The aim of this study was to assess the relationship between arterial cannulations and the development of limb length discrepancies in childhood or impaired growth of the proximal femur.
Material and methodsA retrospective study was conducted on 300 children who required arterial cannulation and/or cardiac catheterisation during childhood in relation to congenital heart diseases. Seven of these patients were referred from the Paediatric Cardiology clinic due to a limb length discrepancy and/or proximal femoral deformities.
ResultsSeven children, with a mean age of 10 years, were referred to our clinic. The mean length discrepancy was 2.7cm, and was more frequent on the right side. Three of the patients presented with proximal femoral deformities: two cases of caput valgum and one of bilateral physeal arrest of the greater trochanter. All children were initially treated with a shoe lift in the shortest limb. One of them required a tibial lengthening and two others are awaiting a similar procedure.
ConclusionWe recommend clinical and radiological follow-ups of patients who have undergone catheterisation during their infancy due to the relationship between these techniques and the risk of developing a limb length discrepancy.
Conocer la posible asociación entre la realización de canalizaciones arteriales con el desarrollo de discrepancias de longitud en los miembros inferiores y de alteraciones del crecimiento del fémur proximal en la infancia.
Material y métodosSe realiza un estudio retrospectivo de 300 niños que precisaron una canalización arterial y/o un cateterismo cardíaco durante la infancia en relación con la existencia de patología cardiovascular congénita. Durante su seguimiento en la consulta de cardiología pediátrica, a 7 de ellos se les detectó una discrepancia de longitud de los miembros inferiores (MM II) por lo que fueron remitidos a nuestras consultas externas para estudio.
ResultadosLos 7 pacientes fueron valorados en nuestra consulta con una media de 10 años de edad. La media de discrepancia de longitud fue de 2,7cm, más frecuente en el lado derecho a expensas de fémur y tibia. Tres de los pacientes presentaron una deformidad de la extremidad proximal del fémur: 2 casos de caput valgum y uno de apofisiodesis aislada bilateral de trocánter mayor. Todos los niños fueron tratados inicialmente con un alza en el miembro más corto. Uno de ellos precisó un alargamiento tibial y 2 de ellos están a la espera de alargamiento para la compensación de la discrepancia.
ConclusiónEs recomendable el seguimiento clínico y radiológico de los pacientes a los que se les haya realizado un cateterismo en su primera infancia por la relación que existe entre estas técnicas y el riesgo de desarrollar una discrepancia de longitud en el miembro inferior.
Length discrepancy between the lower limbs (LL) is one of the most frequent causes for consultation in infantile orthopaedics. In general, the cause of the discrepancy is easily identifiable, with the most common being1 posttraumatic, postinfectious, congenital, palsy, etc. Discrepancies with a vascular origin are exceptional, with the most frequent being limb lengthening due to vascular malformations, like those found in Klippel–Trénaunay–Weber syndrome. Shortening discrepancies with a vascular origin are even more infrequent and caused by an arterial vascular disorder which is generally known.
Heart catheterisation is a complex and invasive procedure which consists in introducing a catheter in order to assess the anatomy of the heart and coronary arteries, as well as to estimate the function of the heart, measure the pressures of the heart cavities, etc. It can even be used with a therapeutic purpose, to close interatrial communication, ductus arteriosus with devices, valvuloplasties, embolisation of collaterals, etc. This technique is commonly employed in the study of congenital cardiopathies affecting newborns.
The most commonly used technique to cannulate femoral vessels is Seldinger's technique,2 described in 1953, which makes it possible to cannulate blood vessels without requiring a surgical access. The considerable advances in catheter size and materials have enabled vascular access in increasingly smaller children. Nevertheless, cannulating femoral vessels in a newborn is still not without risks. Different complications have been described,3 including vascular perforations, sepsis, incorrect placement of the catheter and tear thereof, fatty embolisms, vascular damage caused by the size of the catheter, etc. These complications, less clinically surprising in newborns than in adults, may initially go unnoticed and give rise to long-term growth disorders in the proximal end of the femur and length discrepancies between the LL.
The present work analyses patients with LL length discrepancies and/or alteration of proximal femoral growth who underwent catheterisation during childhood.
Material and methodsA descriptive observational study was carried out, with retrospective data collection of 300 patients undergoing cardiac catheterisation between 1992 and 2004.
A total of 358 catheterisations were performed on 300 patients at our centre during the study period. The causes were congenital cardiopathy or systemic pathology in the first days of life, requiring admission at the intensive care unit (ICU).
Out of the 300 cases, 7 patients (5 girls and 2 boys) were referred to our clinic from the Paediatric Cardiology Service, due to clinical discrepancy of LL length. Each child was clinically and radiographically examined at our outpatient clinic. Data collected included age, gender, duration of monitoring, type of congenital cardiopathy, perinatal problems, number of catheterisations undergone by the patient and at what age, and complications associated with the procedures. Physical explorations were carried out and complementary imaging tests were obtained: LL telemetries to study the LL length discrepancy and hip radiographs to assess the proximal end of the femur.
The epidemiological data collected were statistically analysed using the software package SPSS18. A descriptive study was performed, expressing quantitative variables as means and qualitative variables as absolute values and percentages. The statistical significance of qualitative variables was studied using the chi-squared test.
