The treatment of intertrochanteric fractures using a minimally invasive dynamic hip screw (MIDHS) technique has been reported to provide better results than the conventional technique (CDHS). The present study aims to determine whether there are any differences in terms of transfusion needs, morbidity, length of hospital stay, and economical costs, based on a study of two retrospective cohorts.
Materials and methodsCohorts study of 80 patients with intertrochanteric femoral fractures (31-A1 and 31-A2.1) who underwent DHS procedure from July 2005 to September 2007; 40 of them were treated using the traditional technique (CDHS), and the other 40 using the minimally invasive technique (MIDHS).
ResultsNo differences were found in terms of blood loss, transfusion requirements or morbidity. Mean hospital stay for MIDHS group was 1.3 days lower, reducing the costs regarding the CDHS group by €306.3, but this difference was not statistically significant (P=.3). The time required to perform the surgery was shorter for the MIDHS group: 49.3 versus 78.8minutes (p=0.0001).
DiscussionContrary to previous studies published, the present study did not show any advantage for the MIDHS technique, except for a shorter surgical time to perform the procedure. We consider that the MIDHS could help in improving operating room productivity and efficiency.
El tratamiento de fracturas pertrocantéreas con DHS mediante técnica mínimamente invasiva (MIDHS) ha mostrado resultados superiores a la técnica convencional (CDHS) en estudios previos. El presente estudio pretende determinar si existen diferencias en requerimientos transfusionales, morbilidad, estancia hospitalaria y en el coste asociado, a partir de un análisis retrospectivo de 2 cohortes.
Material y métodoEstudio de cohortes en 80 pacientes con fracturas intertrocantéreas de fémur (31-A1 y 31-A2.1) tratados con implante DHS entre julio de 2005 y septiembre de 2007: 40 de ellos con la técnica convencional y 40 de ellos con técnica MIDHS.
ResultadosNo se observaron diferencias estadísticamente significativas ni en la pérdida sanguínea, ni en requerimientos transfusionales, ni en morbilidad. La estancia hospitalaria en el grupo MIDHS fue 1,3 días menor, con un coste directo de 3,063€ por caso, inferior al grupo CDHS, aunque sin significación estadística (p=0,3). La duración de la intervención fue menor en el grupo MIDHS: 49,3 versus 78,8min (p=0,0001).
DiscusiónContrariamente a lo publicado en estudios previos, en el presente estudio la técnica MIDHS no ha mostrado ventajas excepto por requerir un menor tiempo para realizar la técnica. Consideramos que la técnica MIDHS podría ayudar en mejorar la productividad y eficiencia en el uso de quirófanos.
Intertrochanteric femoral fractures (AO 31-A1 and 31-A2.1)1,2 are very frequent among the elderly population. Thus, it is an increasingly common disease at our emergency services. These type of patients suffer a high number of complications, with long hospital stays and a high healthcare cost.3–5
The most common treatments used in these kind of fractures are endomedullary nailing and the sliding plate-screw system (dynamic hip screw [DHS], DePuy Synthes, Zuchwil, Switzerland), with both options being equally valid.6–9 Although the most recent reviews8 observed less bleeding and shorter duration of the intervention with endomedullary nailing, these differences were also attributed to the type of intertrochanteric fracture and the experience of the surgeon, thus making DHS a method to be taken into account for stable fractures.9–11 DHS has a reduced cost and, in recent years, minimally invasive techniques have been developed for its application (MIDHS).12,13 These have been related to a series of advantages, such as reducing blood loss and morbidity, optimizing and improving management and rehabilitation, and a reduction of hospital stay.13–19 In turn, this entails a reduction of the cost of treatment for these common fractures.
The objective of this study was to determine whether performing a MIDHS technique was associated to fewer blood transfusions, less morbidity, shorter hospital stay and a lower cost, based on a retrospective cohort study.
