The aim of this study was to evaluate the long-term results of the surgical treatment by means of open reduction and internal fixation of displaced supracondylar humerus fractures in a paediatric population.
Patients and methodsDescriptive retrospective study conducted between 1996 and 2003, which included 21 patients who underwent open reduction and internal fixation for the treatment of displaced, supracondylar humerus fractures according to the Gartland classification, which were irreducible by closed methods. The patients were clinically evaluated according to the Flynn criteria (functional and cosmetic). Data collection also included postoperative radiological evaluation, range of movement, the presence of post-operative complications, and a questionnaire on satisfaction with treatment received. The mean age of the patients was 5.8 years. Mean follow-up was 11.52 years.
ResultsThe average post-operative Baumann angle was 17.6°. Final loss of flexion averaged 5.1° (range: 0–20°), and loss of extension 0.71° (range: 0–10°), with 90% of patients demonstrating an elbow range of movement within normal limits. According to the Flynn criteria, functional and cosmetic results were satisfactory in 85.5%. Superficial wound infection and metal work migration were the most common post-operative complications. At the final follow-up all patients, except two, were very happy with the result, and no patient complained of difficulties in carrying out normal living activities or their favourite sports.
ConclusionsIn cases of unsatisfactory reduction or failure to maintain a stable closed reduction, open reduction and internal fixation demonstrate equivalent results to closed procedures.
Evaluar el resultado a largo plazo del tratamiento quirúrgico mediante reducción abierta y fijación interna de las fracturas supracondíleas de húmero desplazadas en la edad pediátrica.
Pacientes y metodologíaEstudio descriptivo retrospectivo sobre 21 pacientes, con una edad media de 5,8 años, intervenidos mediante reducción abierta y fijación interna entre los años 1996-2003 por presentar fractura supracondílea de húmero desplazada según clasificación de Gartland, no reductible por métodos cerrados. Los pacientes fueron valorados según criterios de Flynn (estético y funcional). También fueron evaluados los parámetros radiográficos, complicaciones, rango de movilidad y valoración subjetiva del paciente. El seguimiento medio fue de 11,52 años.
ResultadosUn ángulo de Baumann medio de 17,6° reflejó una satisfactoria reducción postoperatoria de la fractura. Al final del seguimiento, según criterios de Flynn se obtuvieron resultados satisfactorios en el 85,8% de los pacientes. El déficit medio de flexión fue de 5,1° (rango: 0-20°), y de extensión de 0,71° (rango: 0-10°). El 90% de los pacientes presentaron un rango de movilidad del codo con valores dentro de la normalidad. Las complicaciones más frecuentes fueron la infección superficial y la protrusión de las agujas. Al final del seguimiento todos los pacientes menos 2 refirieron estar bastante o muy contentos con el resultado. Ningún paciente refirió dificultades para la realización de sus actividades de la vida diaria, ni para la práctica deportiva.
ConclusionesEn casos de reducción insatisfactoria o fallo para mantener una reducción estable por métodos cerrados, la reducción abierta demuestra resultados comparables al quirúrgico cerrado.
Supracondylar fractures of the distal humerus are the most common fractures of the upper limbs in paediatric age, accounting for 75% of all distal humerus fractures in children. Most occur on the left side, among children aged between 5 and 7 years and with a predominance of males.1–4
The fracture line can affect the entire distal humerus and extended towards both columns, lateral and medial. It is determined by the position of the forearm with respect to the arm at the time of the fall. In over 95% of cases, the fracture takes place by a “hyperextension” mechanism, with a fall and landing on a hand in dorsiflexion and extended elbow. Fractures occurring by a “hyperflexion” mechanism, with a fall and a flexed elbow, are less common, representing less than 5% of all fractures.5–8
The classification of supracondylar fractures of the distal humerus is derived from that described by Reich in 1936, who originally classified them according to whether they followed a “T-shaped” or a “Y-shaped” line. Subsequently, the AO-ASIF (Association for the Study of Internal Fixation) presented a classification based on the fracture pattern and degree of comminution.9 At present, the most commonly used classification is that described by Gartland in 1959, which is prognostic and also establishes treatment recommendations.10 According to this classification, type I fractures are non-displaced fractures in which the full periosteum is preserved. Theoretically, type II fractures only maintain an intact posterior cortical which acts as a hinge, and type III fractures present total displacement, without cortical contact. Based on the series published by Leitch et al., Omid et al. conducted a review of some concepts regarding the treatment of supracondylar humerus fractures in children, thus defining a new type IV not described by Gartland: displaced supracondylar fractures in hyperextension with multidirectional instability, both in flexion and extension. In addition, they also commented on treatment implications.2,11
The goal of treatment of supracondylar fractures of the distal humerus in children is to achieve anatomical reduction of the fracture, in order to prevent the appearance of angular deformities in the long term. In general, conservative treatment is the first choice for type I fractures and surgical treatment is employed in the remaining types.2
Closed reduction combined with percutaneous fixation has become the treatment of choice for displaced supracondylar fractures in children, due to the better results obtained. However, in most published studies, groups undergoing open reduction usually received this treatment due to previous failure in achieving reduction by closed methods. In other words, patients undergoing open reduction generally turned out to be those with complex fractures.6,9,12,13
The aim of our study was to evaluate the long-term results of surgical treatment by open reduction and internal fixation of displaced supracondylar humerus fractures, according to the Gartland classification.