All patients underwent measurement of arterial tension (AT) at rest in the lower and upper limbs. Significant differences were expected between the affected limb and the rest of the limbs; however, the data obtained were not significant.
Six of the patients were diagnosed with congenital cardiopathy at birth: 1 patient with Fallot tetralogy, 2 with severe aortic stenosis, 1 with large vessel transposition and 2 with pulmonary atresia with interventricular communication. All underwent catheterisation in the first 2 months of life, and in some cases repeatedly (9 catheterisations) until adolescence. In all patients, the intention was initially diagnostic and subsequently therapeutic (embolisation, angioplasties, valvuloplasties, etc.). The procedures were carried out indistinctly on the right and left sides, using 3 French and 4 French catheters for arterial catheterisations and between 4 French and 14 French for venous catheterisations (always using the smallest possible catheter which enabled the procedure for the size and weight of the patient).
One of the cases was a premature baby (31 weeks), with a weight of 880g at birth, who was diagnosed with acute sepsis after 1 week of life and required several vascular cannulations to treat and monitor the pathology. After 10 days of life, the patient suffered an episode of hypoperfusion in the lower left limb, with pulse attenuation.
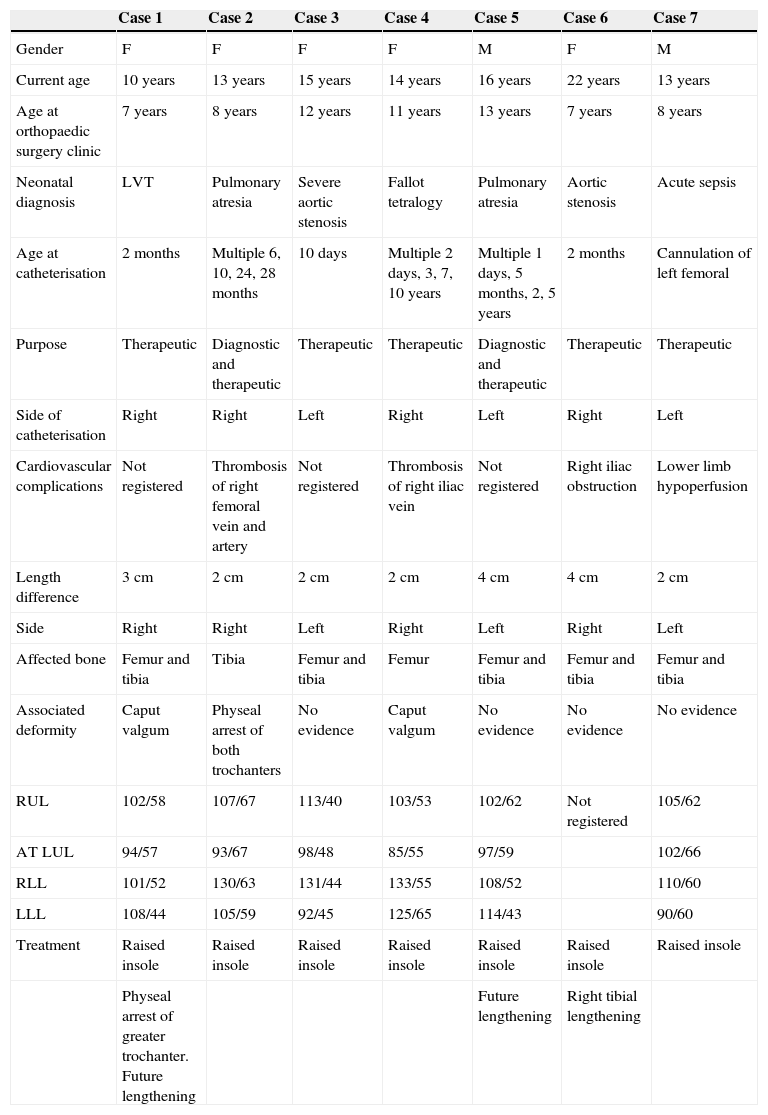
ResultsWe present 7 case reports of clinical length discrepancy in the LL. The clinical details are shown in Table 1.
Summary of results obtained in each patient.
