Giant cell tumours (GCTs) of the bone are benign, but locally invasive tumours. We present a new case of carpus GCT, involving the triquetrum.
The diagnosis required a prior biopsy before doing the block resection. This treatment is the best option to avoid recurrences.
We review the literature on this particular lesion in the carpus bone.
El tumor de células gigantes (TCG) óseo constituye una neoplasia benigna, pero localmente invasiva. Su localización en el carpo es excepcional.
Presentamos un nuevo caso de TCG en el carpo, el cual implicó al piramidal. El diagnóstico requirió de biopsia previa antes de proceder a su exéresis en bloque, tratamiento que constituye la mejor opción para evitar recidivas.
Revisamos la literatura de esta particular lesión en los huesos carpianos.
The giant cell tumour (GCT) is a benign, but locally invasive, neoplasia that represents 5% of all the primitive bone tumours.1 It usually presents in young adults, as a lytic lesion in a long bone epiphysis, especially around the knee. It is seldom fund in the bones of the hand, given that its incidence is 2%. When it does, it habitually affects the phalanges and metacarpals.2–4 The presence of GCT in the carpal bones is truly rare, although the tumour in all the carpals except the pisiform has been described.5
In the triquetrum, there are only 2 case reports of a solitary tumour,6,7 plus 1 on a multicentric form.8 In this article, we present the third case known in literature, a case of GCT isolated in the triquetrum.
Clinical caseThe patient was a 42-year-old woman, ex-smoker without any previous illnesses of interest, who came to the hospital because of pain and functional limitation in the right wrist of 3 months’ development.
The physical examination revealed moderate swelling in the dorsal zone of the carpus, with painful palpation upon pressure in the cubital region. Joint mobility, although painful, was conserved.
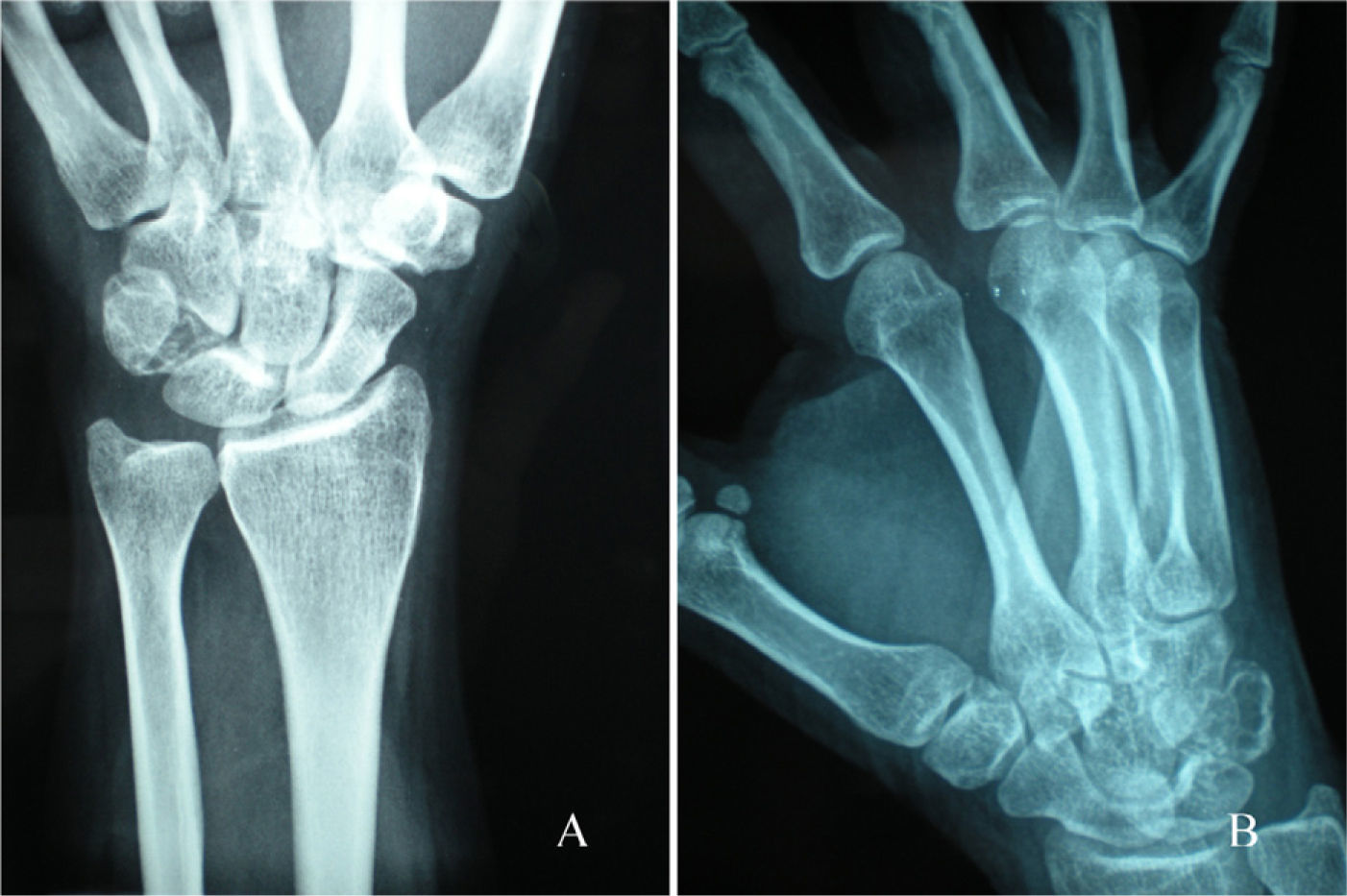
Radiography showed a lytic lesion in the triquetrum (Fig. 1). Complementary computed axial tomography (CAT) and nuclear magnetic resonance (NMR) studies revealed a hypodense lesion that expanded the triquetrum, with cortical scalloping (Fig. 2). There were no images of fracture. However, capture of the adjacent soft tissues was seen, which extended dorsally towards the extensor tendons and in the palm between the capitate and hamate bones but without affecting them. There was no other local or remote affectation. Based on the radiological criteria, it was a benign lesion that could be a GCT.