Patients and methodologyThis was an observational, descriptive and retrospective study conducted at the Department of Orthopaedic Surgery and Traumatology of Hospital Virgen de la Salud in Toledo, Spain, on patients aged less than 14 years who underwent open reduction and internal fixation between 1996 and 2003, due to displaced supracondylar fractures of the distal humerus. A total of 52 open surgical procedures were performed on 51 patients during this period.
We included patients who underwent open reduction and internal fixation due to failure of the treatment by closed methods or to the development of neurovascular complications following reduction manoeuvres. We excluded patients older than 14 years at the time of surgery (approximate age of epiphyseal closure of the distal humerus and olecranon), those who had suffered previous or accompanying injuries which may have affected elbow functionality, those who underwent a surgical technique other than the one being reviewed in this study and those who could not be located.
Out of the 51 patients initially included in the study, 9 were not located with the personal data available, 17 patients did not attend follow-up meetings on several occasions and in 4 cases we had no evidence of closed reduction being attempted previously. Therefore, the final number of patients who were located and who met the inclusion criteria was 21. We collected demographic data including gender, age, anthropometric characteristics, mechanism and causes of injury, associated injuries, as well as information on the surgical intervention and postoperative recovery, through the application of a protocolised questionnaire. During the interview on the subject of this study, we performed a radiological examination and