To analyze the exposure of two Orthopedic Surgeons to ionizing radiations in their daily work, and to review the main national and international recommendations on this subject.
Material and methodsA retrospective study was conducted on the surgical treatments that use fluoroscopy performed by two orthopedic surgeons during a one year period. An evaluation was made of the radiation received, based on measurements of the processes published in the bibliography section. A literature review of international recommendations and regulations is also presented.
ResultsThe radiation received by the two orthopedic surgeons during one year did not exceed the limits of present-day legislation or the new European and international recommendations. The exposure was asymmetrical, with the hands being the most radiated part. The new recommendations reduce the permitted level of radiation on eyes.
DiscussionThe evaluation of the radiation received demonstrates the need for radiation protection, paying particular attention to the hands and eyes. Good knowledge of operating a fluoroscope and radiation safety measures are also essential.
Analizar la exposición a radiaciones ionizantes por parte de dos cirujanos ortopédicos en su práctica diaria y revisar las principales recomendaciones nacionales e internacionales al respecto.
Material y métodoSe efectúo un estudio retrospectivo de la actividad quirúrgica con uso de fluoroscopia realizado por dos cirujanos ortopédicos en un año. Se calculó la radiación recibida basándose en mediciones por procesos publicados en la bilbliografía. Revisión bibliográfica de recomendaciones y normativas internacionales.
ResultadoLa radiación recibida en un año por los dos cirujanos ortopédicos no sobrepasó el límite de la legislación actual ni el de las nuevas recomendaciones europeas e internacionales. La exposición fue asimétrica, siendo las manos la zona más radiada. Las nuevas recomendaciones rebajan los niveles permitidos de radiación en ojos.
DiscusiónLa estimación de radiación recibida hace necesario proteger y vigilar especialmente las manos y los ojos. Son necesarios conocimientos del funcionamiento del fluoroscopio y de las medidas de radioprotección.
It has been demonstrated that exposure to X-rays has harmful effects for orthopedic traumatologists, increasing the incidence of several types of tumors,1 as well as non-tumoral involvement, mainly in the hands2 and eyes.3
Over the past decade, the use of fluoroscopy has increased exponentially in operating rooms, with this increase being clearly observed in our specialty following the rise of minimally invasive traumatology procedures. However, we believe that the level of knowledge about the operation of fluoroscopes, the radioprotection measures and the availability of appropriate insulation and dose meters are significantly insufficient in our profession. Moreover, we consider that there is an underestimation of the radiation emitted by the fluoroscopy arches and miniarches, perhaps due to an assumption that their being modern and digital reduces the levels of radiation they emit, which is not true.
The aim of this work is to warn about the harmful consequences of radiation derived from the use of fluoroscopes in operating rooms, expose common practices which are not safe and highlight the need for adequate radioprotection measures, as well as to promote their use.
Materials and methodsWe conducted a retrospective study of interventions performed with the aid of fluoroscopy by the two first authors, recording the number of total procedures and the type of procedures, as well as those conducted as first surgeon and as second. In all cases, the device employed was a standard fluoroscope (Philips Lybra, Andover, MA, US). In terms of commercial availability, there are standard arch fluoroscopes and those with a reduced arch (miniarches). Both consist of an X-ray emitter and an image intensifier connected by a mobile arch. The standard fluoroscope leaves a free space of approximately 80cm between the Rx tube and the image intensifier, whereas in the mini arch, this space is around 30cm. The Rx tube in standard arches can develop greater electric potentials, kilovolts (kV), and electrical intensities, milliamps (mA). This enables images to be obtained throughout the entire anatomy. However, when both are used on small joints in automatic mode they operate at similar kV and mA levels. The reduction of disperse radiation of the mini arch in C compared to the standard arch is mainly due to the greater proximity between the Rx tube and the image intensifier.
Radiation doses are measured using the concepts of effective dose and equivalent dose. The effective dose is a quantitative indicator of the probability that a stochastic effect may take place, generally cancer, and corresponds to the addition of the equivalent doses weighed in all the tissues and organs of the body. The equivalent dose is a physical magnitude of the radiation absorbed by the body modified according to the biological effect of the type of radiation. The measurement unit used is the milliSievert (mSv).