Materials and methodsWe present a retrospective study of 2 cohorts of patients with intertrochanteric femoral fractures who underwent osteosynthesis with a DHS system following the conventional method (CDHS) or the minimally invasive method (MIDHS), between July 2005 and September 2007. We included a total of 80 patients in the study: 40 were intervened through the MIDHS technique and the other 40 through the CDHS. The criteria for inclusion in the study were: (1) intertrochanteric femoral fractures 31-A1 and 31-A2.1 (according to the AO classification)1,2; (2) age over 60 years; (3) autonomous walking prior to the fracture; (4) satisfactory closed reduction with radiographic control: 0°–10° valgus in an anteroposterior projection and <5° posterior angulation in a lateral projection. We excluded from the study any patients who did not fulfill these criteria.
Patients intervened with the MIDHS technique included all the cases operated with this technique in the previous 2 years. The 40 patients intervened with the CDHS technique were the first 40 consecutive cases who underwent operations with the conventional technique after July 2005. A total of 8 surgeons carried out all the procedures. Three of them performed the MIDHS technique, although their assignment was not randomized. The remaining 5 only performed the CDHS technique. Both groups of patients received intradural anesthesia. Patients were placed in the supine position in a Judet traction table.
The following epidemiological data were recorded for each case: age, gender, body mass index (BMI), laterality, presence of comorbidities and preoperative ASA score. In addition, we also recorded data on the surgical intervention: duration, blood loss calculated through the reduction in hemoglobin during the first postoperative day, blood transfusion rate, number of packed red blood cells transfused and hospital stay. Blood loss was calculated based on the difference between the level of hemoglobin upon admission and the analysis conducted on the first postoperative day.
