To identify the factors with influence on the development of avascular necrosis of the femoral head (ANFH) in patients with non-displaced femoral neck fractures treated with internal fixation.
Material and methodRetrospective study of cases and controls. We included non-displaced femoral neck fractures treated with internal fixation, and that presented ANFH with a postoperative follow-up of at least 2 years. The baseline variables, active comorbidities of the patients, the time for surgery and the number of screws used for osteosynthesis were recorded. Comparisons were made between the groups, those that presented ANFH and those that did not. By area under the curve, the cut-offs of age and time for surgery were located.
ResultsAn association between sex, active comorbidities and number of screws used and the development of ANFH was not observed. The cut-off points for age and time for surgery were ≤69 years and ≤43h, respectively. No significant correlation was observed for the cut-off time for surgery. In the multivariate analysis, age ≤69 years was a significant predictor of the development of ANFH (OR 4.6; 95% CI 1.1–17.9; P=.028).
ConclusionsThe patients aged 69 years or younger were at increased risk of developing ANFH after undisplaced femoral neck fracture treated with percutaneous screws.
Identificar los factores con influencia sobre la aparición de necrosis avascular de cabeza femoral (NACF) en pacientes con fracturas del cuello femoral no desplazadas tratadas con fijación interna.
Material y métodoEstudio retrospectivo de casos y controles. Se incluyeron las fracturas de cuello femoral no desplazada, tratadas con fijación interna, y que presentaron NACF tras un seguimiento postoperatorio de al menos 2 años. Se registraron las variables basales, las comorbilidades activas de los pacientes, así como el tiempo para la cirugía y el número de tornillos utilizados para la osteosíntesis. Se realizaron comparaciones entre los grupos, aquellos que presentaron NACF y los que no. Mediante el área bajo la curva se localizaron los puntos de corte de las variables edad y tiempo para la cirugía.
ResultadosNo encontramos asociación entre el sexo, las comorbilidades activas y el número de tornillos utilizados y el desarrollo de NACF. Los puntos de corte para la edad y el tiempo para la cirugía fueron≤69 años y≤43h, respectivamente. No encontramos asociación estadísticamente significativa para el punto de corte del tiempo para la cirugía. En el análisis multivariante, la edad≤69 años fue un predictor significativo de desarrollo de NACF (OR 4,6; IC 95% 1,1-17,9; p=0,028).
ConclusionesLos pacientes con una edad igual o menor de 69 años presentaban un mayor riesgo de desarrollar NACF tras fractura no desplazada del cuello femoral tratada con fijación percutánea atornillada.
Undisplaced femoral neck fractures (Garden stages I–II) are relatively rare.1 In fractures of the femoral neck, the retinacular vessels of the circumflex arteries that supply the femoral head can be affected; the femoral head consequently suffers a variable period of ischaemia that can lead to its necrosis.2 The rate of avascular necrosis of the femoral head (ANFH) in undisplaced fractures treated with internal fixation is relatively low, between 1% and 5% in the majority of the studies published in the last decade.1,3 However, the development of ANFH is still a challenge for both the patient and the surgeon, as it involves a high rate of reoperation. The most widely used treatment in these undisplaced fractures is internal fixation, whose objective is stabilising the fracture and protecting the vascularisation of the femoral head.1
For displaced fractures treated with internal fixation, various risk factors for ANFH have been described, such as age, sex, degree of displacement and fracture pattern, length of time between injury and surgery, method of internal fixation, quality of the reduction and time of load commencement.4–6 However, the findings in those studies are generally the subject of debates. The meta-analyses and systematic revisions published2,7 have been unable to establish clear conclusions about the factors predisposing to ANFH.
The limited number of studies on risk factors for ANFH in undisplaced fractures is also notable. Some make reference to an associated factor or so,3,8 but those findings are circumstantial because the studies do not focus on ANFH; their priorities are the results of various treatments and their rate of general complications.9,10 This is probably a result of the low prevalence of ANFH in undisplaced fractures, given that most of the studies are retrospective, have series of fewer than 100 undisplaced fractures and feature extensive heterogeneity of patients, ages, surgical methods and follow-up periods. As far as we know, there are no studies that comprehensively analyse the risk factors of ANFH in undisplaced fractures. Consequently, there is a lack of evidence with respect to the potential causes of ANFH in undisplaced fractures.