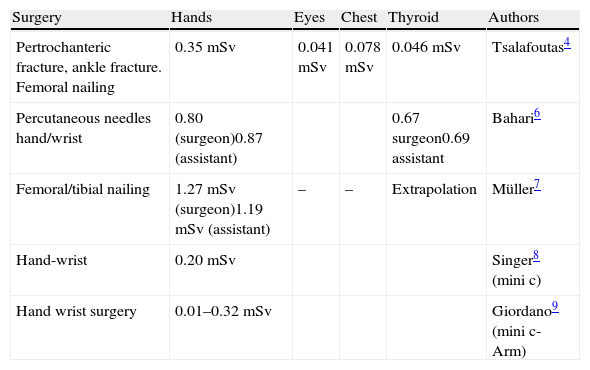
We calculated the equivalent doses received by the two authors based on the estimations of radiation per process conducted by Tsalafoutas et al.4 The estimation in this work was similar to those obtained by different authors in tests with cadavers or using various dose meters in conventional interventions with standard arches or miniarches5–9 (Table 1). In our study, we divided the procedures performed into various groups, according to the technique and anatomical location, although we estimated the mean dose calculated by Tsalafoutas for any of them.
Measurement of radiation by different authors.
| Surgery | Hands | Eyes | Chest | Thyroid | Authors |
| Pertrochanteric fracture, ankle fracture. Femoral nailing | 0.35mSv | 0.041mSv | 0.078mSv | 0.046mSv | Tsalafoutas4 |
| Percutaneous needles hand/wrist | 0.80 (surgeon)0.87 (assistant) | 0.67 surgeon0.69 assistant | Bahari6 | ||
| Femoral/tibial nailing | 1.27mSv (surgeon)1.19mSv (assistant) | – | – | Extrapolation | Müller7 |
| Hand-wrist | 0.20mSv | Singer8 (mini c) | |||
| Hand wrist surgery | 0.01–0.32mSv | Giordano9 (mini c-Arm) |
We conducted a review of the main recommendations issued by national and international bodies, among which we highlight:
- -
IAEA (International Atomic Energy Agency)10 belonging to the international organizations connected to the United Nations. Among other roles, it issues basic safety regulations for protection against radiation, and publishes guidelines and practice codes.
- -
ICRP (International Commission on Radiological Protection), a non-profit organization and independent scientific association which aims to foster the progress of the science of radiological protection for the public good. It periodically publishes scientific documents, including recommendations and guides covering all aspects of radiological protection.11,12
- -
Council of the European Union.13
- -
Current Spanish regulations on the protection of health against ionizing radiation.14
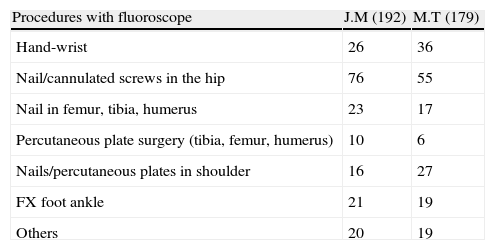
The authors M.T. and J.M. conducted 179 and 192 non-urgent interventions with a standard fluoroscope during the period between April 2012 and March 2013, both included. The majority corresponded to pertrochanteric, subtrochanteric or subcapital hip fractures treated with cannulated screws, which are the types of surgery producing the largest doses of disperse radiation. The section “others” includes forearm and elbow fractures in children, supracondylar humeral and forearm fractures in adults, etc. (see Table 2).
Surgical procedures with fluoroscopy conducted by the two authors in 1 year.
| Procedures with fluoroscope | J.M (192) | M.T (179) |
| Hand-wrist | 26 | 36 |
| Nail/cannulated screws in the hip | 76 | 55 |
| Nail in femur, tibia, humerus | 23 | 17 |
| Percutaneous plate surgery (tibia, femur, humerus) | 10 | 6 |
| Nails/percutaneous plates in shoulder | 16 | 27 |
| FX foot ankle | 21 | 19 |
| Others | 20 | 19 |
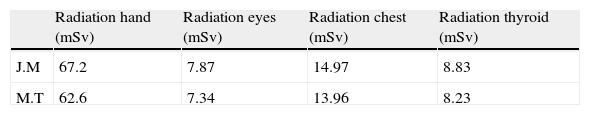
The estimation of the radiation received is far from exceeding the limits described in the current legislation. It shows an asymmetric distribution, affecting the hands in a greater proportion than other locations (Table 3). These calculations did not discriminate between first and second surgeon, assigning the same dose to both.