We recorded the number of cases treated through a minimally invasive technique which had to be converted to an open technique due to difficulties during the intervention. We reviewed both the number of days of hospital admission, which included the period from admission until discharge, and also the days of hospital stay following the intervention, in order to reduce the bias associated to the variability of preoperative stay. We calculated the cost of admission of each group according to the mean daily cost of admission at our center for the studied period: a total of 235.62€/day. This calculation of daily cost only took into account the direct costs of admission, leaving out indirect and intangible costs. We also calculated the cost of the surgical time. Furthermore, we reviewed the rates of complications and reinterventions, considering a follow-up period of 12 months. There were no losses during follow-up in any of the 2 groups.
We followed the blood transfusion criteria of the general protocol for packed red blood cells at our center. According to the protocol, we decided to assess blood transfusion based on a hemoglobin level lower than 8g/dl or hematocrit lower than 24%. We did not carry out transfusion with hemoglobin values above 9g/dl or hematocrit above 27%. In cases with hemoglobin levels between 8 and 9g/dl or hematocrit between 24% and 27%, we transfused those patients who presented signs of hypoxemia or cardiovascular risk.
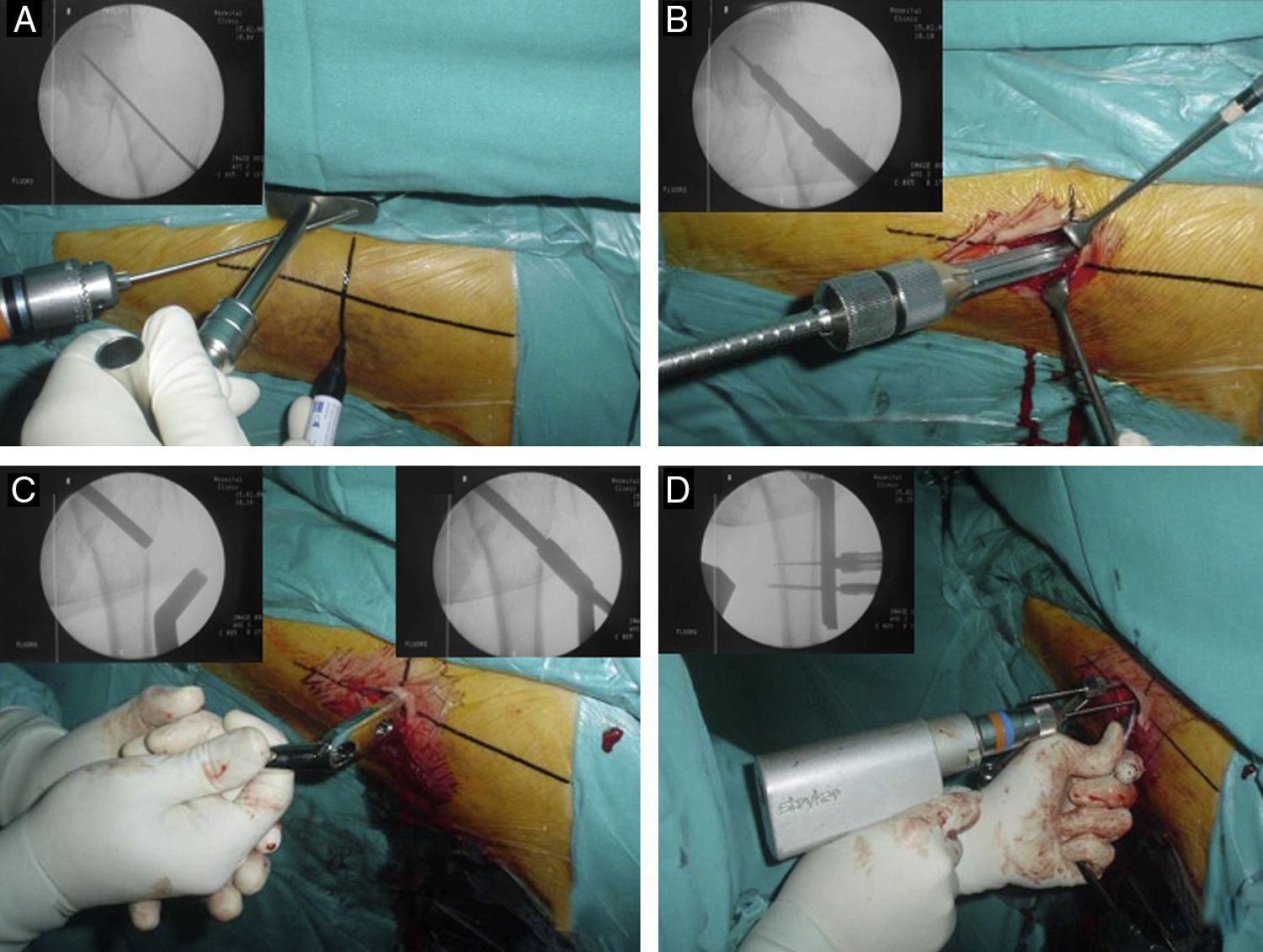
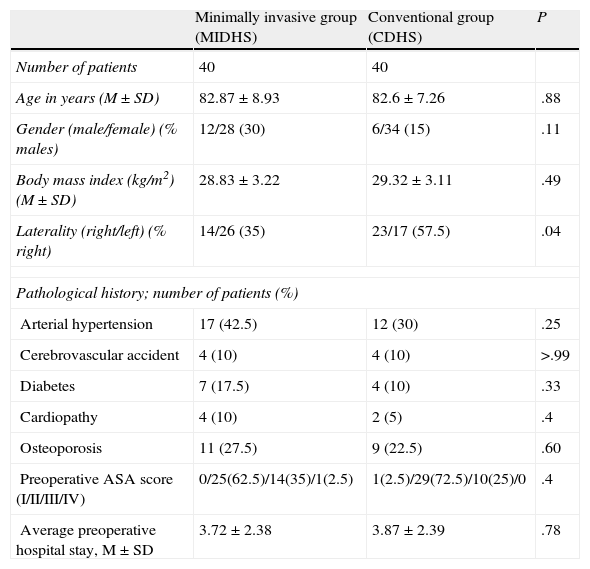
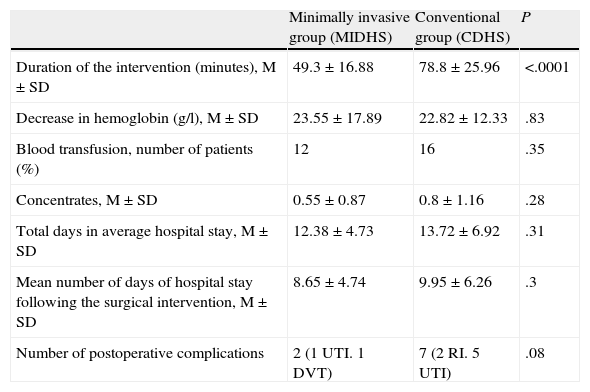
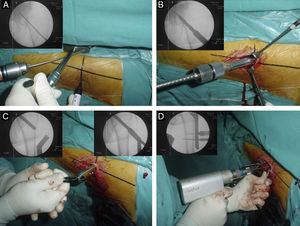
The MIDHS technique was applied according to the description by Alobaid et al.13 With the aid of scopy, the access references were marked with a pen. This was done by placing the 135° plate guide on the anterior side of the hip and ensuring that the guide was aligned with the lateral wall of the femur in the anteroposterior scopy projection (Fig. 1A), and parallel to the femoral diaphysis in the lateral projection. The skin incision could be carried out at this point. The fascia lata section and the trans-vastus lateralis dissection of the femur were carried out until the femoral diaphysis was located in its proximal edge. Next, the cephalic screw was placed after drilling (Fig. 1B) and then the 2 or 4 hole plate was put in position, sliding it under the vastus lateralis facing the exterior and, once inside, turning it 180° until it locked on the cephalic screw and was applied to the external cortical of the femur (Fig. 1C). Lastly, the cortical screws of the plate were placed (Fig. 1D). In our series, MIDHS incisions were between 3 and 4cm (Fig. 2).