The main objective of this study was to identify the factors that influence the development of ANFH in patients with undisplaced fractures of the femoral neck treated with internal fixation.
Material and methodsThis was a retrospective study of cases and controls that was approved by our institutional ethics committee. No informed consent was required as it was considered assessment of clinical practice. From the database of our service, the consecutive patients treated between 2005 and 2015 with the following inclusion criteria were identified: undisplaced femoral neck fracture, treated with internal fixation, and presenting ANFH after a postoperative follow-up of at least 2 years. To adapt the study to standard practice, the only criterion for exclusion was pathological fracture due to a tumour. The indication for internal fixation was undisplaced femoral neck fracture (Garden stages I–II).11 Internal fixation was not performed in stage III–IV fractures.
Of the 140 patients identified as fulfilling the criteria, 16 were excluded for demise, 1 for failure of the internal fixation and 2 for pseudarthrosis (all occurring before 2 postoperative years). None of these patients presented radiographic signs of ANFH in the last evaluation performed. Consequently, the study sample consisted of 121 patients, of whom 12 developed ANFH (study group) and 109 did not (control group).
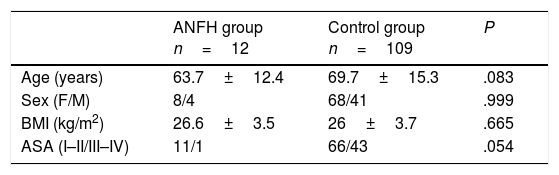
The basal characteristics of both groups are presented in Table 1. In the ANFH group (study group), there were 8 women and 4 men, with a mean age of 63.7 years (range, 44–83). In the control group, there were 68 women and 41 men, with a mean age of 69.7 (range, 18–93). There were no statistically significant differences between the 2 groups (Table 1).
Basal patient characteristics.
| ANFH group n=12 | Control group n=109 | P | |
|---|---|---|---|
| Age (years) | 63.7±12.4 | 69.7±15.3 | .083 |
| Sex (F/M) | 8/4 | 68/41 | .999 |
| BMI (kg/m2) | 26.6±3.5 | 26±3.7 | .665 |
| ASA (I–II/III–IV) | 11/1 | 66/43 | .054 |
Quantitative variables: mean±standard deviation.
ANFH, avascular necrosis of the femoral head; ASA, American Society of Anesthesiologists; BMI, body mass index; F, female; M, male.
All the operations were performed under spinal anaesthesia. The patient was placed on a traction table. The fracture was given fixation in situ, without previous reduction. The surgical approach was percutaneous using lateral pathway. For the internal fixation of all the fractures, 2–3 partially threaded cannulated titanium screws with a diameter of 6.5mm (Asnis™ III, Stryker Trauma, Switzerland) were used. All patients had antibiotic and antithrombotic prophylaxis. The standard procedure was authorisation of sitting at 24h postoperatively and load-bearing at 6 weeks, after radiographic control.
Follow-up and assessmentPre- and postoperative radiological and clinical data for each patient were gathered from the case histories, which all contained the relevant data. All patients had been clinically assessed upon admission. Recorded details included active comorbidities and the factors described in the literature12 as having potential impact on the development of ANFH, including alcoholism, active tobacco use and corticosteroid treatment. Postoperatively, the patients with hip fracture were assessed in a standardised manner at 1, 3, 6 and 12 months, and then annually for at least 2 years. Time until surgery was defined as the hours elapsed since the traumatism.
Radiographic assessment was based on anteroposterior and lateral hip projections. Fracture displacement was classified in agreement with Garden,11 categorising stages I–II as undisplaced. Simple X-rays were used for diagnosing ANFH, defined as any sign of necrosis from Steinberg stage II on.13 Given that the necrosis was seen radiographically, no bone gammagraphy or magnetic resonance was required to diagnose ANFH. Osteosynthesis failure included secondary displacement of the fracture, dismounting of the fixation system, intra-articular protrusion or screw breakage. Pseudarthrosis was considered if, after 6 months, there was no radiographic evidence of consolidation, understood to be bone bridging across at least 3 of 4 cortices in orthogonal projections.