Radiation from both authors extrapolating the measurements by Tsalafoutas.4
| Radiation hand (mSv) | Radiation eyes (mSv) | Radiation chest (mSv) | Radiation thyroid (mSv) | |
| J.M | 67.2 | 7.87 | 14.97 | 8.83 |
| M.T | 62.6 | 7.34 | 13.96 | 8.23 |
The effective dose limit currently applicable in Spain14 for exposed workers is 100mSv over the entire official period of 5 consecutive years, subject to a maximum effective dose of 50mSv in any official year. The equivalent dose limit is 150mSv per official year for the lens of the eye, and 500mSv for the hands, forearms, feet and ankles. Exposed workers in category A are those who are not unlikely to receive an effective dose of over 6mSv per year or exceed 3/10 of the limits of equivalent doses. The Legislation Proposal of the European Union13 establishes the limits recommended by the ICRP,12 which reduce the maximum equivalent dose in eyes to 20mSv per year. It also highlights the need to train staff working with radiation and the basic principles of justification, optimization and limitation.
The current recommendations in Spain for the use of dose meters and monitoring of the health of staff exposed to radiation14 include using individual dose meters which measure the radiation received by the entire organism representatively, without specifying a location. In the case of non-homogeneous radiation, dose meters should be used in the most exposed areas. Workers exposed to radiation should undergo regular healthcare monitoring. The first should take place before occupying the workplace and should then be repeated at least every year or more often if the person in charge of health and safety considers it necessary. The dose record should be kept until the patient is 75 years old or has not been exposed to ionizing radiation at their workplace for 30 years. The IAEA10 recommends using at least 2 dose meters, one under the lead apron and another above, at the height of the eyes or thyroid. If the hands are near to the focus or run the risk of being directly exposed to Rx, then another wrist or ring dose meter should be added.
The Spanish legislation does not specify protective measures against radiation.14 The IAEA10 recommends using 0.25mm lead aprons (which overlap in the anterior part, creating a protection of 0.50mm in the more exposed areas), a thyroid protector and leaded goggles with lateral protection.
DiscussionAlthough the radiation calculated in 1 year did not exceed the current legal limits, it should still be decreased insofar as possible. One of the most effective measures is to use C-shaped miniarches. Out of all the procedures conducted in 1 year by both authors, over 30% could have been performed with this type of fluoroscope. This would have considerably decreased the exposure of both surgeons (between 5 and 10 times less exposure) and their patients.15 The popularization of C-shaped mini arches began through percutaneous foot surgery, and subsequently extended to hand surgery, followed by the wrists, ankles, forearms, etc. It is not applicable in large joints, as it usually has kilovolt and milliamp limitations, but these devices should be available at all hand, foot and general traumatology units.
There are 2 especially relevant anatomical locations: the eyes and hands. The former are particularly radiosensitive and the latter are very close to the source of X-rays. The effects of radiation on the eyes are being revised in depth. Until recently, it was thought that the dose which caused cataracts by a deterministic effect was 5Gy. These calculations were not correct because they did not take into account the latency time between exposure and the onset of cataracts and did not consider early changes in the lens. Recent studies in patients exposed to low doses of radiation16 have shown changes in the lens at much lower doses than the previous. Early alterations start with very low doses of radiation, which do not affect vision initially, but progress until they opacify the lens. Other authors17 have noted subclinical changes with low doses of radiation, more intense and more dose dependent than among the younger population. Chodick et al.18 studied a cohort of Rx technicians and reached the conclusion that there was no limit after which lens disorders take place, and that small doses of radiation increase the possibility of suffering cataracts in the future. Studies conducted with survivors of the atomic bombs dropped on Hiroshima and Nagasaki3 concluded that minor exposures of 0.8Gy caused cataracts and not only minor opacities in the lens. All these studies have led the maximum authority in radioprotection, the ICRP, to propose new exposure limits.6,7 They define as the radiation threshold for the onset of cataracts as 0.5Gy and recommend a maximum mean annual exposure of 20mSv in the lens over 5 years, with no exposures above 50mSv in any of the years. They also insist that these recommendations should be continually revised and highlight the importance of using eye protection from the beginning because the effect is cumulative. They also recommend greater attention to exposure of the brain and heart because they consider that levels above 0.5Gy can cause permanent circulatory alterations in these organs.