| Case 1 | Case 2 | Case 3 | Case 4 | Case 5 | Case 6 | Case 7 | |
|---|---|---|---|---|---|---|---|
| Gender | F | F | F | F | M | F | M |
| Current age | 10 years | 13 years | 15 years | 14 years | 16 years | 22 years | 13 years |
| Age at orthopaedic surgery clinic | 7 years | 8 years | 12 years | 11 years | 13 years | 7 years | 8 years |
| Neonatal diagnosis | LVT | Pulmonary atresia | Severe aortic stenosis | Fallot tetralogy | Pulmonary atresia | Aortic stenosis | Acute sepsis |
| Age at catheterisation | 2 months | Multiple 6, 10, 24, 28 months | 10 days | Multiple 2 days, 3, 7, 10 years | Multiple 1 days, 5 months, 2, 5 years | 2 months | Cannulation of left femoral |
| Purpose | Therapeutic | Diagnostic and therapeutic | Therapeutic | Therapeutic | Diagnostic and therapeutic | Therapeutic | Therapeutic |
| Side of catheterisation | Right | Right | Left | Right | Left | Right | Left |
| Cardiovascular complications | Not registered | Thrombosis of right femoral vein and artery | Not registered | Thrombosis of right iliac vein | Not registered | Right iliac obstruction | Lower limb hypoperfusion |
| Length difference | 3cm | 2cm | 2cm | 2cm | 4cm | 4cm | 2cm |
| Side | Right | Right | Left | Right | Left | Right | Left |
| Affected bone | Femur and tibia | Tibia | Femur and tibia | Femur | Femur and tibia | Femur and tibia | Femur and tibia |
| Associated deformity | Caput valgum | Physeal arrest of both trochanters | No evidence | Caput valgum | No evidence | No evidence | No evidence |
| RUL | 102/58 | 107/67 | 113/40 | 103/53 | 102/62 | Not registered | 105/62 |
| AT LUL | 94/57 | 93/67 | 98/48 | 85/55 | 97/59 | 102/66 | |
| RLL | 101/52 | 130/63 | 131/44 | 133/55 | 108/52 | 110/60 | |
| LLL | 108/44 | 105/59 | 92/45 | 125/65 | 114/43 | 90/60 | |
| Treatment | Raised insole | Raised insole | Raised insole | Raised insole | Raised insole | Raised insole | Raised insole |
| Physeal arrest of greater trochanter. Future lengthening | Future lengthening | Right tibial lengthening |
AT, arterial tension; F, female; LLL, left lower limb; LUL, left upper limb; LVT, large vessel transposition; M, male; RLL, right lower limb; RUL, right upper limb.
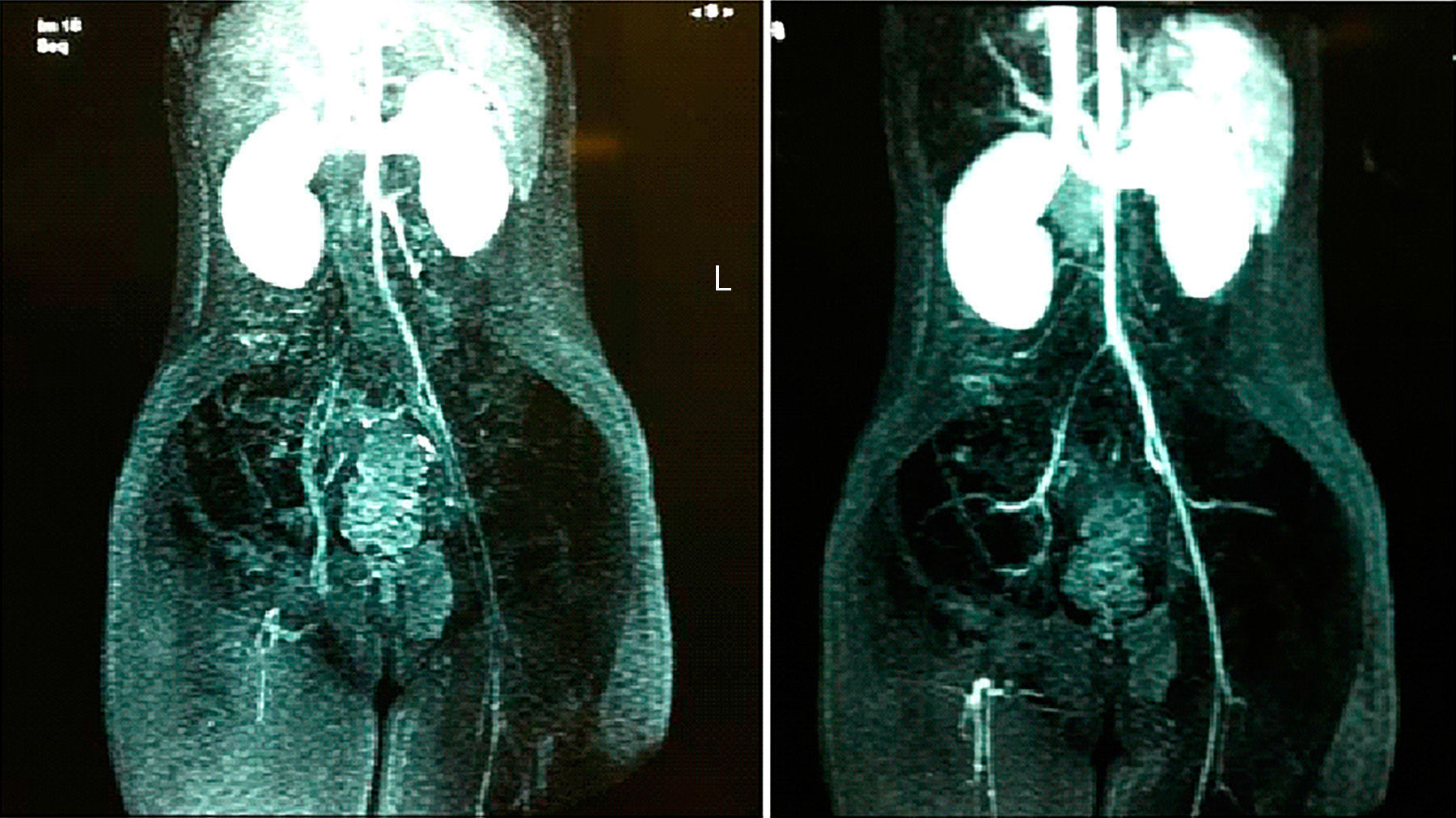
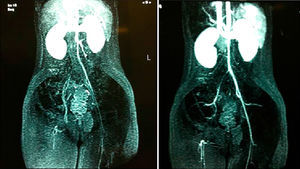
In 50% of the cases, patients suffering a congenital cardiopathy, the existence of a vascular lesion was confirmed in the LL, 1 in the femoral artery and vein, 1 in the right iliac vein and 1 in the right iliac and femoral artery (Fig. 1). The length discrepancy was observed to coincide with the side where the vascular complication took place.
