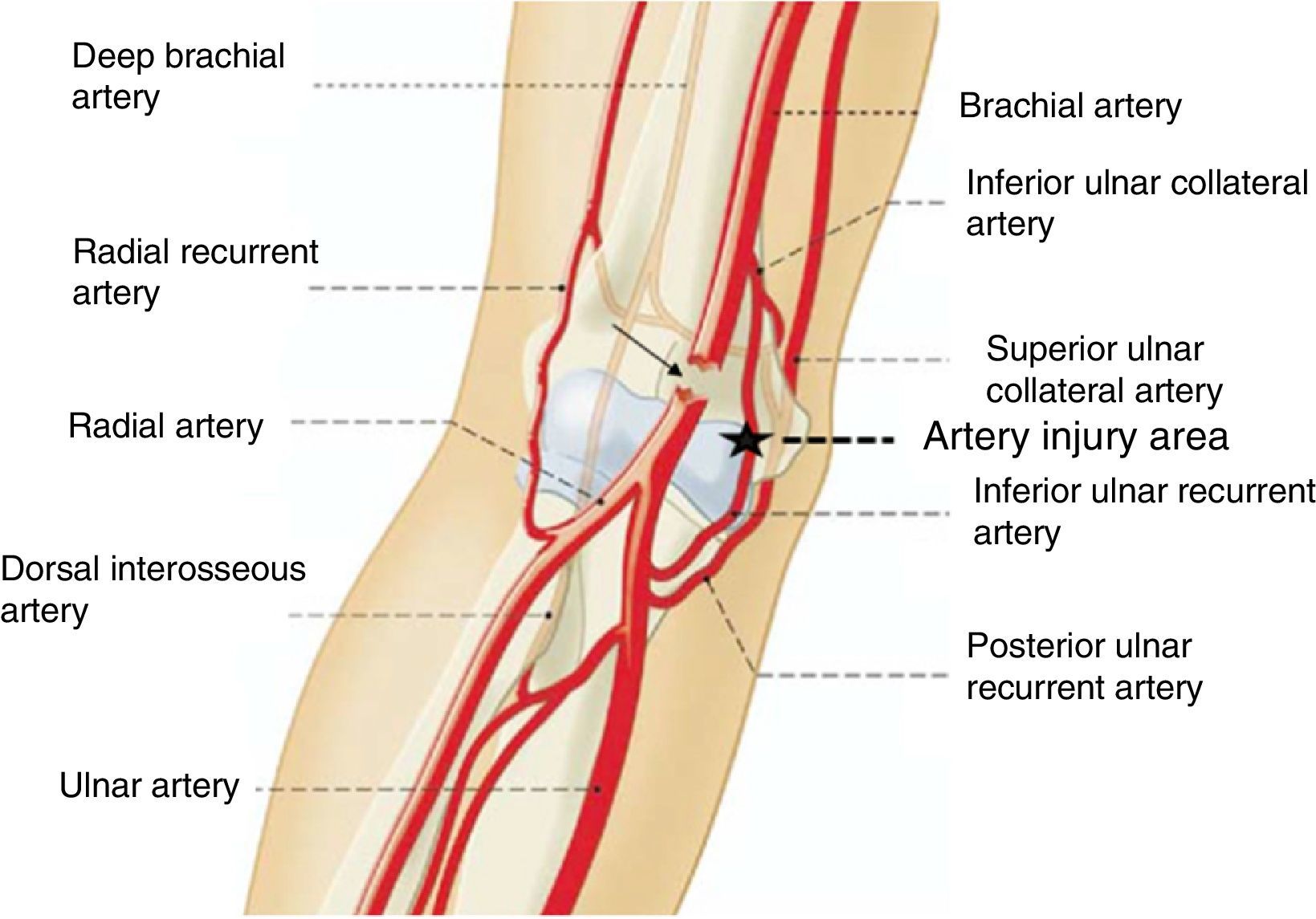
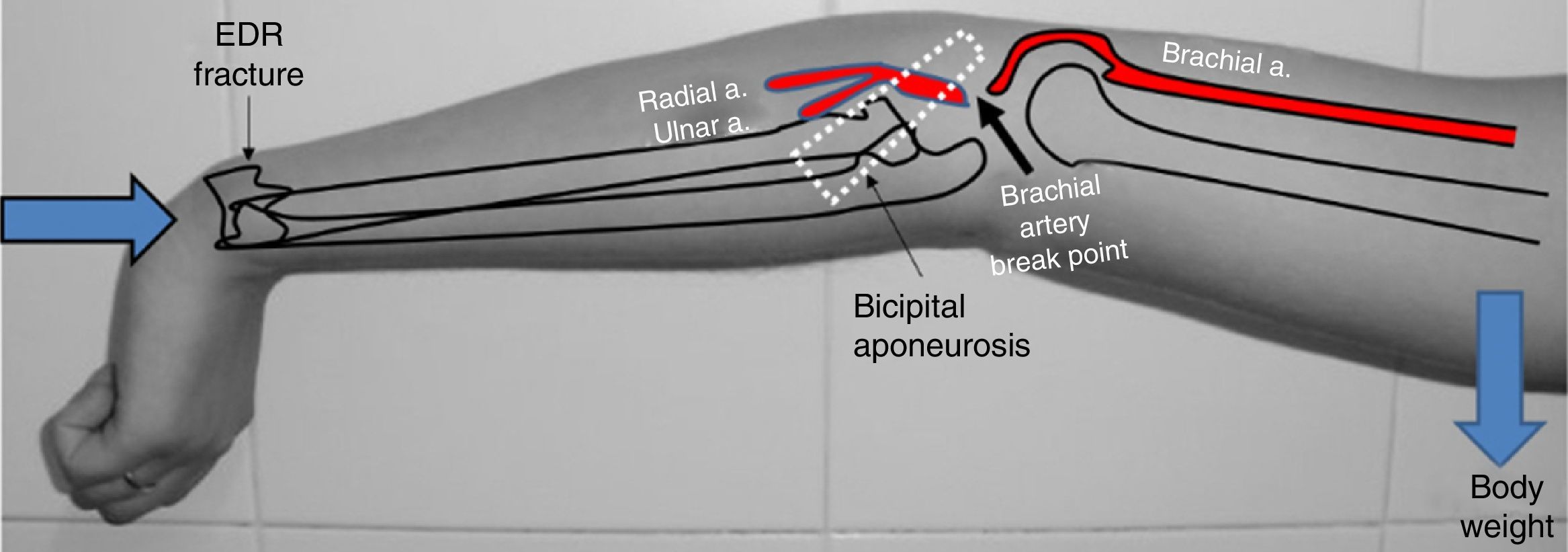
The true pathogenic mechanism of this complex injury is unknown, although post mortem anatomical studies have confirmed that after elbow dislocation by forced hyperextension mechanisms, there is almost always anastomotic rupture between the lower median collateral artery and the anterior ulnar recurrent artery17 (Fig. 7). If a force of these characteristics is thus able to cause this anastomotic rupture, a similar but superior force to the anterior one and maintained over time, may very well be the cause of the injury to the brachial artery. However, to explain both the dislocation of the elbow associated with the brachial artery injury, and the distal radius fracture, we consider that the initial force and cause of the radial fracture would be compression along the longitudinal axis of the extremity, when the patient supported the palm of her hand on the floor on falling. Later, this force would be transformed into another on hyper-extension at elbow level, which would be responsible for the simultaneity of the dislocation and of the brachial artery injury respectively. In the great majority of cases of elbow dislocation associated with brachial artery injury, the latter is located below the bicipital aponeurosis, before the bifurcation into radial and ulnar arteries, respectively,6 which is why we believe that the bicipital aponeurosis (lacertus fibrosus) would act like a bezel over the brachial artery when trapped between the aponeurosis and the distal humerus in its anterior displacement, leading to vasospasm and/or transection (Fig. 8).
This mechanism could explain the injuries in 2 of our patients (cases 1 and 3), but not in the patient who trapped his arm in a roller press (case 2). Despite this, we believe that the pathogenic mechanism was very similar at elbow level, though not at wrist level. The distal radius fracture was thus caused by pure flattening and not by compression. However, the elbow dislocation and injury associated with the brachial artery came about through hyperextension when the forearm was trapped between the rollers, an area which served as a fulcrum where the arm and elbow articulation were hyper-extended by the weight of the body of the person falling to the ground.