Details of the MIDHS technique: (A) Determination of references; (B) drilling of the path of the cephalic screw with radiographic control; (C) placement of the plate with initial radiographic control and after turning it 180°, locking on the cephalic screw and (D) drilling of cortical screws.
In the CDHS technique, an approach of approximately 8–10cm was employed, placing it in the retro-vastus lateralis, applying a 4-hole plate directly into its definitive axis.16–19
In the medical history in electronic form we noted the first year of follow-up, with examinations at 1, 3, 6 and 12 months after the intervention to study the presence of clinical complications and alterations in the radiographic study (failure of the synthesis, consolidation delay or pseudoarthrosis) as well as the indication and performance of a reintervention for any reason.
In order to carry out the statistical study, the data were introduced into and analyzed with the software package OpenEpi version 3.0 (available at: http://www.openepi.com). The Kolmogorov–Smirnov test was used to determine whether the studied variables presented a normal distribution. We used the Student's t test to study continuous variables (age, BMI, duration of surgery, blood loss, transfused packed red blood cells, hospital stay); the χ2 test was used for dichotomous variables with a frequency over 5 (gender, history of pathology, ASA score, transfused patients, postoperative complications). The level of statistical significance was set at P≤.05.
ResultsBoth groups were comparable, with no statistically significant differences regarding age, gender, BMI, history of pathology and preoperative ASA score (Table 1). There were differences regarding the operated side, with more interventions on the right in the conventional groups than in the MIDHS group (P<.05), although this fact does not introduce any bias regarding the objectives of the study. None of the cases operated with the MIDHS technique had to be converted into a conventional technique.
Demographic data.