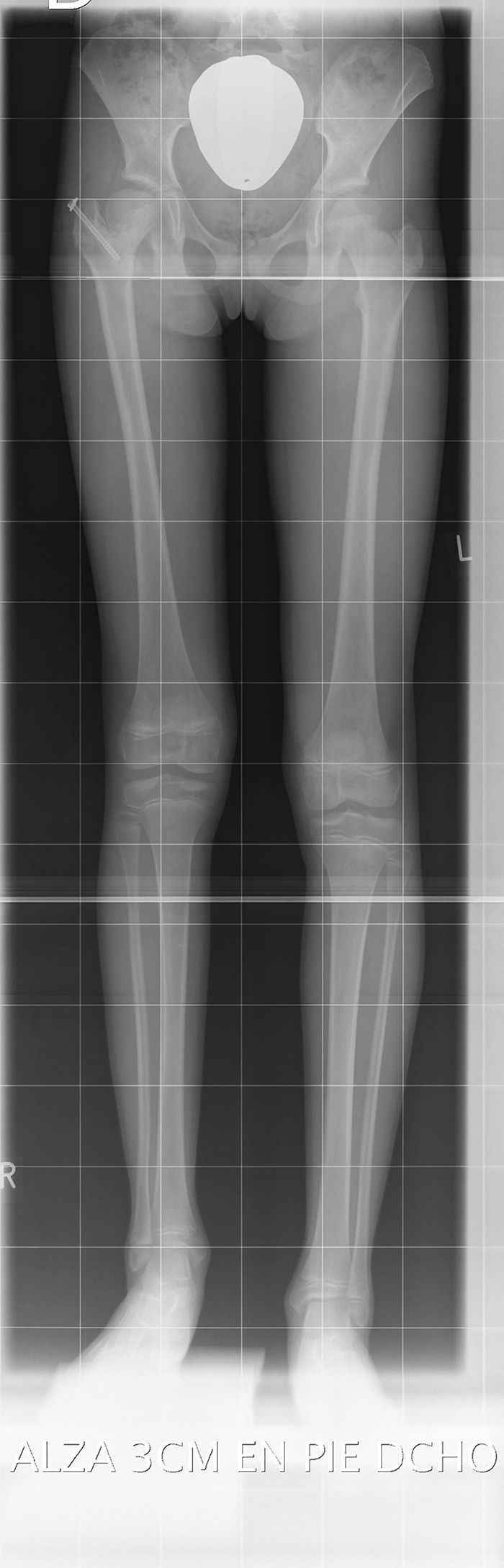
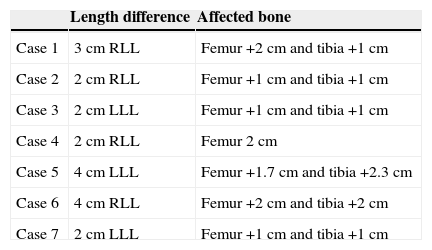
The children reached our clinic through referral from the Cardiology Service, with a mean age of 10 years. The mean length discrepancy was 2.7cm, and more frequent on the right side. In the majority of cases, length discrepancies were at the expense of the femur and tibia (Table 2).
Location of the length difference in each case.
| Length difference | Affected bone | |
|---|---|---|
| Case 1 | 3cm RLL | Femur +2cm and tibia +1cm |
| Case 2 | 2cm RLL | Femur +1cm and tibia +1cm |
| Case 3 | 2cm LLL | Femur +1cm and tibia +1cm |
| Case 4 | 2cm RLL | Femur 2cm |
| Case 5 | 4cm LLL | Femur +1.7cm and tibia +2.3cm |
| Case 6 | 4cm RLL | Femur +2cm and tibia +2cm |
| Case 7 | 2cm LLL | Femur +1cm and tibia +1cm |
LLL, left lower limb; RLL, right lower limb.