The hands are another especially relevant location, due to their greater exposure. Singer8 found radiation levels 187 higher than those estimated previously. The use of conventional arches for hand, wrist, foot and ankle surgery instead of miniarches leads to a radiation exposure which is between 5 and 10 times higher.15 Other authors19 coincide in noting greater disperse radiation from C-shaped arches compared to mini arches, as well as a substantial increase when the Rx tube is placed above the patient.
There are basic recommendations which are applicable to any orthopedic procedure performed with fluoroscopy.10,20 Some refer to the protection of orthopedic surgeons, which should include lead aprons with a thickness of 0.25mm and overlapping in the front part to create a 0.50mm barrier, thyroid protectors and lead goggles with frontal and lateral protection, as basic equipment. The use of lead or wolfram gloves is useful, as long as the hands of the surgeon do not appear in the image, as this would automatically increase the kV and mA of the fluoroscope, being counterproductive. The other recommendations apply to the correct use of the fluoroscope. The image intensifier should be placed as close to the patient as possible, with the Rx tube under and away from the table. Most of the radiation is absorbed by the patient and only a small part reaches the intensifier. Placing the fluoroscope in this way reduces the disperse radiation in sensitive areas, such as the eyes, thyroid and hands. In some cases, the arch can be inverted, that is, the Rx tube can be placed above and the intensifier can be used to support the limb being operated on. When non-radiotransparent operating tables are used, the arch may have to be inverted and placed obliquely, in order to avoid metallic structures, thus increasing disperse radiation. Oblique projections can multiply this radiation by a factor of 5.21 Fluoroscopes can work with the Rx tube emitting continuously (continuous mode) or in pulses (pulsed mode) which is the correct mode. Another parameter to control is resolution. The highest-resolution mode should only be used in very specific cases, as it increases disperse radiation. The width of the X-ray beam can be reduced using a collimator. This will provide images with a reduced field, which may suffice for certain surgical procedures, especially when the arch does not have to be moved, as in the case of distal nailing.
The training of radiation technicians is fundamental. These must know how to manage all the options of the fluoroscope and facilitate the task and safety of both surgeons and patients. Furthermore, orthopedic surgeons must have updated knowledge about the use and risks of fluoroscopes, always bearing in mind that they are responsible for the radioprotection of their patients.
This study has several limitations. The method used to estimate the exposure of the authors is not the most suitable, as it has a significant error margin. Some authors estimate radiation using C shaped mini arches,8,9 which we do not have, so the real radiation in our case would be greater. Moreover, we have calculated the same dose for surgeons and assistants. While this may be acceptable in hand and foot surgery, in other procedures, like trochanteric nailing, it overestimates the radiation received by assistants. Nevertheless, we consider it as a useful approximation. Depending on the references of previous works used,4,6–9 the 2 authors of the article may have exceeded the 3/10 of the equivalent dose limit marked by the current legislation or not. In any case, it is not highly improbable that this may occur, so they should undoubtedly be considered as workers exposed to category A ionizing radiation.
ConclusionsThe radiation received by the 2 orthopedic surgeons in this study was far from the limits established by the current legislation. Nevertheless, significant amounts were registered for the hands and eyes. Knowledge of the basic rules for radioprotection and fluoroscope operation is essential, as are revisions by the healthcare at work service. Ideally, the Spanish legislation will adopt the European recommendations regarding radioprotection and a reduction of limits for the eyes. Radioprotection goggles and wrist or ring dose meters should be used routinely.
Level of evidenceLevel of evidence IV.
Ethical responsibilitiesProtection of people and animalsThe authors declare that this investigation did not require experiments on humans or animals.
Confidentiality of dataThe authors declare that this work does not reflect any patient data.
Right to privacy and informed consentThe authors declare that this work does not reflect any patient data.
Conflict of interestThe authors have no conflict of interest to declare.
Please cite this article as: Torres-Torres M, Mingo-Robinet J, Moreno Barrero M, Rivas Laso JA, Burón Álvarez I, González Salvador M. Radioprotección en quirófanos de traumatología: ¿en qué situación estamos?. Rev Esp Cir Ortop Traumatol. 2014;58:309–313.