| Minimally invasive group (MIDHS) | Conventional group (CDHS) | P | |
| Number of patients | 40 | 40 | |
| Age in years (M±SD) | 82.87±8.93 | 82.6±7.26 | .88 |
| Gender (male/female) (% males) | 12/28 (30) | 6/34 (15) | .11 |
| Body mass index (kg/m2) (M±SD) | 28.83±3.22 | 29.32±3.11 | .49 |
| Laterality (right/left) (% right) | 14/26 (35) | 23/17 (57.5) | .04 |
| Pathological history; number of patients (%) | |||
| Arterial hypertension | 17 (42.5) | 12 (30) | .25 |
| Cerebrovascular accident | 4 (10) | 4 (10) | >.99 |
| Diabetes | 7 (17.5) | 4 (10) | .33 |
| Cardiopathy | 4 (10) | 2 (5) | .4 |
| Osteoporosis | 11 (27.5) | 9 (22.5) | .60 |
| Preoperative ASA score (I/II/III/IV) | 0/25(62.5)/14(35)/1(2.5) | 1(2.5)/29(72.5)/10(25)/0 | .4 |
| Average preoperative hospital stay, M±SD | 3.72±2.38 | 3.87±2.39 | .78 |
CDHS conventional dynamic hip screw technique; M: mean; MIDHS: minimally invasive dynamic hip screw technique; SD: Standard deviation.
The MIDHS technique required less time than the conventional technique, with a statistically significant difference (P<.0001). In the MIDHS group, the duration was of 49.3min (SD 16.88) while in the CDHS group, the duration was of 78.8min (SD 25.96). The mean cost of the intervention time has been calculated as 86.27€ for the MIDHS group and 137.9€ for the CDHS group. This represents a difference of 51.63€ between both techniques.
Nevertheless, we did not observe any statistically significant differences in blood loss between both techniques, as measured by the decrease in hemoglobin during the first 24h. Neither were the transfusion requirements different: 12 transfusions in the MIDHS group versus 16 in the CDHS group (P=.3). The details of the results are shown in Table 2.
Surgical data and clinical results.
| Minimally invasive group (MIDHS) | Conventional group (CDHS) | P | |
| Duration of the intervention (minutes), M±SD | 49.3±16.88 | 78.8±25.96 | <.0001 |
| Decrease in hemoglobin (g/l), M±SD | 23.55±17.89 | 22.82±12.33 | .83 |
| Blood transfusion, number of patients (%) | 12 | 16 | .35 |
| Concentrates, M±SD | 0.55±0.87 | 0.8±1.16 | .28 |
| Total days in average hospital stay, M±SD | 12.38±4.73 | 13.72±6.92 | .31 |
| Mean number of days of hospital stay following the surgical intervention, M±SD | 8.65±4.74 | 9.95±6.26 | .3 |
| Number of postoperative complications | 2 (1 UTI. 1 DVT) | 7 (2 RI. 5 UTI) | .08 |
CDHS: conventional dynamic hip screw technique; DVT: deep vein thrombosis; M: mean; MIDHS: minimally invasive dynamic hip screw technique; RI: respiratory infection; SD: standard deviation; UTI: urinary tract infection.
Postoperative complications on admission were minimal and very similar between both groups, with no significant differences. All patients followed a correct clinical course with the same rehabilitation protocol, allowing sitting at 24h and walking at 48h with a walking frame or 2 crutches, so there were no differences between both groups.
Based on the fact that the direct cost per day of hospital admission was 235.62€ per patient, we can calculate a mean cost of hospital stay of 2916.98±1114.48€ (12.38±4.73 days of average stay, as shown in Table 2) for the MIDHS group compared to 3232.7±1630.49€ (13.72±6.92 days) for the CDHS group. In order to avoid introducing possible bias by differences in preoperative waiting time, the calculation of the average hospital stay following the surgical intervention did not show differences between groups. The MIDHS group had a mean cost of 2038.11±1116.83€ (8.65±4.74 days), while for the CDHS group it was 2344.42±1474.98€ (9.95±6.26 days). Therefore, the difference in average postoperative stay between both groups was 1.3 days shorter for the MIDHS group, which could represent savings of 306.3€ per case compared to the CDHS group, with no statistical significance.
We did not detect any cases with a delay of consolidation, pseudoarthrosis or any other complications during follow-up which required reintervention for any reason during the first year in either of the 2 groups.
DiscussionGiven the high frequency of pertrochanteric fractures in our environment, there is considerable interest in constantly assessing the benefits and drawbacks of the various surgical techniques. The current study shows results which are contrary to previous reports: neither a higher rate of transfusions nor greater complications in one group compared to the other.