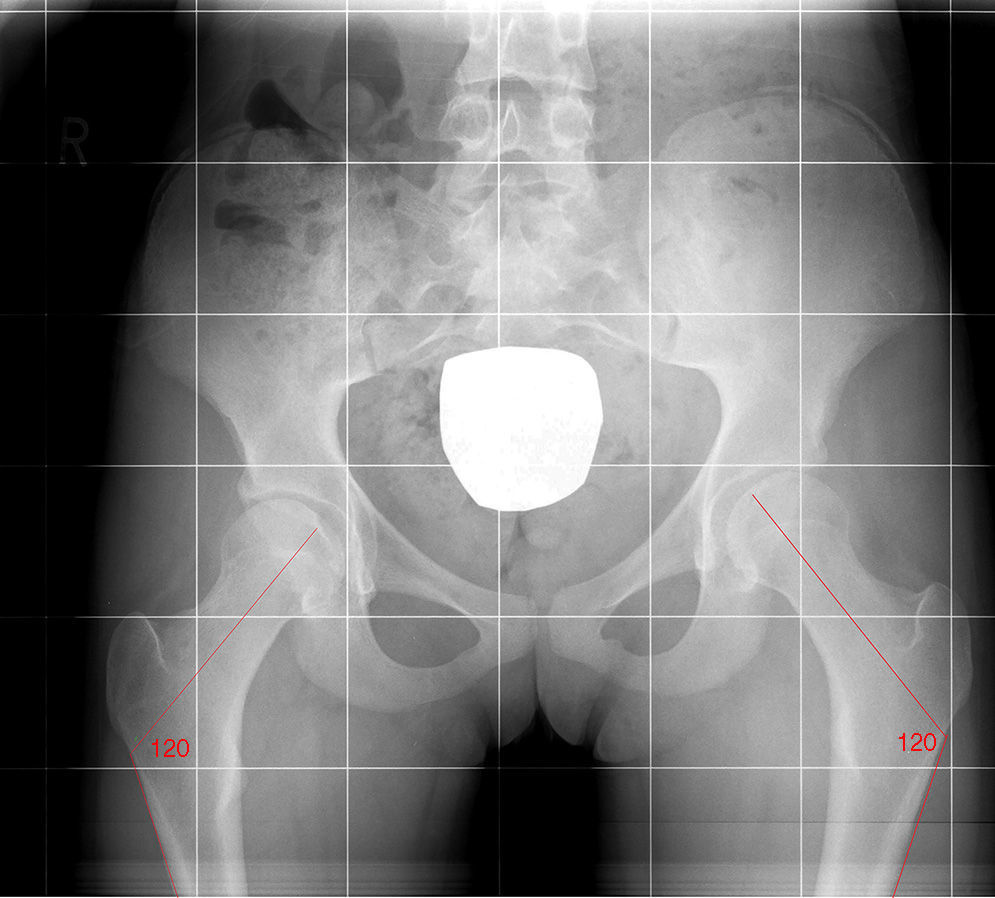
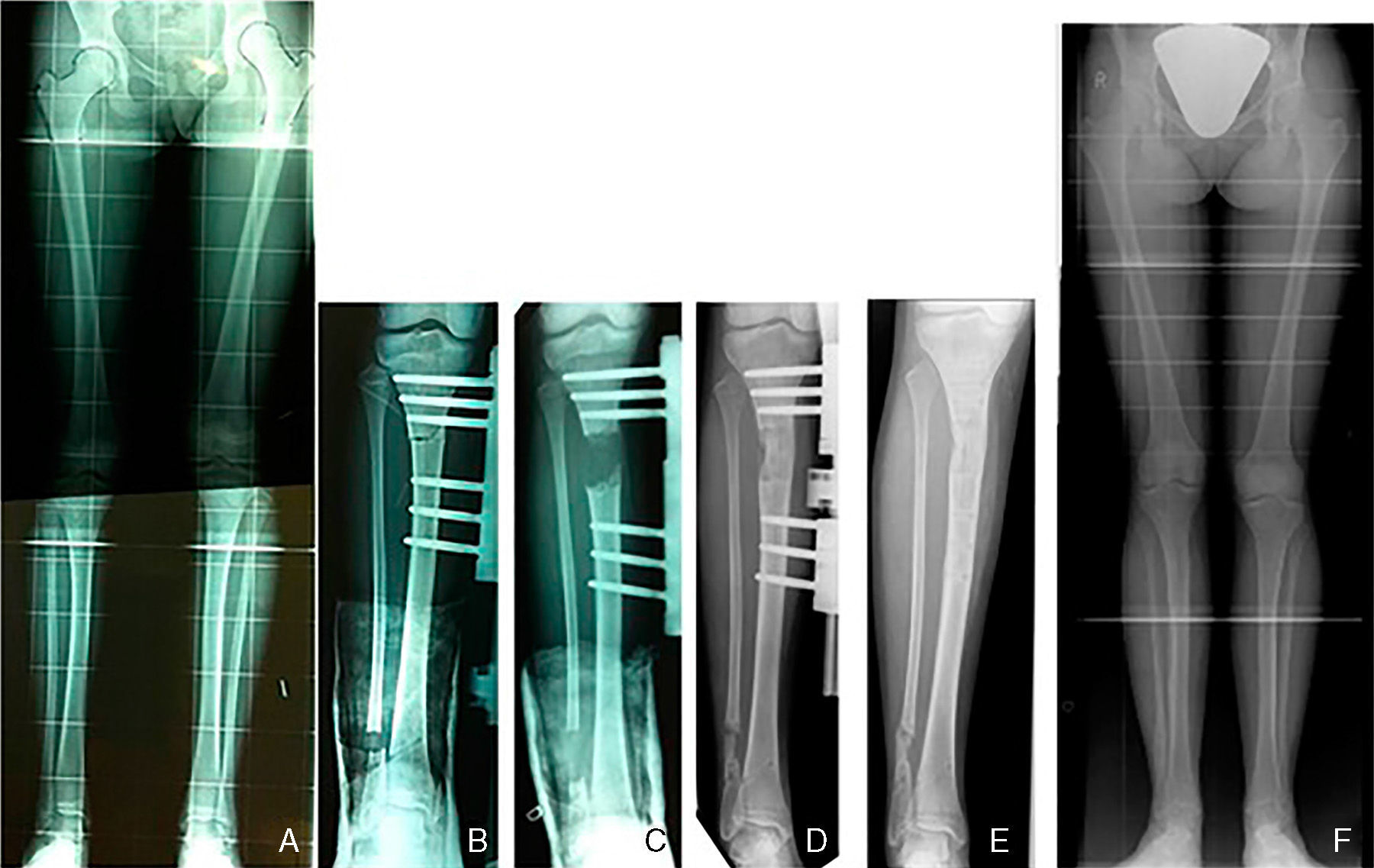
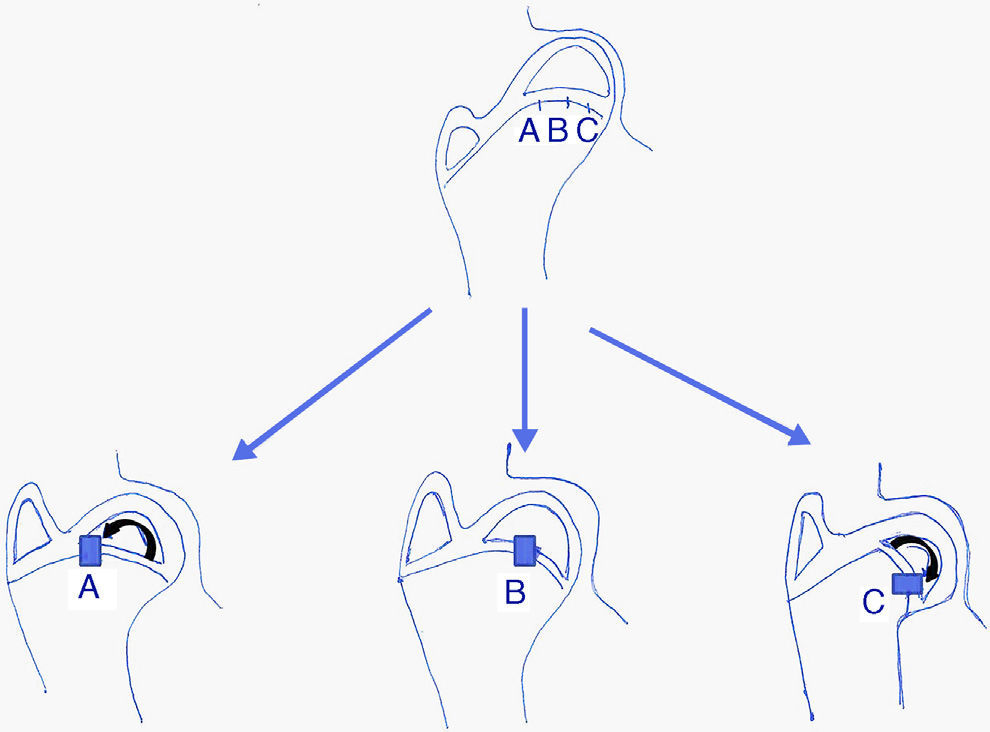
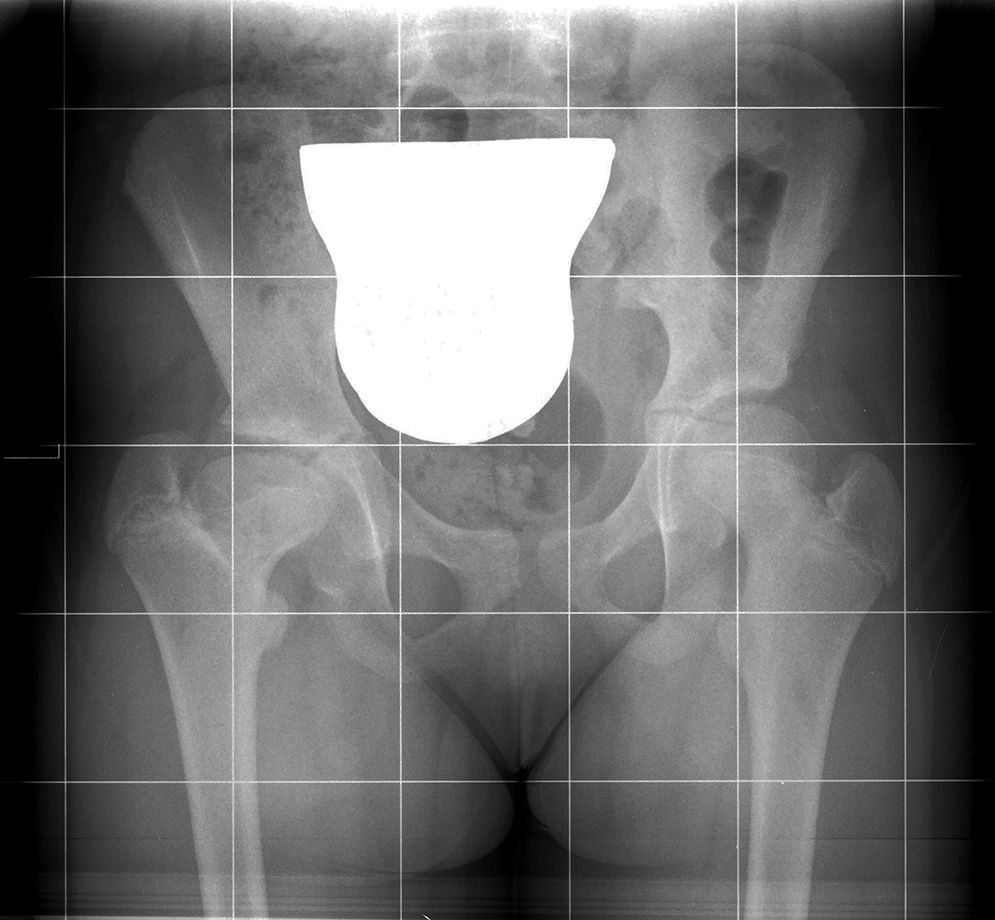
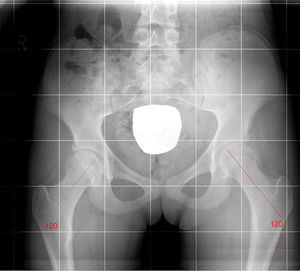
In our series, 3 of the 6 patients presented deformity of the proximal end of the femur. Two children presented valgus deformity of the femoral head and a third presented isolated physeal arrest of both greater trochanters, causing a negative Voss effect with a normal cervicodiaphyseal angle (Fig. 2). One of the cases required surgical treatment due to relative hypergrowth of the greater trochanter, thus undergoing physeal arrest with a percutaneous screw to avoid a progressive failure of the gluteal musculature (Fig. 3).
All 7 cases were initially treated with a raised insole for the short limb, to compensate for the length difference. Children who presented the greatest length discrepancies in the LL required surgical treatment. One of the patients underwent callotasis at the level of the tibia, due to a difference of 4cm (Fig. 4). The other 2 patients, with a length discrepancy of 3 and 4cm, are currently waiting to reach bone maturity in order to undergo femoral lengthening in one case and tibial lengthening in the other.
DiscussionDifferences in length between the lower limbs represent a dynamic process throughout childhood. The frequency of the causes has changed throughout history and with progressive advances in medicine. Infectious causes and poliomyelitis have decreased and/or practically disappeared in our