The biopsy, obtained using radioscopic-guided Tru-Cut, confirmed the diagnosis of GCT.
The treatment consisted of block resection of the lesion and the adjacent soft tissues. During the operation, we verified that the cartilage surfaces of the capitate, lunate, hamate and pisiform bones did not have any alterations. To stabilise the carpus, the lunate was fixed to the radius with a Kirschner wire.
Following 4 weeks of immobilisation with Colles-type cast bandage, rehabilitation with assisted physiotherapy was initiated.
After 2 years of follow-up and after verifying that there was no tumour recurrence, we performed an intracarpal arthrodesis between the lunate–radius and capitate–hamate, with good radiological and clinical evolution.
DiscussionBone GCT is an initially benign primitive tumour. However, it tends to recur locally and has been known to metastasise in some 2–3% of cases.
The tumour presents in young adults, with an incidence peak between those 20 and 30 years old, and is slightly more frequent in women. The lesions are almost always monostotic, as multicentric lesions reach only 1% of all the cases.
The skeletal areas most often affected by GCT are the long bone epiphyses, with the distal femur and proximal tibia representing 50% of the cases: next in order of appearance are the distal radius and the proximal humerus. In the hand, GCT tumour frequency is less than 2% and, within that percentage, the phalanges and metacarpals are the bones most frequently affected.2
In the carpal bones, GCT incidence is even lower, representing some 10–15% of all those occurring in the hand. It has been found in all the carpal bones except the pisiform, with the scaphoid and the hamate being the most frequent. When the presentation is multicentric, it affects several bones due to the direct expansion between adjacent bones.4,5
There are only 2 cases of solitary GCT in the triquetrum: Louis6 presented the first in 1986, treating it by resecting the triquetrum affected and performing intercarpal arthrodesis. In 2009, Kotnis7 published the second case, treated through curettage; there was no recurrence, but there was follow-up for only 4 months.