Several prospective and randomized studies have compared both techniques.13,16–21 Alobaid13 was one of the pioneers in the technique of MIDHS. In his work, in addition to describing the technique step by step, he explained the reason why the area described was safe from the vascular standpoint and carried out a study on 48 patients, observing less bleeding and shorter duration of the intervention in favor of MIDHS with statistically significant differences (P<.001), as well as a trend toward less analgesic requirements (P>.05). In a study on 13 patients, Waters19 also observed less bleeding, introducing the possibility that this could entail a better clinical evolution of these patients. A recent meta-analysis by Cheng et al.22 assessed 6 previous studies, 4 on cases and controls and 2 retrospective and comparative. After the analysis, these authors concluded that the MIDHS technique was associated to less bleeding, shorter hospital stays, less pain and tissue damage and improved rehabilitation and mobility. No differences were reported regarding complications. Cheng et al. also reported on the perioperative benefits of the MIDHS technique compared to the conventional method.
In our study we did not observe significant differences regarding hospital stay. We currently know that this aspect does not only depend on a specific surgical technique, but is rather a matter of multidisciplinary approach and management, in what is currently known as fast track recovery, as proven by multiple studies of total knee and hip arthroplasties.23 On the other hand, after conducting a direct cost analysis, we have not observed any significant differences. The only advantage observed has been a shorter time required for the intervention, with a marked difference of nearly 28min for each operation (P=.0001). Since we have not observed any differences in morbidity and complications during the first year, we consider that the use of the MIDHS technique is still justified, as it can result in an optimization of the productivity and efficiency of surgery rooms.
Regarding other related minimally invasive techniques with more modern implants, such as the PCCP® plate (Orthofix, Verona, Italy) and the Traumax® plate (Integra, Saint Priest, France), we have also observed a reduced risk of bleeding compared to the use of endomedullary nails and DHS plates through a conventional approach.24–26 To the best of our knowledge, there are no studies comparing these implants with the DHS applied through minimally invasive technique. We consider this would be very interesting, since there is a notable difference in the cost of these implants compared to the traditional DHS plate.
The main limitation of our study was its retrospective nature, with a lack of randomization. Another limitation would be the inclusion of only those patients with a previous capacity for walking, as this group of patients tends to associate lower comorbidities: the MIDHS technique could have presented advantages in more complex patients, and this aspect has not been studied. Lastly, the third limitation we wish to point out is the absence of an assessment of indirect costs and costs following discharge. We consider that the main strengths of this study are the strict application of the technique described by Alobaid et al.13 in all cases, limiting the technique to 3 surgeons (thus decreasing variability), the existence of a complete follow-up of all patients, and the fact that all underwent the same transfusion and rehabilitation protocol in the postoperative period.
As conclusion, in the present study, the MIDHS technique has not presented advantages compared to the conventional method regarding risk of bleeding, morbidity, hospital stay and direct costs. Nevertheless, we have observed a reduction of the time required for the intervention, which could entail an improvement in productivity and efficiency in the use of operating rooms.
Level of evidenceLevel of evidence III.
Ethical responsibilitiesProtection of people and animalsThe authors declare that this investigation did not require experiments on humans or animals.
Confidentiality of dataThe authors declare that they have followed the protocols of their workplace on the publication of patient data and that all patients included in the study received sufficient information and gave their written informed consent to participate in the study.
Right to privacy and informed consentThe authors declare having obtained written informed consent from patients and/or subjects referred to in the work. This document is held by the corresponding author.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Méndez-Gil A, Fernández-Valencia Laborde JÁ, Estrada-Masllorens JM, Plaza-García R, Ríos Martín M, Camacho Carrasco P, et al. Técnica DHS mínimamente invasiva: Menor tiempo quirúrgico con similares resultados en el postoperatorio inmediato respecto al DHS convencional. Estudio retrospectivo de cohortes. Rev Esp Cir Ortop Traumatol. 2014;58:351–356.