also collected clinical data and information on the exploration of the operated joint. These included the range of motion using a universal goniometer, chronic residual instability using joint stress manoeuvres (lateral test for the diagnosis of posterolateral instability and valgus stress test for medial instability),14,15 and measurement of pain using a visual analogue scale (VAS).
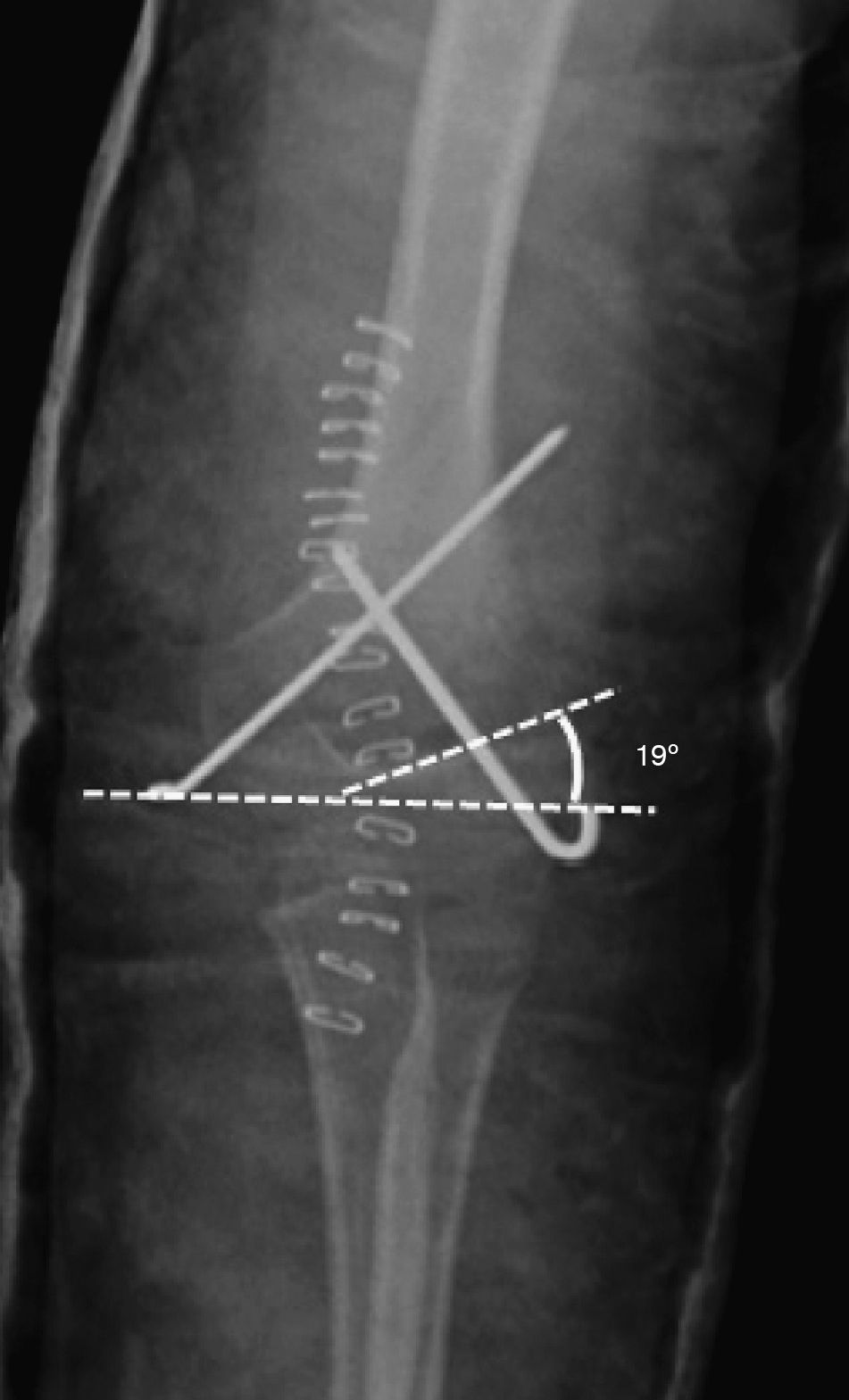
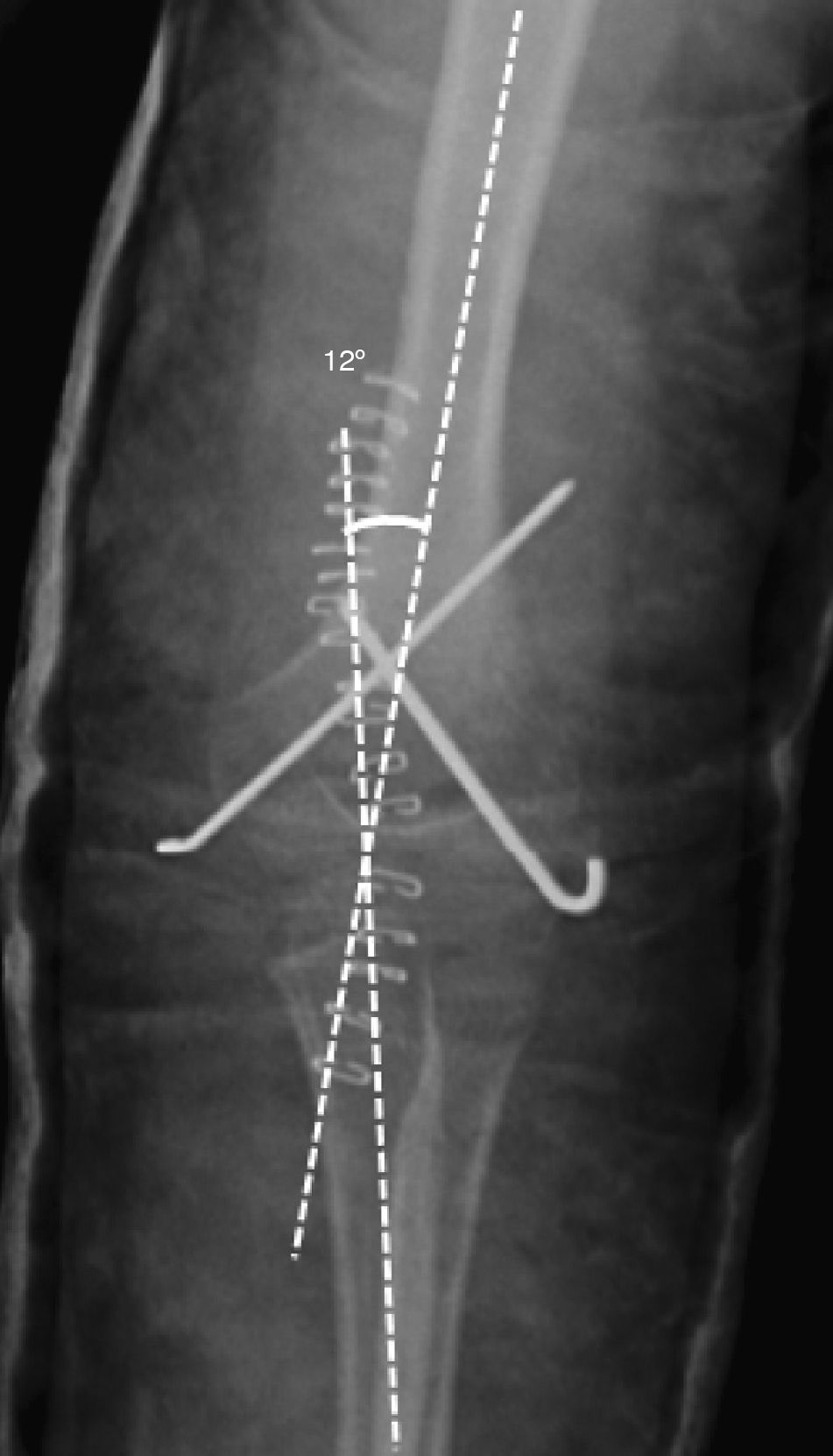
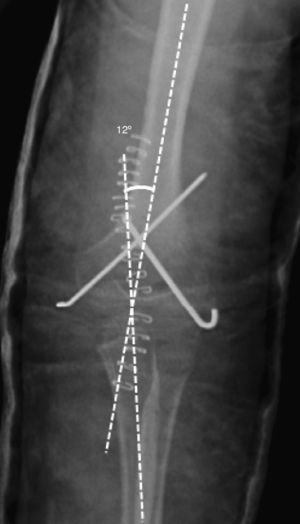
All fractures were classified according to the Gartland scale through the evaluation of preoperative radiographs. In order to evaluate fracture reduction, we calculated the “Baumann angle”16 from postoperative radiographs (Fig. 1). This angle is formed by the perpendicular of the humeral longitudinal axis with respect to the axis of the physeal line (normal range: 9–26°).15–18 We also measured the “humeral-ulnar angle” (load angle) in the radiographs obtained at the end of the follow-up period regarding this study (Fig. 2). This is the angle between the humeral diaphyseal axis with respect to the ulnar diaphyseal axis (normal load angle: 13±6°).19,20
Humeral-ulnar angle (load angle): measures the obliquity between the arm and forearm in extension and supination. It is used in the radiological assessment at the end of the follow-up period. It represents the angle formed by the diaphyseal axis of the humerus with respect to the diaphyseal axis of the ulna (normal load angle: 13±6°).
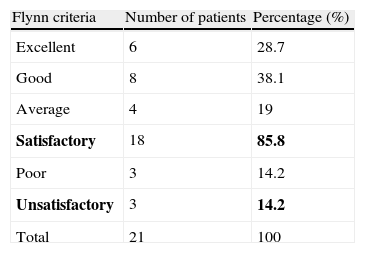