medium, and currently the most common are due to congenital causes, trauma and secondary to surgical procedures carried out during infancy, such as limb preservation following musculoskeletal sarcomas. Vascular causes continue to be the least common, in about 2–5% of cases.
We present 7 cases of children with length discrepancies in the LL who did not present another attributable cause other than vascular lesion by arterial cannulation or catheterisation, which was described over 40 years ago.4,5
The treatment of these length discrepancies with a vascular aetiology depends on the age of the child at the time of diagnosis, the remaining growth potential and the degree of discrepancy. There are different correction methods,6 with the most common being conservative treatment through raised insoles in the shorter limb, indicated when the difference is under 2cm. This was the most frequent situation in our cases, taking into account the scarce proportion represented by the proximal end of the femur in the length of the entire lower limb (under 30%). Epiphysiodesis or growth cessation of the longer limb could be indicated in cases with differences around 2–3cm, whilst extension of the shortest limb would be indicated in differences greater than 3–4cm. Thus, in our series, 1 of the patients required tibial lengthening and the other 2 are currently waiting until bone maturity in order to carry out the procedure. The rest were managed with raised insoles, as the length differences were under 2–3cm.
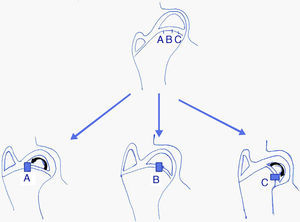
The shape of a proximal end of the femur in adults depends on a harmonic growth of the 3 growth plates7 comprising it during infancy (longitudinal plate, trochanteric plate and femoral neck isthmus plate). Traumatic, infectious, vascular or iatrogenic lesions may lead to a femoral head with a short neck (coxa breva), or a varus or valgus deformity of the head (caput varum or caput valgum) (Fig. 5). In all cases, the greater trochanter may continue growing and cause relative hypergrowth.
In our series, 3 of the patients presented deformity of the proximal end of the femur. Two children presented valgus deformity of the femoral head due to lesion in the most external portion of the physis of the femoral head, possibly due to involvement of one of the branches of the lateral circumflex. In one of these cases we observed hypergrowth of the greater trochanter and a shorter and narrower neck than in the contralateral limb. In the other case, with a more extensive involvement, the same characteristics were observed but there was an additional loss of sphericity of the femoral head and decrease of the joint-trochanter distance of at least 2cm in relation to the other hip. These findings are compatible with involvement not only of the physis of the isthmus, but also of the longitudinal physis (Fig. 6). In the third case, we observed an isolated trochanteric physeal arrest that caused a negative Voss effect, although with a normal cervicodiaphyseal angle due to a probable lesion of the trochanteric growth plate.