Statistical analysisStatistical analysis was performed using the SPSS v.22 and MedCalc v.13 program. To evaluate the quantitative variables, the Mann–Whitney U test was used, after analysis of normality using the Kolmogorov–Smirnov test. Association between qualitative variables was evaluated using Fisher's exact test.
To establish the best cut-off point for age and time until surgery with influence on ANFH development, the coordinates of the area under the curve were used, with the Youden index representing the best relationship between sensitivity and specificity.
The influence of dependent variables on ANFH development was assessed using multivariate logistic regression analysis with backward stepwise method with the cut-off point to eliminate P>.10; the data was expressed as odds ratio with 95% confidence interval. In all tests, the level of statistical significance was set to P (bilateral) <.05.
ResultsMean postoperative follow-up in the ANFH group was 76.2±31.6 months and in the control group, 52.6±25.1 months. The difference was statistically significant (P=.011) due to the follow-up after prosthesis reoperation carried out in all the patients in the ANFH group.
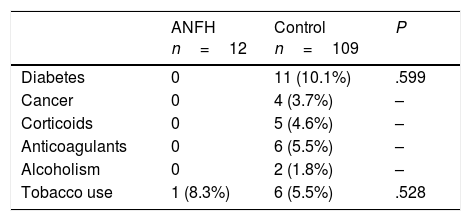
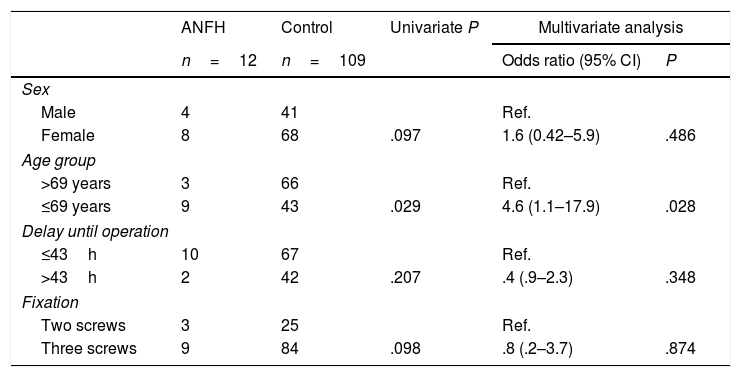
The diagnosis of ANFH was reached at a mean period of 19.7 months (range, 1.1 a 57.7). In the first year of postoperative follow-up, there were 2 cases (16.6%); in the second year, 8 (66.6%); and 2 (16.6%) after 3 or more years. There were no statistically significant differences between the 2 groups in relation to comorbidities or other health factors (Table 2). In the univariate analysis (Table 3), no statistically significant differences were found in sex (P=.097) or the use of 2 or 3 screws (P=.098).
Multivariate analysis for factors predictive of avascular necrosis of the femoral head (ANFH).
| ANFH | Control | Univariate P | Multivariate analysis | ||
|---|---|---|---|---|---|
| n=12 | n=109 | Odds ratio (95% CI) | P | ||
| Sex | |||||
| Male | 4 | 41 | Ref. | ||
| Female | 8 | 68 | .097 | 1.6 (0.42–5.9) | .486 |
| Age group | |||||
| >69 years | 3 | 66 | Ref. | ||
| ≤69 years | 9 | 43 | .029 | 4.6 (1.1–17.9) | .028 |
| Delay until operation | |||||
| ≤43h | 10 | 67 | Ref. | ||
| >43h | 2 | 42 | .207 | .4 (.9–2.3) | .348 |
| Fixation | |||||
| Two screws | 3 | 25 | Ref. | ||
| Three screws | 9 | 84 | .098 | .8 (.2–3.7) | .874 |
CI, confidence interval; Ref., reference value (odds ratio 1).