All patients were assessed according to the Flynn criteria,6,21,22 which evaluate both the functional and the aesthetic result. The aesthetic component considers the load angle and its deviation towards varus or valgus, whereas the functional component is assessed by measuring flexion and extension. The lesser of the 2 results (aesthetic and functional) is considered the overall result. “Excellent”, “good” and “average” results were considered satisfactory (these reflected a loss of load and mobility angle between 0–5°, 6–10° and 11–15°, respectively), while “poor” results (loss>16°) were considered unsatisfactory. A result with cubitus varus was automatically considered a “poor” result.
We also collected the subjective index of patient satisfaction (very satisfied, satisfied, neither satisfied nor disappointed, somewhat disappointed, very disappointed), and the presence of difficulties in performing activities of daily living in relation to the fracture.
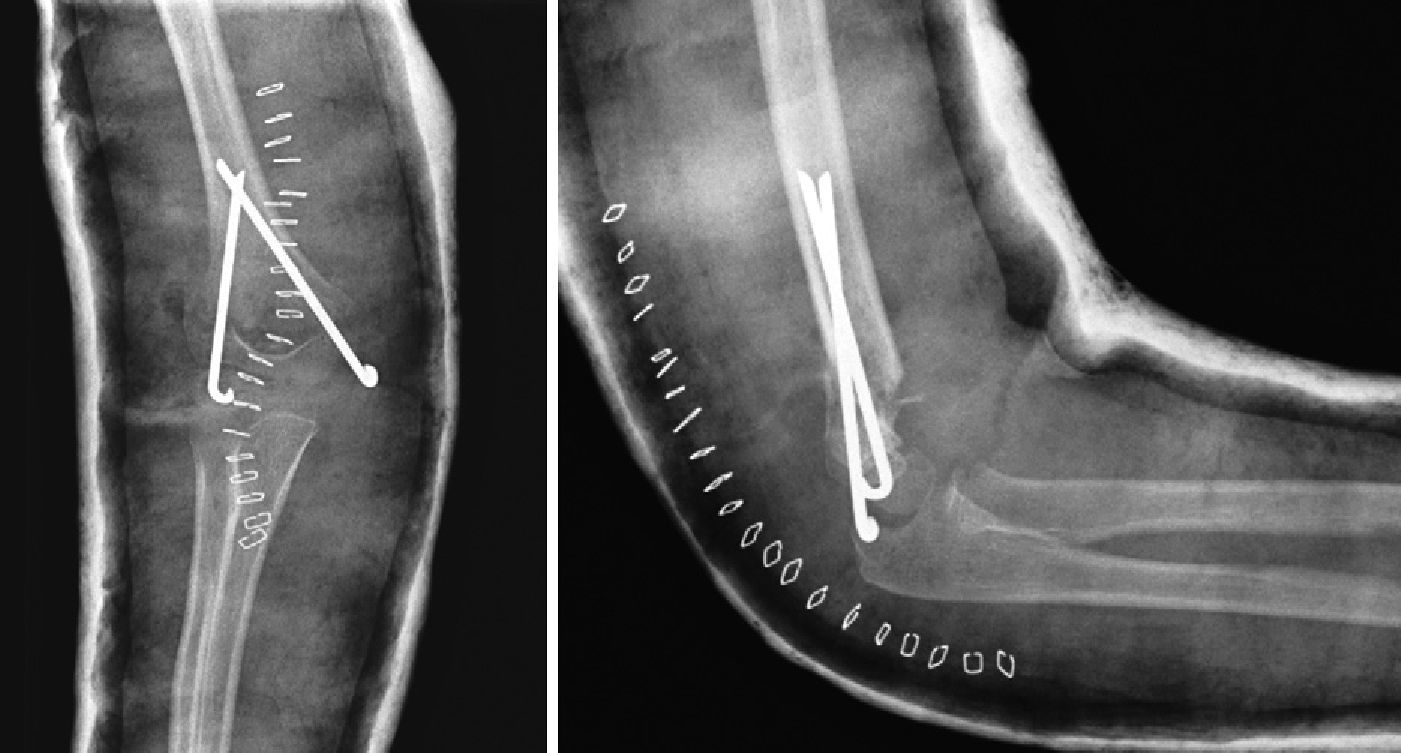
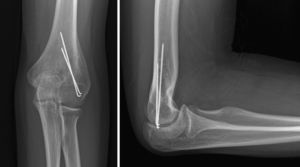
Regarding the surgical technique, all patients underwent open reduction and internal fixation with Kirschner wires or with Rush-type, crossed intramedullary nails. We used a posterior approach with neurolysis of the ulnar nerve and osteotomy of the olecranon through a single section of the tip of the cartilaginous epiphysis using a cold scalpel, and partial detachment of the triceps in a “V” shape with the vertex at the olecranon cartilage being included, exposing the posterior side of the humerus for the reduction and synthesis of the fracture. Closure of the olecranon osteotomy was performed by careful approach and suture of the cartilaginous edges of the osteotomy. In order to avoid prominence of the osteosynthesis material upon the start of elbow mobilisation, we impacted needles or nails on the cortex of the distal humerus, covered by skin.