The first described case of simple dislocation of the elbow associated with brachial artery injury was reported in 1913.18 Since then, approximately 50 cases have been published, the majority of them open,6 as was one of our cases. The common denominator in all of them was the lack of radial pulse16 although this does not ensure the existence of a brachial artery transection, since several cases described were due to vasospasm, as occurred in case 3 of the ones we presented. Indeed, cases of complete injury of the brachial artery have been described, but with the presence of a radial pulse.9 For this reason we recommend examination with the Doppler ultrasound, both prior to treatment and after dislocation reduction.6 If pulse is recuperated after reduction and a Doppler ultrasound confirms continuity of blood flow, the absence of any permanent vascular damage may be confirmed. In contrast, if pulse is not recuperated and the Doppler ultrasound does not detect blood flow continuity, it may be assumed that a complete artery lesion exists, and surgical examination of the same and its repair will be necessary. If no Doppler ultrasound is available, pulse oximetry – the non-invasive measurement of oxygen transported by haemoglobin on the inside of blood vessels – may be a very useful tool for examination and easy access to determine the existence of vascular damage.13 However, if in doubt, the diagnostic test par excellence is angiography or CT angiography which offers a precise confirmation of the injury and its level.
According to the literature, compromise of nerve trunks is more infrequent than that of vascular trunks.52–55 In fact, articles in this regard refer to isolated cases, with any nerve able to be implicated (median, ulnar, radial). The pathogenesis of the nerve injury would be the same as that which took place for the arterial injury, i.e. a hyper-extension with rupture or elongation of the nerve, although the standard occurrence would be a neuropraxia, as occurred in case 2, with compromise of the median nerve. However, in this case, the injury was not caused by elongation but by compression at forearm level, from it being entrapped in the press. Whatever the cause, the prognosis of these neuropraxias is usually good, although there are cases where the patient has had permanent hypoesthesia, as occurred with our patient.