The patients in our series were children with highly complex pathologies who required repeated and prolonged admissions at intensive care units. All of them underwent multiple invasive procedures, including cannulation of femoral vessels for administration of medication and measurement of arterial and venous pressures, among others. Occasionally, secondary to this type of procedures, there were complications such as vascular spasms and thrombosis or other vascular lesions. As previously mentioned, neither vascular catheterisations nor arterial/venous cannulation in newborns is without risks. One of the most frequent complications is vascular spasm,8 which is defined as a temporal and reversible arterial constriction. This is often triggered by the extraction of a blood sample or vascular cannulation. The symptoms are characterised by pallor or transient cyanosis of the affected limb, with a decrease of pulses and perfusion, and usually lasting for less than 4h, although it can be difficult to distinguish from a more severe lesion, like vascular thrombosis, which would produce sequelae. The diagnosis of vasospasm is generally obtained retrospectively, after observing the transient nature of the symptoms and recovery of perfusion. The absence of pulse 3h after vessel cannulation or catheterisation is highly indicative of arterial thrombosis.9
The incidence of arterial complications following catheterisation is around 3.7%, increasing to 7.3% in children aged under 1 year.2 Newborns are particularly susceptible to thromboembolisms10 due to the small calibre of their blood vessels, the immaturity of their thrombolytic and fibrinolytic systems and disorders of haemostatic balance caused by dehydration, septicaemia, hypovolemia and congenital heart disease.
No complications were observed during the procedure in 3 the cases in our series; however, these patients reached our clinic due to difference in length between their LL coinciding with the side where the catheterisation was performed. It could be thought that, in these cases, the length discrepancy in the LL would be secondary to a vascular lesion that may have gone unnoticed. However, it could also be possible that the existence of a heart malformation coincided with another musculoskeletal one, since both are congenital malformations with a certain prevalence.
In a cohort study with 58 children who underwent catheterisation of the femoral artery for diagnostic purposes, Taylor et al.11 observed obstruction of the femoral artery in 19 cases (33%). Of these, 4 cases (8%) presented a shortening of the LL (mean value of 1.6cm, range between 1.5 and 1.7cm). In another retrospective study12 with 34 paediatric patients, 3 of them (8%) presented length discrepancy in the LL following catheterisation of the femoral artery.
A study13 on a series of 7 cases investigated cessation of plate growth in different locations after cannulation of the radial, brachial and femoral arteries. The authors described 2 cases of epiphysiodesis in the upper limb and 4 cases of length discrepancy in the LL and 1 case of coxa valga following cannulation of the femoral artery. Synnes et al.14 presented 2 case reports with length discrepancy following cannulation of the femoral artery. The 2 cases were premature children who required admission in a newborn ICU and who underwent cannulation of the femoral artery on the side presenting length discrepancy.
Guy et al.15 described 4 cases of length discrepancy, 2 in the LL and 2 in the upper limbs, secondary to physeal damage by extravasation of substances used during vascular cannulation.
Klein et al.16 recommended long-term monitoring through the use of teleradiographs in order to measure LL in children suffering length discrepancy who had suffered a iatrogenic vascular lesion. In their study, they analysed 32 patients with a mean age of 2.5 years who had suffered iatrogenic arterial lesions; of these, 21 appeared after an angiography (12 by heart catheterisation), 7 after umbilical catheterisation, 2 after cannulation of the radial artery, 1 after a cardiopulmonary bypass and 1 after spinal fusion. Out of these patients, 9% (3 cases) developed a length discrepancy in the LL; 2 of them due to a clot in the iliac artery following heart catheterisation and the other due to a clot in the femoral artery following cannulation to carry out a cardiopulmonary bypass.
The previously mentioned literature and our series of cases suggest that the length discrepancies were likely due to a vascular lesion following cannulation of the femoral artery by occlusion of the physeal nutrient arteries by spasm, embolism or thrombosis in patients with severe cardiopathies, and were therefore inevitable.
Unfortunately, there are very few studies that help us to delve deeper into the cause of these length discrepancies in a reliable manner (direct and indirect causes, risks, prognosis, etc.) but the fact is that the survival of patients suffering congenital cardiopathy may originate an increase in the number children with length discrepancies in the LL, with variable functional repercussions.
Carrying out these vascular procedures in newborns is necessary and vital for the diagnosis and treatment of their congenital heart pathologies; however, it is important to know not only the possible complications that may appear immediately, but also those that could arise in the long term.
Although vascular aetiology accounts for a small percentage of LL length discrepancies, the association observed in this and other studies highlights the importance of informing parents and primary care paediatricians about these potential complications. Therefore, it is advisable to carry out clinical and radiographic monitoring of patients who undergo femoral catheterisation in their early infancy, due to the risk of developing a length discrepancy in the lower limbs.
Ethical responsibilitiesProtection of people and animalsThe authors declare that this investigation did not require experiments on humans or animals.
Confidentiality of dataThe authors declare that they have followed the protocols of their workplace on the publication of patient data.
Right to privacy and informed consentThe authors declare that this work does not reflect any patient data.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Díaz-Ben B, Balvís-Balvís P, Lozano-Balseiro M, González-Herranz P. Discrepancia de longitud de los miembros inferiores tras canalización arterial en niños. Rev Esp Cir Ortop Traumatol. 2015;60:12–19.