In all cases, the operated limb was immobilised with a brachio-palmar cast or splint during 4–6 weeks. The osteosynthesis material was removed after the eighth or ninth week (Fig. 3).
The results were collected in an Excel database and statistically analysed using the computer software for statistical analysis SPSS®. We established a value of P<.05 as statistically significant difference between groups.
We used the Pearson correlation coefficient to measure the linear relationship between the result obtained after reduction of the fracture and the postoperative result after the follow-up period. We also used the Student t test to study the relationship between the severity of the fracture and postoperative and final radiological results.
ResultsOf the 21 patients included in the study, 14 were males (66.7%) and 7 were females (33.3%), with a mean age of 5.8 years (range: 2–13 years). The injured elbow was the right in 10 cases (47.62%) and the left in the remaining 11 cases (52.38%), being the dominant arm in 13 cases. The mean follow-up period at the time of the review was 11.52 years (range: 8–15 years). Regarding the mechanism of injury, it was difficult to assess how the fracture occurred, given the young age of the patients at the time of trauma. Most took place due to falls from own height, slides or off a bicycle.
According to the Gartland classification, 38% (n=8) of cases corresponded to type II, and 62% (n=13) to type III. Of this total, only 1 fracture was open. In terms of lesions associated to hospital admission, 3 cases presented no radial pulse, although it was recovered after surgery in all cases, without the need for surgical vascular exploration. In 1 patient we noticed an association with Salter and Harris type II epiphysiolysis of the proximal phalanx of the third and fourth fingers of the ipsilateral hand.