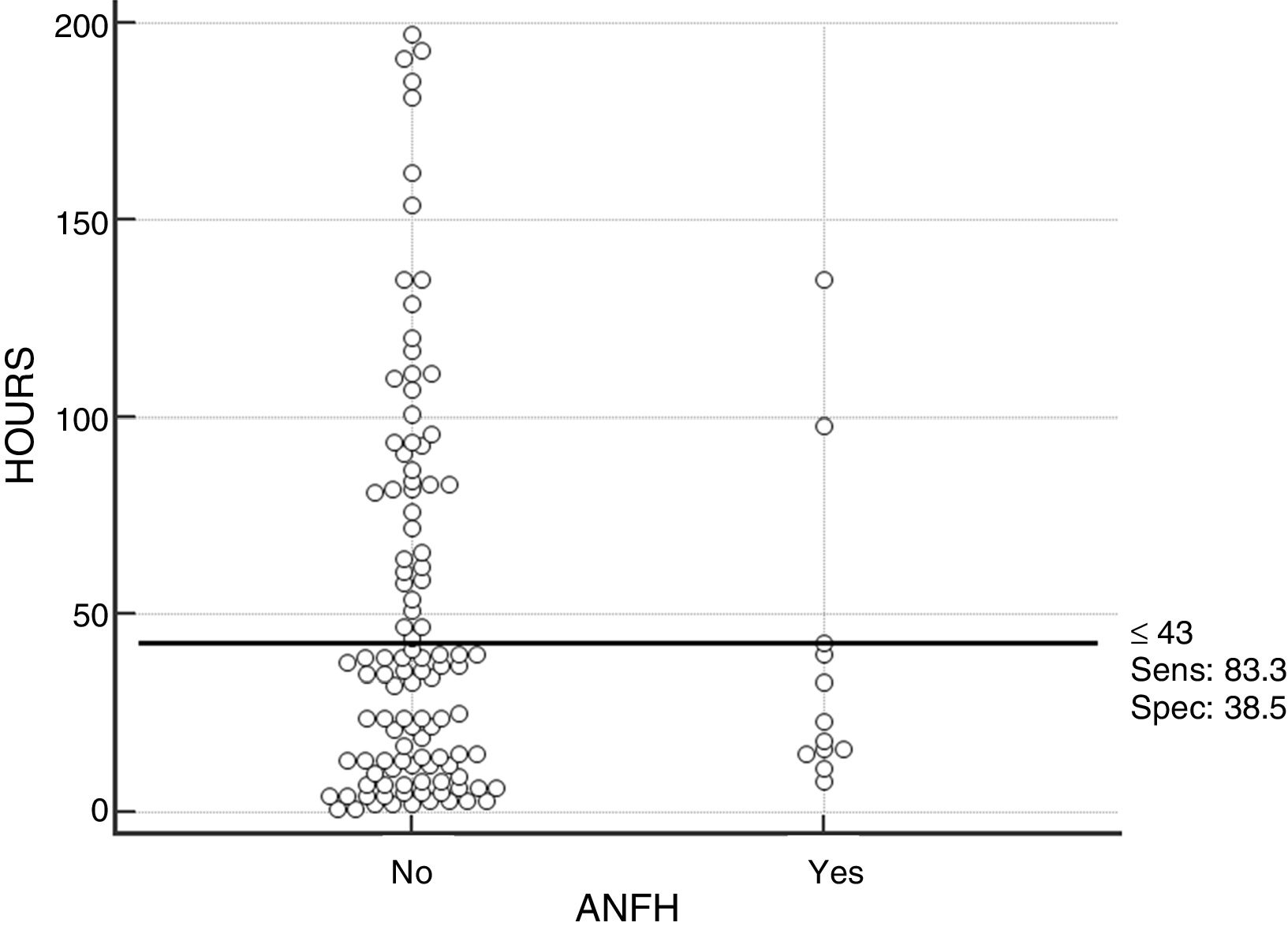
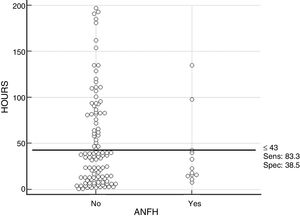
The mean delay until surgery for the entire sample was 48.8±48.1h. We determined that the cut-off point that best discriminated the probability of ANFH development in this study was a time until surgery of 43h (Fig. 1). In the ANFH group, there were 2 (16.7%) patients with a delay greater than 43h, and in the control group there were 42 (38.5%); the difference was not statistically significant (P=.207).