With a multifocal appearance in the carpal bones including the triquetrum, Gupta8 described a case in 1995, affecting the capitate, triquetrum and hamate; it was treated by distal row carpectomy and reconstructed an autologous iliac bone graft.
Diagnosing GCT in the carpal bones can be difficult and can be delayed from symptom appearance, as the tumours are usually not very noticeable. However, the typical clinical presentation consists of pain in the area, slight swelling and movement limitation. All of these are sometimes attributed to an undetected previous trauma.
The diagnosis is based on the radiological and clinical data, confirmed by histological study. There is eccentrically located cortical expansion shown in radiography, with clearly circumscribed borders and no reactive sclerosis. These findings lead to differential diagnosis considering other entities such as aneurysmatic bone cyst, reparative granuloma, chondroblastoma, intra-osseous ganglion or non-ossifying fibroma.7 A CAT details these characteristics and NMR is especially useful in ascertaining the integrity of the surrounding soft tissues.
With these approaches, biopsy should be obtained before surgery or during the operation. It can be radioscopy-guided to obtain a more precise sample, as was done in our case. Microscopically, GCTs are red, friable tissue tumours, which attenuate the cortex but do not destroy it. The tumour component consists of mononuclear cells having the characteristics of the osteoblast progenitors, without a matrix.
However, neither the clinical manifestations nor the anatomopathological appearance serves to predict the behaviour of these tumours, whose development is variable and erratic. As we have pointed out, there may be local recurrences, remote metastasis or spontaneous malignant transformation. Metastasis is frequent in patients who have had local recurrences and generally occur in less than 2 years.2,3
Surgery is the treatment of choice for GCT, which can be of 2 types.9,10 The first is intralesion treatment, consisting of local curettage with or without bone graft. Cement is the most appropriate material to use as a graft, because when it fills the cavity it produces a thermal reaction that damages any tumour cells that might remain and, consequently, reduces the risk of recurrence.11
A more aggressive treatment includes the techniques of marginal removal, extended removal, block resection with or without reconstruction and sometimes amputation. It has been proven that treatment through intralesion procedures – curettage with or without graft – presents a recurrence rate over 50%, and even more in the distal radius; and that the most radical options lower the recurrence rate significantly. Athanasian2 indicated 36% compared with 79% of recurrences with curettage. For that reason, intralesion treatment is applied in cases of clearly resectionable intraosseous affectation and the more radical treatments are performed when there is extra-osseous extension. In those cases, the soft tissues should be protected during surgery because the tendency is dissemination by means of these tissues. Given that GCTs are radiosensitive, radiotherapy is an option that should be considered when surgery is contraindicated.12 In our case, bearing in mind that it was a lesion limited to the triquetrum and adjacent soft tissues, we decided that a block resection was best. Although curettage with a graft (principally cement) has been shown to be a good option, the fact that the soft tissues around the bone were affected led us to choose block resection, which has been shown to reduce recurrence. As multifocal affectation was more frequent in the carpus and recurrence was possible, we accepted the instability that triquetrum resection provokes and did not perform arthrodesis initially. After the 2 years of greatest risk of recurrence had passed, we could carry out arthrodesis with a better guarantee of being a definitive surgery. Bearing in mind everything that has been indicated, it can be stated that there is no standard treatment for GCTs and that such treatment should be individual, based on the tumour location, size and structures through which it extends.
Level of evidenceLevel of evidence IV.
Ethical disclosuresProtection of human and animal subjects. The authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of Data. The authors will declare that they have followed the protocols of their work centre on the publication of patient data and that all the patients included in the study have received sufficient information and have given their informed consent in writing to participate in that study.
Right to privacy and informed consent. The authors must have obtained the informed consent of the patients and /or subjects mentioned in the article. The author for correspondence must be in possession of this document.
Please cite this article as: Gutiérrez-Santiago MM, et al. Tumor de células gigantes en hueso piramidal: caso clínico y revisión de la literatura. Rev Esp Cir Ortop Traumatol. 2012;56(2):149–52.