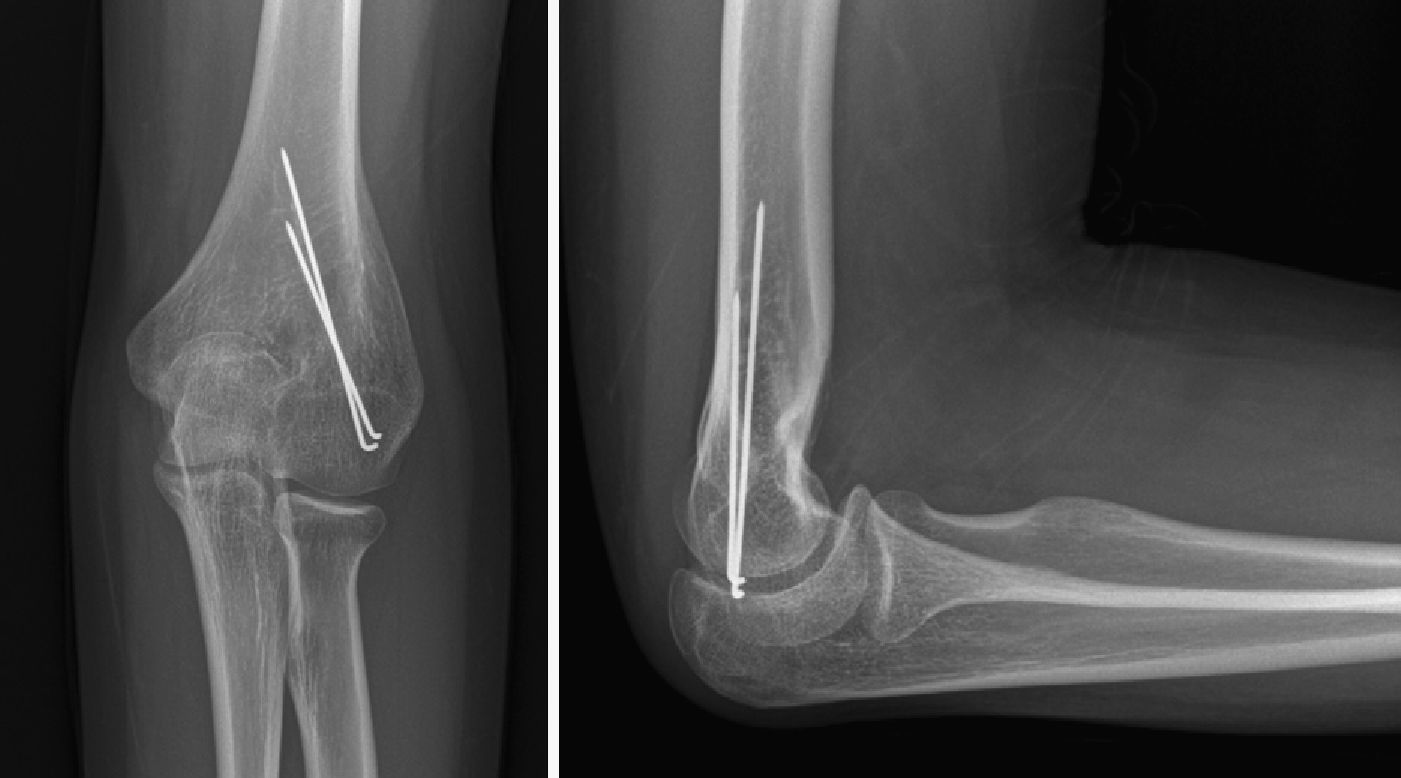
The mean Baumann angle, as measured in the immediate postoperative radiographs, was 17.61° (range: 12–22°). The mean time elapsed until a satisfactory range of elbow motion was recovered was 3.6 months (range: 1–10 months). Patients who showed less collaboration during active exercises, 28.5% in total (n=6), were referred to rehabilitation to regain range of motion. The mean time elapsed until the removal of osteosynthesis material was 6.2 months (range: 2–17 months). In 1 case it was not possible to carry out the removal of osteosynthesis material, given the difficulties encountered during surgery, which advised against this extraction (Fig. 4).
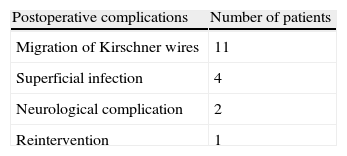
Regarding postoperative complications, 52.38% of patients (n=11) presented some degree of distal migration of the intramedullary nails. Four patients developed a superficial wound infection. There were 2 cases of postoperative neurological complications: 1 patient suffered neuropraxia of the median nerve and 1 patient suffered a mixed paresis of the median and ulnar nerves. Recovery from neurological involvement was complete and spontaneous in both cases. There were no cases of deep infection, Volkman's ischaemic contracture, pseudoarthrosis or myositis ossificans. Finally, 1 patient had to be reoperated due to a deficit in the initial reduction (Table 1).
Postoperative complications.
| Postoperative complications | Number of patients |
| Migration of Kirschner wires | 11 |
| Superficial infection | 4 |
| Neurological complication | 2 |
| Reintervention | 1 |
In 11 patients we observed some degree of distal migration of the intramedullary nails, 4 patients developed superficial wound infection, 2 suffered postoperative neurological complications and 1 patient had to undergo reintervention due to a deficit in the initial reduction. We found no cases of deep infection, Volkman ischaemic contracture, pseudoarthrosis or myositis ossificans.