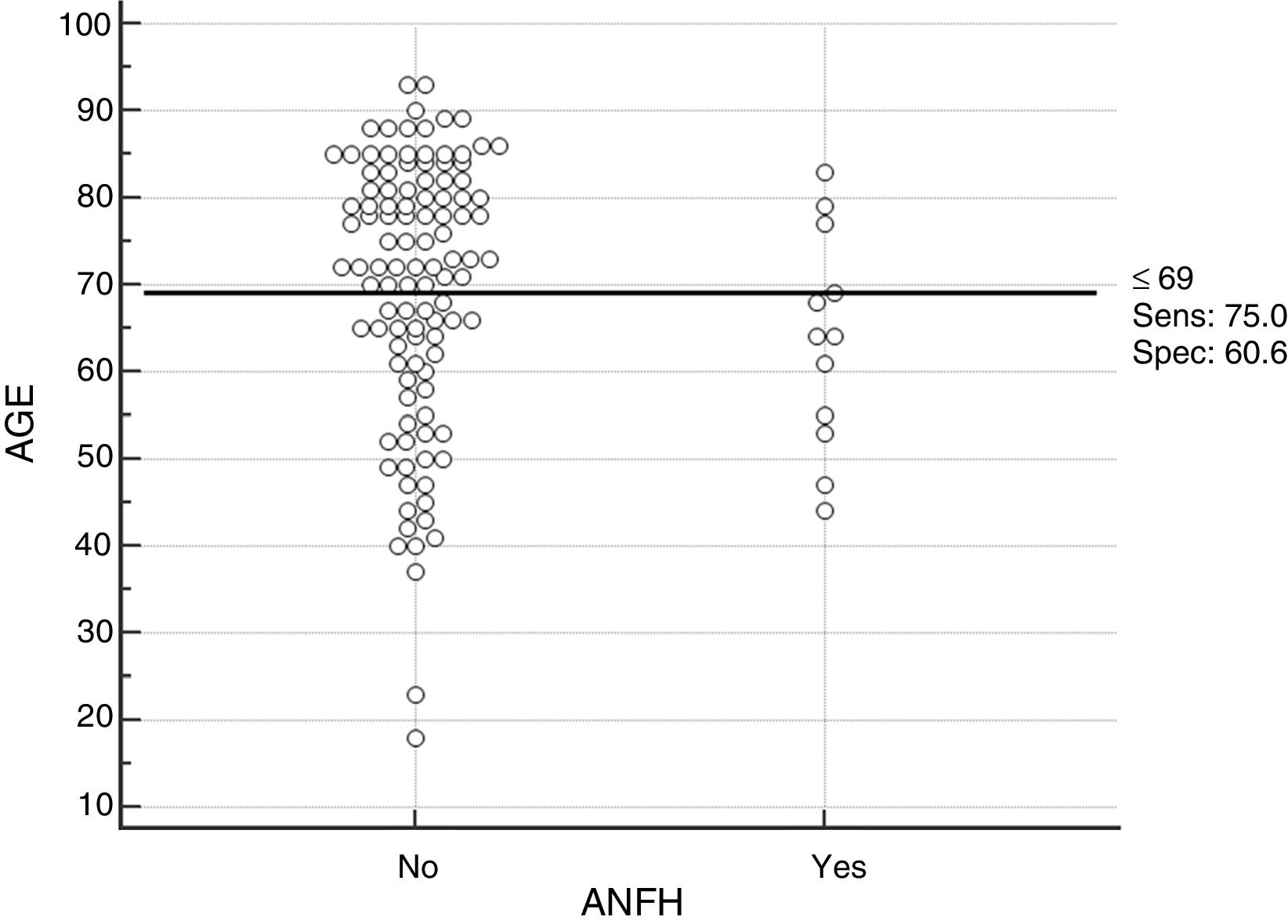
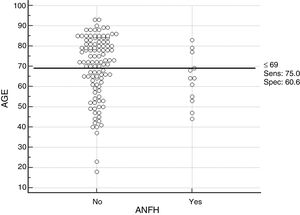
The mean age for the total sample was 69.1±15.3 years. The cut-off point that best described the probability of ANFH development was an age equal to or less than 69 years (Fig. 2). In the ANFH group, there were 9 (75%) patients aged 69 years or less, and in the control group there were 43 (39.4%), which was a statistically significant difference (P=.029).