Treatment of this complete lesion is conditioned by vascular damage. Expedient treatment reduces morbidity. The surgical team must include a trauma surgeon and a vascular surgeon. Firstly the dislocation must be reduced and stabilised. If it is unstable, the fitting of an external fixator is recommended with the elbow at straight angle. This procedure will lead to the control of both the perfusion of the extremity after vascular repair and also the clinical course of surgical wounds. Treatment of the damaged ligaments is optional, although we would recommend reinsertion. Once joint stability has been achieved, the arterial injury is treated. Even though there are published cases where ligation of the brachial artery was performed, arguing that there was sufficient collateral circulation for good perfusion of the extremity, we believe that this is not justified as the risk of secondary thrombosis of collateral arteries, of experiencing ischaemia on exercising, of chronic compartmental syndrome and intolerance to cold is very high. As a result of this, we believe in repair, whether this be through end-to-end sutures,18 in the case of the arterial section being simple, or by means of a bypass with inverted saphenous vein, if there is a loss of substance or because they should resection the lesioned vascular ends.6 Moreover, and after vascular repair, we recommend fasciotomy of the anterior compartment of the forearm to prevent the appearance of a post-perfusion compartmental syndrome. However, we believe that this surgery is not necessary in cases of vasospasm, in which after dislocation reduction the radial pulse is recuperated and the Doppler ultrasound confirms the organic integrity of the brachial artery. With regards to the treatment of the distal radius fracture, we believe it must be essentially surgical as there is usually a pattern of unstable fracture. In this respect, volar plating is the most appropriate osteosynthesis. However, it is not necessary to perform this surgery as emergency surgery. It is actually advisable to delay it for several days to confirm whether the limb is well perfused and also to minimise the appearance of compartment syndrome. With regard to this aspect, it has been observed that 15% of patients with diverse elbow injuries, together with ipsilateral fracture of the distal radius, develop compartment syndrome if they undergo surgical intervention simultaneously.56
Lastly, regarding complications, these will depend on whether good vascular repair has been achieved, and whether there is damage of the attributes governing the elbow joint, be they soft as well as bony. If dislocation is simple, no serious complications will be expected. On the contrary, if dislocation is complex, it would be normal to observe joint stiffness of greater or lesser severity, as occurred in our case 2.
The study of these 3 cases has led us to the following conclusions:
- 1)
Examination of radial pulse and the sensitivity of the fingers is essential in all elbow dislocation, whether it be simple or complex.
- 2)
When there is no radial pulse, examination of the vascular status using Doppler ultrasound or pulsioximetry is essential, both before and after dislocation reduction. If there is any doubt, it is advisable to perform an angiography or CT angiography.
- 3)
In all elbow dislocation associated with distal radius fracture a brachial artery injury on the same side should always be suspected, as there is high probability of it presenting. Lack of diagnosis could have serious consequences.
- 4)
The lack of sensitivity in the fingers is generally a neuropraxia. However, we recommend carrying out an EMG 3 weeks after the lesion to confirm the degree of nerve injury and to be able to act as a consequence of this.
- 5)
Treatment is always urgent and surgical. Firstly, the dislocation must always be reduced. If articulation is stable, no surgical stabilisation of any type is necessary. In contrast, if articulation is unstable, it is advisable to fit an external fixator and reinsert the collateral ligaments. Immediately afterwards, the brachial artery may be repaired. The treatment of the distal radius fracture should be delayed several days to confirm the perfect perfusion of the extremity and also minimise the risk of compartment syndrome. We believe ORIF with volar plating is the best option.
- 6)
Fasciotomy of the anterior compartment of the forearm may be an additional advisable surgical procedure to prevent the appearance of a post-perfusion compartment syndrome. However, this surgery is not necessary in cases of vasospasm, where after dislocation reduction radial pulse was rapidly recuperated and the Doppler ultrasound examination confirmed organic integrity of the brachial artery. In these cases, and provided that articulation is stable after reduction, immobilisation with brachial-ante-brachial dorsal plaster cast and its ensuing management is sufficient.
Level of evidence IV.
Ethical responsibilitiesProtection of human and animal subjectsThe authors declare that for this research no experiments on human beings or animals have been conducted.
Confidentiality of dataThe authors declare they have adhered to the protocols of their centre of work on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of interestThe authors have no conflicts of interests to declare.
Please cite this article as: Trigo Lahoz L, Lamas Gomez C, Sarasquete Reiriz J, de Caso Rodriguez J, Proubasta Renart I. Luxación de codo con fractura ipsilateral del extremo distal del radio asociada a lesión de la arteria braquial. Una nueva entidad patológica de origen traumático. Rev Esp Cir Ortop Traumatol. 2017;61:146–153.