At the end of the follow-up period, joint stress manoeuvres did not demonstrate instability of the intervened elbow in any patient. Pain measured by VAS showed a mean value of 1.28 (range: 0–7) over a maximum of 10 points. A total of 5 patients (23.8%) reported elbow discomfort in relation to efforts, and only 1 patient expressed pain at rest, occasionally and only in relation to “certain positions”. No patient expressed the existence of any limitations to perform activities of daily living, for the normal development of their profession or for sports.
According to Flynn's criteria, we obtained satisfactory results in 85.8% (95% CI) of patients (n=18). Thus, when analysing the aesthetic factor (loss of load angle) independently, 70% of patients presented a result within the range considered as normal (Table 2). When analysing the functional factor independently, 90% of patients presented a range of elbow motion with values within the range considered as normal (flexion: 140–160°; extension: (−10)–0°; pronation: 80–90°; supination: 80–90°).23,24
The mean deficit at the end of the follow-up period was 5.1° for flexion (range: 0–20°), 0.71° for extension (range: 0–10°), 0.83° for pronation (range: 0–35°) and 2.85° for supination (range: 0–20°). The patient who underwent reintervention presented the range of motion farthest from normal values, particularly for flexion and pronation (−20° and −35°, respectively). According to the measurement of load angle or humeral-ulnar angle on radiographs obtained at the end of the follow-up period, there were 4 cases of cubitus valgus (19.04%), with a final mean valgus for the group of 11.85° (range: 4–30°).
We studied the possible linear relationship between the result obtained after the postoperative reduction of the fracture (immediate postoperative Baumann angle) and the result after follow-up (load angle at the end of follow-up). We could not demonstrate a direct relationship (r=0.302) between the radiographic findings of both angles. However, the results did show a trend towards a positive relationship. We believe that an increased sample size would have probably led to a direct association linking both angles.
We could not find statistically significant differences between the severity of the fracture according to the Gartland classification (type II or type III), and the postoperative and final radiological result (postoperative Baumann angle and load angle at the end of follow-up). Therefore, we could not establish that the postoperative and final radiological results (Baumann and load angles) were different depending on the severity of the fracture according to the Gartland classification (P=.751).
Similarly, we also studied the relationship between the severity of the fracture according to the Gartland classification and the final functional result (including all variables independently). We found no significant results (P>.05), except for the extension values (P=.047).
Regarding the overall satisfaction levels, 19 patients reported being satisfied or very satisfied with the final result of the surgical treatment of their fracture. One patient was neither satisfied nor disappointed, and 1 patient reported being somewhat disappointed, but not so much by the functional/aesthetic results as by the treatment received during the follow-up period. No patient reported any limitations to perform activities of daily living, for the normal development of their profession or for sports. This translated into an excellent/good level of satisfaction in 90.47% of cases.
DiscussionTreatment of distal humerus supracondylar fractures in children should aim to achieve anatomical reduction, maintain a stable reduction, restore joint function and prevent the appearance of long-term angular deformities. Thus, orthopaedic treatment is generally established as the first option for Gartland type I fractures, whilst open or closed surgical treatment is reserved for types II, III (and IV), in order to prevent a defective consolidation.2
Closed reduction plus percutaneous fixation has become the treatment of choice due to the superior results obtained. The main arguments employed by those authors25,26 who manifest a preference for an initial surgical treatment by open reduction and internal fixation are: direct visualisation of the open anatomical reduction, the risk of ulnar nerve injury due to the use of crossed percutaneous nails and a theoretically less stable fixation by the single use of lateral percutaneous nails (systems with 2 or 3 nails). However, in the last decade, closed reduction plus percutaneous fixation with Kirschner wires has become the treatment of choice for displaced supracondylar fractures in children, due to the better results obtained in open reduction and internal synthesis. These positive results, in terms of postoperative rigidity and cosmesis, have been reflected in the literature. Some authors even prefer less anatomical closed reductions, instead of opening the fracture. Nevertheless, in most of these studies,6,12,22,25,26 patients who underwent open reduction generally did so due to failure to achieve reduction or to maintain a stable reduction by closed methods, in the presence of neurovascular lesion after manipulation, significant oedema (fractures of several days duration) or in cases of open fractures, in order to perform primary lavage and debridement.22,26,27 In other words, generally, patients undergoing open reduction were also those whose fractures were more complex and in whom the final results would probably be less satisfactory than expected.