Multivariate analysis (Table 3) revealed that only age equal to or less than 69 years was a significant predictor of ANFH (odds ratio 4.6; confidence interval [CI] 95%, 1.1–17.9; P=.028). The patients aged 69 years or less had a risk of developing ANFH 4.6 times greater than those more elderly than that age.
DiscussionThe rate of ANFH following internal fixation of undisplaced fractures of the femoral neck was 9.9% in the present study. Our main result was that an age equal to or less than 69 years was a significant predictor of ANFH development following internal fixation of undisplaced femoral neck fractures, without their being any significant influence from time of delay until surgery, sex or the number of screws used. The cut-off point for age was determined by statistical inference, selecting the age point with greatest sensitivity and specificity in detecting differences between patients with greater or lesser age.
Few previous studies have analysed the association between age and ANFH in undisplaced fractures. Unlike us, Loizou and Parker3 found an association between ANFH incidence and age less than 60 years in displaced fractures, but not for undisplaced fractures. However, follow-up in that study was by telephone, with a mean postoperative period of 1.5 years. In a study with a mean follow-up of 6 years, Do et al.10 observed a higher ANFH incidence among the patients aged less than 70 years with undisplaced cervical fractures, although it was not statistically significant. In displaced cervical fractures treated with internal fixation, the literature reports a higher rate of ANFH in patients of advanced age.4,14
In this study, the time period between the traumatism and surgery had no significant influence on ANFH development. For undisplaced cervical fractures, other authors did not observe any association either3,6,8 comparing intervals greater or less than 12h. Kim et al.15 found an ANFH rate of 7%, similar to ours, for elderly patients operated on within 48h after admission. Likewise, in displaced fractures, Razik et al.16 found that delay until surgery had no impact on ANFH in patients aged less than 60 years. The meta-analyses by Damany et al.2 and Papakostidis et al.5 did not find a correlation between delay until surgery and ANFH. Nevertheless, those studies recommended operating on those patients as soon as possible, because the incidence of reoperations due to other complications (such as pseudarthrosis) and mortality at 1 year were associated with a longer period of surgical delay.5,17,18
Various authors have analysed posterior cervical angulation as a potential risk factor for failure of fixation with screws in undisplaced fractures. Some authors viewed it as a significant factor,19,20 while others felt it was not.21,22 However, those studies did not analyse how cervical angulation influenced ANFH. Do et al.10 reported that cervical angulation was a predictor of fixation failure, but that it was not a significant predictor of ANFH.
Our study included consecutive patients with few exclusion criteria, so selection bias was minimised and the sample was adapted to clinical practice. In addition, the indications, surgical methods and postoperative follow-up were homogeneous. Although the operations were performed by several surgeons, all of them had in-depth experience in this type of surgery. We believe that the follow-up (a minimum of 2 and a half years, up to 4.1 years) was long enough to detect the patients with ANFH, given that the cases described in the literature happened within 2 years postoperatively.20,21 However, this study has several important limitations. In the first place, its retrospective design, which is a consequence of the low prevalence of ANFH in undisplaced fractures. Secondly, the limited number of patients with ANFH, although it is higher than those of the majority of the studies published in the last decade. Neither mortality nor functional results were evaluated, because there was no reason to do so in this study as our study objective was to identify risk factors for the development of ANFH.
In conclusion, the patients with an age equal to or less than 69 years presented a higher risk of developing ANFH after undisplaced femoral neck fracture treated with percutaneous screw fixation. A delay in time until surgery longer than 43h was not a risk factor. However, further studies are needed to corroborate these findings.
Level of evidenceLevel of evidence III.
Conflict of interestsThe authors have no conflicts of interest to declare.
Please cite this article as: Novoa-Parra CD, Pérez-Ortiz S, López-Trabucco RE, Blas-Dobón JA, Rodrigo-Pérez JL, Lizaur-Utrilla A. Factores asociados al desarrollo de necrosis avascular de cabeza femoral tras fractura del cuello femoral no desplazada tratada con fijación interna. Rev Esp Cir Ortop Traumatol. 2019;63:233–238.