The Baumann angle has been established as a good indicator of postoperative reduction in the immediate postoperative analysis of radiological findings. All but 1 patient in this series (who was reoperated due to a deficit in primary reduction) presented a satisfactory Baumann angle. This reflects the correct postoperative anatomical reduction obtained, which is one of the main advantages offered by open reduction. In their study comparing closed and open reductions, Oh et al.25 published better results in the Baumann angle among the open group, although these differences were not significant. However, most published studies do not report such differences.27,28
Regarding functional outcomes, the literature reflects a rate of good results after open reduction ranging between 60% and 85%.12,25–27 In total, 90% of our patients presented excellent or good results. Flynn et al.21 recommended carrying out a separate analysis of the aesthetic and functional factors, arguing that a patient may suffer deformity but have a good function, and vice versa, suffer no deformity and have a poor function. The 4 cases of cubitus valgus (19.04%) in our series represented a slightly higher percentage than that reflected in the general literature.17 However, these 4 patients did present an adequate radiological reduction of the fracture, as demonstrated by measurements of the Baumann angle in the immediate postoperative period. This finding, together with the absence of evidence of a direct relationship between the Baumann angle and the load angle, might suggest the existence of some degree of remodelling of the distal humerus from the postoperative period until the end of growth. This hypothesis has also been noted by other authors.2,3,18
Elbow stiffness is another frequent sequela. In the present study we were not able to find statistically significant differences between the severity of the fracture according to the Gartland classification and the postoperative and final radiological outcomes, or with the functional outcome (P>.05). Soft tissue contusion, capsular fibrosis and age over 10 years have been described as some of the causes associated with the appearance of rigidity. Nevertheless, due to forceful manipulation, excessive attempts at manipulation or open reduction of the fracture (mainly through the posterior approach with detachment of the triceps as described by Hernandez-Ros), the surgery itself could be even more decisive in the appearance of rigidity28–30 than the severity of the fracture. Patients in this series underwent olecranon osteotomy with a single incision at the tip of the epiphyseal cartilage using a cold scalpel. The functional results obtained presented a satisfactory range of motion in 90% of patients, with a mean deficit of 5.1° in flexion and 0.71° in extension, comparable to closed treatment series.
The most important postoperative complications resulting from treatment of this fracture are neurovascular injuries. According to the literature, these affect the radial artery in up to 15% of cases, whilst nerve involvement takes place in 10–20% of cases, with most of them being neuropraxia which recovers favourably without the need for treatment.2,31,32 In our series, 1 patient suffered neuropraxia of the median nerve and 1 patient suffered mixed neuropraxia of the median and ulnar nerves. Both of them recovered spontaneously in the months following surgery. Another early and frequent complication is superficial infection. In our series, the 4 patients who presented superficial wound infection (19%), represented a slightly higher infection rate than that found in the literature.12,26,27 Nevertheless, all cases were resolved with oral antibiotic therapy. Undoubtedly, the most common complication in our series was migration of the osteosynthesis material, as over 50% of patients suffered some degree of migration, possibly related to a delay in removal. Despite its subcutaneous location, some resources which could be employed to prevent distal migration of the osteosynthesis material include penetration of the contralateral cortical upon introduction of nails, the use of threaded nails and insertion of part of the nails outside the skin, for an easier removal after fracture healing.
The present series offered radiological, clinical, functional and subjective satisfaction results which were comparable to those in series employing closed surgical treatment. Although we express our preference for closed reduction and synthesis methods as a first option, we also advocate open reduction in cases of unsatisfactory reduction or failure to maintain a stable reduction by closed methods. We find no justification to accept inappropriate reductions “in order not to open the fracture”, as argued by some authors.
Our study does have a number of limitations, such as the size of the sample, being a retrospective study with a high loss of patients, not performing a comparative study with other techniques or methods of treatment and not investigating the potential clinical and radiological impact of an osteotomy through the epiphyseal cartilage of the olecranon. In addition, the study only presents data from the review of long-term results of surgical treatments.
Ethical responsibilitiesProtection of people and animalsThe authors declare that this investigation did not require experiments on humans or animals.
Confidentiality of dataThe authors declare that they have followed the protocols of their workplace on the publication of patient data and that all patients included in the study received sufficient information and gave their written informed consent to participate in the study.
Right to privacy and informed consentThe authors declare having obtained written informed consent from patients and/or subjects referred to in the work. This document is held by the corresponding author.
Level of evidenceLevel of evidence IV.
Conflict of interestsThe authors have no conflict of interests to declare.
The authors wish to thank Dr. Enrique Gil Garay for his cooperation in the elaboration and development of the manuscript.
Presented at the 48th National Congress of the Spanish Society of Orthopaedics and Traumatology. SECOT. Oviedo, Spain. September 2011.
Please cite this article as: Holgado Moreno E, et al. Revisión de los resultados a los 10 años del tratamiento quirúrgico de las fracturas supracondíleas de húmero en el niño, tratadas mediante reducción abierta y fijación interna. Rev Esp Cir Ortop Traumatol. 2012;56:361–8.